Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports
Abstract
1. Introduction
- Analyze SFMA applicability for a physiotherapist in a sport setting.
- Evaluate SFMA reliability for unexperienced raters, once properly trained.
2. Materials and Methods
2.1. Methodology
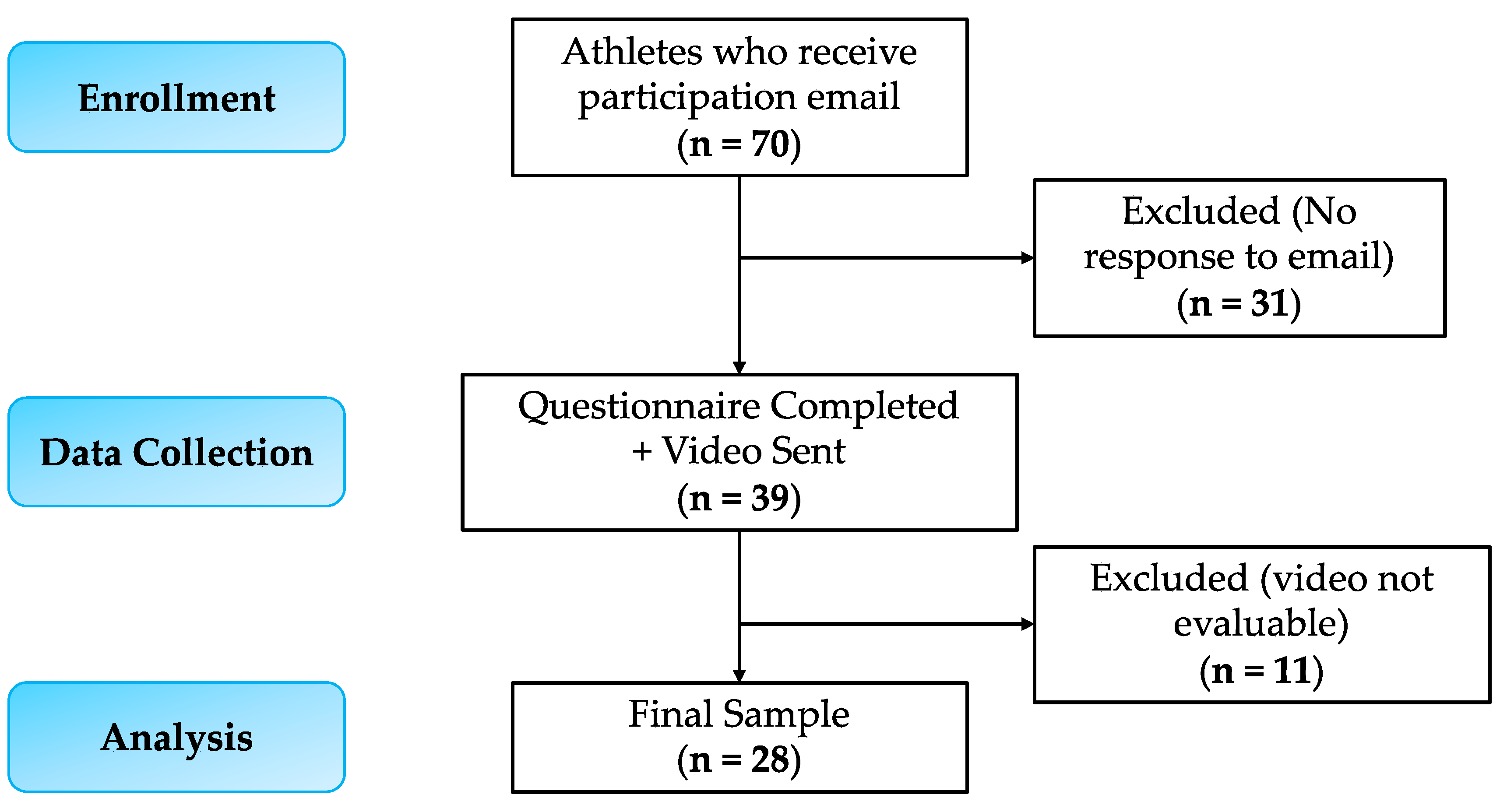
2.2. Participants
- Aged between 15 and 22 years.
- Competitive participation in one of the following sports: football, volleyball, athletics, fencing.
- A minimum of 5 years’ experience in the same sport.
- A frequency of at least 4 training sessions per week.
- Previous major musculoskeletal surgery.
- Limb fracture in the last 6 months.
- Limb muscle injury in the last 3 months.
2.3. SFMA Evaluation
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviation
| SFMA | Selective Functional Movement Assessment; |
| FN | Functional non-painful; |
| FP | Functional painful; |
| DN | Dysfunctional non-painful; |
| DP | Dysfunctional painful; |
| RI | Regional interdependence |
| C Flex | Cervical Flexion; |
| C Ext | Cervical Extension; |
| C Rot R | Cervical Rotation Right; |
| C Rot L | Cervical Rotation Left; |
| UE pattern 1 Right | Upper Extremity Pattern 1 Right; |
| UE pattern 1 Left | Upper Extremity Pattern 1 Left; |
| UE pattern 2 Right | Upper Extremity Pattern 2 Right; |
| UE pattern 2 Left | Upper Extremity Pattern 2 Left; |
| MSF | Multi-Segmental Flexion; |
| MSE | Multi-Segmental Extension; |
| MSR Right | Multi-Segmental Rotation Right; |
| MSR Left | Multi-Segmental Rotation Left; |
| SLS 1 Right | Single Leg Stance 1 Right; |
| SLS 1 Left | Single Leg Stance 1 Left; |
| SLS 2 Right | Single Leg Stance 2 Right; |
| SLS 2 Left | Single Leg Stance 2 Left; |
| K | Cohen’s Kappa |
References
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional Movement Screening: The Use of Fundamental Movements as an Assessment of Function—Part 1. Int. J. Sport Phys. 2014, 9, 396–409. [Google Scholar]
- Cook, G.; Burton, L.; Hoogenboom, B.J.; Voight, M. Functional Movement Screening: The Use of Fundamental Movements as an Assessment of Function—Part 2. Int. J. Sports Phys. Ther. 2014, 9, 549–563. [Google Scholar] [PubMed]
- Stanek, J.M.; Smith, J.; Petrie, J. Intra—And Inter-rater reliability of the selective Functional movement assessment (SFMA) in healthy participants. Int. J. Sports Phys. Ther. 2019, 14, 107. [Google Scholar] [CrossRef]
- Fauntroy, V.; Fyock, M.; Hansen-Honeycutt, J.; Nolton, E.; Ambegaonkar, J.P. Using the Selective Functional Movement Assessment for the Evaluation of Dancers’ Functional Limitations and Dysfunctions: A Critically Appraised Topic. J. Sport Rehabil. 2019, 28, 891–896. [Google Scholar] [CrossRef] [PubMed]
- Wainner, R.S.; Whitman, J.M.; Cleland, J.A.; Flynn, T.W. Regional Interdependence: A Musculoskeletal Examination Model Whose Time Has Come. J. Orthop. Sports Phys. Ther. 2007, 37, 658–660. [Google Scholar] [CrossRef] [PubMed]
- Fernández-De-Las-Peñas, C.; Cleland, J.A.; Huijbregts, P.; Palomeque-Del-Cerro, L.; González-Iglesias, J. Repeated Applications of Thoracic Spine Thrust Manipulation Do Not Lead to Tolerance in Patients Presenting with Acute Mechanical Neck Pain: A Secondary Analysis. J. Man Manip Ther. 2009, 17, 154–162. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, M.J.D.; McRae, M.; Palmer, J.A.; Stowell, T. Immediate Effects of Thoracic Manipulation in Patients with Neck Pain: A Randomized Clinical Trial. Man Ther. 2005, 10, 127–135. [Google Scholar] [CrossRef]
- González-Iglesias, J.; Fernández-De-Las-Peñas, C.; Cleland, J.A.; Gutiérrez-Vega, M.D.R. Thoracic Spine Manipulation for the Management of Patients with Neck Pain: A Randomized Clinical Trial. J. Orthop. Sports Phys. Ther. 2009, 39, 20–27. [Google Scholar] [CrossRef]
- Strunce, J.B.; Walker, M.J.; Boyles, R.E.; Young, B.A. The Immediate Effects of Thoracic Spine and Rib Manipulation on Subjects with Primary Complaints of Shoulder Pain. J. Man. Manip. Ther. 2009, 17, 230–236. [Google Scholar] [CrossRef]
- Mintken, P.E.; Cleland, J.A.; Carpenter, K.J.; Bieniek, M.L.; Keirns, M.; Whitman, J.M. Some Factors Predict Successful Short-Term Outcomes in Individuals with Shoulder Pain Receiving Cervicothoracic Manipulation: A Single-Arm Trial. Phys. Ther. 2010, 90, 26–42. [Google Scholar] [CrossRef]
- Boyles, R.E.; Ritland, B.M.; Miracle, B.M.; Barclay, D.M.; Faul, M.S.; Moore, J.H.; Koppenhaver, S.L.; Wainner, R.S. The Short-Term Effects of Thoracic Spine Thrust Manipulation on Patients with Shoulder Impingement Syndrome. Man. Ther. 2009, 14, 375–380. [Google Scholar] [CrossRef] [PubMed]
- Rowe, J.; Shafer, L.; Kelley, K.; West, N.; Dunning, T.; Smith, R.; Mattson, D.J.; Mack, J.; Schenectady, A.; York, N. Hip Strength and Knee Pain in Females. N. Am. J. Sports Phys. Ther. 2007, 2, 164. [Google Scholar]
- Souza, R.B.; Powers, C.M. Differences in Hip Kinematics, Muscle Strength, and Muscle Activation between Subjects with and without Patellofemoral Pain. J. Orthop. Sports Phys. Ther. 2009, 39, 12–19. [Google Scholar] [CrossRef] [PubMed]
- Finnoff, J.T.; Hall, M.M.; Kyle, K.; Krause, D.A.; Lai, J.; Smith, J. Hip Strength and Knee Pain in High School Runners: A Prospective Study. PMR 2011, 3, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Bolgla, L.A.; Malone, T.R.; Umberger, B.R.; Uhl, T.L. Hip Strength and Hip and Knee Kinematics during Stair Descent in Females with and without Patellofemoral Pain Syndrome. J. Orthop. Sport Phys. Ther. 2008, 38, 12–18. [Google Scholar] [CrossRef]
- Sueki, D.G.; Cleland, J.A.; Wainner, R.S. A Regional Interdependence Model of Musculoskeletal DysFunction: Research, Mechanisms, and Clinical Implications. J. Man. Manip Ther. 2013, 21, 90–102. [Google Scholar] [CrossRef] [PubMed]
- Dolbeer, J.; Mason, J.; Morris, J.; Crowell, M.; Goss, D. Inter-rater reliability of the selective Functional movement (SFMA) by sfma certified physical Therapists with similar clinical and rating experience. Int. J. Sports Phys. Ther. 2017, 12, 752. [Google Scholar] [CrossRef]
- Glaws, K.R.; Juneau, C.M.; Becker, L.C.; Stasi, S.L.d.; Hewett, T.E. Intra- and Inter-rater reliability of the selective Functional movement assessment (SFMA). Int. J. Sports Phys. Ther. 2014, 9, 195. [Google Scholar]
- Goshtigian, G.R.; Swanson, B.T. Using the selective Functional movement assessment and regional Interdependence theory to guide treatment of an athlete with back pain: A case report. Int. J. Sports Phys. Ther. 2016, 11, 575. [Google Scholar]
- Monique Mokha, G.; Sprague, P.A.; Rodriguez, R.; Gatens, D.R. Functional Movement Pattern Training Improves Mechanics in a Female Runner With External Snapping Hip Syndrome. Int. J. Athl. Ther. Train. 2015, 20, 25–33. [Google Scholar] [CrossRef]
- Busch, A.M.; Clifton, D.R.; Onate, J.A.; Ramsey, V.K.; Cromartie, F. Relationship of preseason movement screens with overuse symptoms in collegiate baseball players. Int. J. Sports Phys. Ther. 2017, 12, 960. [Google Scholar] [CrossRef]
- Ionescu, A.M.; Pitsiladis, Y.P.; Rozenstoka, S.; Bigard, X.; Löllgen, H.; Bachl, N.; Debruyne, A.; Pigozzi, F.; Casasco, M.; Jegier, A.; et al. Preparticipation Medical Evaluation for Elite Athletes: EFSMA Recommendations on Standardised Preparticipation Evaluation Form in European Countries. BMJ Open Sport Exerc. Med. 2021, 7, e001178. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Massa, B.; Vecchiato, M.; Mazza, F.; de Blasiis, P.; Romano, A.M.; di Salvatore, M.G.; della Valle, E.; Tarantino, D.; Ruosi, C.; et al. Indirect Structural Muscle Injuries of Lower Limb: Rehabilitation and Therapeutic Exercise. J. Funct. Morphol Kinesiol 2021, 6, 75. [Google Scholar] [CrossRef] [PubMed]
- Palermi, S.; Annarumma, G.; Spinelli, A.; Massa, B.; Serio, A.; Vecchiato, M.; Demeco, A.; Brugin, E.; Sirico, F.; Giada, F.; et al. Acceptability and Practicality of a Quick Musculoskeletal Examination into Sports Medicine Pre-Participation Evaluation. Pediatr. Rep. 2022, 14, 207–216. [Google Scholar] [CrossRef] [PubMed]
- McKinney, J.; Velghe, J.; Fee, J.; Isserow, S.; Drezner, J.A. Defining Athletes and Exercisers. Am. J. Cardiol. 2019, 123, 532–535. [Google Scholar] [CrossRef]
- Brown, P. Movement: Functional Movement Systems—Screening, Assessing, Corrective Strategies on Target Publications. J. Can. Chiropr. Assoc. 2012, 56, 316. [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows, Version 25.0; Released 2017; IBM Corp.: Armonk, NY, USA, 2017. [Google Scholar]
- McHugh, M.L. Interrater Reliability: The Kappa Statistic. Biochem Med. 2012, 22, 276. [Google Scholar] [CrossRef]
- Sim, J.; Wright, C.C. The Kappa Statistic in Reliability Studies: Use, Interpretation, and Sample Size Requirements. Phys. Ther. 2005, 85, 257–268. [Google Scholar] [CrossRef]
- Bujang, M.A.; Baharum, N. Guidelines of the Minimum Sample Size Requirements for Cohen’s Kappa. Epidemiol. Biostat. Public Health 2017, 14, e12267-1–e12267-10. [Google Scholar] [CrossRef]
- Landis, J.R.; Koch, G.G. The Measurement of Observer Agreement for Categorical Data. Biometrics 1977, 33, 159. [Google Scholar] [CrossRef] [PubMed]
- Hux, M. The Value and Effectiveness of the Selective Functional Movement Assessment (SFMA): A Literature Review. Honors Projects 2019. Available online: https://digitalcommons.bridgewater.edu/honors_projects/2 (accessed on 17 November 2022).
- Bannigan, K.; Watson, R. Reliability and Validity in a Nutshell. J. Clin. Nurs. 2009, 18, 3237–3243. [Google Scholar] [CrossRef] [PubMed]
- Riebel, M.; Crowell, M.; Dolbeer, J.; Szymanek, E.; Goss, D. Correlation of self-reported outcome measures and the selective Functional movement assessment (SFMA): An exploration of validity. Int. J. Sports Phys. Ther. 2017, 12, 931–947. [Google Scholar] [CrossRef]
- Huang, L.; Liu, H.; Zhao, L.; Peng, L. The Effect of Exercise Intervention Based Upon the Selective Functional Movement Assessment in an Athlete With Non-Specific Low Back Pain: A Case Report and Pilot Study. Front. Psychol. 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Lamberti, V.; Palermi, S.; Franceschin, A.; Scapol, G.; Lamberti, V.; Lamberti, C.; Vecchiato, M.; Spera, R.; Sirico, F.; Della Valle, E. The Effectiveness of Adapted Personalized Motor Activity (AMPA) to Improve Health in Individuals with Mental Disorders and Physical Comorbidities: A Randomized Controlled Trial. Sports 2022, 10, 30. [Google Scholar] [CrossRef]
- Vecchiato, M.; Quinto, G.; Palermi, S.; Foccardi, G.; Mazzucato, B.; Battista, F.; Duregon, F.; Michieletto, F.; Neunhaeuserer, D.; Ermolao, A. Are Gyms a Feasible Setting for Exercise Training Interventions in Patients with Cardiovascular Risk Factors? An Italian 10-Years Cross-Sectional Survey Comparison. Int. J. Environ. Res. Public Health 2022, 19. [Google Scholar] [CrossRef] [PubMed]
- Matsel, K.A.; Brown, S.N.; Hoch, M.C.; Butler, R.J.; Westgate, P.M.; Malone, T.R.; Uhl, T.L. The Intra- and Inter-Rater Reliability of an Arm Care Screening Tool in High School Baseball Coaches. Int. J. Sports Phys. Ther. 2021, 16, 1532–1540. [Google Scholar] [CrossRef] [PubMed]
- Krzyzanowicz, R.; Baker, R.; Nasypany, A.; Gargano, F.; Seegmiller, J. Patient Outcomes Utilizing the Selective Functional Movement Assessment and Mulligan Mobilizations With Movement on Recreational Dancers With Sacroiliac Joint. Pain: A Case Series. Int. J. Athl. Ther. Train. 2015, 20, 31–37. [Google Scholar] [CrossRef]
| Variable | |
|---|---|
| Age (years)—mean, SD | 17.71 ± 1.96 |
| Male, n (%) | 25 (89.3%) |
| Sports activity—n (%) | Athletics—6 (21.4%) Soccer—14 (50%) Volleyball—5 (17.9%) Fencing—3 (10.7%) |
| Years of practice—mean, SD | 9.82 ± 2.37 |
| Intra-Rater B | Intra-Rater C’ | |||
|---|---|---|---|---|
| Intra-Rater Comparison: Rater B and Rater C (Glaws and Colleagues) | Kappa | % Agreement | Kappa | % Agreement |
| C Flex | 0.654 (0.380–0.928) | 0.821 | 0.440 | 0.890 |
| C Ext | 0.517 (0.198–0.836) | 0.821 | 0.800 | 0.940 |
| C Rot R | 0.633 (0.355–0.911) | 0.821 | 0.600 | 0.890 |
| C Rot L | 0.426 (0.140–0.712) | 0.714 | 0.530 | 0.860 |
| UE pattern 1 Right | 0.397 (0.074–0.720) | 0.643 | 0.660 | 0.830 |
| UE pattern 1 Left | 0.397 (0.027–0.767) | 0.750 | 0.610 | 0.830 |
| UE pattern 2 Right | 0.164 (−0.275–0.603) | 0.786 | 0.600 | 0.890 |
| UE pattern 2 Left | 0.294 (−0.106–0.694) | 0.786 | 0.410 | 0.830 |
| MSF | 0.877 (0.710–1.044) | 0.926 | 0.720 | 0.860 |
| MSE | 0.744 (0.530–0.958) | 0.852 | 0.250 | 0.630 |
| MSR Right | 0.584 (0.214–0.954) | 0.893 | 0.770 | 0.890 |
| MSR Left | 0.462 (0.176–0.748) | 0.750 | 0.620 | 0.830 |
| SLS 1 Right | 0.481 (−0.111–1.073) | 0.929 | 0.760 | 0.890 |
| SLS 1 Left | / | 0.830 | 0.910 | |
| SLS 2 Right | 0.22 (−0.005–0.445) | 0.607 | / | |
| SLS 2 Left | 0.5 (0.122–0.878) | 0.821 | / | |
| OHDS | 0.541 (0.306–0.776) | 0.714 | 0.720 | 0.910 |
| Mean | 0.493 | 0.790 | 0.621 | 0.859 |
| SD | 0.185 | 0.092 | 0.161 | 0.072 |
| Inter-Rater Reliability Rater B | Rater A vs. B1 | Rater A vs. B2 | Inter-Rater A’ vs. C’ | |||
|---|---|---|---|---|---|---|
| Kappa | % Agreement | Kappa | % Agreement | Kappa | % Agreement | |
| C Flex | 0.852 (0.652–1.052) | 0.929 | 0.793 (0.573–1.013) | 0.893 | 0.30 | 0.74 |
| C Ext | 0.687 (0.362–1.012) | 0.893 | 0.663 (0.379–0.947) | 0.857 | 0.62 | 0.86 |
| C Rot R | 0.478 (0.149–0.807) | 0.786 | 0.494 (0.204–0.784) | 0.75 | 0.30 | 0.83 |
| C Rot L | 0.472 (0.174–0.770) | 0.75 | 0.796 (0.575–1.017) | 0.893 | 0.32 | 0.74 |
| UE pattern 1 Right | 0.588 (0.321–0.855) | 0.75 | 0.462 (0.168–0.756) | 0.679 | 0.19 | 0.60 |
| UE pattern 1 Left | 0.218 (−0.168–0.604) | 0.643 | 0.569 (0.236–0.902) | 0.821 | 0.28 | 0.63 |
| UE pattern 2 Right | 0.531 (0.066–0.996) | 0.893 | 0.525 (0.051–0.999) | 0.893 | 0.53 | 0.86 |
| UE pattern 2 Left | 0.611 (0.229–0.993) | 0.893 | 0.3 (−0.104–0.704) | 0.75 | 0.58 | 0.86 |
| MSF | 0.813 (0.607–1.019) | 0.889 | 0.816 (0.618–1.014) | 0.889 | 0.44 | 0.71 |
| MSE | 0.681 (0.430–0.932) | 0.815 | 0.806 (0.604–1.008) | 0.889 | 0.27 | 0.66 |
| MSR Right | 0.517 (0.198–0.836) | 0.821 | 0.614 (0.281–0.947) | 0.857 | 0.33 | 0.66 |
| MSR Left | 0.376 (0.111–0.641) | 0.679 | 0.737 (0.494–0.980) | 0.857 | 0.34 | 0.77 |
| SLS 1 Right | 0.786 (0.382–1.190) | 0.964 | 0.654 (0.033–1.275) | 0.964 | 0.61 | 0.80 |
| SLS 1 Left | 1 | 1 | / | 0.60 | 0.80 | |
| SLS 2 Right | 0.528 (0.220–0.836) | 0.75 | 0.319 (0.027–0.611) | 0.714 | / | |
| SLS 2 Left | 0.7 (0.384–1.016) | 0.893 | 0.576 (0.204–0.948) | 0.857 | / | |
| OHDS | 0.309 (0.070–0.548) | 0.536 | 0.726 (0.501–0.951) | 0.821 | 0.18 | 0.83 |
| Mean | 0.5969 | 0.8167 | 0.6156 | 0.8365 | 0.39 | 0.76 |
| SD | 0.20 | 0.122 | 0.17 | 0.077 | 0.156 | 0.088 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aghi, A.; Salvagnini, D.; Berton, G.; Cecconi, M.; Della Valle, E.; Spera, R.; Mambelli, M.; Palermi, S.; Neunhaeuserer, D.; Vecchiato, M. Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports. Int. J. Environ. Res. Public Health 2023, 20, 2032. https://doi.org/10.3390/ijerph20032032
Aghi A, Salvagnini D, Berton G, Cecconi M, Della Valle E, Spera R, Mambelli M, Palermi S, Neunhaeuserer D, Vecchiato M. Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports. International Journal of Environmental Research and Public Health. 2023; 20(3):2032. https://doi.org/10.3390/ijerph20032032
Chicago/Turabian StyleAghi, Andrea, Daniele Salvagnini, Giovanni Berton, Mattia Cecconi, Elisabetta Della Valle, Rocco Spera, Maria Mambelli, Stefano Palermi, Daniel Neunhaeuserer, and Marco Vecchiato. 2023. "Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports" International Journal of Environmental Research and Public Health 20, no. 3: 2032. https://doi.org/10.3390/ijerph20032032
APA StyleAghi, A., Salvagnini, D., Berton, G., Cecconi, M., Della Valle, E., Spera, R., Mambelli, M., Palermi, S., Neunhaeuserer, D., & Vecchiato, M. (2023). Selective Functional Movement Assessment (SFMA) Reliability and Proposal of Its Use in Sports. International Journal of Environmental Research and Public Health, 20(3), 2032. https://doi.org/10.3390/ijerph20032032







