Impact of the COVID-19 Pandemic on Physical Activity among Mostly Older, Overweight Black Women Living in the Rural Alabama Black Belt
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Assessments
2.3.1. The Impact of COVID-19 on Physical Activity
2.3.2. Physical Activity
2.3.3. Social Cognitive Theory Variables
2.4. Data Analysis
3. Results
3.1. Participant Characteristics
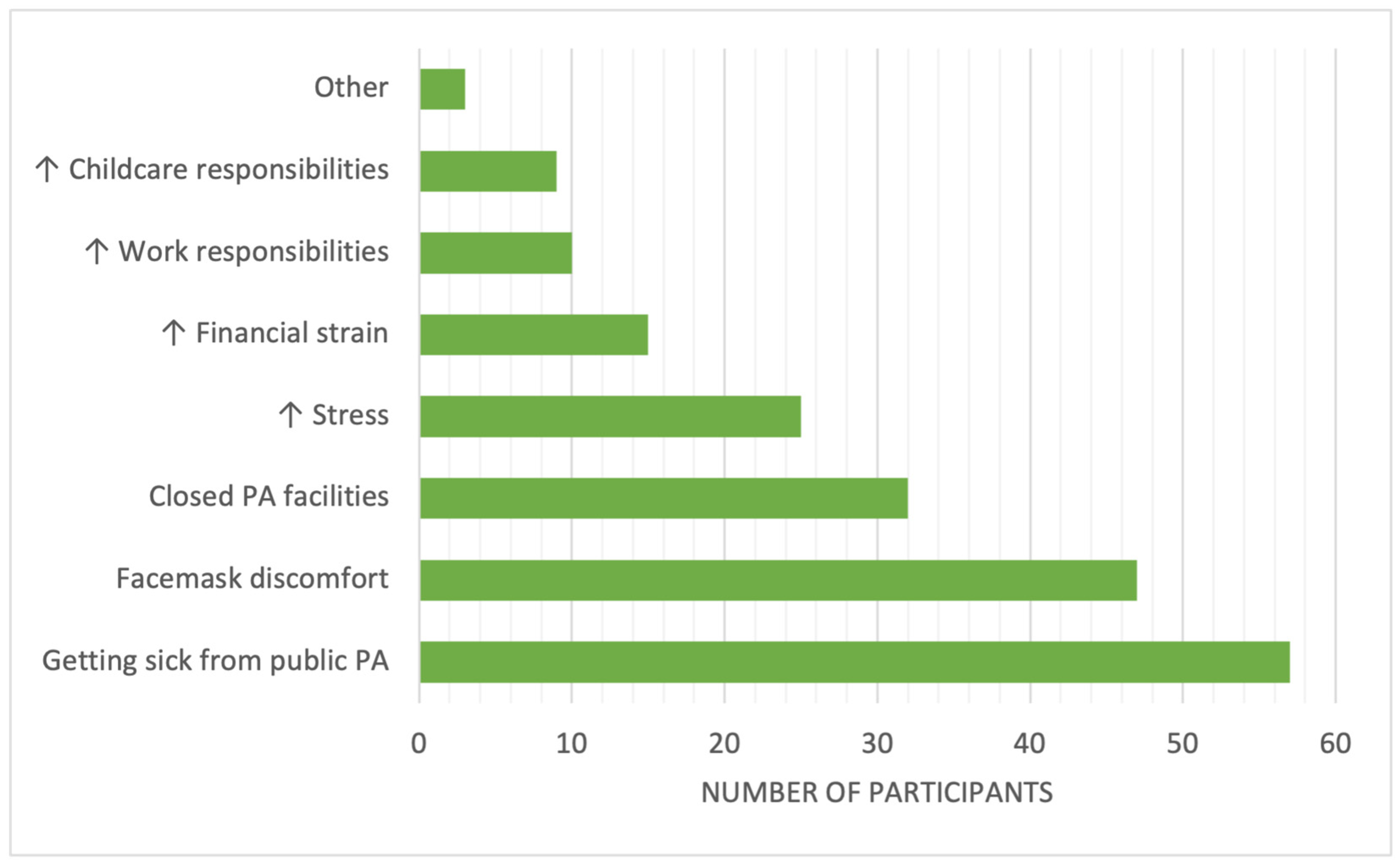
3.2. Impact of COVID-19 on Physical Activity
3.3. Differences in COVID-19’s Impact on Physical Activity by Demographic Characteristics
3.4. Differences in Leisure-Time PA and SCT Constructs by Perceived COVID-19 Impact on PA at 3 Months
3.5. Differences in Leisure-Time PA, SCT Constructs, and Perceived COVID-19 Impact on PA at 3 Months Based on Study Arm
4. Discussion
4.1. Strengths and Limitations
4.2. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Magesh, S.; John, D.; Li, W.T.; Li, Y.; Mattingly-App, A.; Jain, S.; Chang, E.Y.; Ongkeko, W.M. Disparities in COVID-19 Outcomes by Race, Ethnicity, and Socioeconomic Status: A Systematic-Review and Meta-analysis. JAMA Netw. Open 2021, 4, e2134147. [Google Scholar] [CrossRef] [PubMed]
- Hasson, R.; Sallis, J.F.; Coleman, N.; Kaushal, N.; Nocera, V.G.; Keith, N. COVID-19: Implications for Physical Activity, Health Disparities, and Health Equity. Am. J. Lifestyle Med. 2022, 16, 420–433. [Google Scholar] [CrossRef]
- Barr-Anderson, D.J.; Hazzard, V.M.; Hahn, S.L.; Folk, A.L.; Wagner, B.E.; Neumark-Sztainer, D. Stay-at-Home Orders during COVID-19: The Influence on Physical Activity and Recreational Screen Time Change among Diverse Emerging Adults and Future Implications for Health Promotion and the Prevention of Widening Health Disparities. Int. J. Environ. Res. Public Health 2021, 18, 13228. [Google Scholar] [CrossRef] [PubMed]
- Wilke, J.; Mohr, L.; Tenforde, A.S.; Edouard, P.; Fossati, C.; González-Gross, M.; Sánchez Ramírez, C.; Laiño, F.; Tan, B.; Pillay, J.D.; et al. A Pandemic within the Pandemic? Physical Activity Levels Substantially Decreased in Countries Affected by COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 2235. [Google Scholar] [CrossRef] [PubMed]
- Powell, K.E.; King, A.C.; Buchner, D.M.; Campbell, W.W.; DiPietro, L.; Erickson, K.I.; Hillman, C.H.; Jakicic, J.M.; Janz, K.F.; Katzmarzyk, P.T.; et al. The Scientific Foundation for the Physical Activity Guidelines for Americans, 2nd Edition. J. Phys. Act. Health 2018, 16, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Zheng, G.; Qiu, P.; Xia, R.; Lin, H.; Ye, B.; Tao, J.; Chen, L. Effect of Aerobic Exercise on Inflammatory Markers in Healthy Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Front. Aging Neurosci. 2019, 11, 98. [Google Scholar] [CrossRef]
- Chastin, S.F.; Abaraogu, U.; Bourgois, J.G.; Dall, P.M.; Darnborough, J.; Duncan, E.; Dumortier, J.; Pavón, D.J.; McParland, J.; Roberts, N.J.; et al. Effects of Regular Physical Activity on the Immune System, Vaccination and Risk of Community-Acquired Infectious Disease in the General Population: Systematic Review and Meta-Analysis. Sports Med. 2021, 51, 1673–1686. [Google Scholar] [CrossRef] [PubMed]
- Campbell, K.L.; Winters-Stone, K.; Wiskemann, J.; May, A.M.; Schwartz, A.L.; Courneya, K.S.; Zucker, D.; Matthews, C.; Ligibel, J.; Gerber, L.; et al. Exercise Guidelines for Cancer Survivors: Consensus Statement from International Multidisciplinary Roundtable. Med. Sci. Sports Exerc. 2019, 51, 2375–2390. [Google Scholar] [CrossRef]
- Ezzatvar, Y.; Ramírez-Vélez, R.; Izquierdo, M.; Garcia-Hermoso, A. Physical activity and risk of infection, severity and mortality of COVID-19: A systematic review and non-linear dose-response meta-analysis of data from 1 853 610 adults. Br. J. Sports Med. 2022, 56, 1188–1193. [Google Scholar] [CrossRef]
- Fowler, J.H.; Hill, S.J.; Levin, R.; Obradovich, N. Stay-at-home orders associate with subsequent decreases in COVID-19 cases and fatalities in the United States. PLoS ONE 2021, 16, e0248849. [Google Scholar] [CrossRef]
- Umstattd Meyer, M.R.; Perry, C.K.; Sumrall, J.C.; Patterson, M.S.; Walsh, S.M.; Clendennen, S.C.; Hooker, S.P.; Evenson, K.R.; Goins, K.V.; Heinrich, K.M.; et al. Physical Activity-Related Policy and Environmental Strategies to Prevent Obesity in Rural Communities: A Systematic Review of the Literature, 2002–2013. Prev. Chronic Dis. 2016, 13, 150406. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.M.; Gilbert, A.S.; Duncan, D.D.; Wiedenman, E.M. A cross-sectional comparison of physical activity during COVID-19 in a sample of rural and non-rural participants in the US. Int. J. Environ. Res. Public Health 2021, 18, 4991. [Google Scholar] [CrossRef] [PubMed]
- Creech, W.L.; Towner, B.C.; Battista, R.A. Physical Activity Among Adults in Rural Western North Carolina During the COVID-19 Pandemic. Prev. Chronic. Dis. 2022, 19, E74. [Google Scholar] [CrossRef] [PubMed]
- Prior, J.W.; Wong, D.W.S. Exploring different dimensions in defining the Alabama Black Belt. GeoJournal 2022, 87, 1525–1542. [Google Scholar] [CrossRef]
- Dugani, S.B.; Mielke, M.M.; Vella, A. Burden and management of type 2 diabetes in rural United States. Diabetes/Metab. Res. Rev. 2021, 37, e3410. [Google Scholar] [CrossRef]
- Brown, N.I.; Stewart, L.; Rogers, L.Q.; Powell, M.A.; Hardy, C.M.; Baskin, M.L.; Oster, R.A.; Pisu, M.; Demark-Wahnefried, W.; Pekmezi, D. Assessing the built environment, programs, and policies that support physical activity opportunities in the rural Deep South. Prev. Med. Rep. 2023, 33, 102223. [Google Scholar] [CrossRef]
- Robinson, J.C.; Carson, T.L.; Johnson, E.R.; Hardy, C.M.; Shikany, J.M.; Green, E.; Willis, L.M.; Marron Jr, J.V.; Li, Y.; Lee, C.H.; et al. Assessing environmental support for better health: Active living opportunity audits in rural communities in the southern United States. Prev. Med. 2014, 66, 28–33. [Google Scholar] [CrossRef]
- Corley, E.G.; Till, G.; O’Brien, S.; Katsinas, S.G.; Bray, N.J. COVID-19 and Alabama’s Black Belt. Issue Brief No. 55. 30 January 2023. Available online: https://ir.ua.edu/handle/123456789/9928 (accessed on 22 September 2023).
- Brown, N.I.; Powell, M.A.; Baskin, M.; Oster, R.; Demark-Wahnefried, W.; Hardy, C.; Pisu, M.; Thirumalai, M.; Neal, W.N.; Rogers, L.Q.; et al. Design and Rationale for the Deep South Interactive Voice Response System-Supported Active Lifestyle Study: Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2021, 10, e29245. [Google Scholar] [CrossRef]
- Arovah, N.I. The correlates of physical activity during COVID-19 pandemic among Indonesian young adults: A longitudinal study. J. Educ. Health Promot. 2022, 11, 179. [Google Scholar] [CrossRef]
- Thomas, S.; Reading, J.; Shephard, R.J. Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can. J. Sport. Sci. 1992, 17, 338–345. [Google Scholar]
- Godin, G. The Godin-Shephard Leisure-Time Physical Activity Questionnaire. Health Fit. J. Can. 2011, 4, 18–22. [Google Scholar]
- McAuley, E.; Blissmer, B.; Katula, J.; Duncan, T.E. Exercise environment, self-efficacy, and affective responses to acute exercise in older adults. Psychol. Health 2000, 15, 341–355. [Google Scholar] [CrossRef]
- Sallis, J.F.; Grossman, R.M.; Pinski, R.B.; Patterson, T.L.; Nader, P.R. The development of scales to measure social support for diet and exercise behaviors. Prev. Med. 1987, 16, 825–836. [Google Scholar] [CrossRef] [PubMed]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R.; Williams, D.M. Social cognitive mediators of change in a group randomized nutrition and physical activity intervention: Social support, self-efficacy, outcome expectations and self-regulation in the guide-to-health trial. J. Health Psychol. 2010, 15, 21–32. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Zimmerman, S.I.; Orwig, D.; Furstenberg, A.-L.; Magaziner, J. Outcome Expectations for Exercise Scale: Utility and Psychometrics. J. Gerontol. Ser. B 2000, 55, S352–S356. [Google Scholar] [CrossRef]
- Kendzierski, D.; DeCarlo, K.J. Physical Activity Enjoyment Scale: Two Validation Studies. J. Sport Exerc. Psychol. 1991, 13, 50–64. [Google Scholar] [CrossRef]
- Corbett, A.; Wilson, K.E.; Van Horn, A.; Ayers, J.D.; Hurmuz, H.; Aktipis, A. Changes in Physical Activity During the COVID-19 Pandemic: A Mixed Methods Assessment. Int. J. Exerc. Sci. 2022, 16, 327–341. [Google Scholar]
- Zhou, M.; Guo, W. Social factors and worry associated with COVID-19: Evidence from a large survey in China. Soc. Sci. Med. 2021, 277, 113934. [Google Scholar] [CrossRef]
- Gao, H.; Hu, R.; Yin, L.; Yuan, X.; Tang, H.; Luo, L.; Chen, M.; Huang, D.; Wang, Y.; Yu, A.; et al. Knowledge, attitudes and practices of the Chinese public with respect to coronavirus disease (COVID-19): An online cross-sectional survey. BMC Public Health 2020, 20, 1816. [Google Scholar] [CrossRef]
- Allington, D.; McAndrew, S.; Moxham-Hall, V.; Duffy, B. Coronavirus conspiracy suspicions, general vaccine attitudes, trust and coronavirus information source as predictors of vaccine hesitancy among UK residents during the COVID-19 pandemic. Psychol. Med. 2023, 53, 236–247. [Google Scholar] [CrossRef]
- Pickles, K.; Cvejic, E.; Nickel, B.; Copp, T.; Bonner, C.; Leask, J.; Ayre, J.; Batcup, C.; Cornell, S.; Dakin, T.; et al. COVID-19 Misinformation Trends in Australia: Prospective Longitudinal National Survey. J. Med. Internet Res. 2021, 23, e23805. [Google Scholar] [CrossRef] [PubMed]
- Cromer, S.J.; Lakhani, C.M.; Wexler, D.J.; Burnett-Bowie, S.M.; Udler, M.; Patel, C.J. Geospatial Analysis of Individual and Community-Level Socioeconomic Factors Impacting SARS-CoV-2 Prevalence and Outcomes. medRxiv 2020. [Google Scholar] [CrossRef]
- Li, G.H.; Lam, S.K.; Wong, I.C.; Chu, J.K.; Cheung, C.L. Education Attainment, Intelligence and COVID-19: A Mendelian Randomization Study. J. Clin. Med. 2021, 10, 4870. [Google Scholar] [CrossRef] [PubMed]
- Seligman, B.; Ferranna, M.; Bloom, D.E. Social determinants of mortality from COVID-19: A simulation study using NHANES. PLoS Med. 2021, 18, e1003490. [Google Scholar] [CrossRef] [PubMed]
- Sundaram, M.E.; Calzavara, A.; Mishra, S.; Kustra, R.; Chan, A.K.; Hamilton, M.A.; Djebli, M.; Rosella, L.C.; Watson, T.; Chen, H.; et al. Individual and social determinants of SARS-CoV-2 testing and positivity in Ontario, Canada: A population-wide study. CMAJ 2021, 193, E723–E734. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.T.; Testa, C.; Waterman, P.; Krieger, N. Intersectional Inequities in COVID-19 Mortality by Race/Ethnicity and Education in the United States, January 1, 2020–January 31, 2021; Working Paper; Harvard Center for Population and Development Studies: Cambridge, MA, USA, 2021; Volume 21, Number 3. [Google Scholar]
- Concepción-Zavaleta, M.J.; Coronado-Arroyo, J.C.; Zavaleta-Gutiérrez, F.E.; Concepción-Urteaga, L.A. Does level of education influence mortality of SARS-CoV-2 in a developing country? Int. J. Epidemiol. 2021, 49, 2091–2093. [Google Scholar] [CrossRef] [PubMed]
- Drefahl, S.; Wallace, M.; Mussino, E.; Aradhya, S.; Kolk, M.; Brandén, M.; Malmberg, B.; Andersson, G. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden. Nat. Commun. 2020, 11, 5097. [Google Scholar] [CrossRef]
- Chadeau-Hyam, M.; Bodinier, B.; Elliott, J.; Whitaker, M.D.; Tzoulaki, I.; Vermeulen, R.; Kelly-Irving, M.; Delpierre, C.; Elliott, P. Risk factors for positive and negative COVID-19 tests: A cautious and in-depth analysis of UK biobank data. Int. J. Epidemiol. 2020, 49, 1454–1467. [Google Scholar] [CrossRef]
- Larsen, B.; Gilmer, T.; Pekmezi, D.; Napolitano, M.A.; Marcus, B.H. Cost effectiveness of a mail-delivered individually tailored physical activity intervention for Latinas vs. a mailed contact control. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 140. [Google Scholar] [CrossRef][Green Version]
- Larsen, B.; Marcus, B.; Pekmezi, D.; Hartman, S.; Gilmer, T. A Web-Based Physical Activity Intervention for Spanish-Speaking Latinas: A Costs and Cost-Effectiveness Analysis. J. Med. Internet Res. 2017, 19, e43. [Google Scholar] [CrossRef]
- Wegner, L.; Mendoza-Vasconez, A.S.; Mackey, S.; McGuire, V.; To, C.; White, B.; King, A.C.; Stefanick, M.L. Physical activity, well-being, and priorities of older women during the COVID-19 pandemic: A survey of Women’s Health Initiative Strong and Healthy (WHISH) intervention participants. Transl. Behav. Med. 2021, 11, 2155–2163. [Google Scholar] [CrossRef] [PubMed]
- Murukesu, R.R.; Singh, D.K.A.; Shahar, S.; Subramaniam, P. Physical Activity Patterns, Psychosocial Well-Being and Coping Strategies Among Older Persons with Cognitive Frailty of the “WE-RISE” Trial Throughout the COVID-19 Movement Control Order. Clin. Interv. Aging 2021, 16, 415–429. [Google Scholar] [CrossRef] [PubMed]
- Di Lorito, C.; van der Wardt, V.; O’Brien, R.; Gladman, J.; Masud, T.; Harwood, R.H. Impact of COVID-19 lockdown on physical exercise among participants receiving the Promoting Activity, Independence and Stability in Early Dementia (PrAISED) intervention: A repeated measure study. BMC Geriatr. 2022, 22, 605. [Google Scholar] [CrossRef]
- Wijngaards, I.; del Pozo Cruz, B.; Gebel, K.; Ding, D. Exercise frequency during the COVID-19 pandemic: A longitudinal probability survey of the US population. Prev. Med. Rep. 2022, 25, 101680. [Google Scholar] [CrossRef] [PubMed]
- Dunton, G.F.; Wang, S.D.; Do, B.; Courtney, J. Early effects of the COVID-19 pandemic on physical activity locations and behaviors in adults living in the United States. Prev. Med. Rep. 2020, 20, 101241. [Google Scholar] [CrossRef] [PubMed]
- Wunsch, K.; Kienberger, K.; Niessner, C. Changes in Physical Activity Patterns Due to the COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 2250. [Google Scholar] [CrossRef] [PubMed]
- Erwin, P.C.; Mucheck, K.W.; Brownson, R.C. Different Responses to COVID-19 in Four US States: Washington, New York, Missouri, and Alabama. Am. J. Public Health 2021, 111, 647–651. [Google Scholar] [CrossRef]
- Hopkins, S.R.; Dominelli, P.B.; Davis, C.K.; Guenette, J.A.; Luks, A.M.; Molgat-Seon, Y.; Sá, R.C.; Sheel, A.W.; Swenson, E.R.; Stickland, M.K. Face Masks and the Cardiorespiratory Response to Physical Activity in Health and Disease. Ann. Am. Thorac. Soc. 2021, 18, 399–407. [Google Scholar] [CrossRef]
- Scheid, J.L.; Edwards, C.; Seils, M.; West, S.L. Perceived Exertion during Moderate and Vigorous Physical Activity While Mask Wearing: A Quantitative and Qualitative Pilot Study. Int. J. Environ. Res. Public Health 2022, 19, 5698. [Google Scholar] [CrossRef]
| SCT Construct | Tool |
|---|---|
| Self-efficacy | 5-Item Self-Efficacy for Walking Scale [23] |
| Social support | 3-Item Social Support for Exercise Scale [24] |
| Goal setting | 10-Item Exercise Goal Setting Scale [25] |
| Planning | 10-Item Exercise Planning Scale [25] |
| Outcome expectations | 9-Item Outcome Expectations for Exercise Scale [26] |
| Enjoyment | 18-Item Physical Activity Enjoyment Scale [27] |
| Variable | N (%) |
|---|---|
| County | |
| Marengo | 41 (24%) |
| Dallas | 42 (24.6%) |
| Greene | 49 (28.6%) |
| Sumter | 39 (22.8%) |
| Education level | |
| College degree | 94 (55%) |
| No college degree | 77 (45%) |
| Employment status | |
| Full/part time | 76 (44.4%) |
| Unemployed 1 | 95 (55.6%) |
| Living with children 2 | |
| Yes | 55 (32.4%) |
| No | 115 (67.6%) |
| Gender | |
| Male | 16 (9.4%) |
| Female | 155 (90.6%) |
| Marital status | |
| Married | 61 (35.7%) |
| Not married | 110 (64.3%) |
| Annual household income 3 | |
| <$30,000 | 95 (56.5%) |
| ≥$30,000 | 73 (43.5%) |
| Age 4 | |
| ≥60 years old | 88 (51.5%) |
| <60 years old | 83 (48.5%) |
| Race | |
| Black/African American | 168 (98.2%) |
| White | 3 (1.8%) |
| BMI 5 | |
| ≥30 | 130 (76.5%) |
| <30 | 40 (23.5%) |
| Study arm | |
| Intervention | 84 (49.1%) |
| Waitlist control | 87 (50.9%) |
| Variable | Did the COVID-19 Pandemic Make PA More Difficult? | p-Value | |
|---|---|---|---|
| Yes (n = 81) n (%) | No (n = 90) n (%) | ||
| County | |||
| Marengo | 17 (41.5%) | 24 (58.5%) | 0.080 |
| Dallas | 27 (64.3%) | 15 (35.7%) | |
| Greene | 22 (44.9%) | 27 (55.1%) | |
| Sumter | 15 (38.5%) | 22 (61.5%) | |
| Education level | |||
| College degree | 37 (39.4%) | 57 (60.6%) | 0.021 1 |
| No college degree | 44 (57.1%) | 33 (42.9%) | |
| Employment status | |||
| Full/part time | 37 (48.7%) | 39 (51.3%) | 0.758 |
| Unemployed | 44 (46.3%) | 51 (53.7%) | |
| Living with children 1 | |||
| Yes | 32 (58.2%) | 23 (41.8%) | 0.045 1 |
| No | 48 (41.7%) | 67 (58.3%) | |
| Gender | |||
| Male | 2 (12.5%) | 14 (87.5%) | 0.003 2 |
| Female | 79 (51%) | 76 (49%) | |
| Marital status | |||
| Married | 29 (47.5%) | 32 (52.5%) | 0.973 |
| Not married | 52 (47.3%) | 58 (52.7%) | |
| Annual household income | |||
| <$30,000 | 42 (44.2%) | 53 (55.8%) | 0.313 |
| ≥$30,000 | 38 (52.1%) | 35 (48%) | |
| Age | |||
| ≥60 years old | 36 (40.9%) | 52 (59.1%) | 0.082 |
| <60 years old | 45 (54.2%) | 38 (45.8%) | |
| Race 3 | |||
| Black/African American | 80 (47.6%) | 88 (52.4%) | |
| White | 1 (33.3%) | 2 (66.7%) | |
| BMI 4 | |||
| ≥30 | 63 (48.5%) | 67 (51.5%) | 0.509 |
| <30 | 17 (42.5%) | 23 (57.5%) | |
| Study arm | |||
| Intervention | 41 (48.8%) | 43 (51.2%) | 0.711 |
| Waitlist control | 40 (46%) | 47 (54%) | |
| Variable | Less Active (n = 85) | More Active (n = 31) | No Change in PA (n = 55) | |
|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | p-Value | |
| Leisure-time PA (min/week) | 90.6 (81.1) | 177.0 (97) | 111.3 (92.4) | <0.001 * |
| Social support 1 | 8.3 (2.7) | 8.9 (3.7) | 7.9 (3.3) | 0.377 |
| Outcome expectations 2 | 4.0 (0.7) | 4.4 (0.5) | 3.9 (0.9) | 0.023 ** |
| PA enjoyment 3 | 3.7 (0.9) | 3.9 (0.9) | 3.8 (0.9) | 0.527 |
| Goal setting 4 | 2.7 (1.1) | 3.2 (1.1) | 2.6 (1.3) | 0.042 *** |
| Planning 5 | 2.7 (0.6) | 2.9 (0.7) | 2.7 (0.8) | 0.346 |
| Walking self-efficacy 6 | 52.8 (31.4) | 64.5 (28.2) | 53.3 (31.6) | 0.174 |
| Intervention | Wait-List Control | |||||
|---|---|---|---|---|---|---|
| Variable | Less Active (n = 40) | More Active (n = 22) | No Change in PA (n = 22) | Less Active (n = 45) | More Active (n = 9) | No Change in PA (n = 33) |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |
| Leisure-time PA (min/week) | 133.5 (96.2) *,+ | 193.1 (105.3) *,+ | 111.3 (92.4) * | 77.6 (85.3) | 137.7 (61.2) | 96.5 (88.3) |
| Social support 1 | 8.9 (3.4) | 9.1 (3.5) | 7.9 (3.3) | 8.1 (2.2) | 8.3 (4.4) | 7.3 (3.1) |
| Outcome expectations 2 | 4.0 (1) | 4.4 (0.5) | 3.9 (0.9) | 4.0 (0.8) | 4.3 (0.4) | 3.9 (0.8) |
| PA enjoyment 3 | 4.0 (0.8) | 4.2 (0.7) | 3.8 (0.9) | 3.7 (0.9) | 3.3 (1.1) | 3.7 (0.9) |
| Goal setting 4 | 2.9 (1.3) | 3.3 (0.9) | 2.6 (1.3) | 2.7 (1.1) | 3.0 (1.4) | 2.4 (1.2) |
| Planning 5 | 2.8 (0.9) | 3.0 (0.7) | 2.7 (0.8) | 2.6 (0.7) | 2.5 (0.7) | 2.6 (0.8) |
| Walking self-efficacy 6 | 58.2 (32.8) | 67.4 (26.3) | 53.3 (31.6) | 51.0 (31.7) | 57.4 (33) | 50.1 (30.8) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Neal, W.N.; Schleicher, E.A.; Baron, K.; Oster, R.A.; Brown, N.I.; Demark-Wahnefried, W.; Pisu, M.; Baskin, M.L.; Parrish, K.B.; Cole, W.W.; et al. Impact of the COVID-19 Pandemic on Physical Activity among Mostly Older, Overweight Black Women Living in the Rural Alabama Black Belt. Int. J. Environ. Res. Public Health 2023, 20, 7180. https://doi.org/10.3390/ijerph20247180
Neal WN, Schleicher EA, Baron K, Oster RA, Brown NI, Demark-Wahnefried W, Pisu M, Baskin ML, Parrish KB, Cole WW, et al. Impact of the COVID-19 Pandemic on Physical Activity among Mostly Older, Overweight Black Women Living in the Rural Alabama Black Belt. International Journal of Environmental Research and Public Health. 2023; 20(24):7180. https://doi.org/10.3390/ijerph20247180
Chicago/Turabian StyleNeal, Whitney N., Erica A. Schleicher, Kerri Baron, Robert A. Oster, Nashira I. Brown, Wendy Demark-Wahnefried, Maria Pisu, Monica L. Baskin, Kelsey B. Parrish, William Walker Cole, and et al. 2023. "Impact of the COVID-19 Pandemic on Physical Activity among Mostly Older, Overweight Black Women Living in the Rural Alabama Black Belt" International Journal of Environmental Research and Public Health 20, no. 24: 7180. https://doi.org/10.3390/ijerph20247180
APA StyleNeal, W. N., Schleicher, E. A., Baron, K., Oster, R. A., Brown, N. I., Demark-Wahnefried, W., Pisu, M., Baskin, M. L., Parrish, K. B., Cole, W. W., Thirumalai, M., & Pekmezi, D. W. (2023). Impact of the COVID-19 Pandemic on Physical Activity among Mostly Older, Overweight Black Women Living in the Rural Alabama Black Belt. International Journal of Environmental Research and Public Health, 20(24), 7180. https://doi.org/10.3390/ijerph20247180







