The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China
Abstract
1. Introduction
2. Methods
2.1. Study Area and Data Collection
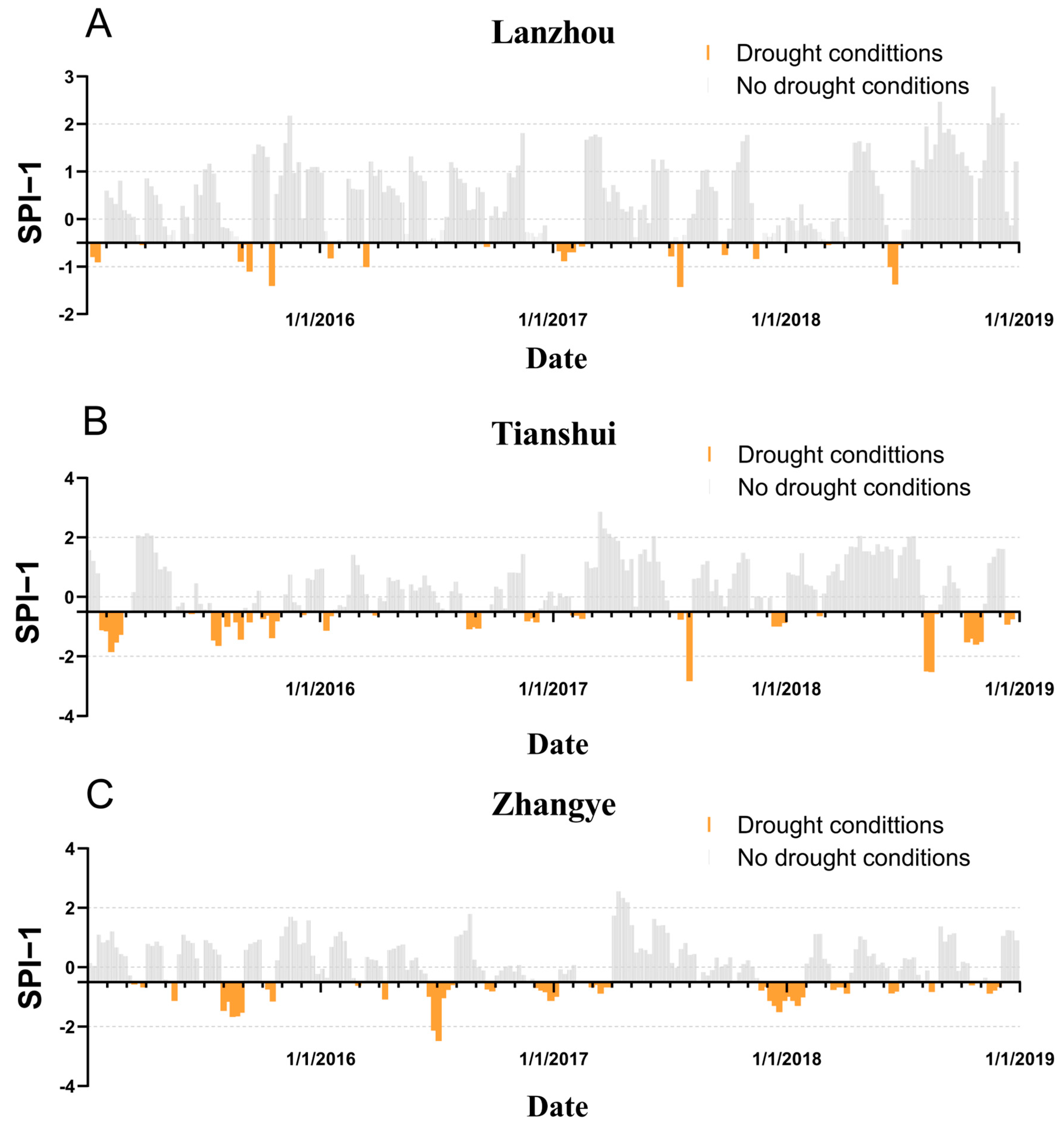
2.2. Drought Index
2.3. Statistical Analysis
2.3.1. GAM Model
2.3.2. DLNM Model
2.3.3. Interaction Effect
3. Results
3.1. Descriptive Statistics
3.2. Correlation Analysis
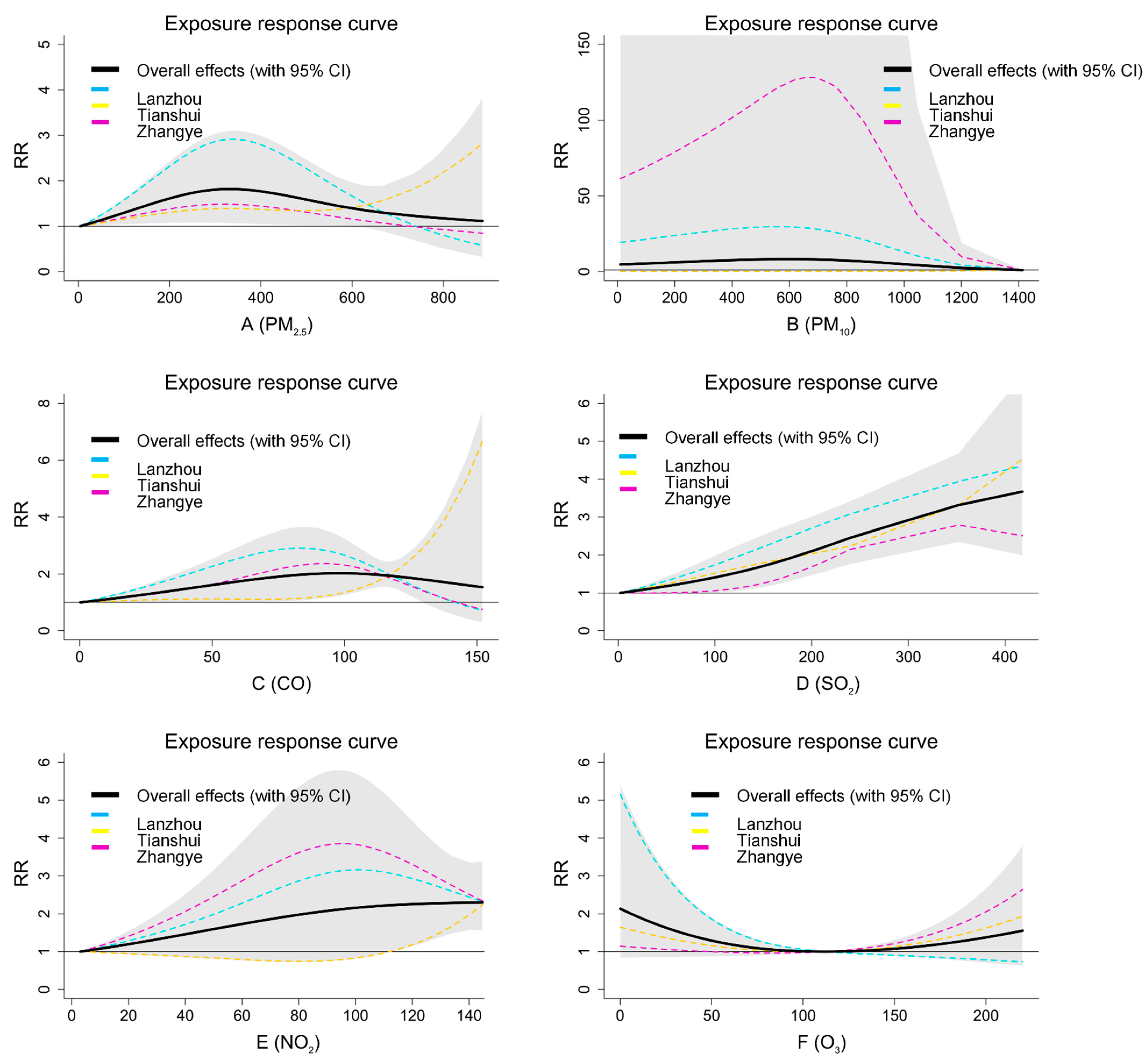
3.3. Individual Effects
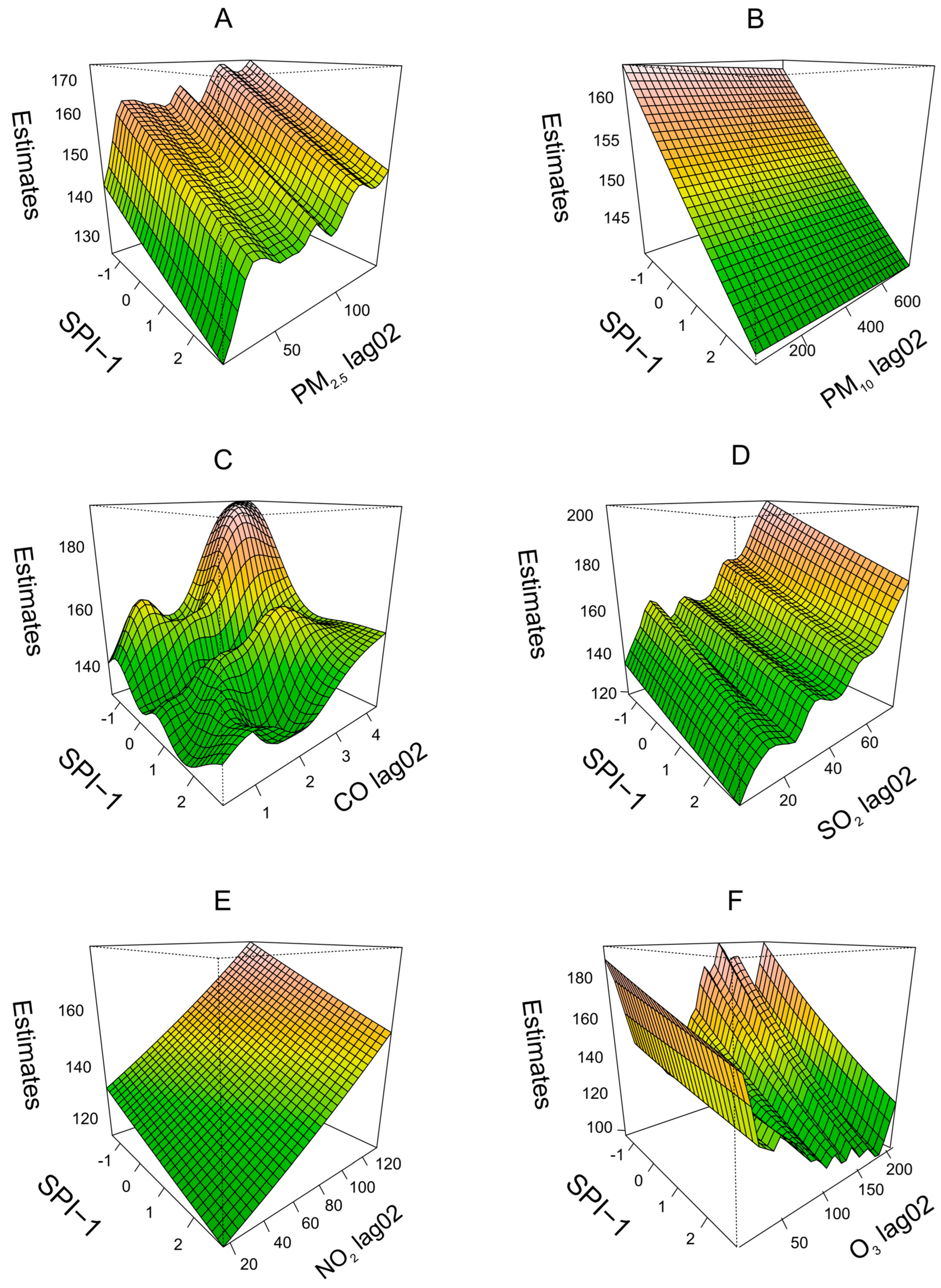
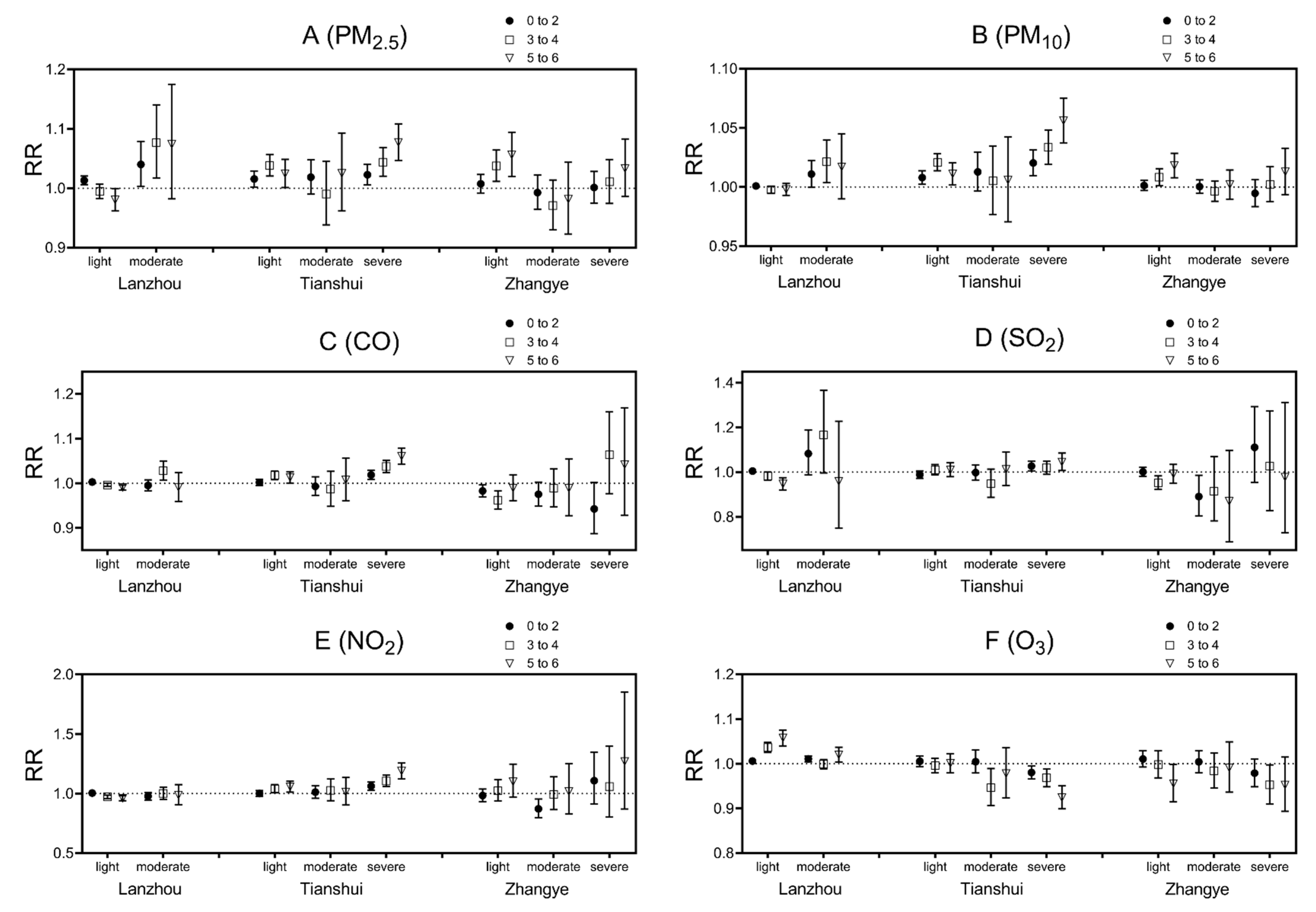
3.4. Interactive Effects
3.5. Subgroup Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Barkin, J.L.; Buoli, M.; Curry, C.L.; Esenwein, S.A.; Upadhyay, S.; Kearney, M.B.; Mach, K. Effects of extreme weather events on child mood and behavior. Dev. Med. Child Neurol. 2021, 63, 785–790. [Google Scholar] [CrossRef] [PubMed]
- Ebi, K.L.; Vanos, J.; Baldwin, J.W.; Bell, J.E.; Hondula, D.M.; Errett, N.A.; Hayes, K.; Reid, C.E.; Saha, S.; Spector, J.; et al. Extreme Weather and Climate Change: Population Health and Health System Implications. Annu. Rev. Public Health 2021, 42, 293–315. [Google Scholar] [CrossRef]
- Palinkas, L.A.; Wong, M. Global climate change and mental health. Curr. Opin. Psychol. 2020, 32, 12–16. [Google Scholar] [CrossRef]
- Weilnhammer, V.; Schmid, J.; Mittermeier, I.; Schreiber, F.; Jiang, L.; Pastuhovic, V.; Herr, C.; Heinze, S. Extreme weather events in europe and their health consequences—A systematic review. Int. J. Hyg. Environ. Health 2021, 233, 113688. [Google Scholar] [CrossRef] [PubMed]
- Mahapatra, B.; Walia, M.; Saggurti, N. Extreme weather events induced deaths in India 2001–2014: Trends and differentials by region, sex and age group. Weather Clim. Extrem. 2018, 21, 110–116. [Google Scholar] [CrossRef]
- Strazdins, L.; Skeat, H. Weathering the Future: Climate Change, Children and Young People, and Decision Making; Australian Research Alliance for Children and Youth Canberra: Canberra, Australia, 2011. [Google Scholar]
- Uddin, R.; Philipsborn, R.; Smith, D.; Mutic, A.; Thompson, L.M. A global child health perspective on climate change, migration and human rights. Curr. Probl. Pediatr. Adolesc. Health Care 2021, 51, 101029. [Google Scholar] [CrossRef] [PubMed]
- Shankar, H.M.; Rice, M.B. Update on Climate Change: Its Impact on Respiratory Health at Work, Home, and at Play. Clin. Chest Med. 2020, 41, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Barnes, C.S. Impact of Climate Change on Pollen and Respiratory Disease. Curr. Allergy Asthma Rep. 2018, 18, 59. [Google Scholar] [CrossRef]
- Wright, R.J. Influences of climate change on childhood asthma and allergy risk. Lancet Child Adolesc. Health 2020, 4, 859–860. [Google Scholar] [CrossRef]
- Urrutia-Pereira, M.; Badellino, H.; Ansotegui, I.J.; Guidos, G.; Solé, D. Climate change and allergic diseases in children and adolescents. Allergol. Immunopathol. 2022, 50 Pt 1, 7–16. [Google Scholar] [CrossRef]
- McMichael, A.J. Climate Change and Children: Health Risks of Abatement Inaction, Health Gains from Action. Children 2014, 1, 99–106. [Google Scholar] [CrossRef]
- Salvador, C.; Nieto, R.; Linares, C.; Díaz, J.; Gimeno, L. Effects of droughts on health: Diagnosis, repercussion, and adaptation in vulnerable regions under climate change. Challenges for future research. Sci. Total Environ. 2020, 703, 134912. [Google Scholar] [CrossRef] [PubMed]
- Romanello, M.; McGushin, A.; Di Napoli, C.; Drummond, P.; Hughes, N.; Jamart, L.; Kennard, H.; Lampard, P.; Rodriguez, B.S.; Arnell, N.; et al. The 2021 report of the Lancet Countdown on health and climate change: Code red for a healthy future. Lancet 2021, 398, 1619–1662. [Google Scholar] [CrossRef] [PubMed]
- Stanke, C.; Kerac, M.; Prudhomme, C.; Medlock, J.; Murray, V. Health effects of drought: A systematic review of the evidence. PLoS Curr. 2013, 5. [Google Scholar] [CrossRef]
- Costello, A.; Abbas, M.; Allen, A.; Ball, S.; Bell, S.; Bellamy, R.; Friel, S.; Groce, N.; Johnson, A.; Kett, M.; et al. Managing the health effects of climate change: Lancet and University College London Institute for Global Health Commission. Lancet 2009, 373, 1693–1733. [Google Scholar] [CrossRef] [PubMed]
- Hashizume, M.; Kim, Y.; Ng, C.F.S.; Chung, Y.; Madaniyazi, L.; Bell, M.L.; Guo, Y.L.; Kan, H.; Honda, Y.; Yi, S.-M.; et al. Health Effects of Asian Dust: A Systematic Review and Meta-Analysis. Environ. Health Perspect. 2020, 128, 66001. [Google Scholar] [CrossRef]
- Zhong, R.; Chen, X.; Lai, C.; Wang, Z.; Lian, Y.; Yu, H.; Wu, X. Drought monitoring utility of satellite-based precipitation products across mainland China. J. Hydrol. 2019, 568, 343–359. [Google Scholar] [CrossRef]
- Ichinose, T.; Yoshida, S.; Hiyoshi, K.; Sadakane, K.; Takano, H.; Nishikawa, M.; Mori, I.; Yanagisawa, R.; Kawazato, H.; Yasuda, A.; et al. The effects of microbial materials adhered to Asian sand dust on allergic lung inflammation. Arch. Environ. Contam. Toxicol. 2008, 55, 348–357. [Google Scholar] [CrossRef]
- Koffi, B.; Schulz, M.; Bréon, F.-M.; Dentener, F.; Steensen, B.M.; Griesfeller, J.; Winker, D.; Balkanski, Y.; Bauer, S.E.; Bellouin, N.; et al. Evaluation of the aerosol vertical distribution in global aerosol models through comparison against CALIOP measurements: AeroCom phase II results. J. Geophys. Res. Atmos. 2016, 121, 7254–7283. [Google Scholar] [CrossRef]
- Manisalidis, I.; Stavropoulou, E.; Stavropoulos, A.; Bezirtzoglou, E. Environmental and Health Impacts of Air Pollution: A Review. Front. Public Health 2020, 8, 14. [Google Scholar] [CrossRef]
- Smith, L.T.; Aragão, L.E.O.C.; Sabel, C.E.; Nakaya, T. Drought impacts on children’s respiratory health in the Brazilian Amazon. Sci. Rep. 2014, 4, 3726. [Google Scholar] [CrossRef] [PubMed]
- Yusa, A.; Berry, P.; Cheng, J.J.; Ogden, N.; Bonsal, B.; Stewart, R.; Waldick, R. Climate Change, Drought and Human Health in Canada. Int. J. Environ. Res. Public Health 2015, 12, 8359–8412. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Wang, S.; Li, L.; Xu, S.; Li, C.; Li, S.; Wang, J.; He, H.; Niu, J.; Zhang, K.; et al. The association between drought and outpatient visits for respiratory diseases in four northwest cities of China. Clim. Chang. 2021, 167, 2. [Google Scholar] [CrossRef]
- Berman, J.D.; Ebisu, K.; Peng, R.D.; Dominici, F.; Bell, M.L. Drought and the risk of hospital admissions and mortality in older adults in western USA from 2000 to 2013: A retrospective study. Lancet Planet Health 2017, 1, e17–e25. [Google Scholar] [CrossRef]
- Orru, H.; Ebi, K.; Forsberg, B. The Interplay of Climate Change and Air Pollution on Health. Curr. Environ. Health Rep. 2017, 4, 504–513. [Google Scholar] [CrossRef]
- Bernard, S.M.; Samet, J.M.; Grambsch, A.; Ebi, K.L.; Romieu, I. The potential impacts of climate variability and change on air pollution-related health effects in the United States. Environ. Health Perspect. 2001, 109 (Suppl. 2), 199–209. [Google Scholar] [CrossRef]
- Gu, J.; Shi, Y.; Zhu, Y.; Chen, N.; Wang, H.; Zhang, Z.; Chen, T. Ambient air pollution and cause-specific risk of hospital admission in China: A nationwide time-series study. PLoS Med. 2020, 17, e1003188. [Google Scholar] [CrossRef]
- Wu, Z.Q.; Miao, C.; Li, H.; Wu, S.; Gao, H.; Liu, W.; Li, W.; Xu, L.; Liu, G.; Zhu, Y. The lag-effects of meteorological factors and air pollutants on child respiratory diseases in Fuzhou, China. J. Glob. Health 2022, 12, 11010. [Google Scholar] [CrossRef]
- Yang, H.; Yan, C.; Li, M.; Zhao, L.; Long, Z.; Fan, Y.; Zhang, Z.; Chen, R.; Huang, Y.; Lu, C.; et al. Short term effects of air pollutants on hospital admissions for respiratory diseases among children: A multi-city time-series study in China. Int. J. Hyg. Environ. Health 2021, 231, 113638. [Google Scholar] [CrossRef]
- Mirsaeidi, M.; Motahari, H.; Khamesi, M.T.; Sharifi, A.; Campos, M.; Schraufnagel, D.E. Climate Change and Respiratory Infections. Ann. Am. Thorac. Soc. 2016, 13, 1223–1230. [Google Scholar] [CrossRef]
- Jain, N.; Lodha, R.; Kabra, S.K. Upper respiratory tract infections. Indian J. Pediatr. 2001, 68, 1135–1138. [Google Scholar] [CrossRef] [PubMed]
- Zeru, T.; Berihu, H.; Buruh, G.; Gebrehiwot, H. Magnitude and factors associated with upper respiratory tract infection among under-five children in public health institutions of Aksum town, Tigray, Northern Ethiopia: An institutional based cross-sectional study. PAMJ 2020, 36, 307. [Google Scholar] [CrossRef] [PubMed]
- de Benedictis, F.M.; Bush, A. Recurrent lower respiratory tract infections in children. BMJ 2018, 362, k2698. [Google Scholar] [CrossRef] [PubMed]
- Fang, F.; Ma, L.; Fan, H.; Che, X.; Chen, M. The spatial differentiation of quality of rural life based on natural controlling factors: A case study of Gansu Province, China. J. Environ. Manag. 2020, 264, 110439. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.R.; Xiao, C.; Li, J.; Tang, J.; Geng, X.; Cui, L.; Zhai, J. Association between air pollution and upper respiratory tract infection in hospital outpatients aged 0–14 years in Hefei, China: A time series study. Public Health 2018, 156, 92–100. [Google Scholar] [CrossRef] [PubMed]
- Amani, M.; Salehi, B.; Mahdavi, S.; Masjedi, A.; Dehnavi, S. Temperature-Vegetation-soil Moisture Dryness Index (TVMDI). Remote Sens. Environ. 2017, 197, 1–14. [Google Scholar] [CrossRef]
- Wei, W.; Zhang, H.; Zhou, J.; Zhou, L.; Xie, B.; Li, C. Drought monitoring in arid and semi-arid region based on multi-satellite datasets in northwest, China. Environ. Sci. Pollut. Res. 2021, 28, 51556–51574. [Google Scholar] [CrossRef]
- Ratajczak, A.; Badyda, A.; Czechowski, P.; Czarnecki, A.; Dubrawski, M.; Feleszko, W. Air Pollution Increases the Incidence of Upper Respiratory Tract Symptoms among Polish Children. J. Clin. Med. 2021, 10, 2150. [Google Scholar] [CrossRef]
- Ziou, M.; Tham, R.; Wheeler, A.J.; Zosky, G.R.; Stephens, N.; Johnston, F.H. Outdoor particulate matter exposure and upper respiratory tract infections in children and adolescents: A systematic review and meta-analysis. Environ. Res. 2022, 210, 112969. [Google Scholar] [CrossRef]
- Gestro, M.; Condemi, V.; Bardi, L.; Fantino, C.; Solimene, U. Meteorological factors, air pollutants, and emergency department visits for otitis media: A time series study. Int. J. Biometeorol. 2017, 61, 1749–1764. [Google Scholar] [CrossRef]
- Kim, K.-H.; Kabir, E.; Kabir, S. A review on the human health impact of airborne particulate matter. Environ. Int. 2015, 74, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Glencross, D.A.; Ho, T.-R.; Camiña, N.; Hawrylowicz, C.M.; Pfeffer, P.E. Air pollution and its effects on the immune system. Free Radic. Biol. Med. 2020, 151, 56–68. [Google Scholar] [CrossRef]
- Arias-Pérez, R.D.; Taborda, N.A.; Gómez, D.M.; Narvaez, J.F.; Porras, J.; Hernandez, J.C. Inflammatory effects of particulate matter air pollution. Environ. Sci. Pollut. Res. 2020, 27, 42390–42404. [Google Scholar] [CrossRef] [PubMed]
- Kampa, M.; Castanas, E. Human health effects of air pollution. Environ. Pollut. 2008, 151, 362–367. [Google Scholar] [CrossRef] [PubMed]
- Salvador, C.; Nieto, R.; Linares, C.; Díaz, J.; Alves, C.; Gimeno, L. Drought effects on specific-cause mortality in Lisbon from 1983 to 2016: Risks assessment by gender and age groups. Sci. Total Environ. 2021, 751, 142332. [Google Scholar] [CrossRef] [PubMed]
- Salvador, C.; Vicedo-Cabrera, A.M.; Libonati, R.; Russo, A.; Garcia, B.N.; Belem, L.B.C.; Gimeno, L.; Nieto, R. Effects of Drought on Mortality in Macro Urban Areas of Brazil between 2000 and 2019. Geohealth 2022, 6, e2021GH000534. [Google Scholar] [CrossRef]
- Salvador, C.; Nieto, R.; Linares, C.; Díaz, J.; Gimeno, L. Short-term effects of drought on daily mortality in Spain from 2000 to 2009. Environ. Res. 2020, 183, 109200. [Google Scholar] [CrossRef]
- Trenberth, K.E.; Dai, A.; Van Der Schrier, G.; Jones, P.D.; Barichivich, J.; Briffa, K.R.; Sheffield, J. Global warming and changes in drought. Nat. Clim. Chang. 2014, 4, 17–22. [Google Scholar] [CrossRef]
- Wolkoff, P. Indoor air humidity, air quality, and health—An overview. Int. J. Hyg. Environ. Health 2018, 221, 376–390. [Google Scholar] [CrossRef]
- Moriyama, M.; Hugentobler, W.J.; Iwasaki, A. Seasonality of Respiratory Viral Infections. Annu. Rev. Virol. 2020, 7, 83–101. [Google Scholar] [CrossRef]
- Guenther, A.B.; Jiang, X.; Heald, C.L.; Sakulyanontvittaya, T.; Duhl, T.; Emmons, L.K.; Wang, X. The Model of Emissions of Gases and Aerosols from Nature version 2.1 (MEGAN2. 1): An extended and updated framework for modeling biogenic emissions. Geosci. Model Dev. 2012, 5, 1471–1492. [Google Scholar] [CrossRef]
- Fussell, J.C.; Kelly, F. Mechanisms underlying the health effects of desert sand dust. Environ. Int. 2021, 157, 106790. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Xie, Y.; Cai, L.; Dong, W.; Zhang, Q.; Zhang, L. Impact of the 2011 Southern US drought on ground-level fine aerosol concentration in summertime. J. Atmos. Sci. 2015, 72, 1075–1093. [Google Scholar] [CrossRef]
- Hu, Y.; Wang, S.; Yang, X.; Kang, Y.; Ning, G.; Du, H. Impact of winter droughts on air pollution over Southwest China. Sci. Total Environ. 2019, 664, 724–736. [Google Scholar] [CrossRef]
- Ault, T.R. On the essentials of drought in a changing climate. Science 2020, 368, 256–260. [Google Scholar] [CrossRef] [PubMed]
- Koebsch, F.; Gottschalk, P.; Beyer, F.; Wille, C.; Jurasinski, G.; Sachs, T. The impact of occasional drought periods on vegetation spread and greenhouse gas exchange in rewetted fens. Philos. Trans. R. Soc. B Biol. Sci. 2020, 375, 20190685. [Google Scholar] [CrossRef]
- Zhang, S.; Chen, X.; Dai, C.; Wang, J.; Wang, H. Associations between air pollutants and risk of respiratory infection: Patient-based bacterial culture in sputum. Environ. Geochem. Health 2022, 44, 4007–4016. [Google Scholar] [CrossRef]
- Zhang, H.; Yan, L.; Chen, X.; Zhang, C. The association between short-term exposure to air pollutants and rotavirus infection in Wuhan, China. J. Med. Virol. 2021, 93, 4831–4839. [Google Scholar] [CrossRef]
- Naclerio, R.M.; Pinto, J.; Assanasen, P.; Baroody, F.M. Observations on the ability of the nose to warm and humidify inspired air. Rhinology 2007, 45, 102. [Google Scholar]
- Keck, T.; Leiacker, R.; Heinrich, A.; Kühnemann, S.; Rettinger, G. Humidity and temperature profile in the nasal cavity. Rhinology 2000, 38, 167–171. [Google Scholar]
- Murgia, V.; Manti, S.; Licari, A.; De Filippo, M.; Ciprandi, G.; Marseglia, G.L. Upper respiratory tract infection-associated acute cough and the urge to cough: New insights for clinical practice. Pediatr. Allergy Immunol. Pulmonol. 2020, 33, 3–11. [Google Scholar] [CrossRef] [PubMed]
- Clark, S.E. Commensal bacteria in the upper respiratory tract regulate susceptibility to infection. Curr. Opin. Immunol. 2020, 66, 42–49. [Google Scholar] [CrossRef] [PubMed]
- Ciencewicki, J.; Jaspers, I. Air Pollution and Respiratory Viral Infection. Inhal. Toxicol. 2007, 19, 1135–1146. [Google Scholar] [CrossRef] [PubMed]

| Variable | City | Mean ± SD | Min | P25 | P50 | P75 | Max | |
|---|---|---|---|---|---|---|---|---|
| Outpatient | Visits | Lanzhou | 125.3 ± 51.7 | 27 | 93 | 117 | 149 | 406 |
| Tianshui | 35.9 ± 16.5 | 5 | 24 | 34 | 44 | 130 | ||
| Zhangye | 26.9 ± 11.9 | 0 | 19 | 26 | 34 | 107 | ||
| Age | 0–2 | Lanzhou | 83.6 ± 33.0 | 16 | 62 | 81 | 102 | 243 |
| Tianshui | 19.3 ± 8.1 | 2 | 13 | 18 | 24 | 56 | ||
| Zhangye | 16.4 ± 7.3 | 0 | 11 | 16 | 21 | 50 | ||
| 3–4 | Lanzhou | 30.1 ± 17.4 | 1 | 18 | 28 | 37 | 129 | |
| Tianshui | 10.7 ± 6.6 | 0 | 6 | 10 | 14 | 51 | ||
| Zhangye | 6.2 ± 4.3 | 0 | 3 | 5 | 9 | 28 | ||
| 5–6 | Lanzhou | 11.6 ± 8.5 | 0 | 6 | 10 | 14 | 67 | |
| Tianshui | 5.8 ± 4.7 | 0 | 3 | 5 | 7 | 42 | ||
| Zhangye | 3.0 ± 2.7 | 0 | 1 | 2 | 4 | 32 | ||
| Meteorology | Mean temperature (°C) | Lanzhou | 11.5 ± 10.0 | −12.4 | 2.3 | 12.7 | 19.9 | 30.4 |
| Tianshui | 12.5 ± 9.3 | −10.2 | 4.1 | 13.5 | 20.5 | 30.4 | ||
| Zhangye | 8.8 ± 12.1 | −22.4 | −1.7 | 10.3 | 19.5 | 30.8 | ||
| Mean relative humidity (%) | Lanzhou | 50.5 ± 15.0 | 16 | 39 | 50 | 61.5 | 94 | |
| Tianshui | 64.9 ± 12.4 | 21 | 56 | 65 | 74 | 97 | ||
| Zhangye | 46.4 ± 16.4 | 11 | 35 | 45 | 57 | 100 | ||
| Variables | City | Mean ± SD | Min | P25 | P50 | P75 | Max |
|---|---|---|---|---|---|---|---|
| PM2.5 (μg/m3) | Lanzhou | 47.6 ± 24.6 | 6.5 | 30.9 | 41.0 | 57.0 | 205.7 |
| Tianshui | 41.0 ± 28.2 | 4.0 | 22.0 | 32.0 | 52.0 | 200.0 | |
| Zhangye | 36.3 ± 28.3 | 3.0 | 19.0 | 30.0 | 46.0 | 418.0 | |
| PM10 (μg/m3) | Lanzhou | 122.0 ± 94.2 | 21.1 | 73.5 | 103.0 | 141.9 | 1413.8 |
| Tianshui | 83.7 ± 56.3 | 10.0 | 45.0 | 66.0 | 108.0 | 684.0 | |
| Zhangye | 90.9 ± 92.3 | 6.0 | 42.0 | 67.0 | 104.0 | 886.0 | |
| CO (mg/m3) | Lanzhou | 1.3 ± 0.7 | 0.2 | 0.8 | 1.0 | 1.5 | 5.0 |
| Tianshui | 0.9 ± 0.5 | 0.2 | 0.5 | 0.7 | 1.1 | 3.8 | |
| Zhangye | 0.6 ± 0.4 | 0.1 | 0.4 | 0.5 | 0.8 | 4.6 | |
| SO2 (μg/m3) | Lanzhou | 20.5 ± 15.2 | 3.2 | 9.3 | 15.0 | 28.0 | 87.8 |
| Tianshui | 24.8 ± 23.6 | 2.0 | 9.0 | 12.0 | 36.0 | 176.0 | |
| Zhangye | 23.2 ± 27.6 | 2.0 | 8.0 | 14.0 | 20.0 | 152.0 | |
| NO2 (μg/m3) | Lanzhou | 54.4 ± 21.9 | 11.0 | 38.4 | 51.8 | 66.0 | 144.8 |
| Tianshui | 35.6 ± 15.6 | 7.0 | 24.0 | 32.0 | 46.0 | 100.0 | |
| Zhangye | 21.0 ± 8.8 | 3.0 | 14.0 | 20.0 | 26.0 | 52.0 | |
| O3 (μg/m3) | Lanzhou | 62.9 ± 38.9 | 0.7 | 36.4 | 58.6 | 80.4 | 220.0 |
| Tianshui | 90.6 ± 34.3 | 4.0 | 65.0 | 91.0 | 116.0 | 210.0 | |
| Zhangye | 105.6 ± 27.6 | 38.0 | 85.0 | 105.0 | 124.0 | 229.0 |
| Air Pollutants | City | Drought Condition | ||
|---|---|---|---|---|
| Light Drought | Moderate Drought | Severe Drought | ||
| PM2.5 | Lanzhou | 1.006 (1.012, 1.000) * | 1.066 (1.036, 1.098) *** | |
| Tianshui | 1.024 (1.014, 1.034) *** | 1.019 (0.996, 1.043) | 1.042 (1.029, 1.054) *** | |
| Zhangye | 1.017 (1.005, 1.030) ** | 0.995 (0.974, 1.017) | 1.014 (0.995, 1.033) | |
| PM10 | Lanzhou | 1.000 (0.998, 1.001) | 1.018 (1.009, 1.027) *** | |
| Tianshui | 1.013 (1.009, 1.017) *** | 1.012 (0.998, 1.025) | 1.033 (1.025, 1.041) *** | |
| Zhangye | 1.004 (1.001, 1.008) * | 1.002 (0.997, 1.006) | 1.001 (0.994, 1.009) | |
| CO | Lanzhou | 1.000 (0.998, 1.002) | 1.005 (0.995, 1.015) | |
| Tianshui | 1.008 (1.003, 1.014) ** | 0.997 (0.980, 1.014) | 1.034 (1.026, 1.041) *** | |
| Zhangye | 0.979 (0.969, 1.032) | 0.979 (0.959, 1.000) | 1.001 (0.958, 1.047) | |
| SO2 | Lanzhou | 0.993 (0.984, 1.002) | 1.114 (1.033, 1.201) ** | |
| Tianshui | 0.999 (0.986, 1.011) | 0.995 (0.968, 1.023) | 1.031 (1.015, 1.046) *** | |
| Zhangye | 0.987 (0.972, 1.002) | 0.884 (0.818, 0.956) ** | 1.036 (0.926, 1.159) | |
| NO2 | Lanzhou | 0.991 (0.985, 0.998) * | 0.986 (0.960, 1.012) | |
| Tianshui | 1.021 (1.003, 1.039) * | 1.014 (0.973, 1.057) | 1.103 (1.078, 1.129) *** | |
| Zhangye | 1.114 (0.965, 1.286) | 0.917 (0.856, 0.983) * | 1.114 (0.965, 1.286) | |
| O3 | Lanzhou | 1.018 (1.013, 1.023) *** | 1.008 (1.002, 1.013) ** | |
| Tianshui | 1.002 (0.993, 1.010) | 0.989 (0.969, 1.009) | 0.964 (0.954, 0.975) *** | |
| Zhangye | 1.007 (0.993, 1.021) | 1.009 (0.990, 1.028) | 0.975 (0.952, 0.998) * | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, Y.; Sun, J.; Lei, R.; Zheng, J.; Tian, X.; Xue, B.; Luo, B. The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China. Int. J. Environ. Res. Public Health 2023, 20, 1959. https://doi.org/10.3390/ijerph20031959
Li Y, Sun J, Lei R, Zheng J, Tian X, Xue B, Luo B. The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China. International Journal of Environmental Research and Public Health. 2023; 20(3):1959. https://doi.org/10.3390/ijerph20031959
Chicago/Turabian StyleLi, Yanlin, Jianyun Sun, Ruoyi Lei, Jie Zheng, Xiaoyu Tian, Baode Xue, and Bin Luo. 2023. "The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China" International Journal of Environmental Research and Public Health 20, no. 3: 1959. https://doi.org/10.3390/ijerph20031959
APA StyleLi, Y., Sun, J., Lei, R., Zheng, J., Tian, X., Xue, B., & Luo, B. (2023). The Interactive Effects between Drought and Air Pollutants on Children’s Upper Respiratory Tract Infection: A Time-Series Analysis in Gansu, China. International Journal of Environmental Research and Public Health, 20(3), 1959. https://doi.org/10.3390/ijerph20031959






