Innovative Pedagogical Strategies in Health Professions Education: Active Learning in Dental Materials Science
Abstract
1. Introduction
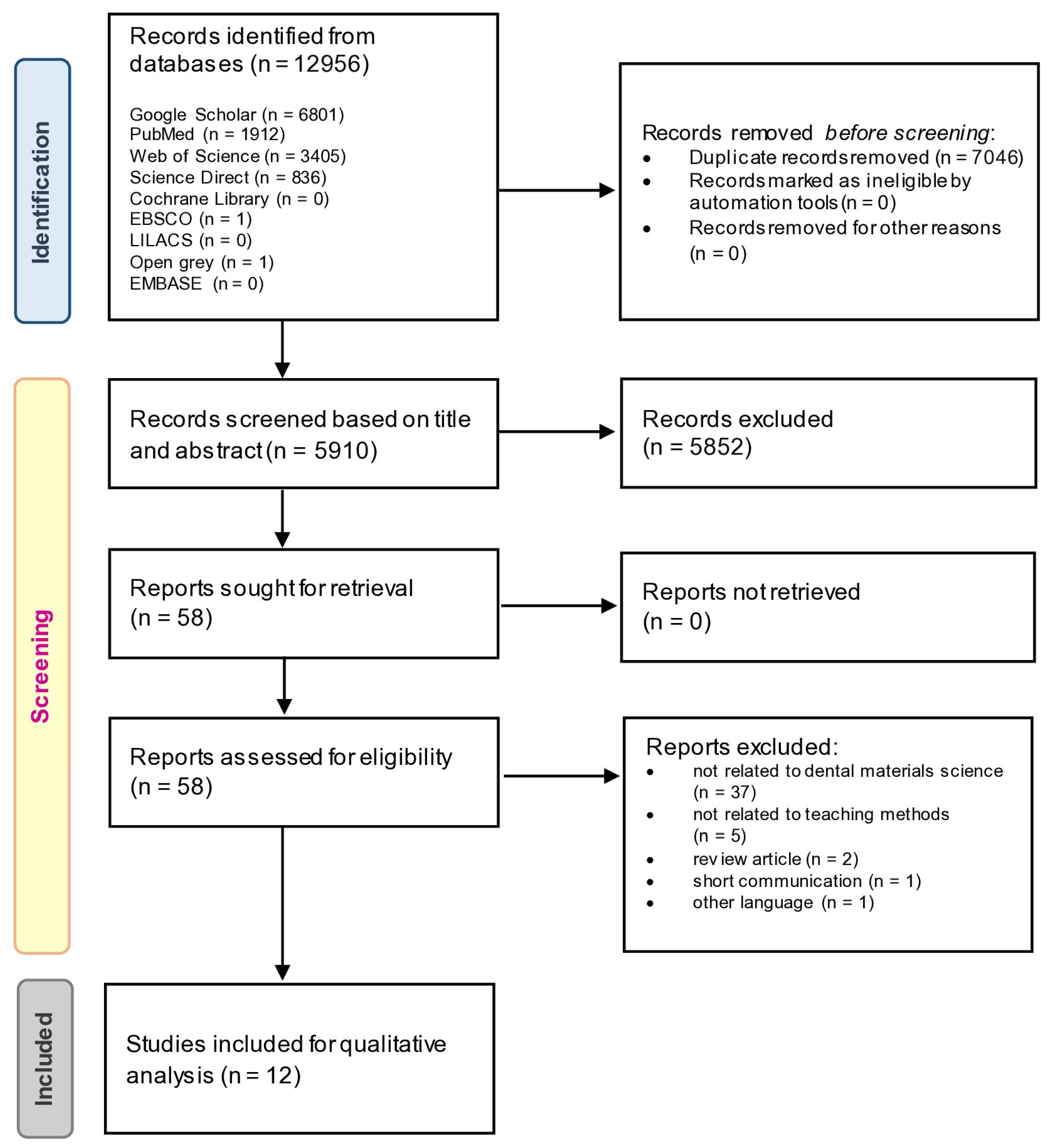
2. Materials and Methods
2.1. Search Strategy
2.2. Study Selection
- (1)
- Randomized, non-randomized, cohort, case-control, or cross-sectional studies.
- (2)
- Presented in the English language.
- (3)
- Teaching methods for dental materials science courses.
- (1)
- Expert opinions, short communications, reviews, case reports, or case series.
- (2)
- Teaching methods for other dental-related courses.
2.3. Data Extraction
2.4. Risk of Bias Assessment
3. Results
3.1. Search Strategy
3.2. Risk of Bias Assessment
3.3. Pedagogical Strategies
3.3.1. Flipped Classroom
3.3.2. Clinical-Based Learning
3.3.3. Computer-Assisted Learning
3.3.4. Group Discussion
3.3.5. Microteaching with BOPPPS Model
3.3.6. Game-Based Learning
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Komabayashi, T.; Razak, A.A.; Bird, W.F. Dental education in Malaysia. Int. Dent J. 2007, 57, 429–432. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.S.S.; Tan, W.W.; Afrashtehfar, K.I. Exploring the Learning Experience of High-Performing Preclinical Undergraduate Dental Students: A Qualitative Study. Educ. Sci. 2022, 12, 801. [Google Scholar] [CrossRef]
- Yang, Y.; You, J.; Wu, J.; Hu, C.; Shao, L. The Effect of Microteaching Combined with the BOPPPS Model on Dental Materials Education for Predoctoral Dental Students. J. Dent. Educ. 2019, 83, 567–574. [Google Scholar] [CrossRef] [PubMed]
- Gali, S.; Shetty, V.; Murthy, N.S.; Marimuthu, P. Bridging the gap in 1(st) year dental material curriculum: A 3 year randomized cross over trial. J. Indian Prosthodont. Soc. 2015, 15, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Kumar, V.; Gadbury-Amyot, C.C. A case-based and team-based learning model in oral and maxillofacial radiology. J. Dent. Educ. 2012, 76, 330–337. [Google Scholar] [CrossRef]
- Soni, V.; Kotsane, D.F.; Moeno, S.; Molepo, J. Perceptions of students on a stand-alone dental materials course in a revised dental curriculum. Eur. J. Dent. Educ. 2021, 25, 117–123. [Google Scholar] [CrossRef] [PubMed]
- Vanka, A.; Vanka, S.; Wali, O. Flipped classroom in dental education: A scoping review. Eur. J. Dent. Educ. 2020, 24, 213–226. [Google Scholar] [CrossRef] [PubMed]
- Chuenjitwongsa, S.; Oliver, R.G.; Bullock, A.D. Competence, competency-based education, and undergraduate dental education: A discussion paper. Eur. J. Dent. Educ. 2018, 22, 1–8. [Google Scholar] [CrossRef]
- Yip, H.K.; Smales, R.J.; Newsome, P.R.; Chu, F.C.; Chow, T.W. Competency-based education in a clinical course in conservative dentistry. Br. Dent. J. 2001, 191, 517–522. [Google Scholar] [CrossRef]
- Lee, C.; Kim, S.W. Effectiveness of a Flipped Classroom in Learning Periodontal Diagnosis and Treatment Planning. J. Dent Educ. 2018, 82, 614–620. [Google Scholar] [CrossRef]
- Saran, R.; Kumar, S. Use of crossword puzzle as a teaching aid to facilitate active learning in dental materials. Indian J. Appl. Res. 2015, 5, 456–457. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef]
- OCEBM Levels of Evidence Working Group. “The Oxford Levels of Evidence 2”. Oxford Centre for Evidence-Based Medicine. Available online: https://www.cebm.ox.ac.uk/resources/levels-of-evidence/ocebm-levels-of-evidence (accessed on 23 November 2022).
- Sagsoz, O.; Karatas, O.; Turel, V.; Yildiz, M.; Kaya, E. Effectiveness of Jigsaw learning compared to lecture-based learning in dental education. Eur. J. Dent Educ. 2017, 21, 28–32. [Google Scholar] [CrossRef]
- Joshi, J.P.; Deshmukh, S.P.; Kahar, A.R.; Radke, U.M. Flipped Classroom: The future classroom for Dental Students? JIDA J. Indian Dent. Assoc. 2018, 12, 12–17. [Google Scholar]
- Qazi, H.S.; Ashar, A.; Ahmad, S.A. Impact of an innovative approach of teaching science of dental materials on the learning experiences of undergraduate students. PAFMJ 2019, 69, 582–588. [Google Scholar]
- Binnie, R.S.L.; Bonsor, S.J. The implementation of a flipped classroom approach at a UK dental school. Br. Dent. J. 2021, 231, 405–408. [Google Scholar] [CrossRef]
- Kruppke, B. Digital Experiments in Higher Education—A “How to” and “How It Went” for an Interactive Experiment Lecture on Dental Materials. Educ. Sci. 2021, 11, 190. [Google Scholar] [CrossRef]
- Barbour, M.E. Electronic Voting in Dental Materials Education: The Impact on Students’ Attitudes and Exam Performance. J. Dent. Educ. 2008, 72, 1042–1047. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Tang, L.; Li, S.; Gong, X. Set Up and Practice of a Model of “Integrated-Into-Clinic” in the Teaching of Dental Materials. Int. J. Humanit. Soc. Sci. Educ. 2018, 5, 103–106. [Google Scholar]
- Doloca, A.; Tanculescu, O.; Trandafir, L.; Ciongradi, I.; Stoleriu, S.; Mocanu, R.; Ifteni, G. Dental Materials and Their Selection–Virtual Patient (VP) Software from a Student Perspective. Mater. Plast. 2016, 53, 370–374. [Google Scholar]
- Deshpande, S.; Joshi, J.; Radke, U. Effect of dental laboratory exposure on dental students: A preliminary investigation. MedEdPublish 2018, 7, 12. [Google Scholar] [CrossRef]
- Dong, Y.; Yin, H.; Du, S.; Wang, A. The effects of flipped classroom characterized by situational and collaborative learning in a community nursing course: A quasi-experimental design. Nurse Educ. Today 2021, 105, 105037. [Google Scholar] [CrossRef]
- Wang, Z.; Kohno, E.Y.; Fueki, K.; Ueno, T.; Inamochi, Y.; Takada, K.; Wakabayashi, N. Multilevel factor analysis of flipped classroom in dental education: A 3-year randomized controlled trial. PLoS ONE 2021, 16, e0257208. [Google Scholar] [CrossRef]
- Gianoni-Capenakas, S.; Lagravere, M.; Pacheco-Pereira, C.; Yacyshyn, J. Effectiveness and Perceptions of Flipped Learning Model in Dental Education: A Systematic Review. J. Dent. Educ. 2019, 83, 935–945. [Google Scholar] [CrossRef]
- Chuang, H.-H.; Weng, C.-Y.; Chen, C.-H. Which students benefit most from a flipped classroom approach to language learning? Br. J. Educ. Technol. 2018, 49, 56–68. [Google Scholar] [CrossRef]
- van der Hoeven, D.; Zhu, L.; Busaidy, K.; Quock, R.L.; Holland, J.N.; van der Hoeven, R. Integration of Basic and Clinical Sciences: Student Perceptions. Med. Sci. Educ. 2020, 30, 243–252. [Google Scholar] [CrossRef]
- Serrano, C.M.; Botelho, M.G.; Wesselink, P.R.; Vervoorn, J.M. Challenges in the transition to clinical training in dentistry: An ADEE special interest group initial report. Eur. J. Dent. Educ. 2018, 22, e451–e457. [Google Scholar] [CrossRef]
- Paolone, G.; Mazzitelli, C.; Formiga, S.; Kaitsas, F.; Breschi, L.; Mazzoni, A.; Tete, G.; Polizzi, E.; Gherlone, E.; Cantatore, G. One-year impact of COVID-19 pandemic on Italian dental professionals: A cross-sectional survey. Minerva Dent. Oral Sci. 2022, 71, 212–222. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos, L.M. Online learning after the COVID-19 pandemic: Learners’ motivations. Front. Educ. 2022, 7, 879091. [Google Scholar] [CrossRef]
- Ali, K.; Zahra, D.; McColl, E.; Salih, V.; Tredwin, C. Impact of early clinical exposure on the learning experience of undergraduate dental students. Eur. J. Dent Educ. 2018, 22, e75–e80. [Google Scholar] [CrossRef]
- Towns, M.H.; Kreke, K.; Fields, A. An Action Research Project: Student Perspectives on Small-Group Learning in Chemistry. J. Chem. Educ. 2000, 77, 111. [Google Scholar] [CrossRef]
- Deshpande, S.R.; Shastri, S. A cross-sectional study to evaluate teaching skills of postgraduate medical students using component skill approach in microteaching. J. Educ. Health Promot. 2020, 9, 362. [Google Scholar] [PubMed]
- Shekharappa, K.R.; Tejaswi, C.N.; Patil, S.S.; Lakshmikanth, B.M. Microteaching revisited! A tool for improving undergraduate student seminars. Indian J. Physiol. Pharmacol. 2021, 64, S70–S75. [Google Scholar] [CrossRef]
- Hu, K.; Ma, R.J.; Ma, C.; Zheng, Q.K.; Sun, Z.G. Comparison of the BOPPPS model and traditional instructional approaches in thoracic surgery education. BMC Med. Educ. 2022, 22, 447. [Google Scholar] [CrossRef]
- Gudadappanavar, A.M.; Benni, J.M.; Javali, S.B. Effectiveness of the game-based learning over traditional teaching-learning strategy to instruct pharmacology for Phase II medical students. J. Educ. Health Promot. 2021, 10, 91. [Google Scholar]
- Koivisto, J.-M.; Haavisto, E.; Niemi, H.; Katajisto, J.; Multisilta, J. Elements Explaining Learning Clinical Reasoning Using Simulation Games. Int. J. Serious Games 2016, 3, 29–43. [Google Scholar] [CrossRef]
- Saxena, A.; Nesbitt, R.; Pahwa, P.; Mills, S. Crossword puzzles: Active learning in undergraduate pathology and medical education. Arch. Pathol. Lab. Med. 2009, 133, 1457–1462. [Google Scholar] [CrossRef]
- Patrick, S.; Vishwakarma, K.; Giri, V.P.; Datta, D.; Kumawat, P.; Singh, P.; Matreja, P.S. The usefulness of crossword puzzle as a self-learning tool in pharmacology. J. Adv. Med. Educ. Prof. 2018, 6, 181. [Google Scholar]
- Rosenberg, H.; Grad, H.A.; Matear, D.W. The Effectiveness of Computer-Aided, Self-Instructional Programs in Dental Education: A Systematic Review of the Literature. J. Dent. Educ. 2003, 67, 524–532. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Maatouk, R.M.; McCullagh, A.P.G. Flipped Classroom Questions. Br. Dent. J. 2022, 232, 285. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I. Use of Evidence-Based Practice Among New Dental Graduates Needs Improving. Br. Dent. J. 2022, 232, 458. [Google Scholar] [CrossRef] [PubMed]

| Search Strategy | |
|---|---|
| #1 | ((teaching AND dental material) OR (teaching AND dental materials) OR (teaching AND dental biomaterial) OR (teaching AND dental biomaterials) OR (teaching AND dental materials science) OR (teaching AND dental materials science)) |
| #2 | ((pedagogy AND dental material) OR (pedagogy AND dental materials) OR (pedagogy AND dental biomaterial) OR (pedagogy AND dental biomaterials) OR (pedagogy AND dental materials science) OR (pedagogy AND dental materials science)) |
| #3 | ((pedagogical AND dental material) OR (pedagogical AND dental materials) OR (pedagogical AND dental biomaterial) OR (pedagogical AND dental biomaterials) OR (pedagogical AND dental materials science) OR (pedagogical AND dental materials science)) |
| #4 | ((instruction AND dental material) OR (instruction AND dental materials) OR (instruction AND dental biomaterial) OR (instruction AND dental biomaterials) OR (instruction AND dental materials science) OR (instruction AND dental materials science)) |
| #5 | ((learning AND dental material) OR (learning AND dental materials) OR (learning AND dental biomaterial) OR (learning AND dental biomaterials) OR (learning AND dental materials science) OR (learning AND dental materials science)) |
| #6 | ((training AND dental material) OR (training AND dental materials) OR (training AND dental biomaterial) OR (training AND dental biomaterials) OR (training AND dental materials science) OR (training AND dental materials science)) |
| #7 | ((coaching AND dental material) OR (coaching AND dental materials) OR (coaching AND dental biomaterial) OR (coaching AND dental biomaterials) OR (coaching AND dental materials science) OR (coaching AND dental materials science)) |
| #8 | ((education AND dental material) OR (education AND dental materials) OR (education AND dental biomaterial) OR (education AND dental biomaterials) OR (education AND dental materials science) OR (education AND dental materials science)) |
| No. | Author | Year | Country | No. of Participant | Study Design | Teaching Method | General Outcomes |
|---|---|---|---|---|---|---|---|
| 1 | Gali, S. et al. [4] | 2015 | India | 170 UG students | RCT | Case-oriented small group discussions | Students felt that group discussions were more interesting, more comfortable asking questions, helped them understand the subject better, and provided a clearer picture for clinical correlation compared to traditional lecture classes. |
| 2 | Yang, Y. et al. [3] | 2019 | China | 105 fourth-year PD students | NRCT (historically controlled study) | Microteaching combined with the BOPPPS model | Microteaching with the BOPPPS model can increase dental students’ enthusiasm and interest, promote critical thinking, and boost students’ academic performance as well as teaching quality. |
| 3 | Binnie, R.S.L. et al. [20] | 2021 | U.K. | N/A | NRCT (controlled before-and-after study) | FC | Most students were satisfied with the FC approach delivery strategy, instruction time allotted, information accessibility, and content understanding. Students also concurred that the FC was enjoyable and effective. |
| 4 | Qazi, H.S. et al. [19] | 2019 | Pakistan | 101 first-year UG students | NRCT (historically controlled study) | Clinical rotation | Significant improvement in the clinical correlation of dental materials among students, along with higher satisfaction levels and more positive perceptions. Although it required more resources, the faculty found it a pleasant experience. |
| 5 | Saran, R. et al. [11] | 2015 | India | 70 second-year UG students | NRCT (cross-sectional study) | Crossword puzzle | Most students claimed that crossword puzzles aided in effective teaching and comprehension of the topic, making the learning process more productive. They generally supported this teaching method in dental materials. |
| 6 | Kruppke, B. [21] | 2021 | Germany | N/A | NRCT (cross-sectional study) | Digital spaced-experimental lectures | The technical implementation of the experimental lecture in the digital space was rated very well among students. The technical methods for activating the students also received positive feedback. |
| 7 | Deshpande, S. et al. [25] | 2018 | India | 60 second-year UG students | NRCT | Computer-assisted lecture + video and live demonstration | There was an improved understanding of related topics among students in the experimental group, evident from their test scores, and students perceived the teaching method positively. |
| 8 | Joshi, J.P. et al. [18] | 2018 | India | 80 second-year UG students | RCT | FC | Despite that the assessment score of students in the FC model was superior to that of the traditional classroom model, there was no significant difference in knowledge content. |
| 9 | Barbour, M.E. [22] | 2008 | U.K. | 142 second-year UG students | NRCT (historically controlled study) | Electronic voting | eVoting system had no significant impact on students’ examination results, but it received favorable perceptions among students, with greater learning engagement. |
| 10 | Sagsoz, O. et al. [17] | 2015 | Turkey | 50 third-year UG students | RCT | Jigsaw learning | The pre-test and the post-test found no discernible difference between the lecture-based and Jigsaw methods, but the Jigsaw learning performed better in the retention test. |
| 11 | Zhao, X. et al. [23] | 2018 | China | N/A | NRCT (cross-sectional study) | “Integrated-Into-Clinic” model | Both teaching and learning efficiency increased significantly with teachers having more time to allocate the fundamental knowledge-based teaching, while students desired to learn and the competence for self-directed learning improved. |
| 12 | Doloca, A. et al. [24] | 2016 | Romania | 73 third-year UG students | NRCT (cross-sectional study) | Virtual Patient (VP) software | The results indicated that VP could be an efficient tool for improving knowledge assimilation and clinical skills. This strategy received a good response and acceptance from the students. |
| Component Study | Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) Assessment Tool | Level of Evidence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Bias Due to Confounding | Bias in Selection of Participants into the Study | Bias in Classification of Interventions | Bias Due to Deviations from Intended Interventions | Bias Due to Missing Data | Bias in Measurement of Outcomes | Bias in Selection of the Reported Result | Overall Risk | ||
| Yang, Y. et al. [3] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Binnie, R.S.L. et al. [20] | Low | NI | NI | Low | Low | Moderate | Low | Moderate | 3 |
| Qazi, H.S. et al. [19] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Saran, R. et al. [11] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Kruppke, B. [21] | Low | NI | NI | NI | NI | Low | Moderate | Moderate | 3 |
| Deshpande, S. et al. [25] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Barbour, M.E. [22] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Zhao, X. et al. [23] | Low | Low | Low | Low | Low | Moderate | Moderate | Moderate | 3 |
| Doloca, A. et al. [24] | Low | Low | Low | Low | Low | Low | Low | Low | 3 |
| Revised Cochrane risk-of-bias tool for randomized trials (RoB 2) | |||||||||
| Risk of bias arising from the randomization process | Risk of bias due to deviations from the intended interventions | Risk of bias due to missing outcome data | Risk of bias in measurement of the outcome | Risk of bias in selection of the reported result | Overall Risk | ||||
| Gali, S. et al. [4] | Some concern | Low | High | Low | Low | High | 2 | ||
| Joshi, J.P. et al. [18] | Some concern | Low | Low | Low | Low | Some concern | 2 | ||
| Sagsoz, O. et al. [17] | Some concern | Low | Low | Low | Low | Some concern | 2 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, G.S.S.; Tan, W.-W.; Tan, H.-J.; Khoo, C.-W.; Afrashtehfar, K.I. Innovative Pedagogical Strategies in Health Professions Education: Active Learning in Dental Materials Science. Int. J. Environ. Res. Public Health 2023, 20, 2041. https://doi.org/10.3390/ijerph20032041
Lin GSS, Tan W-W, Tan H-J, Khoo C-W, Afrashtehfar KI. Innovative Pedagogical Strategies in Health Professions Education: Active Learning in Dental Materials Science. International Journal of Environmental Research and Public Health. 2023; 20(3):2041. https://doi.org/10.3390/ijerph20032041
Chicago/Turabian StyleLin, Galvin Sim Siang, Wen-Wu Tan, Hung-Jia Tan, Chia-Wee Khoo, and Kelvin I. Afrashtehfar. 2023. "Innovative Pedagogical Strategies in Health Professions Education: Active Learning in Dental Materials Science" International Journal of Environmental Research and Public Health 20, no. 3: 2041. https://doi.org/10.3390/ijerph20032041
APA StyleLin, G. S. S., Tan, W.-W., Tan, H.-J., Khoo, C.-W., & Afrashtehfar, K. I. (2023). Innovative Pedagogical Strategies in Health Professions Education: Active Learning in Dental Materials Science. International Journal of Environmental Research and Public Health, 20(3), 2041. https://doi.org/10.3390/ijerph20032041







