Abstract
Background: This study aimed to estimate absenteeism costs and identify their predictors in non-hospitalized patients in Sweden. Methods: This cross-sectional study’s data were derived from the longitudinal project conducted at Uppsala University Hospital. The mean absenteeism costs due to COVID-19 were calculated using the human capital approach, and a Poisson regression analysis was employed to determine predictors of these costs. Results: The findings showed that the average absenteeism cost due to COVID-19 was USD 1907.1, compared to USD 919.4 before the pandemic (p < 0.001). Notably, the average absenteeism cost for females was significantly higher due to COVID-19 compared to before the pandemic (USD 1973.5 vs. USD 756.3, p = 0.001). Patients who had not fully recovered at the 12-month follow-up exhibited significantly higher costs than those without symptoms at that point (USD 3389.7 vs. USD 546.7, p < 0.001). The Poisson regression revealed that several socioeconomic factors, including age, marital status, country of birth, educational level, smoking status, BMI, and occupation, along with COVID-19-related factors such as severity at onset, pandemic wave, persistent symptoms at the follow-up, and newly introduced treatment for depression after the infection, were significant predictors of the absenteeism costs. Conclusions: Our study reveals that the mean absenteeism costs due to COVID-19 doubled compared to the year preceding the pandemic. This information is invaluable for decision-makers and contributes to a better understanding of the economic aspects of COVID-19.
1. Introduction
The COVID-19 pandemic, caused by the SARS-CoV-2 virus, has emerged as a global health crisis, profoundly impacting all aspects of life, including economic conditions [1]. The economic implications of COVID-19 encompass both direct medical expenses and indirect costs associated with factors such as illness, premature mortality, and absenteeism [2,3]. Regarding the expenses tied to hospitalization, studies conducted in the USA estimated that the median hospital stay length per patient was 5 days, while average costs of hospitalization per patient were USD 3045, with a median cost of USD 12,046 [4,5]. Another report from China indicated that the mean length of hospital stay was 16.26 days, and the mean expenditure for hospitalization of moderate COVID-19 cases amounted to USD 1177. Additionally, each additional year of the patient’s age corresponded to a 0.9% increase in total hospital expense [6].
In Greece, a study determined that direct costs constituted 18.8% of the overall costs, and, during the period from February to May 2020, 80% of all COVID-19-related cases were attributed to healthcare personnel absenteeism [7]. A study in Iran, focusing on patients requiring hospitalization followed by home recovery, found that COVID-19 directly accounted for 32% of the total economic burden, leaving the remaining proportion to indirect costs, primarily driven by absenteeism [8].
Several studies have showed a rise in sick leave duration and frequency during the pandemic in comparison to the pre-pandemic periods [9,10,11]. However, there are still limited studies on absenteeism due to COVID-19. These few existing studies, for example, from Greece, Iran, and Qatar, based on healthcare workers only, have highlighted the elevated and unpredictable rates of workforce absenteeism associated with COVID-19 [7,12,13]. Notably, absenteeism acts as a critical factor, resulting in reduced productivity, increased expenses, overload of other workers, and potential repercussion on the quality of care delivered [14]. Consequently, a comprehensive exploration of absenteeism costs is essential to grasp the complete economic dimensions of COVID-19, particularly in the post-pandemic period, and to offer valuable insights to aid policymakers in economic recovery efforts [15].
In addition, no prior studies have endeavored to estimate absenteeism costs in Sweden. To address this gap, our study aimed to compute absenteeism costs and identify their predictors among non-hospitalized healthcare workers and other occupational groups with laboratory-confirmed COVID-19, spanning from 10 March to 31 December 2020 in Sweden.
2. Materials and Methods
2.1. Study Design
The data for this cross-sectional study were derived from the longitudinal project titled “COMBAT post-COVID”, which was conducted at Uppsala University Hospital and detailed in other publications [16,17,18]. The project aimed to monitor non-hospitalized patients with COVID-19 who were receiving follow-up care at the outpatient infectious disease department. The study included data collected from all symptomatic adult patients (18 years old or older) diagnosed with COVID-19 at the Department of Infectious Diseases between 10 March 2020 and 31 December 2020. The categorization of pandemic waves in this study was established by the Swedish Board of Health and Welfare (Socialstyrelsen, Stockholm, Sweden) based on the number of active cases: wave-1 spanning from 10 March 2020 to 30 September 2020 and wave-2 spanning from 1 October 2020 to 30 December 2020 [19]. Patients were eligible for inclusion if they possessed a valid diagnostic test result indicating a positive polymerase chain reaction (PCR) test for SARS-CoV-2 by nasopharyngeal swab, thereby confirming their COVID-19 diagnosis.
A survey was administered to the patients within a time span of 45 to 51 weeks, approximately equivalent to 12 months, following their diagnosis of COVID-19. The distribution of questionnaires primarily occurred via email, facilitated by the use of REDCap [20]. In cases where patients lacked an email contact, the questionnaire was dispatched through traditional postal services to their residential addresses, accompanied by a prepaid return envelope. For those who received the email-based survey, up to two reminders were dispatched at intervals of one and two weeks following the initial contact. Conversely, patients who were sent the standard postal questionnaire did not receive additional reminders due to the constraints of the 12-month post-COVID-19 timeframe. The survey was conducted between 10 March 2021 and 15 January 2022. A total of 401 non-hospitalized adult patients with a confirmed diagnosis of COVID-19 responded to the questionnaire, constituting 56% of the eligible participants, as illustrated in Figure 1.
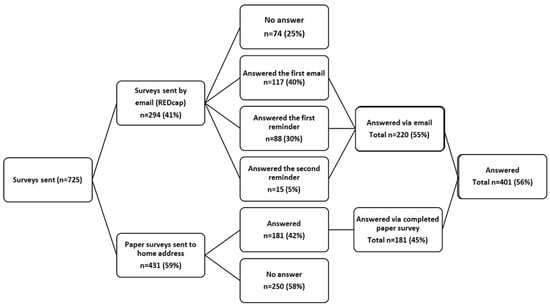
Figure 1.
The flow chart of the study population.
All responders provided digital or written informed consent when filling out the questionnaire. The study was approved by the institutional ethics committee of Uppsala University Hospital (EPN number 2020-05707) and conducted in accordance with the Helsinki Declaration.
2.2. Absenteeism Costs
The outcome measure focused on assessing absenteeism costs. These costs were quantified using the number of self-reported sick leave days attributed to COVID-19 and those occurring a year prior to the pandemic (referred to as “pre-COVID-19”, spanning from January 2019 to February 2020). These sick leave days were utilized to compute the respective costs associated with absenteeism or loss of productivity due to COVID-19 and in the period preceding the pandemic.
The computation of these costs was achieved through the application of the human capital approach. This methodology involves assigning a monetary value to the productivity lost due to factors such as illness or premature mortality with the aim of reflecting an individual’s contribution to the overall national productivity [21]. As per this approach, the monetary value of lost productivity resulting from missed workdays is deemed equivalent to an individual’s daily wage multiplied by the number of days absent from work.
The calculation of lost productivity cost attributed to COVID-19 is expressed in US dollars. To determine the wage value for patients who experienced sick leave, the minimum wages based on the statistics from Sweden were employed [22]. Specifically, for patients with sick leave days, the average monthly salary for Sweden in 2020, which amounted to USD 4125, was utilized to estimate the daily wage value. Consequently, the value of a daily wage was computed as USD 138. All reported costs are standardized to constant 2022 US dollars, utilizing purchasing power parities (PPP) for accuracy and comparability.
2.3. Other Included Variables
In this study, various relevant predictors of lost productivity costs attributed to COVID-19 were taken into consideration. These predictors encompassed: gender (male or female); age (divided into four groups: up to 30 years old, 31 to 40 years old, 41 to 50 years old, and over 50 years old); marital status (married/in a partnership or single/divorced/widow(er)); country of birth (divided into four groups: born in Sweden with Swedish parents, born in Sweden with one Swedish parent, born in Sweden but parents not born in Sweden, not born in Sweden); highest educational level (categorized as having received at least 3 years of university education or no university education); smoking status (grouped into three categories: current smokers, former smokers, and never smokers); snuff use (yes or no); Body Mass Index, BMI, in kg/m2 (based on self-reported weight and length and divided into: underweight: <18.5; normal: 18.5–25.9; overweight: 25.0–29.9; and obese 30); pre-existing comorbidity (included hypertension, heart disease, hypo/hyperthyroidism, diabetes type 2, lung disease, cancer, depression/anxiety; grouped as no or one or at least two comorbidities); self-reported severity of COVID-19 onset (mild, moderate, or severe); recovery equal to no self-reported persisting symptoms at 12-month follow-up (yes or no); job status (employed/currently working or on parental leave or not employed, including looking for the job, retired, and student); occupation (classified into healthcare workers with patient contact, including medical doctor, nurse, assistant nurse, physiotherapist, psychologist, occupational therapist, or healthcare workers without patient contact, including managers, and other occupations not related to healthcare, including manual workers and managers); working hours/percent of average 40 h week (divided into 81–100%, 50–80%, and <50%); pandemic wave (first or second); and self-reported information on newly introduced treatment for depression/anxiety (including psychological treatment or medication) after contracting COVID-19.
2.4. Statistical Analysis
Categorical variables are presented by providing the number and proportion, while continuous variables are presented with the mean and standard deviation (SD). Absenteeism costs attributed to COVID-19 were computed based on variables during and before the COVID-19 pandemic. A t-test analysis was employed to examine the differences in expenses after and before the COVID-19 pandemic. Subsequently, Poisson regression was utilized to explore the factors influencing absenteeism costs resulting from COVID-19 [23,24]. The decision to use Poisson regression was primarily driven by the nature of the outcome variable, which involved count data derived from multiplying the number of days by a specific value. Additionally, the dataset exhibited a significant presence of zero values, with 75% of patients in this study demonstrating no costs. This led to a skewed distribution of the dependent variable.
In Poisson regression, the dependent variable (Y) is limited to non-negative integer values, representing counted objects dependent on specific characteristics (x). The probability of Y, often referred to as the “number of events”, follows a Poisson distribution and is given by:
where µ represents the average number of events in the Poisson distribution. This distribution is commonly employed to model infrequent occurrences within certain time intervals. In the Poisson regression model, the logarithmic function used is ln(μi) = ηi. This allows the relationship function to be expressed in Equations (2) and (3) as follows:
where i is the observation unit i = 1,2,…, n, and β is a vector of coefficients associated with Xi. A p-value < 0.05 was defined as statistically significant. All statistical analyses were performed using Stata 14 (Stata Corp., College Station, TX, USA).
Ln µi = β0 + β1X1i + β2X2i + … + βkXki
µi = exp (XiTβ) = exp (β0 + β1X1i + β2X2i + … + βkXki)
3. Results
3.1. The Study Patients’ Characteristics
The human capital approach calculated costs for a working population, and 42 study patients that were not employed due to studies (n = 6), retirement (n = 18), job seeking (n = 13), or being on parental leave (n = 5) were excluded from the cost estimation analysis. There were, in total, 359 non-hospitalized patients working while answering the survey at the 12-month follow-up after COVID-19. The sociodemographic and clinical characteristics of all the responders are presented in Table 1. Approximately 73.4 of the study patients were female. The mean age of the patients was 43.46 years, and 81% were born in Sweden. There were 52.3% who had reported persisting symptom(s) one year after contracting COVID-19. Of the responders, 89.3% were employed/in current work. The total number of missed workdays before and during the COVID-19 pandemic was 2332 (mean = 6.7) and 4823 (mean = 13.8), respectively.

Table 1.
Characteristics of patients (n = 359) included in the study.
3.2. The Lost Productivity Cost (USD) Due to Absenteeism
Table 2 presents the mean lost productivity costs attributed to absenteeism due to COVID-19 during both wave-1 and wave-2 of the pandemic, as well as during the year before the pandemic, in Sweden. The average cost of absenteeism was notably higher for females and, to a lesser extent, for males during the pandemic in comparison to the pre-pandemic period. However, the mean absenteeism costs due to COVID-19 did not exhibit a significant difference between genders. Among the study participants, those aged 41 to 50 experienced the highest average cost of sick leave due to COVID-19 in comparison to other age groups. Healthcare workers with patient contact and also other occupations had a significant increase in absenteeism costs at one-year follow-up. Then, working between 80 and 100% of average working hours (40 h/week), having no coexisting comorbidity, and never having used nicotine products such as cigarette and snuff were associated with higher productivity loss due to COVID-19 absenteeism.

Table 2.
The lost productivity cost in USD due to absenteeism based on self-reported sick leave days due to COVID-19 and those a year before the pandemic reported by the study patients (n = 359).
Patients without a university education faced significantly higher mean absenteeism costs during the pandemic than they did before. Participants who had not fully recovered at the 12-month follow-up after contracting COVID-19, those who reported severe symptoms at the onset of COVID-19, and those with newly introduced treatment for depression/anxiety after the infection incurred significantly higher absenteeism costs.
3.3. The Predictors of the Higher Absenteeism Costs Due to COVID-19
The Poisson regression identified various factors that predict the occurrence of absenteeism costs due to COVID-19 in non-hospitalized patients, Table 3. These factors included socioeconomic variables such as gender, age, marital status, country of birth, educational level, occupation, BMI, and smoking status. Additionally, COVID-19-related variables such as severity of infection at onset, pandemic wave, persistent symptoms at the follow-up, and newly introduced treatment for depression after COVID-19 were significant predictors. For example, absenteeism costs were, on average, 7.5% higher in men than in women.

Table 3.
Poisson regression results of the absenteeism costs in the study patients (n = 359).
4. Discussion
The primary findings of this study underscore the substantial increase in mean absenteeism caused by COVID-19 within the timeframe of 10 March to 31 December 2020, as it surpassed twofold when contrasted with the year preceding the pandemic for non-hospitalized patients in Sweden. We showed that the total costs of absenteeism due to COVID-19 were USD 665,574. Our study demonstrated that being female, being between 41 and 50 years old, lacking university education, experiencing more severe COVID-19 symptoms at onset, and enduring persisting symptoms at the one-year follow-up were all significantly linked to heightened absenteeism costs due to COVID-19, as compared to the pre-pandemic period. Furthermore, our research identified various socioeconomic factors, including gender, age, marital status, country of birth, educational level, smoking status, BMI, and occupation, as well as COVID-19-related factors such as severity at onset, pandemic wave, persistent symptoms at follow-up, and newly introduced treatment for depression after the infection, as significant predictors of absenteeism costs.
In accordance with our results, healthcare personnel with patient contact reported lower mean sick leave days due to COVID-19 compared to other occupational groups (12.7 vs. 20.7 days). The previous studies on absenteeism rate due to COVID-19 addressing occupational groups were based only on healthcare personnel and are difficult to compare with our findings due to differences in methodology used to assess absenteeism. However, research from Iran conducted between February and September 2020 revealed that the average duration of absenteeism due to COVID-19 was 16 days, accompanied by an average cost of USD 671.4 per patient [12]. Then, a study conducted in Greece between February and May 2020 demonstrated that the average absenteeism duration due to COVID-19 was 25.8 days [7]. To our knowledge, our study is the first that evaluated absenteeism due to COVID-19 in occupational groups other than healthcare occupational groups. The higher duration of sick leave in other occupational groups might be related to healthcare personnel, despite having higher vulnerability to the infection, being more prone to using protection equipment and keeping physical distance, as recommended from the early days of the pandemic [25].
Our study demonstrated that the mean absenteeism costs due to COVID-19, as compared to costs prior to the pandemic, were notably higher among females compared to males. Furthermore, middle-aged patients exhibited higher costs when contrasted with individuals in other age groups. This observation aligns harmoniously with findings from studies conducted in Iran, Qatar, and Greece, which primarily focused on healthcare workers with milder infections [7,12,13]. Likewise, studies conducted prior to the pandemic indicated that women in Sweden tend to experience higher rates of sickness absence compared to men [26]. Additionally, international studies have suggested that women face lower odds of returning to work following various health conditions [27,28].
Furthermore, our findings revealed a positive correlation between age and the likelihood of incurring absenteeism costs due to COVID-19, with patients between 41 and 50 years old incurring 183% greater costs than those under 30 years, aligning with findings from prior studies [8,12]. A study involving hospitalized patients further illustrated that, with each additional year of a patient’s age, total hospital expenses increased by 0.9% [6].
Furthermore, our analysis indicated that study participants without a university education experienced higher absenteeism costs due to COVID-19, as compared to costs prior to the pandemic, than those with a university education. This finding harmonizes with a previous international study where lower education was associated with extended sick leave due to various diagnoses [29,30]. Higher education has been linked to elevated socioemotional status and a propensity for overall better health, increased life expectancy, and higher job satisfaction [31].
In line with a previous study from Iran, we found that increasing age predicted absenteeism costs due to COVID-19 or increased these costs [12]. Similarly to the study from Qatar, we found that COVID-19-related absenteeism increased during the first wave of the pandemic compared to the pre-COVID-19 period. Moreover, the absenteeism rate was even higher in the second wave compared to the first wave [13]. In addition, we showed that not being fully recovered at the follow-up was a factor associated with absenteeism costs. This finding aligns with a study conducted in China; however, this was a study on direct costs of hospitalization, which reported that healthcare costs for severe cases were 9.5 times higher than for non-severe cases [32]. Then, the previous research showed that coexisting depression/anxiety increases the risk of prolonged sickness absence [9,10,11], and it is in line with our study, where we found that newly introduced treatment for depression/anxiety was a predictor of absenteeism costs.
The novelty of our study is that no previous study on absenteeism costs due to COVID-19 has been conducted in Sweden. In addition, no previous existing studies in the area on non-hospitalized patients considered occupations other than those in healthcare. The strength of our study is that we assessed productivity losses both before and during the pandemic and evaluated predictors of absenteeism costs including several clinical and sociodemographic variables. By using the Poisson regression, we could demonstrate which of the variables predict absenteeism costs. This multi-faceted methodology enhanced the depth and accuracy of our findings.
However, this study had several limitations. We faced the challenge of not having access to information about patients’ salary or about whether they worked full time or part time. Additionally, we lacked individual wage data for each study participant. Instead, we employed the minimum wages per person employed in Sweden in 2020 as a proxy for the daily wage value. Additionally, it is important to note that our study cohort consisted of a relatively small number of participants, with the majority being healthcare personnel and female. This composition could potentially limit the generalizability of our findings. Previous research has consistently demonstrated that healthcare personnel are placed in a high-risk category for COVID-19, subsequently heightening their susceptibility to sick leave due to the infection [17,33]. This occupational category skew is largely due to the prioritization of testing for SARS-CoV-2 in the initial months of the pandemic, with healthcare workers being at the forefront in many countries. Furthermore, our cost estimates could potentially be underestimated due to the exclusion of hospitalized patients from our analysis. Consequently, the derived results from our absenteeism cost estimates might not be readily applicable to the entire Swedish population. Then, our study drew on self-reported retrospective data, encompassing factors such as the duration of sick leave, the severity of disease onset, and the persistence of symptoms at the one-year follow-up. It is important to note that this retrospective nature introduces the potential for reporting bias.
5. Conclusions
Our study reveals that absenteeism costs due to non-hospitalized COVID-19 can be significant, with an overall increase of more than twofold during the two first waves of the pandemic compared to the pre-pandemic period. Moreover, our findings emphasize the pivotal role of various socioeconomic factors including gender, age, marital status, country of birth, educational level, occupation, smoking status, and BMI, as well as COVID-19-related factors such as severity of COVID-19 at onset, pandemic wave, persistent symptoms at follow-up, and newly introduced treatment for depression after COVID-19, as significant predictors of absenteeism costs. These results not only underscore the significance of accounting for absenteeism costs when assessing the economic ramifications of COVID-19 but also suggest that strategies to mitigate these costs should be prioritized by policymakers.
Author Contributions
Conceptualization, M.A.K. and H.J.; methodology, M.A.K. and A.F.; software, A.F.; validation, M.A.K., H.J. and S.L.; formal analysis, M.A.K. and A.F.; investigation, M.A.K., H.J. and S.L.; resources, M.A.K.; data curation, A.F. and M.A.K.; writing—original draft preparation, A.F.; writing—review and editing, M.A.K., S.L. and H.J.; visualization, M.A.K.; supervision, M.A.K., project administration, M.A.K.; funding acquisition, M.A.K. All authors have read and agreed to the published version of the manuscript.
Funding
We acknowledge Åke Wiberg Stiftelsen (stipendium M22-0119 and M21-0080), Lars Hiertas Minne Stiftelsen (stipendium F02021-0144 and F02022-0098), Sven and Dagmar Saléns Stiftelse (stipendium 2022), and Tore Nilsons Stiftelsen (stipendium 2021-00935) for support.
Institutional Review Board Statement
All responders provided digital or written informed consent when filling out the questionnaire. The study was approved by the institutional ethics committee of Uppsala University Hospital (EPN number 2020-05707) and conducted in accordance with the Helsinki Declaration.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data can be made available on demand.
Conflicts of Interest
All authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
References
- Anderson, R.M.; Heesterbeek, H.; Klinkenberg, D.; Hollingsworth, T.D. How will country-based mitigation measures influence the course of the COVID-19 epidemic? Lancet 2020, 395, 931–934. [Google Scholar] [CrossRef] [PubMed]
- Ohsfeldt, R.L.; Choong, C.K.; Mc Collam, P.L.; Abedtash, H.; Kelton, K.A.; Burge, R. Inpatient Hospital Costs for COVID-19 Patients in the United States. Adv. Ther. 2021, 38, 5557–5595. [Google Scholar] [CrossRef] [PubMed]
- Shakor, J.K.; Isa, R.A.; Babakir-Mina, M.; Ali, S.I.; Hama-Soor, T.A.; Abdulla, J.E. Health related factors contributing to COVID-19 fatality rates in various communities across the world. J. Infect. Dev. Ctries. 2021, 15, 1263–1272. [Google Scholar] [CrossRef] [PubMed]
- Di Fusco, M.; Shea, K.M.; Lin, J.; Nguyen, J.L.; Angulo, F.J.; Benigno, M.; Malhotra, D.; Emir, B.; Sung, A.H.; Hammond, J.L. Health outcomes and economic burden of hospitalized COVID-19 patients in the United States. J. Med. Econ. 2021, 24, 308–317. [Google Scholar] [CrossRef] [PubMed]
- Bartsch, S.M.; Ferguson, M.C.; McKinnell, J.A.; O’Shea, K.J.; Wedlock, P.T.; Siegmund, S.S.; Lee, B.Y. The Potential Health Care Costs And Resource Use Associated With COVID-19 In The United States: A simulation estimate of the direct medical costs and health care resource use associated with COVID-19 infections in the United States. Health Aff. 2020, 39, 927–935. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Chen, L.; Shi, L. Determinants of Hospitalization Costs among Moderate Cases of COVID-19. INQUIRY J. Health Care Organ. Provis. Financ. 2022, 59, 00469580211059483. [Google Scholar] [CrossRef]
- Maltezou, H.; Giannouchos, T.; Pavli, A.; Tsonou, P.; Dedoukou, X.; Tseroni, M.; Papadima, K.; Hatzigeorgiou, D.; Sipsas, N.; Souliotis, K. Costs associated with COVID-19 in healthcare personnel in Greece: A cost-of-illness analysis. J. Hosp. Infect. 2021, 114, 126–133. [Google Scholar] [CrossRef]
- Rajabi, M.; Rezaee, M.; Omranikhoo, H.; Khosravi, A.; Keshmiri, S.; Ghaedi, H.; Pourreza, A. Cost of Illness of COVID-19 and Its Consequences on Health and Economic System. Inquiry 2022, 59, 469580221144398. [Google Scholar] [CrossRef]
- Grandi, J.L.; Silva, C.O.; Barbosa, D.A. Work absences among hospital cleaning staff during the SARS-CoV-2 (COVID-19) pandemic. Rev. Bras. Med. Trab. 2022, 20, 45–54. [Google Scholar] [CrossRef]
- Challener, D.W.; Breeher, L.E.; Frain, J.; Swift, M.D.; Tosh, P.K.; O’Horo, J. Healthcare personnel absenteeism, presenteeism, and staffing challenges during epidemics. Infect. Control Hosp. Epidemiol. 2021, 42, 388–391. [Google Scholar] [CrossRef]
- Palstam, A.; Westerlind, E.; Sunnerhagen, K.S.; Persson, H.C. Recurrent sick leave after COVID-19: Investigating the first wave of the pandemic in a comprehensive Swedish registry-based study. BMC Public Health 2021, 21, 1914. [Google Scholar] [CrossRef] [PubMed]
- Faramarzi, A.; Javan-Noughabi, J.; Tabatabaee, S.S.; Najafpoor, A.A.; Rezapour, A. The lost productivity cost of absenteeism due to COVID-19 in health care workers in Iran: A case study in the hospitals of Mashhad University of Medical Sciences. BMC Health Serv. Res. 2021, 21, 1169. [Google Scholar] [CrossRef] [PubMed]
- Al-Nuaimi, A.A.; Abdeen, S.; Abed Alah, M.; AlHajri, S.; Semaan, S.; Al-Kuwari, M.G. Sickness absenteeism among primary health care workers in Qatar before and during the COVID-19 pandemic. J. Occup. Med. Toxicol. 2023, 18, 3. [Google Scholar] [CrossRef] [PubMed]
- Garbin, A.J.I.; Nascimento, C.; Zacharias, F.C.M.; Garbin, C.A.S.; Moimaz, S.A.S.; Saliba, N.A. Sickness absenteeism of Primary Health Care professionals before and during the COVID-19 pandemic. Rev. Bras. Enferm. 2022, 75 (Suppl. S1), e20220028. [Google Scholar] [CrossRef]
- Larkin, H.D. COVID-19 Health Policies and Economies in Nordic Countries. JAMA 2022, 328, 1029. [Google Scholar] [CrossRef]
- Kisiel, M.A.; Janols, H.; Nordqvist, T.; Bergquist, J.; Hagfeldt, S.; Malinovschi, A.; Svartengren, M. Predictors of post-COVID-19 and the impact of persistent symptoms in non-hospitalized patients 12 months after COVID-19, with a focus on work ability. Ups. J. Med. Sci. 2022, 127. [Google Scholar] [CrossRef]
- Kisiel, M.A.; Nordqvist, T.; Westman, G.; Svartengren, M.; Malinovschi, A.; Janols, H. Patterns and predictors of sick leave among Swedish non-hospitalized healthcare and residential care workers with COVID-19 during the early phase of the pandemic. PLoS ONE 2021, 16, e0260652. [Google Scholar] [CrossRef]
- Kisiel, M.A.; Lee, S.; Malmquist, S.; Rykatkin, O.; Holgert, S.; Janols, H.; Janson, C.; Zhou, X. Clustering Analysis Identified Three Long COVID Phenotypes and Their Association with General Health Status and Working Ability. J. Clin. Med. 2023, 12, 3617. [Google Scholar] [CrossRef]
- Socialstyrelse. Analys av Första och Andra COVID-19 Vågen (The Analysis of the First and Second Wave of COVID-19 in Sweden). 2021. Available online: https://www.socialstyrelsen.se/globalassets/sharepoint-dokument/artikelkatalog/ovrigt/2021-5-7371.pdf (accessed on 19 August 2019).
- Lyon, J.A.; Garcia-Milian, R.; Norton, H.F.; Tennant, M.R. The use of Research Electronic Data Capture (REDCap) software to create a database of librarian-mediated literature searches. Med. Ref. Serv. Q. 2014, 33, 241–252. [Google Scholar] [CrossRef]
- Zhang, W.; Bansback, N.; Anis, A.H. Measuring and valuing productivity loss due to poor health: A critical review. Soc. Sci. Med. 2011, 72, 185–192. [Google Scholar] [CrossRef]
- Statystic Sweden. (SCB) Salary Structures, Whole Economy 1992–2022. Available online: https://www.scb.se/en/finding-statistics/statistics-by-subject-area/labour-market/wages-salaries-and-labour-costs/salary-structures-whole-economy/ (accessed on 2 September 2023).
- Verbeek, M. A Guide to Modern Econometrics, 5th ed.; John Wiley & Son: Hoboken, NJ, USA, 2017. [Google Scholar]
- Otok, B.W.; Rachmawati, D.S.; Purhadi; Purnami, S.W.; Mahpolah, M. Poisson Regression Modeling of Diarrhea Events in Pasuruan Regency with Maximum Likelihood Estimates and Generalized Method Moment. Int. J. Prev. Med. 2021, 12, 103. [Google Scholar] [CrossRef] [PubMed]
- Huy, N.T.; Chico, R.M.; Huan, V.T.; Shaikhkhalil, H.W.; Uyen, V.N.T.; Qarawi, A.T.A.; Alhady, S.T.M.; Vuong, N.L.; Truong, L.V.; Luu, M.N.; et al. Awareness and preparedness of healthcare workers against the first wave of the COVID-19 pandemic: A cross-sectional survey across 57 countries. PLoS ONE 2021, 16, e0258348. [Google Scholar] [CrossRef] [PubMed]
- Haukenes, I.; Hammarstrom, A. Workplace gender composition and sickness absence: A register-based study from Sweden. Scand. J. Public Health 2023, 14034948231176108. [Google Scholar] [CrossRef] [PubMed]
- Street, T.D.; Lacey, S.J. A systematic review of studies identifying predictors of poor return to work outcomes following workplace injury. Work 2015, 51, 373–381. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Z.; Dreyer, R.P.; Spertus, J.A.; Masoudi, F.A.; Li, J.; Zheng, X.; Li, X.; Wu, C.; Bai, X.; Hu, S.; et al. Factors Associated With Return to Work After Acute Myocardial Infarction in China. JAMA Netw. Open 2018, 1, e184831. [Google Scholar] [CrossRef] [PubMed]
- Swedish Insurance Agency. Försäkringskassan, Report-Effekter som COVID-19 har på Sjukskrivningen; Diarienummer, 2020/000065. 2021, Volume 1. Available online: https://www.forsakringskassan.se/download/18.62c6089e1799604047f194f/1660564286183/effekter-som-covid-19-har-pa-sjukforsakringen-delrapport-1-svar-pa-regeringsuppdrag-dnr-fk-2020-000065.pdf (accessed on 2 September 2023).
- Seglem, K.B.; Orstavik, R.; Torvik, F.A.; Roysamb, E.; Vollrath, M. Education differences in sickness absence and the role of health behaviors: A prospective twin study. BMC Public Health 2020, 20, 1689. [Google Scholar] [CrossRef]
- Raghupathi, V.; Raghupathi, W. The influence of education on health: An empirical assessment of OECD countries for the period 1995–2015. Arch. Public Health 2020, 78, 20. [Google Scholar] [CrossRef]
- Jin, H.; Wang, H.; Li, X.; Zheng, W.; Ye, S.; Zhang, S.; Zhou, J.; Pennington, M. Economic burden of COVID-19, China, January-March, 2020: A cost-of-illness study. Bull. World Health Organ. 2021, 99, 112–124. [Google Scholar] [CrossRef]
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.G.; Ma, W.; Mehta, R.S.; Warner, E.T.; Sikavi, D.R.; Lo, C.H.; et al. Risk of COVID-19 among front-line health-care workers and the general community: A prospective cohort study. Lancet Public Health 2020, 5, e475–e483. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).