Social Determinants and Prevalence of Antenatal Depression among Women in Rural Bangladesh: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design, Setting, and Sampling
2.2. Survey Instrument
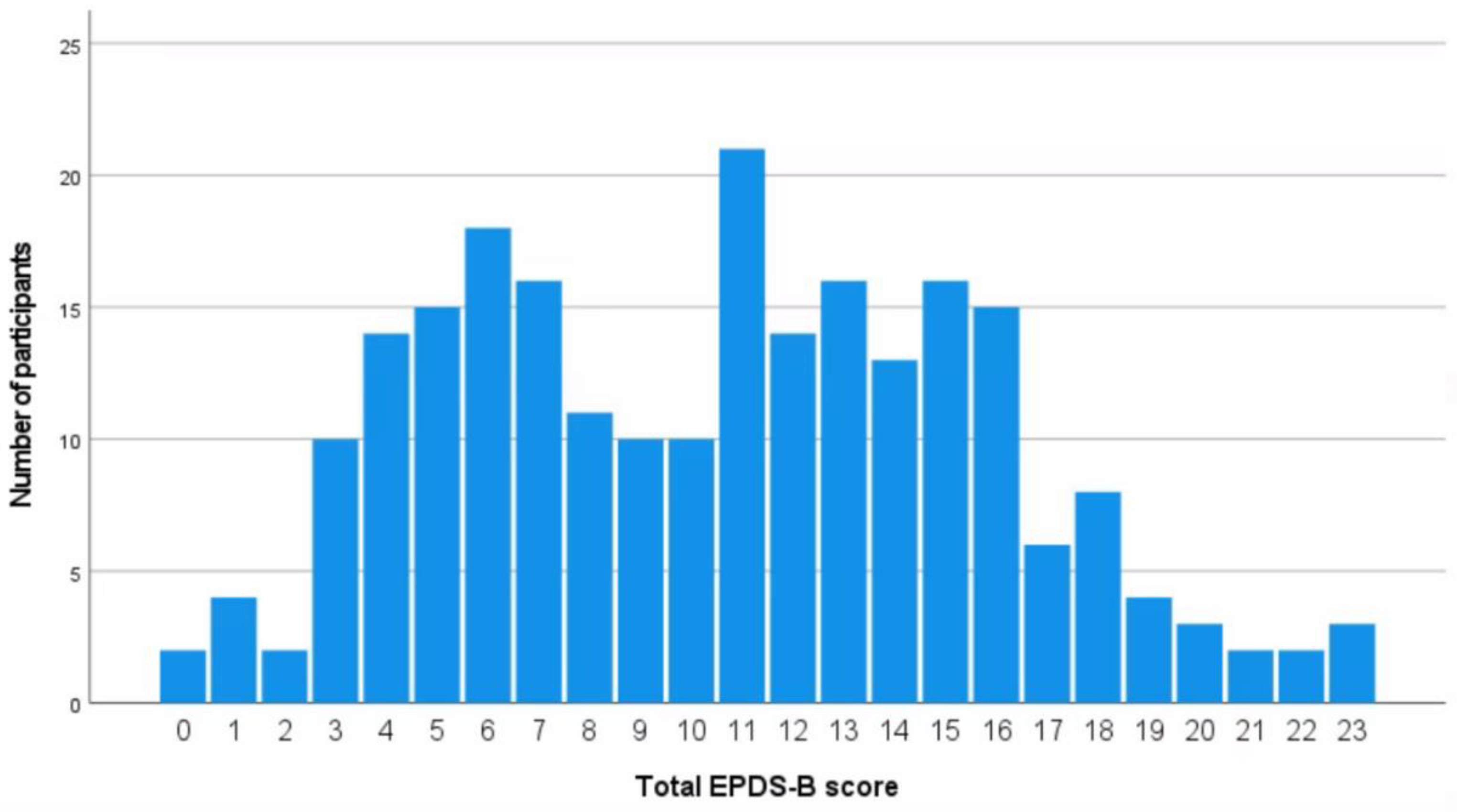
2.3. Dependent/Outcome Variable—Antenatal Depressive Symptoms (ADS)
2.4. Independent Variables—Social Determinants
2.5. Data Collection Procedure
2.6. Statistical Analysis
2.7. Ethical Considerations
3. Results
4. Discussion
4.1. Key Findings
4.2. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- James, S.L.G.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuehner, C. Why is depression more common among women than among men? Lancet Psychiatry 2017, 4, 146–158. [Google Scholar] [CrossRef] [PubMed]
- Nasreen, H.E.; Kabir, Z.N.; Forsell, Y.; Edhborg, M. Prevalence and associated factors of depressive and anxiety symptoms during pregnancy: A population based study in rural Bangladesh. BMC Women’s Health 2011, 11, 22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chandran, M.; Tharyan, P.; Muliyil, J.; Abraham, S. Post-partum depression in a cohort of women from a rural area of Tamil Nadu, India. Incidence and risk factors. Br. J. Psychiatry 2002, 181, 499–504. [Google Scholar] [CrossRef] [Green Version]
- Rahman, A.; Iqbal, Z.; Harrington, R. Life events, social support and depression in childbirth: Perspectives from a rural community in the developing world. Psychol. Med. 2003, 33, 1161–1167. [Google Scholar] [PubMed] [Green Version]
- Hoffman, S.; Hatch, M.C. Depressive symptomatology during pregnancy: Evidence for an association with decreased fetal growth in pregnancies of lower social class women. Health Psychol. 2000, 19, 535–543. [Google Scholar] [CrossRef]
- Overview World Bank. Available online: https://www.worldbank.org/en/country/bangladesh/overview (accessed on 24 December 2021).
- Gausia, K.; Fisher, C.; Ali, M.; Oosthuizen, J. Antenatal depression and suicidal ideation among rural Bangladeshi women: A community-based study. Arch. Women Ment. Health 2009, 12, 351–358. [Google Scholar]
- Howard, L.M.; Khalifeh, H. Perinatal mental health: A review of progress and challenges. World Psychiatry 2020, 19, 313–327. [Google Scholar] [CrossRef]
- Shidhaye, P.; Giri, P. Maternal Depression: A Hidden Burden in Developing Countries. Ann. Med. Health Sci. Res. 2014, 4, 463–465. [Google Scholar] [CrossRef] [Green Version]
- Islam, A. Mental Health and the Health System in Bangladesh: Situation Analysis of a Neglected Domain. AJPN 2015, 3, 57. [Google Scholar] [CrossRef] [Green Version]
- Nuri, N.N.; Sarker, M.; Ahmed, H.U.; Hossain, M.D.; Beiersmann, C.; Jahn, A. Pathways to care of patients with mental health problems in Bangladesh. Int. J. Ment. Health Syst. 2018, 12, 39. [Google Scholar] [CrossRef] [PubMed]
- Islam, S.; Islam, M.A.; Padmadas, S.S. High fertility regions in Bangladesh: A marriage cohort analysis. J. Biosoc. Sci. 2010, 42, 705–719. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kabir, A.; Ali, R.; Islam, M.S.; Kawsar, L.A.; Islam, M.A. A comparison of regional variations of fertility in Bangladesh. Int Q Community Health Educ. 2009, 29, 275–291. [Google Scholar] [CrossRef] [PubMed]
- Joarder, T.; Chaudhury, T.Z.; Mannan, I. Universal Health Coverage in Bangladesh: Activities, Challenges, and Suggestions. Adv. Public Health 2019, 2019, e4954095. [Google Scholar] [CrossRef] [PubMed]
- Pourhoseingholi, M.A.; Vahedi, M.; Rahimzadeh, M. Sample size calculation in medical studies. Gastroenterol. Hepatol. Bed Bench 2013, 6, 14–17. [Google Scholar]
- Bangladesh Map. On the World Map. Available online: https://ontheworldmap.com/bangladesh/ (accessed on 20 January 2022).
- Khan, B.; Avan, B.I. Qualitative adaptation of child behaviour problem instruments in a developing-country setting. East. Mediterr. Health J. 2014, 20, 450–458. [Google Scholar] [CrossRef]
- Gausia, K.; Fisher, C.; Algin, S.; Oosthuizen, J. Validation of the Bangla version of the Edinburgh Postnatal Depression Scale for a Bangladeshi sample. J. Reprod. Infant Psychol. 2007, 25, 308–315. [Google Scholar] [CrossRef]
- Rubertsson, C.; Börjesson, K.; Berglund, A.; Josefsson, A.; Sydsjö, G. The Swedish validation of Edinburgh Postnatal Depression Scale (EPDS) during pregnancy. Nord. J. Psychiatry 2011, 65, 414–418. [Google Scholar] [CrossRef]
- Parkerson, G.R., Jr.; Broadhead, W.E.; Tse, C.K. Validation of the Duke Social Support and Stress Scale. Fam. Med. 1991, 23, 357–360. [Google Scholar] [PubMed]
- Bhopal, S.; Roy, R.; Verma, D.; Kumar, D.; Avan, B.; Khan, B.; Gram, L.; Sharma, K.; Amenga-Etego, S.; Panchal, S.N.; et al. Impact of adversity on early childhood growth & development in rural India: Findings from the early life stress sub-study of the SPRING cluster randomised controlled trial (SPRING-ELS). PLoS ONE 2019, 14, e0209122. [Google Scholar]
- García-Moreno, C.; Jansen, H.A.; Ellsberg, M.; Heise, L.; Watts, C. WHO Multi-Country Study on Women’s Health and Domestic Violence Against Women: Initial Results on Prevalence, Health Outcomes and Women’s Responses; World Health Organization: Geneva, Switzerland, 2005.
- Riley, R.D.; Ensor, J.; I E Snell, K.; Jr, F.E.H.; Martin, G.P.; Reitsma, J.B.; Moons, K.G.M.; Collins, G.; van Smeden, M. Calculating the sample size required for developing a clinical prediction model. BMJ 2020, 368, m441. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gul, F.; Sherin, A.; Jabeen, M.; Khan, S.A. Association of stress with anxiety and depression during pregnancy. J. Pak. Med. Assoc. 2017, 67, 1803–1808. [Google Scholar] [PubMed]
- Sheeba, B.; Nath, A.; Metgud, C.S.; Krishna, M.; Venkatesh, S.; Vindhya, J.; Murthy, G.V.S. Prenatal Depression and Its Associated Risk Factors Among Pregnant Women in Bangalore: A Hospital Based Prevalence Study. Front. Public Health 2019, 7, 108. [Google Scholar] [CrossRef] [PubMed]
- Insan, N.; Weke, A.; Forrest, S.; Rankin, J. Social determinants of antenatal depression and anxiety among women in South Asia: A systematic review & meta-analysis. PLoS ONE 2022, 17, e0263760. [Google Scholar]
- Visentin, D.C.; Cleary, M.; Hunt, G.E. The earnestness of being important: Reporting non-significant statistical results. J. Adv. Nurs. 2020, 76, 917–919. [Google Scholar] [CrossRef] [Green Version]
- Gelaye, B.; Rondon, M.B.; Araya, R.; Williams, M.A. Epidemiology of maternal depression, risk factors, and child outcomes in low-income and middle-income countries. Lancet Psychiatry 2016, 3, 973–982. [Google Scholar] [CrossRef] [Green Version]
- Rouhi, M.; Rouhi, N.; Vizheh, M.; Salehi, K. Male child preference: Is it a risk factor for antenatal depression among Iranian women? Br. J. Midwifery 2017, 25, 572–578. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, Y.; Wen, S.; Guo, X.; Xu, L.; Chen, B.; Chen, P.; Xu, X.; Wang, Y. Association between social and family support and antenatal depression: A hospital-based study in Chengdu, China. BMC Pregnancy Childbirth 2019, 19, 420. [Google Scholar] [CrossRef] [Green Version]
- George, C.; Lalitha, A.R.N.; Antony, A.; Kumar, A.V.; Jacob, K.S. Antenatal depression in coastal South India: Prevalence and risk factors in the community. Int. J. Soc. Psychiatry 2016, 62, 141–147. [Google Scholar] [CrossRef]
- Shidhaye, P.; Shidhaye, R.; Phalke, V. Association of gender disadvantage factors and gender preference with antenatal depression in women: A cross-sectional study from rural Maharashtra. Soc. Psychiatry Psychiatr. Epidemiol. 2017, 52, 737–748. [Google Scholar] [CrossRef]
- Loo, K.K.; Li, Y.; Tan, Y.; Luo, X.; Presson, A.; Shih, W. Prenatal anxiety associated with male child preference among expectant mothers at 10–20 weeks of pregnancy in Xiangyun County, China. Int. J. Gynaecol. Obstet. 2010, 111, 229–232. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sayem, A.M.; Nury, A.T.M.d.S. An assessment of attitude towards equitable gender norms among Muslim women in Bangladesh. Women’s Stud. Int. Forum 2013, 40, 102–110. [Google Scholar] [CrossRef]
- Williams, A.; Sarker, M.; Ferdous, S.T. Cultural Attitudes toward Postpartum Depression in Dhaka, Bangladesh. Med. Anthropol. 2018, 37, 194–205. [Google Scholar] [CrossRef]

| Variable | Study Sample (n = 235) |
|---|---|
| Age | |
| Median age in years, (IQR) | 25 (6) |
| Trimester, n (%) | |
| First | 57 (24.2) |
| Second | 100 (42.6) |
| Third | 71 (30.3) |
| Unknown | 7 (3.0) |
| Marital status, n (%) | |
| Married | 235 (100) |
| Highest level of education, n (%) | |
| No schooling/Pre-SSC | 178 (75.8) |
| SSC or above | 56 (23.8) |
| Do not know | 1 (0.4) |
| Paid work, n (%) | |
| Yes | 5 (2.1) |
| No | 230 (97.9) |
| Gender of baby, n (%) | |
| Girl | 7 (3.0) |
| Boy | 9 (3.8) |
| Do not know | 207 (88.1) |
| Prefer not to say | 12 (5.1) |
| Gender preference, n (%) | |
| Girl | 31 (13.2) |
| Boy | 51 (21.7) |
| No preference | 133 (56.6) |
| Prefer not to say | 20 (8.5) |
| Perceived husband’s gender preference, n (%) | |
| Girl | 30 (12.8) |
| Boy | 65 (27.7) |
| No preference | 119 (50.6) |
| Prefer not to say | 21 (8.9) |
| Want pregnancy, n (%) | |
| Yes | 142 (60.4) |
| No | 20 (8.5) |
| Prefer not to say | 73 (31.1) |
| Perceive husband wants pregnancy, n (%) | |
| Yes | 152 (64.7) |
| No | 17 (7.2) |
| Prefer not to say | 66 (28.1) |
| Worried about childbirth/labour, n (%) | |
| Yes | 200 (85.1) |
| No | 17 (7.2) |
| Prefer not to say | 18 (7.7) |
| Family support | |
| Family support score, mean (SD) | 50.0 (17.3) |
| Intimate Partner Violence (IPV), n (%) | |
| Before pregnancy | |
| Yes | 64 (27.2) |
| No | 86 (36.6) |
| Prefer not to say | 85 (36.2) |
| During pregnancy | |
| Yes | 32 (13.6) |
| No | 110 (46.8) |
| Prefer not to say | 93 (39.6) |
| Antenatal Depressive Symptoms (ADS), n (%) | |
| Yes | 133 (56.6) |
| No | 102 (43.4) |
| Variables | ADS n = 133 (%) | Non-ADS n = 102 (%) | p-Value c |
|---|---|---|---|
| Trimester | |||
| First | 33 (24.8) | 24 (23.5) | |
| Second | 56 (42.1) | 44 (43.1) | 0.79 |
| Third | 37 (27.8) | 34 (33.3) | |
| Education | |||
| No schooling/Pre-SSC | 106 (79.7) | 72 (70.6) | 0.084 |
| SSC or above | 26 (19.5) | 30 (29.4) | |
| IPV before pregnancy | |||
| Yes | 53 (39.8) | 11 (10.8) | <0.001 * |
| No | 37 (27.8) | 49 (48.0) | |
| IPV during pregnancy | |||
| Yes | 26 (19.5) | 6 (5.88) | 0.002 * |
| No | 56 (42.1) | 54 (52.9) | |
| Gender preference | |||
| Boy | 38 (28.6) | 13 (12.7) | |
| Girl | 15 (11.3) | 16 (15.7) | 0.013 * |
| No preference | 69 (51.9) | 64 (62.7) | |
| Perceived husband’s gender preference | |||
| Boy | 51 (38.3) | 14 (13.7) | |
| Girl | 15 (11.3) | 15 (14.7) | <0.001 * |
| No preference | 57 (42.9) | 62 (60.8) | |
| Want baby | |||
| Yes | 89 (66.9) | 53 (52.0) | 0.524 |
| No | 14 (10.5) | 6 (5.9) | |
| Perceive husband wants pregnancy | |||
| Yes | 99 (74.4) | 53 (52.0) | 0.606 |
| No | 10 (7.5) | 7 (6.9) | |
| Variables | ADS mean (SD) | Non-ADS mean (SD) | p-value t |
| Age | 24.33 (5.43) | 24.23 (4.20) | 0.871 |
| Family support | 46.4 (18.7) | 52.3 (14.7) | 0.009 * |
| Variables | AOR (95% CI) | p-Value c |
|---|---|---|
| IPV before pregnancy | ||
| Yes | 10.4 (2.7–39.7) | <0.001 * |
| No | 1 | |
| IPV during pregnancy | ||
| Yes | 1.4 (0.3–7.1) | 0.656 |
| No | 1 | |
| Gender preference | ||
| Boy | 0.21 (0.04–1.2) | 0.085 |
| Girl | 0.34 (0.04–3.2) | 0.348 |
| No preference | 1 | |
| Perceived husband’s gender preference | ||
| Boy | 9.9 (1.6–59.6) | 0.012 * |
| Girl | 2.4 (0.29–19.1) | 0.418 |
| No preference | 1 | |
| Variables | p-value t | |
| Family support | 0.94 (0.91–0.97) | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Insan, N.; Forrest, S.; Jaigirdar, A.; Islam, R.; Rankin, J. Social Determinants and Prevalence of Antenatal Depression among Women in Rural Bangladesh: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 2364. https://doi.org/10.3390/ijerph20032364
Insan N, Forrest S, Jaigirdar A, Islam R, Rankin J. Social Determinants and Prevalence of Antenatal Depression among Women in Rural Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(3):2364. https://doi.org/10.3390/ijerph20032364
Chicago/Turabian StyleInsan, Nafisa, Simon Forrest, Aqil Jaigirdar, Reduanul Islam, and Judith Rankin. 2023. "Social Determinants and Prevalence of Antenatal Depression among Women in Rural Bangladesh: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 3: 2364. https://doi.org/10.3390/ijerph20032364
APA StyleInsan, N., Forrest, S., Jaigirdar, A., Islam, R., & Rankin, J. (2023). Social Determinants and Prevalence of Antenatal Depression among Women in Rural Bangladesh: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(3), 2364. https://doi.org/10.3390/ijerph20032364





