First-Year Implementation of the EXercise for Cancer to Enhance Living Well (EXCEL) Study: Building Networks to Support Rural and Remote Community Access to Exercise Oncology Resources
Abstract
1. Introduction
2. Materials and Methods
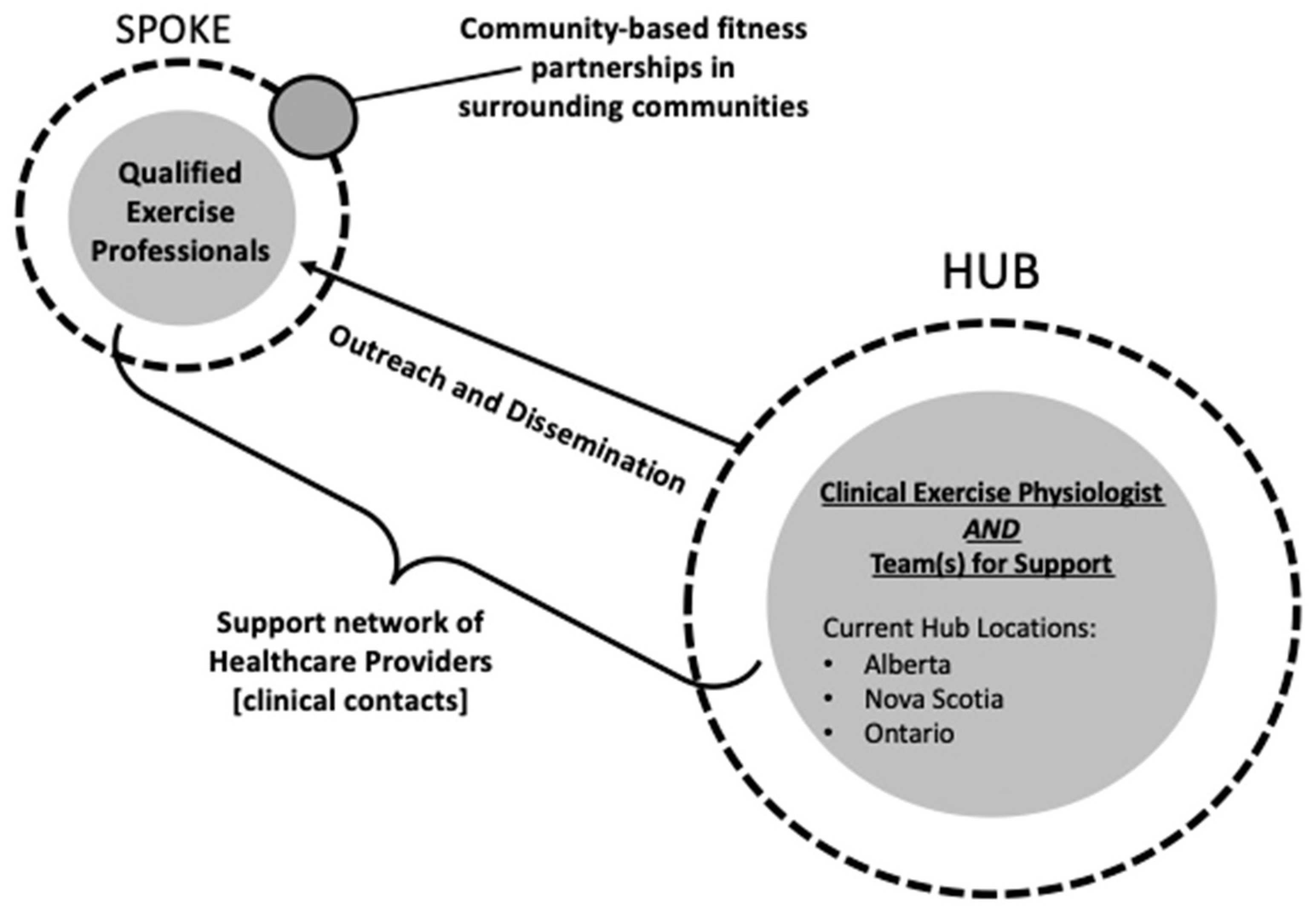
2.1. Study Design
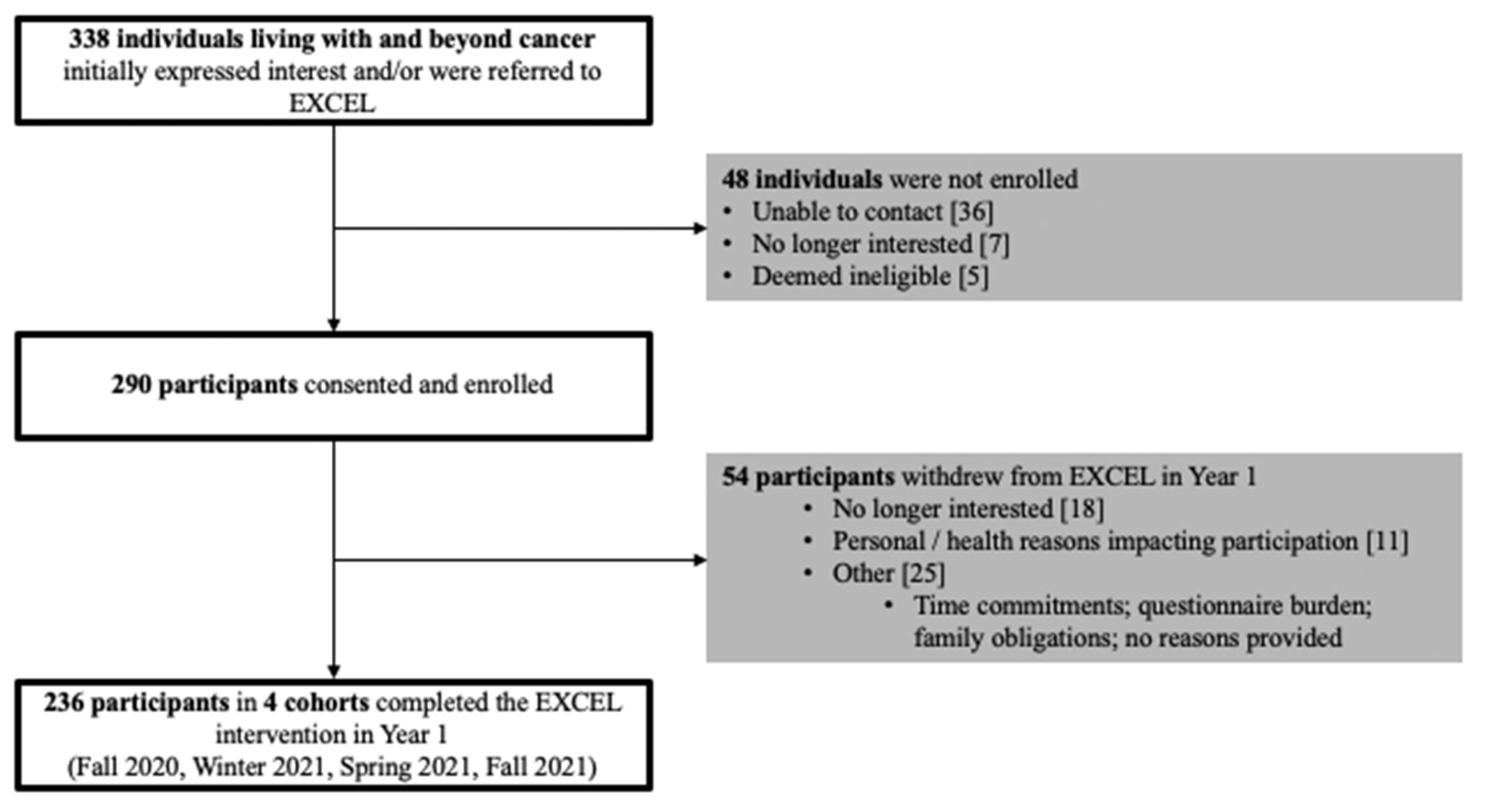
2.2. Participants
2.3. EXCEL Exercise-Oncology Program
2.4. RE-AIM Outcomes
2.4.1. Reach
2.4.2. Adoption
Healthcare Provider Network
Qualified Exercise Professional Network
2.4.3. Implementation
2.5. Analysis
3. Results
3.1. Reach
3.1.1. Participant Demographics and Clinical Characteristics
3.1.2. EXCEL Study Enrolment, Study Refusal, Referral Type, and Referral Resources
3.2. Adoption
3.2.1. Healthcare Provider Network
3.2.2. Qualified Exercise Professional Network
3.3. Implementation
4. Discussion
4.1. Reach and Adoption
4.2. Implementation
4.3. Future Directions: EXCEL Implementation Strategies
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Campbell, K.L.; Winters-Stone, K.M.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.S.; Matthews, C.E.; Ligibel, J.A.; Gerber, L.H.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef] [PubMed]
- Ottenbacher, A.J.; Day, R.S.; Taylor, W.C.; Sharma, S.V.; Sloane, R.; Snyder, D.C.; Kraus, W.E.; Demark-Wahnefried, W. Exercise among breast and prostate cancer survivors—What are their barriers? J. Cancer Surviv. 2011, 5, 413–419. [Google Scholar] [CrossRef] [PubMed]
- Eng, L.; Pringle, D.; Su, J.; Shen, X.; Mahler, M.; Niu, C.; Charow, R.; Tiessen, K.; Lam, C.; Halytskyy, O.; et al. Patterns, perceptions, and perceived barriers to physical activity in adult cancer survivors. Support. Care Cancer 2018, 26, 3755–3763. [Google Scholar] [CrossRef]
- Lawler, S.; Spathonis, K.; Masters, J.; Adams, J.; Eakin, E. Follow-up care after breast cancer treatment: Experiences and perceptions of service provision and provider interactions in rural Australian women. Support. Care Cancer 2010, 19, 1975–1982. [Google Scholar] [CrossRef] [PubMed]
- Butow, P.N.; Phillips, F.; Schweder, J.; White, K.; Underhill, C.; Goldstein, D.; Clinical Oncological Society of Australia. Psychosocial well-being and supportive care needs of cancer patients living in urban and rural/regional areas: A systematic review. Support. Care Cancer 2011, 20, 1–22. [Google Scholar] [CrossRef] [PubMed]
- Levit, L.A.; Byatt, L.; Lyss, A.P.; Paskett, E.D.; Levit, K.; Kirkwood, K.; Schenkel, C.; Schilsky, R.L. Closing the Rural Cancer Care Gap: Three Institutional Approaches. JCO Oncol. Pract. 2020, 16, 422–430. [Google Scholar] [CrossRef] [PubMed]
- Winters-Stone, K.M.; Boisvert, C.; Li, F.; Lyons, K.S.; Beer, T.M.; Mitri, Z.; Meyers, G.; Eckstrom, E.; Campbell, K.L. Delivering exercise medicine to cancer survivors: Has COVID-19 shifted the landscape for how and who can be reached with supervised group exercise? Support. Care. Cancer. 2022, 30, 1903–1906. [Google Scholar] [CrossRef]
- Sagarra-Romero, L.; Butragueño, J.; Gomez-Bruton, A.; Lozano-Berges, G.; Vicente-Rodríguez, G.; Morales, J.S. Effects of an online home-based exercise intervention on breast cancer survivors during COVID-19 lockdown: A feasibility study. Support. Care Cancer 2022, 30, 6287–6297. [Google Scholar] [CrossRef]
- MacDonald, A.M.; Chafranskaia, A.; Lopez, C.J.; Maganti, M.; Bernstein, L.J.; Chang, E.; Langelier, D.M.; Obadia, M.; Edwards, B.; Oh, P.; et al. CaRE @ Home: Pilot Study of an Online Multidimensional Cancer Rehabilitation and Exercise Program for Cancer Survivors. JCM 2020, 9, 3092. [Google Scholar] [CrossRef]
- Garcia-Roca, M.E.; Rodriguez-Arrastia, M.; Ropero-Padilla, C.; Domingo, C.H.; Folch-Ayora, A.; Temprado-Albalat, M.D.; Boldo-Roda, A.; Collado-Boira, E. Breast Cancer Patients’ Experiences with Online Group-Based Physical Exercise in a COVID-19 Context: A Focus Group Study. JPM 2022, 12, 356. [Google Scholar] [CrossRef]
- Myers, S.A.; Weller, S.; Schwartz, S.; Van Patten, C.; LeVasseur, N.; Faulkner, G.; Campbell, K.L. Feasibility of a Supervised Virtual Exercise Program for Women on Hormone Therapy for Breast Cancer. Transl. J. ACSM 2022, 7, e000213. [Google Scholar] [CrossRef]
- Rogers, L.Q.; Goncalves, L.; Martin, M.Y.; Pisu, M.; Smith, T.L.; Hessong, D.; Oster, R.A.; Qu, H.; Shewchuk, R.; Iqbal, F.; et al. Beyond efficacy: A qualitative organizational perspective on key implementation science constructs important to physical activity intervention translation to rural community cancer care sites. J. Cancer Surviv. 2019, 13, 537–546. [Google Scholar] [CrossRef] [PubMed]
- Purdy, G.M.; Sobierajski, F.M.; Dolgoy, N.D.; McNeely, M.L. Evaluating implementation and pragmatism of cancer-specific exercise programs: A scoping review. J Cancer Surviv. 2022, 16, 374–387. [Google Scholar] [CrossRef]
- Mina, D.S.; Sabiston, C.; Au, D.; Fong, A.; Capozzi, L.; Langelier, D.; Chasen, M.; Chiarotto, J.; Tomasone, J.; Jones, J.; et al. Connecting People with Cancer to Physical Activity and Exercise Programs: A Pathway to Create Accessibility and Engagement. Curr. Oncol. 2018, 25, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Culos-Reed, N.; Wagoner, C.W.; Dreger, J.; McNeely, M.L.; Keats, M.; Santa Mina, D.; Cuthbert, C.; Capozzi, L.C.; Francis, G.J.; Chen, G.; et al. Implementing an exercise oncology model to reach rural and remote individuals living with and beyond cancer: A hybrid effectiveness-implementation protocol for project EXCEL (EXercise for Cancer to Enhance Living Well). BMJ Open 2022, 12, e063953. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Vogt, T.M.; Boles, S.M. Evaluating the public health impact of health promotion interventions: The RE-AIM framework. Am. J. Public Health 1999, 89, 1322–1327. [Google Scholar] [CrossRef] [PubMed]
- Glasgow, R.E.; Harden, S.M.; Gaglio, B.; Rabin, B.; Smith, M.L.; Porter, G.C.; Ory, M.G.; Estabrooks, P.A. RE-AIM Planning and Evaluation Framework: Adapting to New Science and Practice With a 20-Year Review. Front. Public Health 2019, 7, 64. [Google Scholar] [CrossRef] [PubMed]
- McNeely, M.L.; Sellar, C.; Williamson, T.; Shea-Budgell, M.; Joy, A.A.; Lau, H.Y.; Easaw, J.C.; Murtha, A.D.; Vallance, J.; Courneya, K.; et al. Community-based exercise for health promotion and secondary cancer prevention in Canada: Protocol for a hybrid effectiveness-implementation study. BMJ open 2019, 9, e029975. [Google Scholar] [CrossRef]
- Developing Meaningful Categories for Distinguishing Levels of Remoteness in Canada. Available online: https://www150.statcan.gc.ca/n1/en/pub/11-633-x/11-633-x2020002-eng.pdf?st=-C6R8DT1 (accessed on 1 January 2023).
- Bredin, S.S.D.; Gledhill, N.; Jamnik, V.K.; Warburton, D.E.R. PAR-Q+ and ePARmed-X+: New risk stratification and physical activity clearance strategy for physicians and patients alike. Can. Fam. Physician 2013, 59, 273–277. [Google Scholar]
- Common Terminology Criteria for Adverse Events (CTCAE), Version 5; NIH: Bethesda, MD, USA, 2017.
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. The REDCap consortium: Building an international community of software platform partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Culos-Reed, S.N. The Importance of Exercise in Cancer Patients: The EXCEL Program. Available online: https://www.lungcancercanada.ca/en-CA/Resources/Lung-Cancer-Voices-Podcast-Main/Lung-Cancer-Voices-Podcast.aspx (accessed on 1 November 2022).
- Wagoner, C.W.; Capozzi, L.C.; Culos-Reed, S.N. Tailoring the Evidence for Exercise Oncology within Breast Cancer Care. Curr. Oncol. 2022, 29, 4827–4841. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.L.; Cormie, P.; Weller, S.; Alibhai, S.M.H.; Bolam, K.A.; Campbell, A.; Cheville, A.L.; Dalzell, M.-A.; Hart, N.H.; Higano, C.S.; et al. Exercise Recommendation for People with Bone Metastases: Expert Consensus for Health Care Providers and Exercise Professionals. JCO Oncol. Pract. 2022, 18, e697–e709. [Google Scholar] [CrossRef] [PubMed]
- Yoga for Young Adults Affected by Cancer. Available online: https://kinesiology.ucalgary.ca/labs/health-and-wellness/research/research-studies/pediatric-oncology-research/yoga-young-adults (accessed on 30 November 2022).
- Bansal, M.; Rana, B.; Ghotra, H.; King-Shier, K.; Bridel, W.; Culos-Reed, S.N. Exploring physical activity experiences, barriers, and facilitators among individuals of South Asian heritage living with and beyond cancer. Ethn. Health, 2022; under review. [Google Scholar]
- Rana, B.; MacRae, H.; Yang, L.; Bridel, W.; Culos-Reed, S.N. Equity, diversity, and inclusion across exercise oncology: A focus on LGBTQIA2S+ living with and beyond cancer. In Proceedings of the Canadian Association of Psychosocial Oncology-Presentation, Toronto, ON, Canada, 29 August–1 September 2022. [Google Scholar]
- Schmidt, M.E.; Wiskemann, J.; Ulrich, C.M.; Schneeweiss, A.; Steindorf, K. Self-reported physical activity behavior of breast cancer survivors during and after adjuvant therapy: 12 months follow-up of two randomized exercise intervention trials. Acta Oncol. 2017, 56, 618–627. [Google Scholar] [CrossRef]
- De Groef, A.; Demeyer, H.; de Kinkelder, C.; Althuis, S.D.-V.; Asnong, A.; Dams, L.; Van der Gucht, E.; De Vrieze, T.; Haenen, V.; Evenepoel, M.; et al. Physical Activity Levels of Breast Cancer Patients Before Diagnosis Compared to a Reference Population: A Cross-Sectional Comparative Study. Clin. Breast Cancer 2022, 22, e708–e717. [Google Scholar] [CrossRef]
- De Groef, A.; Geraerts, I.; Demeyer, H.; Van der Gucht, E.; Dams, L.; de Kinkelder, C.; Dukers-van Althuis, S.; Van Kampen, M.; Devoogdt, N. Physical activity levels after treatment for breast cancer: Two-year follow-up. Breast 2018, 40, 23–28. [Google Scholar] [CrossRef]
- Kennedy, M.A.; Bayes, S.; Newton, R.U.; Zissiadis, Y.; Spry, N.A.; Taaffe, D.R.; Hart, N.H.; Galvão, D.A. Implementation barriers to integrating exercise as medicine in oncology: An ecological scoping review. J. Cancer Surviv. 2021, 16, 865–881. [Google Scholar] [CrossRef]
- Daun, J.T.; Capozzi, L.C.; Urgoiti, G.R.; McDonough, M.H.; Easaw, J.C.; McNeely, M.L.; Francis, G.J.; Williamson, T.; Danyluk, J.; McLaughlin, E.; et al. ACE-Neuro: A tailored exercise oncology program for neuro-oncology patients–Study protocol. Contemp. Clin. Trials Commun. 2022, 28, 100925. [Google Scholar] [CrossRef]
- Daun, J.T.; Twomey, R.; Capozzi, L.C.; Crump, T.; Francis, G.J.; Matthews, T.W.; Chandarana, S.; Hart, R.D.; Schrag, C.; Matthews, J.; et al. The feasibility of patient-reported outcomes, physical function, and mobilization in the care pathway for head and neck cancer surgical patients. Pilot Feasibility Stud. 2022, 8, 114. [Google Scholar] [CrossRef]
- Schmitz, K.H.; Campbell, A.M.; Stuiver, M.M.; Pinto, B.M.; Schwartz, A.L.; Morris, G.S.; Ligibel, J.A.; Cheville, A.; Galvão, D.A.; Alfano, C.M.; et al. Exercise is medicine in oncology: Engaging clinicians to help patients move through cancer. CA Cancer J. Clin. 2019, 69, 468–484. [Google Scholar] [CrossRef]
- Schmitz, K.H.; Stout, N.L.; Mpp, M.M.; Campbell, A.; Schwartz, A.L.; Grimmett, C.; Meyerhardt, J.A.; Do, J.M.S. Moving through cancer: Setting the agenda to make exercise standard in oncology practice. Cancer 2020, 127, 476–484. [Google Scholar] [CrossRef] [PubMed]
- Ford, S.; Buscemi, J.; Hirko, K.; Laitner, M.; Newton, R.L.; Jonassaint, C.; FitzGibbon, M.; Klesges, L. Society of Behavioral Medicine (SBM) urges Congress to ensure efforts to increase and enhance broadband internet access in rural areas. Transl. Behav. Med. 2020, 10, 489–491. [Google Scholar] [CrossRef] [PubMed]

| Variable | Participants (n = 236) |
|---|---|
| Age (years) † | 57.3 (12.5) |
| Location | |
| Rural/Remote | 199 (84.3) |
| Urban | 37 (15.7) |
| Sex | |
| Female | 192 (82.1) |
| Male | 42 (17.9) |
| Ancestral Ethnicity | |
| Aboriginal | 4 (1.7) |
| Asian | 14 (5.9) |
| British | 81 (34.3) |
| Caribbean | 1 (0.4) |
| European | 72 (30.5) |
| Latin/Central and South America | 6 (2.5) |
| Multi-ethnic | 38 (16.1) |
| No information provided | 20 (8.5) |
| Education | |
| High school or less | 25 (10.7) |
| More than high school | 209 (89.3) |
| Employment Status | |
| Full Time | 41 (17.5) |
| Part Time | 31 (13.2) |
| Retired | 85 (36.3) |
| Homemaker | 8 (3.4) |
| Disability | 56 (23.9) |
| Temporarily Unemployed | 13 (5.6) |
| Marital Status | |
| Not Married | 55 (23.5) |
| Married | 152 (65.0) |
| Common Law | 27 (11.5) |
| Cancer Type | |
| Breast | 126 (53.4) |
| Lung | 20 (8.5) |
| Hematologic | 19 (8.1) |
| Gynecological | 16 (6.8) |
| Prostate | 16 (6.8) |
| Skin | 6 (2.5) |
| Brain | 6 (2.5) |
| Colon | 6 (2.5) |
| Head and Neck | 5 (2.1) |
| Other ‡ | 16 (6.8) |
| Advanced Cancer | |
| Yes | 64 (27.4) |
| No | 170 (72.6) |
| Treatment Status | |
| On | 128 (54.7) |
| Off | 106 (45.3) |
| Treatment Type for participants ‘On’ treatment | |
| Chemotherapy | 33 (26.2) |
| Radiation | 5 (4.0) |
| Hormone Therapy | 52 (41.3) |
| Combination * | 16 (12.7) |
| Other ** | 20 (15.9) |
| Variable (n, % of Year One Total) | Alberta | Nova Scotia | Ontario | Year One Total |
|---|---|---|---|---|
| Reach (n, % of Year one total) | ||||
| Enrolled Participants | 113 | 60 | 63 | 236 |
| Direct HCP Referral | 0 | 18 | 2 | 20 (8.5%) |
| Indirect HCP Referral | 33 | 2 | 2 | 37 (15.7%) |
| Self-Referral | 80 | 40 | 59 | 179 (75.8%) |
| Adoption—QEP Network (n) | ||||
| Fitness Professional Partnerships | 13 | 7 | 12 | 32 |
| Health and Wellness Organizations | 4 | 6 | 9 | 19 |
| Individual QEPs | 9 | 1 | 3 | 13 |
| Trained QEPs | 17 | 12 | 16 | 45 |
| QEPs Delivering EXCEL Classes | 9 | 6 | 7 | 22 |
| Implementation (n or %) | ||||
| Exercise Intervention Adherence | 76.7% | 82.3% | 77.0% | 78.2% |
| Fitness-Assessment Completion | ||||
| Baseline | 100.0% | 93.3% | 100.0% | 98.3% |
| 12-week | 92.0% | 90.0% | 85.7% | 89.8% |
| Patient-Reported Outcome Completion | ||||
| Baseline | 99.1% | 96.7% | 92.1% | 96.6% |
| 12-week | 92.0% | 90.0% | 77.8% | 87.7% |
| Exercise Classes Implemented | 16 | 14 | 7 | 37 |
| Referral Resource Descriptions | Number of Times Resources Were Indicated |
|---|---|
| Word of Mouth (57.7%) | |
| Friend or Family Member | 3 |
| Previous or Current Participant | 21 |
| Support Group | 34 |
| Health and Wellness Organizations and Programs | 77 |
| EXCEL Team Outreach (20.1%) | |
| Online Presentations | 1 |
| Social Media or Websites | 19 |
| Study Staff | 27 |
| Healthcare Provider (18.8%) | |
| Social Worker | 1 |
| Lymphedema Specialist | 1 |
| HCP provided brochure in clinic | 3 |
| Patient Navigator | 3 |
| Care Coordinator | 3 |
| Primary Care Network | 5 |
| Oncologist | 12 |
| Nurse | 16 |
| Print Materials (3.4%) | |
| Posters | 3 |
| Brochures | 5 |
| HCP Organizations (n = 11) | Number of Presentations (n = 14) | Hub That Provided Presentation |
|---|---|---|
| Cancer Centres | ||
| Tom Baker Cancer Centre | 3 | Alberta |
| Allan Blair Cancer Centre | 1 | Alberta |
| Margery E. Yuill Cancer Centre | 1 | Alberta |
| Jack Ady Cancer Centre | 1 | Alberta |
| Cancer Care Organizations | ||
| Nova Scotia Health (Medical Oncology) | 1 | Nova Scotia |
| Nova Scotia Cancer Care Clinic | 1 | Nova Scotia |
| Canadian Association of General Practitioners in Oncology | 1 | Nova Scotia |
| Canadian Association of Psychosocial Oncology | 1 | Alberta |
| Cancer Care Ontario | 1 | Ontario |
| Non-Profit Organizations | ||
| Exercise is Medicine | 2 | Alberta |
| Inpower | 1 | Alberta |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wagoner, C.W.; Dreger, J.; Keats, M.R.; Santa Mina, D.; McNeely, M.L.; Cuthbert, C.; Capozzi, L.C.; Francis, G.J.; Trinh, L.; Sibley, D.; et al. First-Year Implementation of the EXercise for Cancer to Enhance Living Well (EXCEL) Study: Building Networks to Support Rural and Remote Community Access to Exercise Oncology Resources. Int. J. Environ. Res. Public Health 2023, 20, 1930. https://doi.org/10.3390/ijerph20031930
Wagoner CW, Dreger J, Keats MR, Santa Mina D, McNeely ML, Cuthbert C, Capozzi LC, Francis GJ, Trinh L, Sibley D, et al. First-Year Implementation of the EXercise for Cancer to Enhance Living Well (EXCEL) Study: Building Networks to Support Rural and Remote Community Access to Exercise Oncology Resources. International Journal of Environmental Research and Public Health. 2023; 20(3):1930. https://doi.org/10.3390/ijerph20031930
Chicago/Turabian StyleWagoner, Chad W., Julianna Dreger, Melanie R. Keats, Daniel Santa Mina, Margaret L. McNeely, Colleen Cuthbert, Lauren C. Capozzi, George J. Francis, Linda Trinh, Daniel Sibley, and et al. 2023. "First-Year Implementation of the EXercise for Cancer to Enhance Living Well (EXCEL) Study: Building Networks to Support Rural and Remote Community Access to Exercise Oncology Resources" International Journal of Environmental Research and Public Health 20, no. 3: 1930. https://doi.org/10.3390/ijerph20031930
APA StyleWagoner, C. W., Dreger, J., Keats, M. R., Santa Mina, D., McNeely, M. L., Cuthbert, C., Capozzi, L. C., Francis, G. J., Trinh, L., Sibley, D., Langley, J., Chiekwe, J., Ester, M., Foucaut, A.-M., & Culos-Reed, S. N. (2023). First-Year Implementation of the EXercise for Cancer to Enhance Living Well (EXCEL) Study: Building Networks to Support Rural and Remote Community Access to Exercise Oncology Resources. International Journal of Environmental Research and Public Health, 20(3), 1930. https://doi.org/10.3390/ijerph20031930








