Alcohol Prevention in Urgent and Emergency Care (APUEC): Development and Evaluation of Workforce Digital Training on Screening, Brief Intervention, and Referral for Treatment
Abstract
:1. Introduction
1.1. Global Burden of Alcohol Consumption
1.2. The Need for Alcohol Misuse Prevention in Urgent and Emergency Care Settings
1.3. Barriers to Implementing SBIRT
1.4. The Need for Training and Education on SBIRT
1.5. Study Aim and Research Questions
2. Materials and Methods
2.1. Reusable Learning Objects
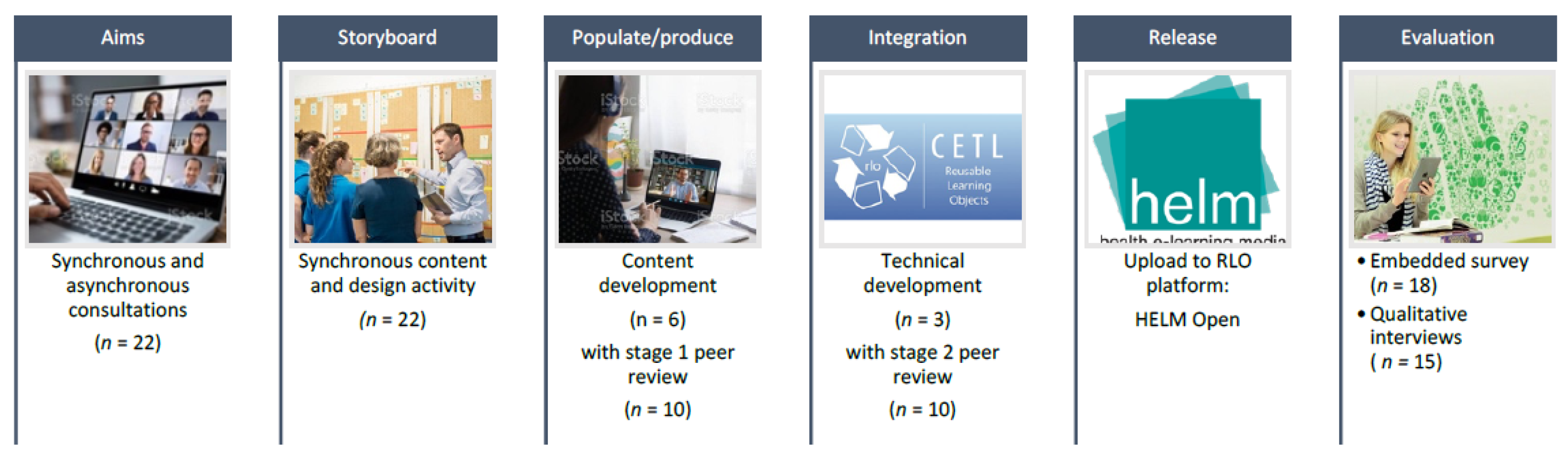
2.2. ASPIRE Methodology
2.2.1. Step 1: Establishing the Aims
2.2.2. Step 2: Storyboarding
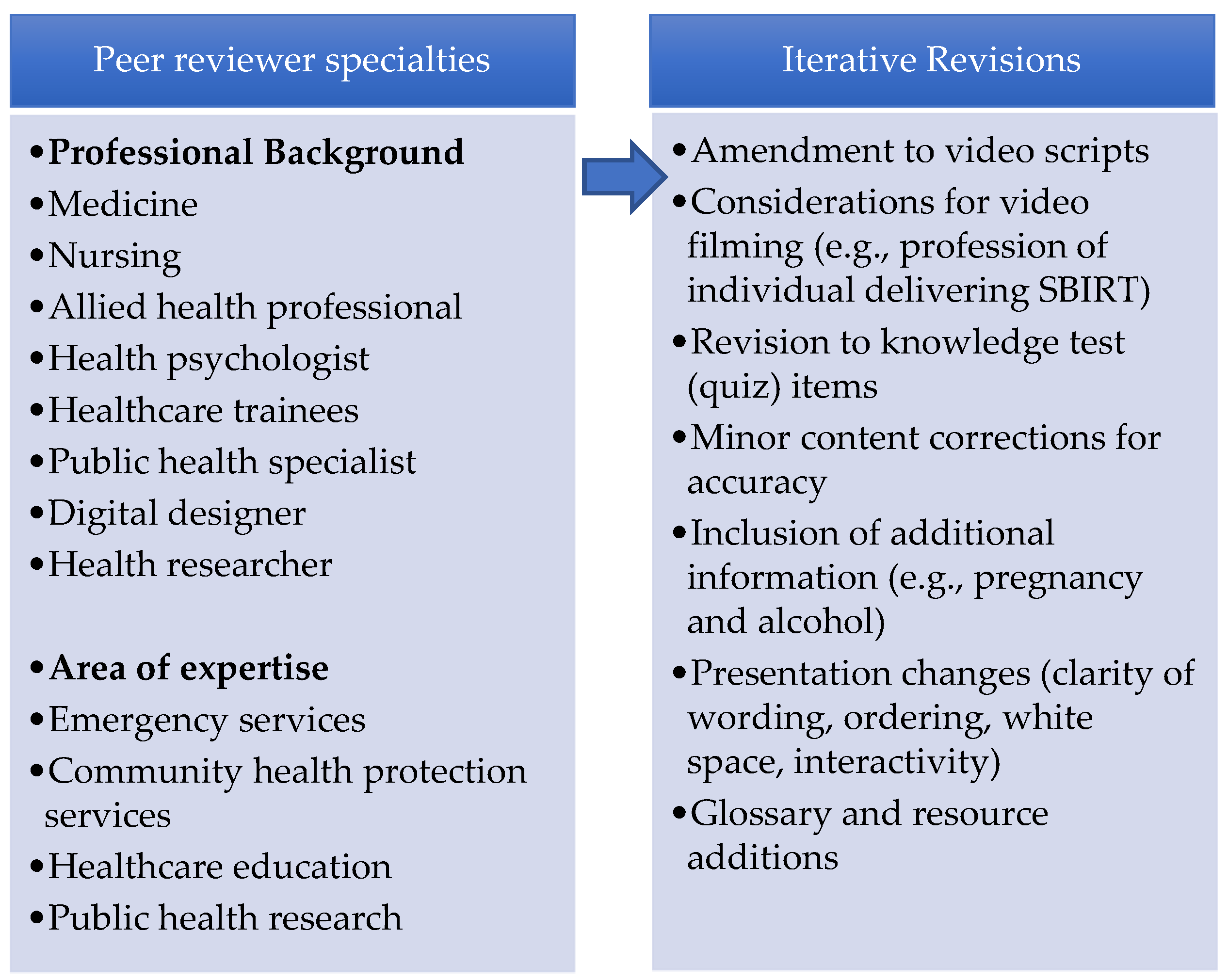
2.2.3. Step 3: Populating/Production
2.2.4. Step 4: Integration
2.2.5. Step 5: Release
2.2.6. Step 6: Evaluation
3. Results
3.1. Level 1
3.2. Level 2
“…we need to start introducing this cultural change in the clinicians’ minds that we don’t just medicate patients for the different symptoms that they come, but we look a little bit deeper into root causes” .[ID105, Male, Doctor]
“I think it just shows that you can make quite a punchy small effect from something small, so there must be able to make other ones, for other situations like drugs, smoking” .[ID107, Female, ACP]
“it helps you ask the right questions to the patients and actually understand the answers that they giving you, because at the moment I think a lot of clinicians, they will say how much alcohol do you drink? They tell them I don’t know, one bottle of wine every other day, but as a clinician you don’t know what that translates to” .[ID105, Male, Doctor]
“I think if you make it awkward when you’re questioning, the patient’s gonna feel awkward as well. So, it’s just about, think, being confident in your questioning and it’s just saying like I’m gonna be asking you some difficult questions, but I’ve got to kind of ask you about it so you know, sometimes it’s the elephant in the room, isn’t it?” .[ID114, Female, Nurse]
3.3. Level 3
“it starts the conversation and people have it in the back of their mind…it might take if, like us a few more times, them coming maybe to start the process, ‘cause people might be a bit reluctant or want to start but don’t know, just like there’s some obstacles in the way it might take a while” .[ID111, Female, Nurse]
“So that this becomes more meaningful and impactful in a way that even if the patient says no to me right now, there’s something they will probably go back home and think about it and maybe if they see another healthcare professional, and this topic is again discussed, something springs or kind of you know, just comes up from there and it has a longitudinal impact and positive effect on our patients” .[ID104, Female, Doctor]
“It’s something that beyond the healthcare sector can actually go into schools, teachers can use them, safety providers can use them. And so it, it transcends beyond the healthcare system itself” .[ID115, Male, Doctor]
“…someone who’s had lived experience of being helped by an intervention or being helped by a referral process, being helped by a bit of education to add some real potency” .[ID102, Male, ACP]
“I think moving forward we will see more educated patients where they present to their health service, health care services and they want to be consulted on their lifestyle as well and it’s very interesting point where we are because we’re moving from sick care to health care… What can we do to not get sick in the first place?” .[ID105, Male, Doctor]
4. Discussion
Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rehm, J.; Gmel Sr, G.E.; Gmel, G.; Hasan, O.S.; Imtiaz, S.; Popova, S.; Probst, C.; Roerecke, M.; Room, R.; Samokhvalov, A.V. The relationship between different dimensions of alcohol use and the burden of disease—An update. Addiction 2017, 112, 968–1001. [Google Scholar] [CrossRef] [PubMed]
- Roerecke, M.; Rehm, J. Alcohol use disorders and mortality: A systematic review and meta-analysis. Addiction 2013, 108, 1562–1578. [Google Scholar] [CrossRef]
- Stockwell, T.; Andreasson, S.; Cherpitel, C.; Chikritzhs, T.; Dangardt, F.; Holder, H.; Naimi, T.; Sherk, A. The burden of alcohol on health care during COVID-19. Drug Alcohol Rev. 2021, 40, 3–7. [Google Scholar] [CrossRef] [PubMed]
- GBD 2016 Alcohol Collaborators. Alcohol use and burden for 195 countries and territories, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2018, 392, 1015–1035. [Google Scholar] [CrossRef] [PubMed]
- Rehm, J.; Mathers, C.; Popova, S.; Thavorncharoensap, M.; Teerawattananon, Y.; Patra, J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet 2009, 373, 2223–2233. [Google Scholar] [CrossRef]
- Stockwell, T.; Andréasson, S.; Cherpitel, C.; Chikritzhs, T.; Dangardt, F.; Holder, H.; Naimi, T.; Sherk, A. Time for carefully tailored set of alcohol policies to reduce health-care burden and mitigate potential unintended consequences? Drug Alcohol Rev. 2021, 40, 17–18. [Google Scholar] [CrossRef]
- World Health Organisation. Global Coordination Mechanism on the Prevention and Control of NCDs. Available online: http://www.who.int/global-coordination-mechanism/ncd-themes/sustainable-development-goals/en/ (accessed on 21 November 2021).
- World Health Organization. Global Strategy to Reduce Harmful Use of Alcohol. Available online: https://www.who.int/substance_abuse/activities/gsrhua/en/ (accessed on 21 November 2021).
- Manthey, J.; Shield, K.D.; Rylett, M.; Hasan, O.S.; Probst, C.; Rehm, J. Global alcohol exposure between 1990 and 2017 and forecasts until 2030: A modelling study. Lancet 2019, 393, 2493–2502. [Google Scholar] [CrossRef]
- Shield, K.; Manthey, J.; Rylett, M.; Probst, C.; Wettlaufer, A.; Parry, C.D.; Rehm, J. National, regional, and global burdens of disease from 2000 to 2016 attributable to alcohol use: A comparative risk assessment study. Lancet Public Health 2020, 5, e51–e61. [Google Scholar] [CrossRef]
- Botwright, S.; Sutawong, J.; Kingkaew, P.; Anothaisintawee, T.; Dabak, S.V.; Suwanpanich, C.; Promchit, N.; Kampang, R.; Isaranuwatchai, W. Which interventions for alcohol use should be included in a universal healthcare benefit package? An umbrella review of targeted interventions to address harmful drinking and dependence. BMC Public Health 2023, 23, 382. [Google Scholar] [CrossRef]
- Nadkarni, A.; Massazza, A.; Guda, R.; Fernandes, L.T.; Garg, A.; Jolly, M.; Andersen, L.S.; Bhatia, U.; Bogdanov, S.; Roberts, B.; et al. Common strategies in empirically supported psychological interventions for alcohol use disorders: A meta-review. Drug Alcohol Rev. 2023, 42, 94–104. [Google Scholar] [CrossRef]
- Tan, C.J.; Shufelt, T.; Behan, E.; Chantara, J.; Koomsri, C.; Gordon, A.J.; Chaiyakunapruk, N.; Dhippayom, T. Comparative effectiveness of psychosocial interventions in adults with harmful use of alcohol: A systematic review and network meta-analysis. Addiction 2023, 118, 1414–1429. [Google Scholar] [CrossRef] [PubMed]
- Kelly, J.F.; Humphreys, K.; Ferri, M. Alcoholics Anonymous and other 12-step programs for alcohol use disorder. Cochrane Database Syst. Rev. 2020, 55, 641–651. [Google Scholar] [CrossRef]
- Bertholet, N.; Daeppen, J.B.; Wietlisbach, V.; Fleming, M.; Burnand, B. Reduction of alcohol consumption by brief alcohol intervention in primary care: Systematic review and meta-analysis. Arch. Intern. Med. 2005, 165, 986–995. [Google Scholar] [CrossRef] [PubMed]
- Barata, I.A.; Shandro, J.R.; Montgomery, M.; Polansky, R.; Sachs, C.J.; Duber, H.C.; Weaver, L.M.; Heins, A.; Owen, H.S.; Josephson, E.B. Effectiveness of SBIRT for alcohol use disorders in the emergency department: A systematic review. West. J. Emerg. Med. 2017, 18, 1143. [Google Scholar] [CrossRef] [PubMed]
- Kaner, E.F.; Beyer, F.R.; Muirhead, C.; Campbell, F.; Pienaar, E.D.; Bertholet, N.; Daeppen, J.B.; Saunders, J.B.; Burnand, B. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Syst. Rev. 2018, 2, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Dedert, E.A.; McDuffie, J.R.; Stein, R.; McNiel, J.M.; Kosinski, A.S.; Freiermuth, C.E.; Hemminger, A.; Williams, J.W., Jr. Electronic interventions for alcohol misuse and alcohol use disorders: A systematic review. Ann. Intern. Med. 2015, 163, 205–214. [Google Scholar] [CrossRef]
- Hutton, A.; Prichard, I.; Whitehead, D.; Thomas, S.; Rubin, M.; Sloand, E.; Powell, T.W.; Frisch, K.; Newman, P.; Goodwin Veenema, T. mHealth interventions to reduce alcohol use in young people: A systematic review of the literature. Compr. Child Adolesc. Nurs. 2020, 43, 171–202. [Google Scholar] [CrossRef]
- Kruse, C.S.; Lee, K.; Watson, J.B.; Lobo, L.G.; Stoppelmoor, A.G.; Oyibo, S.E. Measures of effectiveness, efficiency, and quality of telemedicine in the management of alcohol abuse, addiction, and rehabilitation: Systematic review. J. Med. Internet Res. 2020, 22, e13252. [Google Scholar] [CrossRef]
- Korecki, J.R.; Schwebel, F.J.; Votaw, V.R.; Witkiewitz, K. Mindfulness-based programs for substance use disorders: A systematic review of manualized treatments. Subst. Abus. Treat. Prev. Policy 2020, 15, 51. [Google Scholar] [CrossRef]
- Farhadian, N.; Moradi, S.; Zamanian, M.H.; Farnia, V.; Rezaeian, S.; Farhadian, M.; Shahlaei, M. Effectiveness of naltrexone treatment for alcohol use disorders in HIV: A systematic review. Subst. Abus. Treat Prev. Policy 2020, 15, 24. [Google Scholar] [CrossRef]
- Trapero-Bertran, M.; Gil-Domenech, D.; Vargas-Martinez, A.M. Economic evaluations of interventions aimed at the prevention, treatment and/or rehabilitation of alcohol-related disorders: A systematic review. Adicciones 2023, 35, 325–348. [Google Scholar] [CrossRef]
- Connor, J.P.; Haber, P.S.; Hall, W.D. Alcohol use disorders. Lancet 2016, 387, 988–998. [Google Scholar] [CrossRef] [PubMed]
- Mekonen, T.; Chan, G.C.K.; Connor, J.; Hall, W.; Hides, L.; Leung, J. Treatment rates for alcohol use disorders: A systematic review and meta-analysis. Addiction 2021, 116, 2617–2634. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Manthey, J.; Martinez, A.; Rehm, J. Alcohol use disorder severity and reported reasons not to seek treatment: A cross-sectional study in European primary care practices. Subst. Abus. Treat. Prev. Policy 2015, 10, 32. [Google Scholar] [CrossRef] [PubMed]
- Milic, J.; Glisic, M.; Voortman, T.; Borba, L.P.; Asllanaj, E.; Rojas, L.Z.; Troup, J.; Kiefte-de Jong, J.C.; van Beeck, E.; Muka, T. Menopause, ageing, and alcohol use disorders in women. Maturitas 2018, 111, 100–109. [Google Scholar] [CrossRef]
- Moore, K.E.; Stein, M.D.; Kurth, M.E.; Stevens, L.; Hailemariam, M.; Schonbrun, Y.C.; Johnson, J.E. Risk factors for self-stigma among incarcerated women with alcohol use disorder. Stigma Health 2020, 5, 158–167. [Google Scholar] [CrossRef]
- Weine, E.R.; Kim, N.S.; Lincoln, A.K. Understanding lay assessments of alcohol use disorder: Need for treatment and associated stigma. Alcohol Alcohol. 2016, 51, 98–105. [Google Scholar] [CrossRef]
- Van Boekel, L.C.; Brouwers, E.P.; Van Weeghel, J.; Garretsen, H.F. Stigma among health professionals towards patients with substance use disorders and its consequences for healthcare delivery: Systematic review. Drug Alcohol Depend. 2013, 131, 23–35. [Google Scholar] [CrossRef]
- Barbosa, C.; McKnight-Eily, L.R.; Grosse, S.D.; Bray, J. Alcohol screening and brief intervention in emergency departments: Review of the impact on healthcare costs and utilization. J. Subst. Abus. Treat. 2020, 117, 108096. [Google Scholar] [CrossRef]
- Landy, M.S.; Davey, C.J.; Quintero, D.; Pecora, A.; McShane, K.E. A systematic review on the effectiveness of brief interventions for alcohol misuse among adults in emergency departments. J. Subst. Abus. Treat. 2016, 61, 1–12. [Google Scholar] [CrossRef]
- Carvalho, A.F.; Heilig, M.; Perez, A.; Probst, C.; Rehm, J. Alcohol use disorders. Lancet 2019, 394, 781–792. [Google Scholar] [CrossRef]
- Indig, D.; Copeland, J.; Conigrave, K.M.; Rotenko, I. Attitudes and beliefs of emergency department staff regarding alcohol-related presentations. Int. Emerg. Nurs. 2009, 17, 23–30. [Google Scholar] [CrossRef]
- Cunningham, R.M.; Harrison, S.R.; McKay, M.P.; Mello, M.J.; Sochor, M.; Shandro, J.R.; Walton, M.A.; D’Onofrio, G. National survey of emergency department alcohol screening and intervention practices. Ann. Emerg. Med. 2010, 55, 556–562. [Google Scholar] [CrossRef]
- Blake, H.; Yildirim, M.; Premakumar, V.; Morris, L.; Miller, P.; Coffey, F. Attitudes and current practice in alcohol screening, brief intervention, and referral for treatment among staff working in urgent and emergency settings: An open, cross-sectional international survey. PLoS ONE 2023, 18, e0291573. [Google Scholar] [CrossRef]
- Robson, S.; Stephenson, A.; McCarthy, C.; Lowe, D.; Conlen, B.; Gray, A.J. Identifying opportunities for health promotion and intervention in the ED. Emerg. Med. J. 2021, 38, 927–932. [Google Scholar] [CrossRef]
- Weiland, T.J.; Dent, A.W.; Phillips, G.A.; Lee, N.K. Emergency clinician-delivered screening and intervention for high-risk alcohol use: A qualitative analysis. Emerg. Med. Australas. 2008, 20, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Gargaritano, K.L.; Murphy, C.; Auyeung, A.B.; Doyle, F. Systematic review of clinician-reported barriers to provision of brief advice for alcohol intake in hospital inpatient and emergency settings. Alcohol. Clin. Exp. Res. 2020, 44, 2386–2400. [Google Scholar] [CrossRef] [PubMed]
- Schofield, B.; Rolfe, U.; McClean, S.; Hoskins, R.; Voss, S.; Benger, J. What are the barriers and facilitators to effective health promotion in urgent and emergency care? A systematic review. BMC Emerg. Med. 2022, 22, 95. [Google Scholar] [CrossRef] [PubMed]
- van der Westhuizen, C.; Malan, M.; Naledi, T.; Roelofse, M.; Myers, B.; Stein, D.J.; Lahri, S.A.; Sorsdahl, K. Patient outcomes and experience of a task-shared screening and brief intervention service for problem substance use in South African emergency centres: A mixed methods study. Addict. Sci. Clin. Pract. 2021, 16, 31. [Google Scholar] [CrossRef] [PubMed]
- Chan, P.S.-F.; Fang, Y.; Wong, M.C.-S.; Huang, J.; Wang, Z.; Yeoh, E.K. Using consolidated framework for implementation research to investigate facilitators and barriers of implementing alcohol screening and brief intervention among primary care health professionals: A systematic review. Implement. Sci. 2021, 16, 91. [Google Scholar] [CrossRef]
- Schermer, C.R.; Gentilello, L.M.; Hoyt, D.B.; Moore, E.E.; Moore, J.B.; Rozycki, G.S.; Feliciano, D.V. National survey of trauma surgeons’ use of alcohol screening and brief intervention. J. Trauma 2003, 55, 849–856. [Google Scholar] [CrossRef] [PubMed]
- Adams, E.J.; Morris, L.; Marshall, G.; Coffey, F.; Miller, P.D.; Blake, H. Effectiveness and implementation of interventions for health promotion in urgent and emergency care settings: An umbrella review. BMC Emerg. Med. 2023, 23, 41. [Google Scholar] [CrossRef] [PubMed]
- Keen, A.; Thoele, K.; Oruche, U.; Newhouse, R. Perceptions of the barriers, facilitators, outcomes, and helpfulness of strategies to implement screening, brief intervention, and referral to treatment in acute care. Implement. Sci. 2021, 16, 44. [Google Scholar] [CrossRef] [PubMed]
- Blake, H.; Vaughan, B.; Bartle, C.; Yarker, J.; Munir, F.; Marwaha, S.; Daly, G.; Russell, S.; Meyer, C.; Hassard, J.; et al. Managing Minds at Work: Development of a Digital Line Manager Training Program. Int. J. Environ. Res. Public Health 2022, 19, 8006. [Google Scholar] [CrossRef] [PubMed]
- Scariot, C.A.; Heemann, A.; Padovani, S. Understanding the collaborative-participatory design. Work 2012, 41, 2701–2705. [Google Scholar] [CrossRef]
- Blake, H.; Fecowycz, A.; Starbuck, H.; Jones, W. COVID-19 Vaccine Education (CoVE) for health and care workers to facilitate global promotion of the COVID-19 vaccines. Int. J. Environ. Res. Public Health 2022, 19, 653. [Google Scholar] [CrossRef]
- Blake, H.; Somerset, S.; Evans, C. Development and fidelity testing of the test@ work digital toolkit for employers on workplace health checks and opt-in HIV testing. Int. J. Environ. Res. Public Health 2020, 17, 379. [Google Scholar] [CrossRef]
- Windle, R.; Wharrad, H.; Coolin, K.; Taylor, M. Collaborate to create: Stakeholder participation in open content creation. In Proceedings of the Association for Learning Technology Conference (ALT-C) Connect, Collaborate, Create, Coventry, UK, 6–8 September 2016. [Google Scholar]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ Res. Methods Rep. 2014, 348, 16–87. [Google Scholar] [CrossRef]
- Kirkpatrick, J.D.; Kirkpatrick, W.K. Kirkpatrick’s Four Levels of Training Evaluation; Association for Talent Development: Alexandria, VA, USA, 2016. [Google Scholar]
- Kirkpatrick, D.L. Evaluating Training Programs. The Four Levels; Berrett-Koehler Organizational Performance Series; Berret-Koehler Publishers, Inc.: Oakland, CA, USA, 1994. [Google Scholar]
- Blake, H.; Coffey, F. Evaluation of the APUEC Package: Alcohol Prevention in Urgent and Emergency Care. Available online: https://www.protocols.io/view/evaluation-of-the-apuec-package-alcohol-prevention-bp2l6xkn1lqe/v1 (accessed on 3 October 2023).
- Leeder, D.; McLachlan, J.C.; Rodrigues, V.; Stephens, N.; Wharrad, H.; McElduff, P. Universities’ Collaboration in eLearning (UCeL): A virtual community of practice in health professional education. In IADIS Web-Based Communities; IADIS Press: Lisbon, Portugal, 2004; pp. 386–393. [Google Scholar]
- Taylor, M.; Wharrad, H.; Konstantinidis, S. Immerse yourself in ASPIRE-adding persuasive technology methodology to the ASPIRE Framework. In Proceedings of the International Conference on Interactive Collaborative Learning, Dresden, Germany, 22–24 September 2021; pp. 1106–1117. [Google Scholar]
- Wharrad, H.; Windle, R.; Taylor, T. Designing digital education and training for health. In Digital Innovations in Healthcare Education and Training; Konstantinidis, S., Bamidis, P., Zary, N., Eds.; Academic Press: Cambridge, MA, USA, 2021. [Google Scholar]
- Wenger-Trayner, E.; Wenger-Trayner, B. An Introduction to Communities of Practice: A Brief Overview of the Concept and Its Uses. 2015. Available online: https://www.wenger-trayner.com/introduction-to-communities-of-practice (accessed on 31 October 2023).
- The Mural® Visual Collaboration Platform. Available online: https://www.mural.com (accessed on 31 October 2023).
- Wharrad, H.; Morales, R.; Windle, R.; Bradley, C. A toolkit for a multilayered, cross institutional evaluation strategy. In Proceedings of the EdMedia+ Innovate Learning, Vienna, Austria, 30 June 2008; pp. 4921–4925. [Google Scholar]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef]
- Kirkpatrick, A.; O’Connor, J.; Campbell, A.; Cooper, M. Web Content Accessibility Guidelines (WCAG) 2.1. Available online: https://www.w3.org/TR/WCAG21/ (accessed on 21 September 2023).
- Kelly, B.; Phipps, L.; Swift, E. Developing a holistic approach for e-learning accessibility. Can. J. Learn. Technol./Rev. Can. Apprentiss. Technol. 2004, 30, 1–15. [Google Scholar] [CrossRef]
- Jun, S.; Plint, A.C.; Campbell, S.M.; Curtis, S.; Sabir, K.; Newton, A.S. Point-of-care Cognitive Support Technology in Emergency Departments: A Scoping Review of Technology Acceptance by Clinicians. Acad. Emerg. Med. 2018, 25, 494–507. [Google Scholar] [CrossRef]
- Lim, H.M.; Ng, C.J.; Wharrad, H.; Lee, Y.K.; Teo, C.H.; Lee, P.Y.; Krishnan, K.; Abu Hassan, Z.F.; Yong, P.V.C.; Yap, W.H.; et al. Knowledge transfer of eLearning objects: Lessons learned from an intercontinental capacity building project. PLoS ONE 2022, 17, e0274771. [Google Scholar] [CrossRef] [PubMed]
- Moore, J.; Goodman, P.; Selway, J.; Hawkins-Walsh, E.; Merritt, J.; Dombrowski, J. SBIRT education for nurse practitioner students: Integration into an MSN program. J. Nurs. Educ. 2017, 56, 725–732. [Google Scholar] [CrossRef] [PubMed]
- Belfiore, M.N.; Blinka, M.D.; BrintzenhofeSzoc, K.; Shields, J. Screening, brief intervention, and referral to treatment (SBIRT) curriculum integration and sustainability: Social work and nursing faculty perspectives. Subst. Abus. 2018, 39, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Broyles, L.M.; Gordon, A.J.; Rodriguez, K.L.; Hanusa, B.H.; Kengor, C.; Kraemer, K.L. Evaluation of a pilot training program in alcohol screening, brief intervention, and referral to treatment for nurses in inpatient settings. J. Addict. Nurs. 2013, 24, 8–19. [Google Scholar] [CrossRef]
- Rankin, J.A.; Then, K.L.; Atack, L. Can emergency nurses’ triage skills be improved by online learning? Results of an experiment. J. Emerg. Nurs. 2013, 39, 20–26. [Google Scholar] [CrossRef]
- Hersey, P.; McAleer, S. Developing an e-learning resource for nurse airway assistants in the emergency department. Br. J. Nurs. 2017, 26, 217–221. [Google Scholar] [CrossRef]
- Arabani Nezhad, M.; Ayatollahi, H.; Heidari Beigvand, H. Development and evaluation of an e-learning course in oxygen therapy. BMC Med. Educ 2022, 22, 776. [Google Scholar] [CrossRef]
- Smeekens, A.E.; Broekhuijsen-van Henten, D.M.; Sittig, J.S.; Russel, I.M.; ten Cate, O.T.; Turner, N.M.; van de Putte, E.M. Successful e-learning programme on the detection of child abuse in emergency departments: A randomised controlled trial. Arch. Dis. Child. 2011, 96, 330–334. [Google Scholar] [CrossRef]
- Inuenwi, B.; Lommel, L.; Peter, S.B.; Carley, A. Increasing Understanding and Perceived Confidence of Nurses Working in an Emergency Department in Assessing Patients at Risk of Violent Behavior. Clin. Nurse Spec. 2023, 37, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Walker, R.; Bennett, C.; Kumar, A.; Adamski, M.; Blumfield, M.; Mazza, D.; Truby, H. Evaluating online continuing professional development regarding weight management for pregnancy using the new world Kirkpatrick model. J. Contin. Educ. Health Prof. 2019, 39, 210–217. [Google Scholar] [CrossRef] [PubMed]
- Moreau, K.A.; Eady, K.; Sikora, L.; Horsley, T. Digital storytelling in health professions education: A systematic review. BMC Med. Educ. 2018, 18, 208. [Google Scholar] [CrossRef] [PubMed]
- Zielinska-Tomczak, L.; Przymuszala, P.; Tomczak, S.; Krzysko-Pieczka, I.; Marciniak, R.; Cerbin-Koczorowska, M. How do dieticians on Instagram teach? The potential of the Kirkpatrick Model in the evaluation of the effectiveness of nutritional education in social media. Nutrients 2021, 13, 2005. [Google Scholar] [CrossRef] [PubMed]
- Sinclair, P.; Kable, A.; Levett-Jones, T. The effectiveness of internet-based e-learning on clinician behavior and patient outcomes: A systematic review protocol. JBI Evid. Synth. 2015, 13, 52–64. [Google Scholar] [CrossRef]
- Brown, R.C.; Straub, J.; Bohnacker, I.; Plener, P.L. Increasing knowledge, skills, and confidence concerning students’ suicidality through a gatekeeper workshop for school staff. Front. Psychol. 2018, 9, 1233. [Google Scholar] [CrossRef]



| Breakout Group Questions | To Consider: |
|---|---|
| Q1. What do you think is important to include in this RLO about brief interventions for alcohol prevention in urgent and emergency settings? | What are the key topics we should cover? What are the most important guidelines healthcare staff need to know about? What sort of information will be essential for urgent and emergency staff to understand to be able to deliver brief health promotion intervention around alcohol? Think about:
|
| Q2. How do you think the information should be best presented for maximum engagement? | How best to present the content? How to make it interactive? Is there a better order for materials? What will encourage people to engage with this training? |
| Q3. What evidence-based resources should we signpost people to? | Extra resources aimed at staff using the RLO Helpful resources for signposting service users |
| ID | Gender | Occupation |
|---|---|---|
| 101 | Female | Emergency Department Assistant (EDA) |
| 102 | Male | Advanced Clinical Practitioner (ACP) |
| 103 | Female | Clinical Support Worker (CSW) Manager |
| 104 | Female | Doctor |
| 105 | Male | Doctor |
| 106 | Female | ACP/Teaching Fellow |
| 107 | Female | ACP |
| 108 | Female | Nurse |
| 109 | Female | Nurse |
| 110 | Female | Nurse |
| 111 | Female | Nurse |
| 112 | Female | Nurse |
| 113 | Female | Nurse |
| 114 | Female | Nurse |
| 115 | Male | Doctor |
| Level (1–3) † | Sub-Component | Measure | Data Collection | ||
|---|---|---|---|---|---|
| Post-Survey | Interview | ||||
| 1 | Reach | Channel for receipt of the resource User role: healthcare professional or student Geographical region | X | X | |
| Use | Helpfulness for learning Main reason for accessing Ease /problems with use (technical, level of difficulty, context, cultural) | X | X | ||
| Satisfaction | Overall view and rating of the resource Elements most liked Elements least liked Recommendation to others | X | X | ||
| Engagement | View towards interactive elements (menu, narration adjustments, video clips, information boxes, click boxes, quiz, extra resources) | X | |||
| Relevance | Relevance to self or others Opportunity to use the resource | X | |||
| 2 | Knowledge | Evidence of new learning | X | ||
| Skill | Feeling equipped with useful knowledge | X | |||
| Attitude | Views towards APUEC training/change in views | X | |||
| Confidence | Changes in confidence to communicate (patients or clients) | X | |||
| Commitment | Estimated future use and resource sharing | X | |||
| 3 | Behaviour changes | User application of knowledge Reported behavioural changes | X X | ||
| Required drivers | Target audiences Mechanisms for dissemination | X X | |||
| Survey Items | N (%) |
|---|---|
| I believe patients should be screened for their alcohol consumption in UEC settings | 17 (94.5) |
| I believe that UEC settings are suitable places to deliver brief interventions for alcohol prevention | 18 (100) |
| I believe that brief advice from a healthcare professional can help patients to reduce their drinking and/or seek help with their drinking | 16 (88.9) |
| I believe some patients should be referred for treatment for their alcohol consumption in urgent and emergency care settings | 18 (100) |
| I have the knowledge to screen my patients for alcohol consumption | 15 (83.3) |
| I know what tools to use to screen my patients for alcohol consumption | 14 (77.8) |
| I feel confident I can screen my patients for alcohol consumption | 15 (83.3) |
| I have the knowledge to give brief advice to my patients about reducing their alcohol consumption | 14 (77.7) |
| I feel confident that I can give brief advice to my patients about reducing their alcohol consumption | 15 (83.4) |
| I have the skills to give brief advice about alcohol with my patients | 14 (77.8) |
| I intend to increase the number of patients I screen for alcohol consumption | 15 (82.9) |
| I intend to increase the number of patients I give brief advice to about their alcohol consumption | 16 (88.8) |
| Level (1–3) † | Sub-Component | Measure | N (%) |
|---|---|---|---|
| (1) Reaction | Reach | Channel for receipt of the resource A course learning resource Recommended by peer/colleague Type of User Healthcare professional “I think everybody, all healthcare professionals, regardless of their hierarchy or their background, would benefit” [ID104, Female, Doctor]. “I feel like most health professionals should know about it so they can pass it on to patients, their relatives, staff”. [ID103, Female, CSW manager]. | 11 (61.1) 8 (44.4) 18 (100) |
| Use | Helpful or very helpful rating: Problems with use (% yes) No problems Technical issues Level of difficulty Language difficulty Contextual or cultural differences Other issues (e.g., personal device issue, lack of time to complete) “this training was very structured and it’s standardised” [ID104, Female, Doctor]. “succinct enough that they kept my attention…. the fact they had transcripts there, that was great” [ID102, Male, ACP]. “it was really good with the voiceovers as well… I sometimes struggle with my reading, so actually having it to listen to was really helpful” [ID113, Female, Nurse]. | 18 (100) 16 (88.9) 2 (11.1) 0 (0.0) 0 (0.0) 0 (0.0) 0 (0.0) | |
| Satisfaction | Would recommend to others: “I think it’s invaluable” [ID105, Male, Doctor]. “I really enjoyed doing it” [ID112, Female, Nurse]. “it’s really been educative, and you know, it stimulates the way one learns quickly … it’s something that everyone would be happy to do any time” [ID115, Male, Doctor]. | 18 (100) | |
| Engagement | View towards interactive elements: “it’s been quite informative and quite interactive” [ID108, Female, Nurse]. “the use of video, the use of quizzes” [ID105, Male, Doctor]. “I think you remember it more when you’re actively doing something” [ID112, Female, Nurse]. | - | |
| Relevance | Relevance to self or others: “very relevant, I think in A&E … we get so many alcohol related injuries in the whole population…from the students right through to the elderly” [ID108, Female, Nurse]. “it is something we deal with every day, like multiple of our patients in our teams will be alcohol related or drug related” [ID110, Female, Nurse]. | - | |
| (2) Learning | Knowledge | Learned something new: “I like the kind of the tools that were involved. Yeah, it gave me some food for thought” [ID102, Male, ACP]. “the reference to the AUDIT-C umm tool for screening for alcohol. Pretty simple questions, really nice stratification of risk” [ID105, Male, Doctor]. “I know how to easily … keep on track, engage with them, keep on track with the conversation because it’s all straight in my head” [ID115, Male, Doctor]. | - |
| Skill | Feeling equipped with useful knowledge: “when I’m talking to patients or colleagues … about their alcohol, about their relationship and its potential impact, I think it will help … give me a bit more structure, which I’m not doing now … how I approach the subject and allow them to talk so we can move through it together” [ID102, Male, ACP]. “I’m learning to even incorporate all of those social determinants of health just to find out and yes, it does give us a lot of information to me, as a doctor to decide and help personalise care for this patient based on their individual circumstances” [ID104, Female, Doctor]. “it was a good resource to learn about how to initiate that conversation with people who aren’t necessarily being admitted to ED for alcohol use. So I thought that that aspect of it was quite handy cause it is a bit of an awkward conversation to have, isn’t it?” [ID110, Female, Nurse]. “it’s given me more of an insight into what exactly to ask to cut out all the ‘gobbledygook’ and just get to the point. But at the same time have that patient relationship but know exactly what the important questions are to ask as opposed to going through a whole quiz about drinking” [ID109, Female, Urgent care practitioner]. | - | |
| Attitude | Views towards alcohol prevention and/or SBIRT: “we have to start talking about health improvement” [ID110, Female, Nurse]. “I hope it empowers people to that, you know, actually, we’re all responsible for having these conversations, and we all can have an impact on a patient’s health and well-being. So we should be having these conversations” [ID106, Female, ACP]. “I think it should be less of a taboo and I think the more we have these conversations with patients, the easier it comes for us just to make it into our, like our normal” [ID107, Female, ACP]. “I think A&E is a great place to kind of capture people and make…meaningful kind of adjustments or impacts” [ID102, Male, ACP]. “if we’ve got people with better health kind of knowledge it could lead to better outcomes. So ultimately it leads to a reduced stress on the system. Potentially” [ID102, Male, ACP]. | - | |
| Confidence | Increased confidence to deliver SBIRT: “I think once you’ve had that extra training, you’ve got the knowledge base and you know where to signpost people” [ID108, Female, Nurse]. “it just helps them [staff] become better communicators with our patients, you know, like the videos making sure that we’re not, we’re not kind of coming across as judgmental” [ ID106, Female, ACP]. “…had I received that, that teaching, that training, looked at that resource, six, seven, eight years ago when I was a more junior member of staff, absolutely it would have given me the confidence” [ID106, Female, ACP]. “it has reinforced me in, in having this confidence that whatever I am doing and the approach that I have had so far” [ID104, Female, Doctor]. “it’s giving me more confidence and understanding” [ID107, Female, ACP]. “I feel, I feel a lot more comfortable talking about it” [ID111, Female, Nurse]. | - | |
| Commitment | Estimated future use and resource sharing: “that’s really good. I’ll implement that, that’s a really simple thing I can do” [ID112, Female, Nurse]. “I think I would want to be able to share it to perhaps other people. If they were like learning how to give out advice, absolutely I think it would probably benefit a lot of people” [ID106, Female, ACP]. | - | |
| (3) Transfer/ Behaviour | Behavioural intention and/or behavioural changes | User application of knowledge and reported behavioural intentions and/or changes: “I’ll be referring, referring them to alcohol specialists or the teams that we have on site” [ID101, Female, EDA]. | - |
| Required drivers | Target audiences and mechanisms for dissemination (i.e., who should use SBIRT, approaches for transfer of learning into practice, and when should it happen). “It should be everyone… who has a contact to the patient and depending on who, who is able to see the patient first” [ID115, Male, Doctor]. “just everybody because I think everybody has got the opportunity to, to give that advice even if it’s just 5 min” [ID106, Female, ACP]. “it’s the approachability of that person. So if, like the doctor says, well I’ve tried to have this conversation with this patient, would you mind just going in and seeing if you can get them to open up a little bit more, if we support each other within the wider team” [ID110, Female, Nurse]. ‘sometimes the quiet 10 min chat you get is when you’ve taken a patient round to X-ray. So that could be a nurse, an EDA, CSW” [ID113, Female, Nurse]. “Like we work together as a unit, I feel like that would be quite a good way to get rid of those kind of barriers” [ID110, Female, Nurse]. | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Blake, H.; Adams, E.J.; Chaplin, W.J.; Morris, L.; Mahmood, I.; Taylor, M.G.; Langmack, G.; Jones, L.; Miller, P.; Coffey, F. Alcohol Prevention in Urgent and Emergency Care (APUEC): Development and Evaluation of Workforce Digital Training on Screening, Brief Intervention, and Referral for Treatment. Int. J. Environ. Res. Public Health 2023, 20, 7028. https://doi.org/10.3390/ijerph20227028
Blake H, Adams EJ, Chaplin WJ, Morris L, Mahmood I, Taylor MG, Langmack G, Jones L, Miller P, Coffey F. Alcohol Prevention in Urgent and Emergency Care (APUEC): Development and Evaluation of Workforce Digital Training on Screening, Brief Intervention, and Referral for Treatment. International Journal of Environmental Research and Public Health. 2023; 20(22):7028. https://doi.org/10.3390/ijerph20227028
Chicago/Turabian StyleBlake, Holly, Emma J. Adams, Wendy J. Chaplin, Lucy Morris, Ikra Mahmood, Michael G. Taylor, Gillian Langmack, Lydia Jones, Philip Miller, and Frank Coffey. 2023. "Alcohol Prevention in Urgent and Emergency Care (APUEC): Development and Evaluation of Workforce Digital Training on Screening, Brief Intervention, and Referral for Treatment" International Journal of Environmental Research and Public Health 20, no. 22: 7028. https://doi.org/10.3390/ijerph20227028
APA StyleBlake, H., Adams, E. J., Chaplin, W. J., Morris, L., Mahmood, I., Taylor, M. G., Langmack, G., Jones, L., Miller, P., & Coffey, F. (2023). Alcohol Prevention in Urgent and Emergency Care (APUEC): Development and Evaluation of Workforce Digital Training on Screening, Brief Intervention, and Referral for Treatment. International Journal of Environmental Research and Public Health, 20(22), 7028. https://doi.org/10.3390/ijerph20227028








