Physical Activity Level, Barriers, and Facilitators for Exercise Engagement for Chronic Community-Dwelling Stroke Survivors in Low-Income Settings: A Cross-Sectional Study in Benin
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics Considerations
2.2. Setting
2.3. Participants and Recruitment
2.4. Procedure
2.5. Outcome Measures
2.5.1. International Physical Activity Questionnaire-Long Form (IPAQ-LF-Benin)
2.5.2. Stroke Exercise Preference Inventory-13 (SEPI-13)
2.6. Statistical Analysis
3. Results
3.1. Participants
3.2. Description of the Sample
3.3. Physical Activity Level and Perceived Barriers and Facilitators for Stroke Survivors
3.3.1. Level of PA Practice for People with Stroke
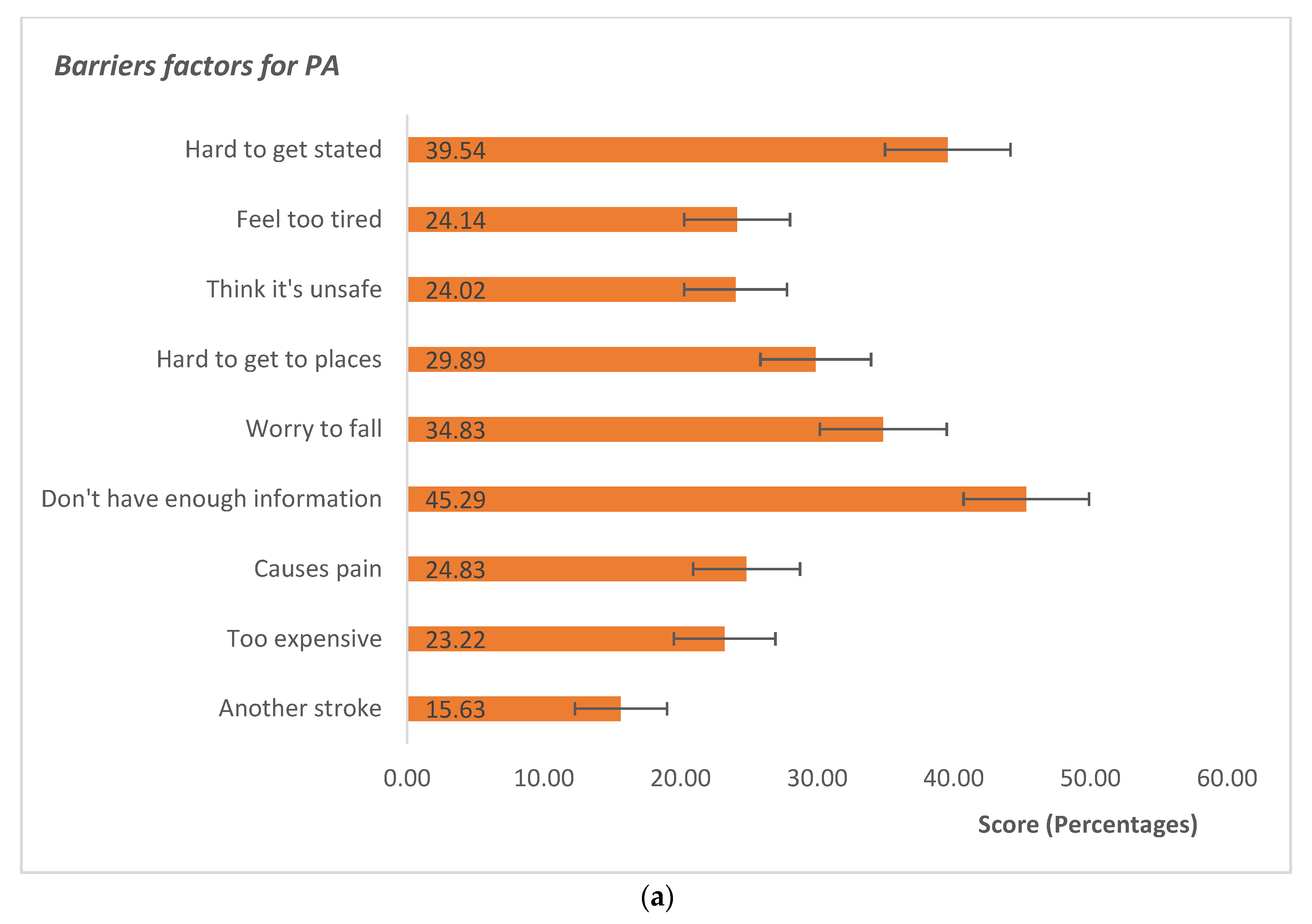
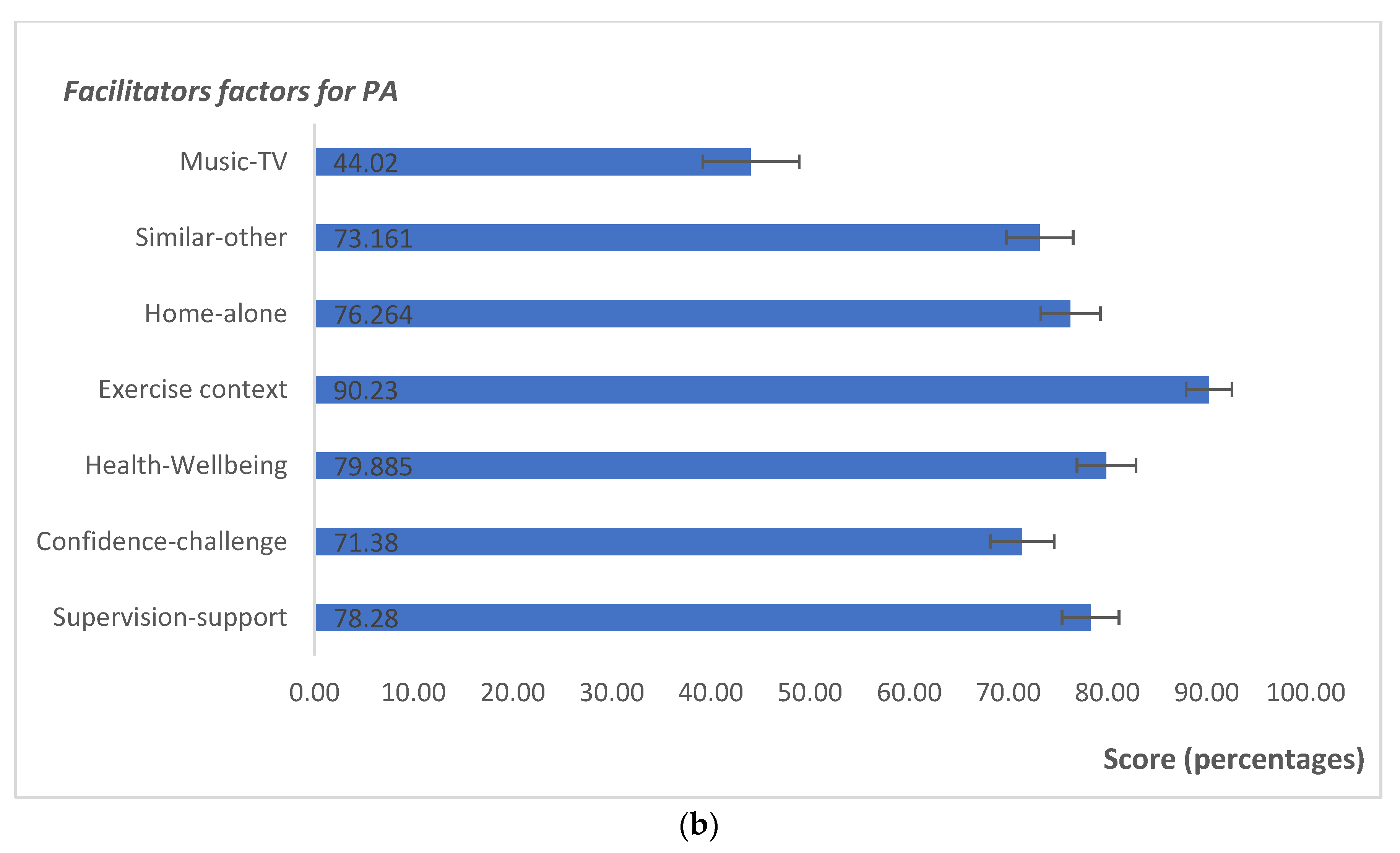
3.3.2. Barriers and Facilitators
3.4. Relationship between PA Level and Other Factors
4. Discussion
4.1. Strengths and Limitations
4.2. Implications and Recommendations for Clinical Field and Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sacco, R.L.; Kasner, S.E.; Broderick, J.P.; Caplan, L.R.; Connors, J.; Culebras, A.; Elkind, M.S.; George, M.G.; Hamdan, A.D.; Higashida, R.T. An updated definition of stroke for the 21st century: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2013, 44, 2064–2089. [Google Scholar] [CrossRef] [PubMed]
- Adoukonou, T.; Kossi, O.; Fotso Mefo, P.; Agbetou, M.; Magne, J.; Gbaguidi, G.; Houinato, D.; Preux, P.-M.; Lacroix, P. Stroke case fatality in sub-Saharan Africa: Systematic review and meta-analysis. Int. J. Stroke 2021, 16, 902–916. [Google Scholar] [CrossRef] [PubMed]
- Adoukonou, T.; Kossi, O.; Agbétou, M.; Tchaou, B.; Agballa, G.; Houinato, D. Short term (3 months) prognosis of stroke in Parakou. Neurosci. Med. 2018, 9, 81–93. [Google Scholar] [CrossRef]
- Roth, G.A.; Mensah, G.A.; Johnson, C.O.; Addolorato, G.; Ammirati, E.; Baddour, L.M.; Barengo, N.C.; Beaton, A.Z.; Benjamin, E.J.; Benziger, C.P. Global burden of cardiovascular diseases and risk factors, 1990–2019: Update from the GBD 2019 study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, J.H.; Wang, E.; Smith, D. Barriers associated with exercise and community access for individuals with stroke. J. Rehabil. Res. Dev. 2008, 45, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Noukpo, S.I.; Kossi, O.; Triccas, L.T.; Adoukonou, T.; Feys, P. Content and effectiveness of community-based rehabilitation on quality of life in people post stroke: A systematic review with meta-analysis. Disabil. CBR Incl. Dev. 2022, 33, 75–107. [Google Scholar] [CrossRef]
- Billinger, S.A.; Arena, R.; Bernhardt, J.; Eng, J.J.; Franklin, B.A.; Johnson, C.M.; Mackay-Lyons, M.; Macko, R.F.; Mead, G.E.; Roth, E.J.; et al. Physical activity and exercise recommendations for stroke survivors: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2532–2553. [Google Scholar] [CrossRef]
- Morris, J.H.; Macgillivray, S.; McFarlane, S. Interventions to promote long-term participation in physical activity after stroke: A systematic review of the literature. Arch. Phys. Med. Rehabil. 2014, 95, 956–967. [Google Scholar] [CrossRef]
- Nindorera, F.; Nduwimana, I.; Thonnard, J.L.; Kossi, O. Effectiveness of walking training on balance, motor functions, activity, participation and quality of life in people with chronic stroke: A systematic review with meta-analysis and meta-regression of recent randomized controlled trials. Disabil. Rehabil. 2021, 44, 3760–3771. [Google Scholar] [CrossRef]
- Ainsworth, B.E.; Haskell, W.L.; Herrmann, S.D.; Meckes, N.; Bassett, D.R., Jr.; Tudor-Locke, C.; Greer, J.L.; Vezina, J.; Whitt-Glover, M.C.; Leon, A.S. 2011 Compendium of Physical Activities: A second update of codes and MET values. Med. Sci. Sports Exerc. 2011, 43, 1575–1581. [Google Scholar] [CrossRef]
- Tremblay, M. Letter to the Editor: Standardised use of the terms “sedentary” and “sedentary behaviours". Afr. J. Phys. Act. Health Sci. 2012, 18, 200–204. [Google Scholar]
- Gill, J.M.; Bhopal, R.; Douglas, A.; Wallia, S.; Bhopal, R.; Sheikh, A.; Forbes, J.F.; McKnight, J.; Sattar, N.; Murray, G. Sitting time and waist circumference are associated with glycemia in UK South Asians: Data from 1,228 adults screened for the PODOSA trial. Diabetes Care 2011, 34, 1214–1218. [Google Scholar] [CrossRef]
- Veerman, J.L.; Healy, G.N.; Cobiac, L.J.; Vos, T.; Winkler, E.A.; Owen, N.; Dunstan, D.W. Television viewing time and reduced life expectancy: A life table analysis. Br. J. Sports Med. 2012, 46, 927–930. [Google Scholar] [CrossRef]
- Moore, S.A.; Hallsworth, K.; Jakovljevic, D.G.; Blamire, A.M.; He, J.; Ford, G.A.; Rochester, L.; Trenell, M.I. Effects of community exercise therapy on metabolic, brain, physical, and cognitive function following stroke: A randomized controlled pilot trial. Neurorehabil. Neural Repair 2015, 29, 623–635. [Google Scholar] [CrossRef]
- Cramp, M.C.; Greenwood, R.J.; Gill, M.; Lehmann, A.; Rothwell, J.C.; Scott, O.M. Effectiveness of a community-based low intensity exercise programme for ambulatory stroke survivors. Disabil. Rehabil. 2010, 32, 239–247. [Google Scholar] [CrossRef]
- Mead, G.E.; Greig, C.A.; Cunningham, I.; Lewis, S.J.; Dinan, S.; Saunders, D.H.; Fitzsimons, C.; Young, A. Stroke: A randomized trial of exercise or relaxation. J. Am. Geriatr. Soc. 2007, 55, 892–899. [Google Scholar] [CrossRef]
- Macko, R.F.; Ivey, F.M.; Forrester, L.W.; Hanley, D.; Sorkin, J.D.; Katzel, L.I.; Silver, K.H.; Goldberg, A.P. Treadmill exercise rehabilitation improves ambulatory function and cardiovascular fitness in patients with chronic stroke: A randomized, controlled trial. Stroke 2005, 36, 2206–2211. [Google Scholar] [CrossRef]
- Mudge, S.; Barber, P.A.; Stott, N.S. Circuit-based rehabilitation improves gait endurance but not usual walking activity in chronic stroke: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2009, 90, 1989–1996. [Google Scholar] [CrossRef]
- Saunders, D.H.; Sanderson, M.; Hayes, S.; Johnson, L.; Kramer, S.; Carter, D.D.; Jarvis, H.; Brazzelli, M.; Mead, G.E. Physical fitness training for stroke patients. Cochrane Database Syst. Rev. 2020, 2020, CD003316. [Google Scholar]
- Scottish Intercollegiate Guidelines Network. Management of Patients with Stroke or TIA: Assessment, Investigation, Immediate Management and Secondary Prevention: A National Clinical Guideline; Scottish Intercollegiate Guidelines Network: Edinburgh, UK, 2008; ISBN 1-905813-40-6. [Google Scholar]
- Kaminsky, L.A.; Montoye, A.H. Physical activity and health: What is the best dose? J. Am. Heart Assoc. 2014, 3, e001430. [Google Scholar] [CrossRef]
- Butler, E.N.; Evenson, K.R. Prevalence of physical activity and sedentary behavior among stroke survivors in the United States. Top. Stroke Rehabil. 2014, 21, 246–255. [Google Scholar] [CrossRef] [PubMed]
- Adeniyi, A.; Idowu, O.; Ogwumike, O.; Adeniyi, C. Comparative influence of self-efficacy, social support and perceiived barriers on low physical activity development in patients with type 2 diabetes, hypertension or stroke. Ethiop. J. Health Sci. 2012, 22, 113–119. [Google Scholar] [PubMed]
- McDonnell, M.N.; Esterman, A.J.; Williams, R.S.; Walker, J.; Mackintosh, S.F. Physical activity habits and preferences in the month prior to a first-ever stroke. PeerJ 2014, 2, e489. [Google Scholar] [CrossRef] [PubMed]
- Damush, T.M.; Plue, L.; Bakas, T.; Schmid, A.; Williams, L.S. Barriers and facilitators to exercise among stroke survivors. Rehabil. Nurs. 2007, 32, 253–262. [Google Scholar] [CrossRef] [PubMed]
- Idowu, O.A.; Adeniyi, A.F.; Ogwumike, O.O.; Fawole, H.O.; Akinrolie, O. Perceived barriers to physical activity among Nigerian stroke survivors. Pan Afr. Med. J. 2015, 21, 274. [Google Scholar] [CrossRef] [PubMed]
- English, C.; Manns, P.J.; Tucak, C.; Bernhardt, J. Physical activity and sedentary behaviors in people with stroke living in the community: A systematic review. Phys. Ther. 2014, 94, 185–196. [Google Scholar] [CrossRef] [PubMed]
- Van Swieten, J.; Koudstaal, P.; Visser, M.; Schouten, H.; Van Gijn, J. Interobserver agreement for the assessment of handicap in stroke patients. stroke 1988, 19, 604–607. [Google Scholar] [CrossRef]
- Hall, K.S.; Gao, S.; Emsley, C.L.; Ogunniyi, A.O.; Morgan, O.; Hendrie, H.C. Community screening interview for dementia (CSI ‘D’); performance in five disparate study sites. Int. J. Geriatr. Psychiatry 2000, 15, 521–531. [Google Scholar] [CrossRef]
- Resnick, B.; Michael, K.; Shaughnessy, M.; Nahm, E.S.; Kopunek, S.; Sorkin, J.; Orwig, D.; Goldberg, A.; Macko, R.F. Inflated perceptions of physical activity after stroke: Pairing self-report with physiologic measures. J. Phys. Act. Health 2008, 5, 308–318. [Google Scholar] [CrossRef]
- Chau, M.W.R.; Chan, S.P.; Wong, Y.W.; Lau, M.Y.P. Reliability and validity of the Modified Functional Ambulation Classification in patients with hip fracture. Hong Kong Physiother. J. 2013, 31, 41–44. [Google Scholar] [CrossRef]
- Wu, G.; Sanderson, B.; Bittner, V. The 6-minute walk test: How important is the learning effect? Am. Heart J. 2003, 146, 129–133. [Google Scholar] [CrossRef]
- Williams, N. The Borg rating of perceived exertion (RPE) scale. Occup. Med. 2017, 67, 404–405. [Google Scholar] [CrossRef]
- Wall, J.C.; Bell, C.; Campbell, S.; Davis, J. The Timed Get-up-and-Go test revisited: Measurement of the component tasks. J. Rehabil. Res. Dev. 2000, 37, 109–113. [Google Scholar]
- Honado, S.A. Adaptation et Validation du Questionnaire International de L’activité Physique (IPAQ) Chez Les Personnes Saines et Les Survivants D’un Accident Vasculaire Cérébral au Bénin; Université Laval: Québec, QC, Canada, 2019. [Google Scholar]
- IPAQ Research Committee. International Physical Activity Questionnaire (IPAQ); IPAQ Research Committee: Ottawa, ON, Canada, 2005. [Google Scholar]
- Bonner, N.S.; O’Halloran, P.D.; Bernhardt, J.; Cumming, T.B. Developing the stroke exercise preference inventory (SEPI). PLoS ONE 2016, 11, e0164120. [Google Scholar] [CrossRef]
- Houehanou, Y.C.N.; Agbetou, M.; Kossi, O.; Agonnoudé, M.; Hountada, H.; Adoukonou, T. Prevalence and factors associated with stroke risk factors in an urban community of Parakou, Northern Benin, 2016. PLoS Glob. Public Health 2022, 2, e0000667. [Google Scholar] [CrossRef]
- Ferreira, A.J.; Aguiar, L.T.; Martins, J.C.; Faria, C.D.C.D.M. Stroke survivors with the same levels of exercise as healthy individuals have lower levels of physical activity. Neurol. Sci. 2022, 43, 3729–3735. [Google Scholar] [CrossRef]
- Ruescas-Nicolau, M.-A.; Sánchez-Sánchez, M.L.; Cortés-Amador, S.; Pérez-Alenda, S.; Arnal-Gómez, A.; Climent-Toledo, A.; Carrasco, J.J. Validity of the international physical activity questionnaire long form for assessing physical activity and sedentary behavior in subjects with chronic stroke. Int. J. Environ. Res. Public. Health 2021, 18, 4729. [Google Scholar] [CrossRef]
- Adjiwanou, V.; LeGrand, T. Gender inequality and the use of maternal healthcare services in rural sub-Saharan Africa. Health Place 2014, 29, 67–78. [Google Scholar] [CrossRef]
- Owoo, N.S.; Lambon-Quayefio, M.P. Mixed methods exploration of Ghanaian women’s domestic work, childcare and effects on their mental health. PLoS ONE 2021, 16, e0245059. [Google Scholar] [CrossRef]
- Teo, K.; Lear, S.; Islam, S.; Mony, P.; Dehghan, M.; Li, W.; Rosengren, A.; Lopez-Jaramillo, P.; Diaz, R.; Oliveira, G. Prevalence of a healthy lifestyle among individuals with cardiovascular disease in high-, middle- and low-income countries: The Prospective Urban Rural Epidemiology (PURE) study. JAMA 2013, 309, 1613–1621. [Google Scholar] [CrossRef]
- Gagnon, M.-A.; Batcho, C.S.; Best, K.L. A description of physical activity behaviors, barriers, and motivators in stroke survivors in Quebec. Disabil. Health J. 2022, 15, 101265. [Google Scholar] [CrossRef] [PubMed]
- Diaz, R.; Miller, E.K.; Kraus, E.; Fredericson, M. Impact of adaptive sports participation on quality of life. Sports Med. Arthrosc. Rev. 2019, 27, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Jaarsma, E.A.; Dijkstra, P.U.; Geertzen, J.; Dekker, R. Barriers to and facilitators of sports participation for people with physical disabilities: A systematic review. Scand. J. Med. Sci. Sports 2014, 24, 871–881. [Google Scholar] [CrossRef] [PubMed]
- Pandian, J.D.; Sudhan, P. Stroke epidemiology and stroke care services in India. J. Stroke 2013, 15, 128. [Google Scholar] [CrossRef] [PubMed]
- Débora Pacheco, B.; Guimaraes Caetano, L.C.; Amorim Samora, G.; Sant’Ana, R.; Fuscaldi Teixeira-Salmela, L.; Scianni, A.A. Perceived barriers to exercise reported by individuals with stroke, who are able to walk in the community. Disabil. Rehabil. 2021, 43, 331–337. [Google Scholar] [CrossRef]
- Nicholson, S.; Sniehotta, F.F.; Van Wijck, F.; Greig, C.A.; Johnston, M.; McMurdo, M.E.; Dennis, M.; Mead, G.E. A systematic review of perceived barriers and motivators to physical activity after stroke. Int. J. Stroke 2013, 8, 357–364. [Google Scholar] [CrossRef]
- Jackson, S.M. An Investigation of Factors Influencing Physical Activity Levels in People Living in the Community after Stroke; University of Western Australia: Crawley, Australia, 2015. [Google Scholar]
- Simpson, L.A.; Eng, J.J.; Tawashy, A.E. Exercise perceptions among people with stroke: Barriers and facilitators to participation. Int. J. Ther. Rehabil. 2011, 18, 520–529. [Google Scholar] [CrossRef]
- Ford, C.D.; Kim, M.J.; Dancy, B.L. Perceptions of hypertension and contributing personal and environmental factors among rural Southern African American women. Ethn. Dis. 2009, 19, 407. [Google Scholar]
- Webb, M.S.; Gonzalez, L.O. The burden of hypertension: Mental representations of African American women. Issues Ment. Health Nurs. 2006, 27, 249–271. [Google Scholar] [CrossRef]
- Choi, Y.-A.; Lee, J.S.; Park, J.H.; Kim, Y.H. Patterns of physical activity and sedentary behavior and their associated factors among nondisabled stroke survivors. Maturitas 2022, 158, 10–15. [Google Scholar] [CrossRef]
- Gordon, N.F.; Gulanick, M.; Costa, F.; Fletcher, G.; Franklin, B.A.; Roth, E.J.; Shephard, T. Physical activity and exercise recommendations for stroke survivors: An American Heart Association scientific statement from the Council on Clinical Cardiology, Subcommittee on Exercise, Cardiac Rehabilitation, and Prevention; the Council on Cardiovascular Nursing; the Council on Nutrition, Physical Activity, and Metabolism; and the Stroke Council. Circulation 2004, 109, 2031–2041. [Google Scholar]
- Wang, C.; Redgrave, J.; Shafizadeh, M.; Majid, A.; Kilner, K.; Ali, A.N. Aerobic exercise interventions reduce blood pressure in patients after stroke or transient ischaemic attack: A systematic review and meta-analysis. Br. J. Sports Med. 2019, 53, 1515–1525. [Google Scholar] [CrossRef]
- Chad, K.E.; Reeder, B.A.; Harrison, E.L.; Ashworth, N.L.; Sheppard, S.M.; Schultz, S.L.; Bruner, B.G.; Fisher, K.L.; Lawson, J.A. Profile of physical activity levels in community-dwelling older adults. Med. Sci. Sports Exerc. 2005, 37, 1774. [Google Scholar] [CrossRef]
- Juarbe, T.; Turok, X.P.; Pérez-Stable, E.J. Perceived benefits and barriers to physical activity among older Latina women. West. J. Nurs. Res. 2002, 24, 868–886. [Google Scholar] [CrossRef]
- Salazar, M.K. Interviewer bias: How it affects survey research. Aaohn J. 1990, 38, 567–572. [Google Scholar] [CrossRef]
- Marsden, D.L.; Dunn, A.; Callister, R.; McElduff, P.; Levi, C.R.; Spratt, N.J. A home-and community-based physical activity program can improve the cardiorespiratory fitness and walking capacity of stroke survivors. J. Stroke Cerebrovasc. Dis. 2016, 25, 2386–2398. [Google Scholar] [CrossRef]
- Lahtio, H.; Rintala, A.; Immonen, J.; Sjögren, T. The Effectiveness of Physical Activity-Promoting Web-and Mobile-Based Distance Weight Loss Interventions on Body Composition in Rehabilitation Settings: Systematic Review, Meta-analysis, and Meta-Regression Analysis. J. Med. Internet Res. 2022, 24, e25906. [Google Scholar] [CrossRef]
- Lear, S.A.; Hu, W.; Rangarajan, S.; Gasevic, D.; Leong, D.; Iqbal, R.; Casanova, A.; Swaminathan, S.; Anjana, R.M.; Kumar, R. The effect of physical activity on mortality and cardiovascular disease in 130 000 people from 17 high-income, middle-income, and low-income countries: The PURE study. Lancet 2017, 390, 2643–2654. [Google Scholar] [CrossRef]
| Sample Mean ± SD/Median (IQR)/n (%) | PA Moderate-Intense | OR (95% IC) | p | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Socio demographic factors | |||||
| Age (years) | 53.6 ± 10.3 | - | - | ||
| Age category (years) | |||||
| <50 | 29 (33.3) | 19 (65.5) | 10 (34.5) | 1 | |
| 50–60 | 32 (36.8) | 18 (56.3) | 14 (43.7) | 1.5 [0.5–4.2] | 0.459 |
| >60 | 26 (29.9) | 13 (50.0) | 13 (50.0) | 1.9 [0.6–5.6] | 0.244 |
| Sex | |||||
| Male | 52 (59.8) | 29 (55.8) | 23 (44.2) | 1 | |
| Female | 35 (40.2) | 20 (57.1) | 15 (42.9) | 0.9 [0.4–2.2] | 0.899 |
| Marital status | |||||
| Married | 73 (83.9) | 36 (49.3) | 37 (50.7) | 1 | |
| Single/Divorced/widower | 14 (16.1) | 13 (92.9) | 1 (7.1) | 0.07 [0.01–0.6] | 0.001 * |
| Profession | |||||
| Employed | 31 (35.6) | 21 (67.8) | 10 (32.2) | 1 | |
| Independent | 23 (26.4) | 11 (47.8) | 12 (52.2) | 2.3 [0.7–6.9] | 0.140 |
| Unemployed/household/other | 33 (37.9) | 17 (51.5) | 16 (48.5) | 1.9 [0.7–5.5] | 0.186 |
| Education level | |||||
| Illiterate | 11 (12.6) | 6 (57.6) | 5 (42.4) | 1 | |
| Primary | 28 (32.5) | 13 (46.4) | 15 (53.6) | 1.4 [0.3–5.6] | 0.648 |
| Secondary | 30 (34.5) | 17 (56.7) | 13 (43.3) | 0.9 [0.2–3.7] | 0.903 |
| Superior | 18 (20.7) | 13 (72.2) | 5 (27.8) | 0.4 [0.09–2.2] | 0.331 |
| Social insurance | |||||
| Yes | 38 (43.7) | 11 (28.9) | 27 (71.1) | 3.0 [1.2–7.4] | 0.015 * |
| No | 49 (56.3) | 27 (55.1) | 22 (44.9) | 1 | |
| Clinical characteristics | |||||
| Type of stroke | |||||
| Ischemic | 62 (71.3) | 36 (58.1) | 26 (41.9) | 1 | |
| Hemorrhagic | 18 (20.7) | 7 (38.9) | 11 (61.1) | 2.2 [0.7–6.4] | 0.151 |
| Non determined | 7 (8.0) | 6 (85.7) | 1 (14.3) | 0.2 [0.03–2.0] | 0.156 |
| Time after stroke (months) | 11 (IQR: 15) | - | - | ||
| Time after stroke category (months) | |||||
| [0–6] | 25 (28.7) | 16 (64.0) | 9 (36.0) | 1 | |
| [6–12] | 25 (28.7) | 17 (68.0) | 8 (32.0) | 0.8 [0.3–2.7] | 0.765 |
| >12 | 37 (42.6) | 16 (43.2) | 21 (56.8) | 2.3 [0.8–6.6] | 0.108 |
| Vascular risk factors (before stroke) | |||||
| None | 13 (14.9) | 2 (15.4) | 11 (84.6) | 6.8 [1.3–34.9] | 0.021 * |
| High blood pressure | 32 (36.8) | 11 (34.4) | 21 (65.6) | 2.3 [0.9–6.2] | 0.081 |
| Diabetes | 4 (4.6) | 4 (100.0) | 0 (0.0) | - | |
| At least two risk factors/other | 38 (43.6) | 21 (55.3) | 17 (44.7) | 1 | |
| Stroke topography | |||||
| Unknown | 35 (40.2) | 19 (54.3) | 16 (45.7) | 1 | |
| Mild cerebral artery | 32 (36.8) | 22 (68.8) | 10 (31.2) | 0.5 [0.1–1.5] | 0.224 |
| Cerebral anterior/Cerebral posterior | 6 (6.9) | 5 (83.3) | 1 (16.7) | 0.2 [0.02–2.2] | 0.190 |
| Other | 14 (16.1) | 3 (21.4) | 11 (78.6) | 4.4 [1.0–18.4]] | 0.036 * |
| Affected hemisphere | |||||
| Left | 56 (64.4) | 23 (41.1) | 33 (58.9) | 1 | |
| Right | 31 (35.6) | 15 (48.4) | 16 (51.6) | 0.7 [0.3–1.8] | 0.510 |
| Functional rehabilitation after stroke (months) | |||||
| <1 | 28 (32.2) | 8 (28.6) | 20 (71.4) | 2.2 [0.7–6.5] | 0.156 |
| 1–3 | 30 (34.5) | 14 (46.7) | 16 (53.3) | 1 | |
| 4–6 | 13 (14.9) | 8 (61.5) | 5 (38.5) | 0.5 [0.1–2.1] | 0.370 |
| >6 | 16 (18.4) | 8 (50.0) | 8 (50.0) | 0.9 [0.3–2.9] | 0.829 |
| Other therapy | |||||
| No | 19 (21.8) | 10 (52.6) | 9 (47.4) | 1.2 [0.4–3.4] | 0.714 |
| Yes | 68 (78.2) | 39 (57.4) | 29 (42.6) | 1 | |
| Modified Rankin Scale | |||||
| <3 | 60 (69.0) | 21 (35.0) | 39 (65.0) | 1 | |
| ≥3 | 27 (31.0) | 17 (63.0) | 10 (37.0) | 0.3 [0.1–0.8] | 0.014 * |
| Functional Ambulatory Classification | |||||
| <4 | 15 (17.2) | 11 (73.3) | 4 (26.7) | 0.2 [0.1–0.8] | 0.019 * |
| ≥4 | 72 (82.7) | 27 (37.5) | 45 (62.5) | 1 | |
| 6MWT (m) | 245.0 ± 178.9 | - | - | ||
| Borg (after 6MWT) | |||||
| ≥12 | 27 (31.0) | 16 (59.3) | 11 (40.7) | 0.4 [0.2–1.0] | 0.049 * |
| <12 | 60 (69.0) | 22 (36.7) | 38 (63.3) | 1 | |
| Home and community factors | |||||
| Living condition | |||||
| Family home | 29 (33.3) | 16 (55.2) | 13 (44.8) | 1.0 [0.4–2.4] | 0.968 |
| Apartment | 5 (5.7) | 4 (80.0) | 1 (20.0) | 0.3 [0.03–2.9] | 0.275 |
| House home | 53 (60.9) | 29 (54.7) | 24 (45.3) | 1 | |
| Living situation | |||||
| Living alone | 4 (4.6) | 3 (75.0) | 1 (25.0) | 0.6 [0.1–5.8] | 0.537 |
| Dependent children | 62 (71.3) | 39 (62.9) | 23 (37.1) | 1 | |
| Living with others | 21 (24.1) | 14 (66.7) | 7 (33.3) | 0.8 [0.3–2.4] | 0.756 |
| Driving status | |||||
| Independent | 34 (49.1) | 22 (64.7) | 12 (35.3) | 1 | |
| Dependent on caregiver | 33 (37.9) | 13 (39.4) | 20 (60.6) | 2.8 [1.0–7.6] | 0.038 * |
| Public transportation | 20 (23.0) | 14 (70.0) | 6 (30.0) | 0.8 [0.2–2.6] | 0.690 |
| Available support | |||||
| No | 13 (14.9) | 9 (69.2) | 4 (30.8) | 0.5 [0.1–1.8] | 0.375 |
| Yes | 74 (85.1) | 40 (54.1) | 34 (45.9) | 1 | |
| Intensity of Activity | Median MET-Minutes/Week (IQR) | Minimum | Maximum |
|---|---|---|---|
| Total physical activity | 985.5 (IQR:2520) | 0 | 56,826 |
| MET-minutes/week per domain | |||
| Total work | 0 (IQR: 0) | 0 | 20,853 |
| Total transport | 231 (IQR:693) | 0 | 5544 |
| Total domestic | 0 (IQR:370) | 0 | 35,280 |
| Total leisure | 0 (IQR:400) | 0 | 6344 |
| MET-minutes/week per domain category | |||
| Total walking activity | 396 (IQR:1254) | 0 | 12,078 |
| Total moderate activity | 120 (IQR:540) | 0 | 55,440 |
| Total vigorous activity | 0 (IQR: 0) | 0 | 7200 |
| Type of Physical Activity | Sex | Age Category | ||||
|---|---|---|---|---|---|---|
| Male (n = 52) | Female (n = 35) | [20–40] (n = 6) | [40–60] (n = 58) | [60–80] (n = 23) | ||
| Intense PA at least 3 days/week, resulting in energy expenditure of at least 1500, N (%) | No | 50 (57.5) | 32 (36.8) | 6 (6.9) | 55 (63.2) | 21 (24.1) |
| Yes | 2 (2.3) | 3 (3.4) | 0 (0.0) | 3 (3.5) | 2 (2.3) | |
| At least 30 min of moderate PA or walking/day for 5 days or more/week, N (%) | No | 26 (29.9) | 25 (28.7) | 3 (3.5) | 33 (37.9) | 15 (17.2) |
| Yes | 26 (29.9) | 10 (11.5) | 3 (3.5) | 25 (28.7) | 8 (9.2) | |
| Low intensity, N (%) | No | 26 (29.9) | 13 (14.9) | 5 (5.7) | 22(25.3) | 12 (13.8) |
| Yes | 26 (29.9) | 22 (25.3) | 3 (3.5) | 31 (35.6) | 14 (16.1) | |
| Level of activity | N (%) | |||||
| Low | 46 (52.9%) | |||||
| Moderate | 36 (41.4%) | |||||
| High | 5 (5.7%) | |||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Noukpo, S.I.; Triccas, L.T.; Bonnechère, B.; Adoukonou, T.; Feys, P.; Kossi, O. Physical Activity Level, Barriers, and Facilitators for Exercise Engagement for Chronic Community-Dwelling Stroke Survivors in Low-Income Settings: A Cross-Sectional Study in Benin. Int. J. Environ. Res. Public Health 2023, 20, 1784. https://doi.org/10.3390/ijerph20031784
Noukpo SI, Triccas LT, Bonnechère B, Adoukonou T, Feys P, Kossi O. Physical Activity Level, Barriers, and Facilitators for Exercise Engagement for Chronic Community-Dwelling Stroke Survivors in Low-Income Settings: A Cross-Sectional Study in Benin. International Journal of Environmental Research and Public Health. 2023; 20(3):1784. https://doi.org/10.3390/ijerph20031784
Chicago/Turabian StyleNoukpo, Sènadé Inès, Lisa Tedesco Triccas, Bruno Bonnechère, Thierry Adoukonou, Peter Feys, and Oyéné Kossi. 2023. "Physical Activity Level, Barriers, and Facilitators for Exercise Engagement for Chronic Community-Dwelling Stroke Survivors in Low-Income Settings: A Cross-Sectional Study in Benin" International Journal of Environmental Research and Public Health 20, no. 3: 1784. https://doi.org/10.3390/ijerph20031784
APA StyleNoukpo, S. I., Triccas, L. T., Bonnechère, B., Adoukonou, T., Feys, P., & Kossi, O. (2023). Physical Activity Level, Barriers, and Facilitators for Exercise Engagement for Chronic Community-Dwelling Stroke Survivors in Low-Income Settings: A Cross-Sectional Study in Benin. International Journal of Environmental Research and Public Health, 20(3), 1784. https://doi.org/10.3390/ijerph20031784







