¡Miranos! An 8-Month Comprehensive Preschool Obesity Prevention Program in Low-Income Latino Children: Effects on Children’s Gross Motor Development
Abstract
:1. Introduction
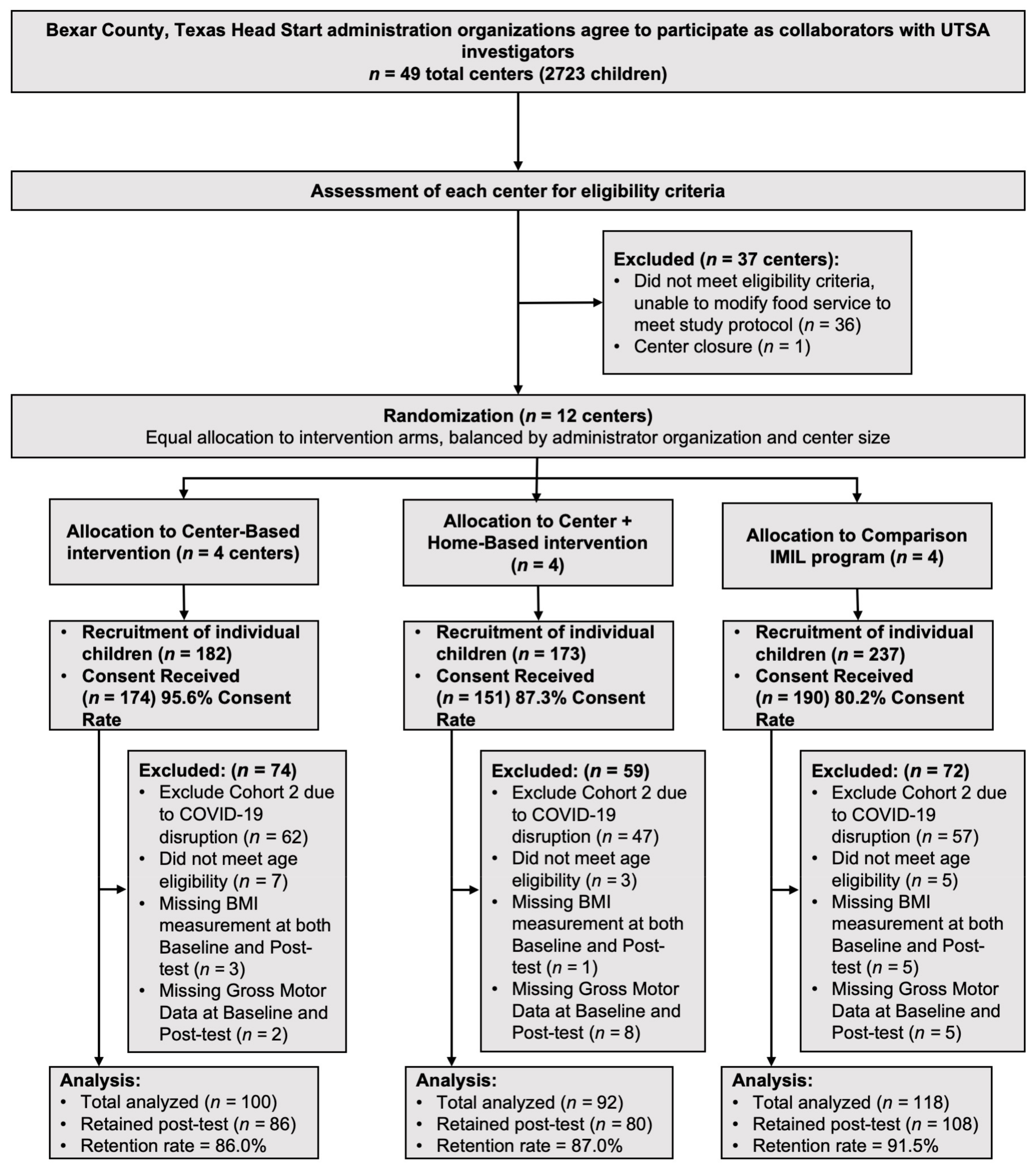
2. Materials and Methods
2.1. Study Design
2.2. Study Setting and Participants
2.3. Description of ¡Míranos! Intervention
2.4. Study Measurements
2.5. Statistical Analyses
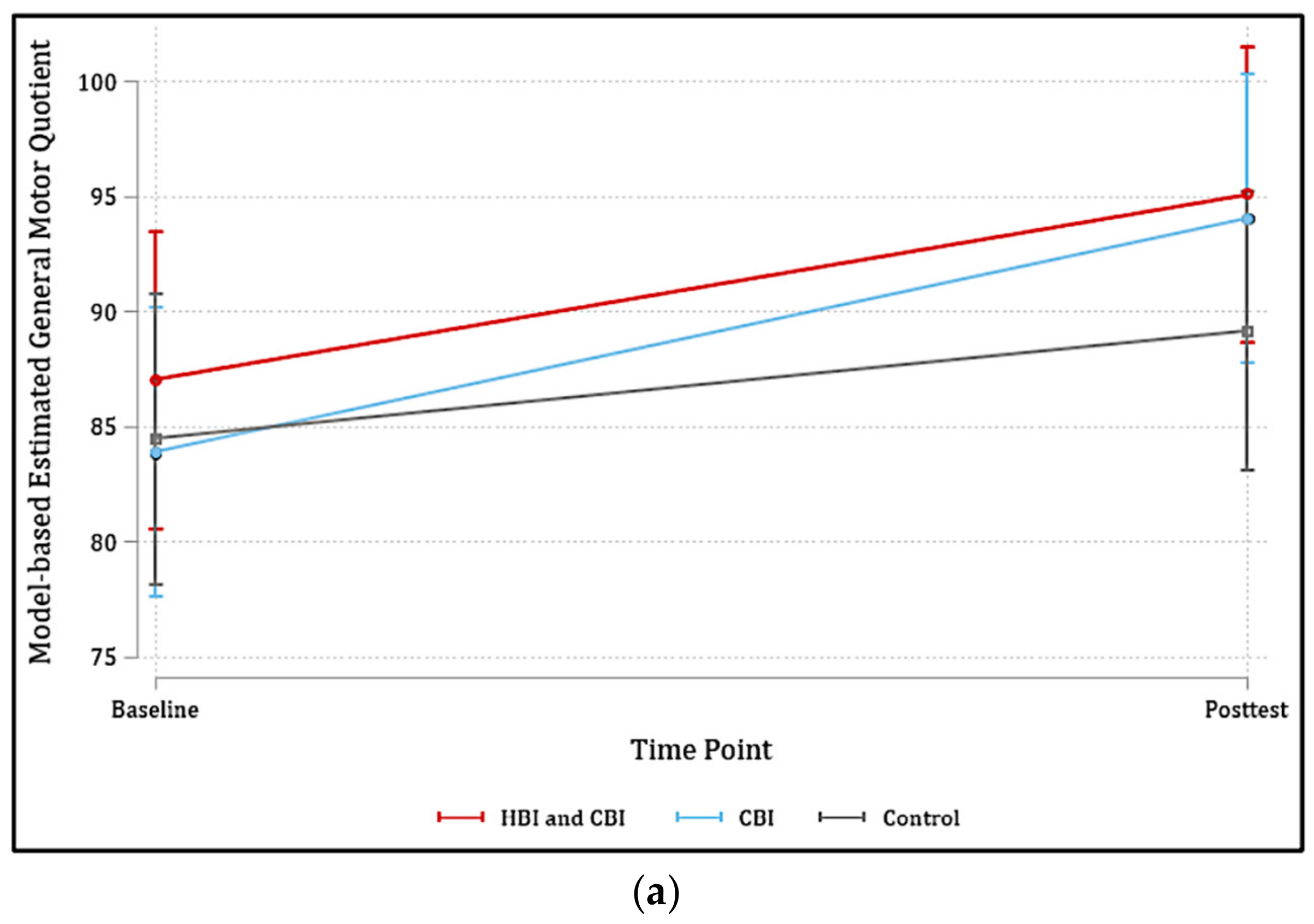
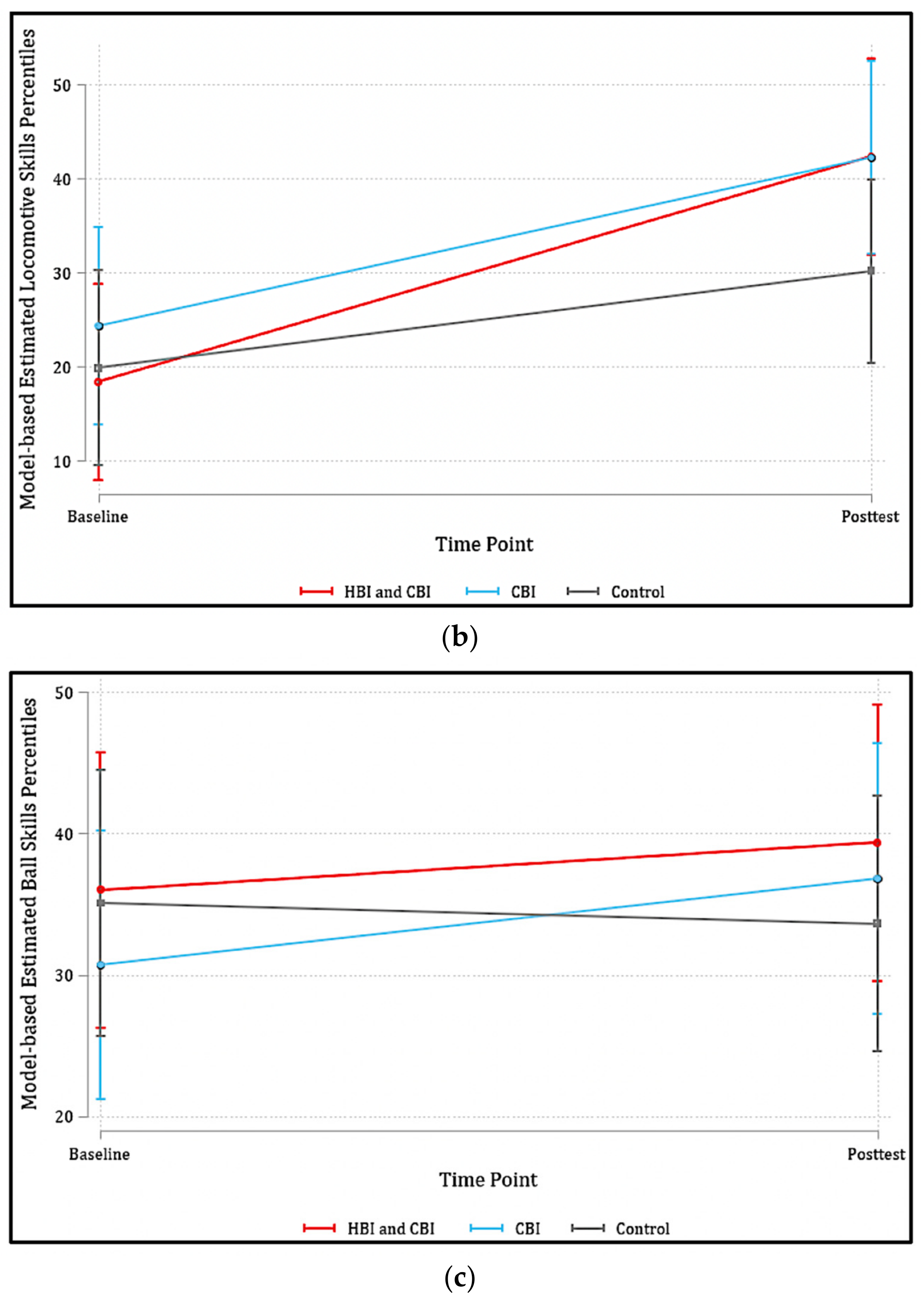
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Gallahue, D. Understanding Motor Development; McGraw-Hill Higher Education: Irvine, CA, USA, 2011. [Google Scholar]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A developmental perspective on the role of motor skill competence in physical activity: An emergent relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Clark, J.E.; Metcalfe, J.S. The mountain of motor development: A metaphor. Mot. Dev. Res. Rev. 2002, 2, 183–202. [Google Scholar]
- Hulteen, R.M.; Lander, N.J.; Morgan, P.J.; Barnett, L.M.; Robertson, S.J.; Lubans, D.R. Validity and reliability of field-based measures for assessing movement skill competency in lifelong physical activities: A systematic review. Sports Med. 2015, 45, 1443–1454. [Google Scholar] [CrossRef] [PubMed]
- Henderson, S.E.; Sugden, D.; Barnett, A.L. Movement assessment battery for children-2. Res. Dev. Disabil. 1992, 2, 1925–1939. [Google Scholar]
- Schembri, R.; Quinto, A.; Aiello, F.; Pignato, S.; Sgrò, F. The relationship between the practice of physical activity and sport and the level of motor competence in primary school children. J. Phys. Educ. Sport 2019, 19, 1994–1998. [Google Scholar]
- Tonge, K.L.; Jones, R.A.; Okely, A.D. Correlates of children’s objectively measured physical activity and sedentary behavior in early childhood education and care services: A systematic review. Prev. Med. 2016, 89, 129–139. [Google Scholar] [CrossRef]
- Barnett, L.M.; Lai, S.K.; Veldman, S.L.; Hardy, L.L.; Cliff, D.P.; Morgan, P.J.; Zask, A.; Lubans, D.R.; Shultz, S.P.; Ridgers, N.D. Correlates of gross motor competence in children and adolescents: A systematic review and meta-analysis. Sports Med. 2016, 46, 1663–1688. [Google Scholar] [CrossRef]
- Barnett, L.M.; Van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Does childhood motor skill proficiency predict adolescent fitness? Med. Sci. Sports Exerc. 2008, 40, 2137–2144. [Google Scholar] [CrossRef]
- Barnett, L.M.; Van Beurden, E.; Morgan, P.J.; Brooks, L.O.; Beard, J.R. Childhood motor skill proficiency as a predictor of adolescent physical activity. J. Adolesc. Health 2009, 44, 252–259. [Google Scholar] [CrossRef]
- Diamond, A. Effects of physical exercise on executive functions: Going beyond simply moving to moving with thought. Ann. Sports Med. Res. 2015, 2, 1011. [Google Scholar]
- Barros, W.M.A.; Silva, K.G.d.; Silva, R.K.P.; Souza, A.P.d.S.; Silva, A.B.J.d.; Silva, M.R.M.; Fernandes, M.S.d.S.; Souza, S.L.d.; Souza, V.d.O.N. Effects of overweight/obesity on motor performance in children: A systematic review. Front. Endocrinol. 2022, 12, 759165. [Google Scholar] [CrossRef] [PubMed]
- Pagani, L.S.; Messier, S. Links between motor skills and indicators of school readiness at kindergarten entry in urban disadvantaged children. J. Educ. Dev. Psychol. 2012, 2, 95. [Google Scholar] [CrossRef]
- Stein, M.; Auerswald, M.; Ebersbach, M. Relationships between motor and executive functions and the effect of an acute coordinative intervention on executive functions in kindergartners. Front. Psychol. 2017, 8, 859. [Google Scholar] [CrossRef] [PubMed]
- Niederer, I.; Kriemler, S.; Gut, J.; Hartmann, T.; Schindler, C.; Barral, J.; Puder, J.J. Relationship of aerobic fitness and motor skills with memory and attention in preschoolers (Ballabeina): A cross-sectional and longitudinal study. BMC Pediatr. 2011, 11, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Diamond, A. Interrelated and interdependent. Dev. Sci. 2007, 10, 152–158. [Google Scholar] [CrossRef]
- Bowman, B.T.; Donovan, M.S.; Burns, M.S. Eager to Learn: Educating Our Preschoolers. [Full Report and Executive Summary]; ERIC: Washington, DC, USA, 2001. [Google Scholar]
- Hagan, J.F.; Shaw, J.; Duncan, P. Bright Futures; American Academy of Pediatrics: Itasca, IL, USA, 2017. [Google Scholar]
- Clark, J.E.; Clements, R.L.; Guddemi, M.; Morgan, D.W.; Pica, R.; Pivarnik, J.M.; Rudisill, M.; Small, E.; Virgilio, S.J. Active Start: A Statement of Physical Activity Guidelines for Children Birth to Five Years; ERIC: Washington, DC, USA, 2002. [Google Scholar]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The physical activity guidelines for Americans. JAMA 2018, 320, 2020–2028. [Google Scholar] [CrossRef]
- Kwon, S.; O’neill, M. Socioeconomic and familial factors associated with gross motor skills among US children aged 3–5 years: The 2012 NHANES National Youth Fitness Survey. Int. J. Environ. Res. Public Health 2020, 17, 4491. [Google Scholar] [CrossRef]
- Brian, A.; Bardid, F.; Barnett, L.M.; Deconinck, F.J.; Lenoir, M.; Goodway, J.D. Actual and perceived motor competence levels of Belgian and United States preschool children. J. Mot. Learn. Dev. 2018, 6, S320–S336. [Google Scholar] [CrossRef]
- Pope, M.L.; Liu, T.; Getchell, N. Object-control skills in Hispanic preschool children enrolled in head start. Percept. Mot. Ski. 2011, 112, 193–200. [Google Scholar] [CrossRef]
- Liu, T.; Hamilton, M.; Smith, S. Motor proficiency of the Head Start and typically developing children on MABC-2. J. Child Adolesc. Behav. 2015, 3, 198. [Google Scholar]
- Liu, T.; Hoffmann, C.; Hamilton, M. Motor skill performance by low SES preschool and typically developing children on the PDMS-2. Early Child. Educ. J. 2017, 45, 53–60. [Google Scholar] [CrossRef]
- Morley, D.; Till, K.; Ogilvie, P.; Turner, G. Influences of gender and socioeconomic status on the motor proficiency of children in the UK. Hum. Mov. Sci. 2015, 44, 150–156. [Google Scholar] [CrossRef] [PubMed]
- Okely, A.D.; Booth, M.L. Mastery of fundamental movement skills among children in New South Wales: Prevalence and sociodemographic distribution. J. Sci. Med. Sport 2004, 7, 358–372. [Google Scholar] [CrossRef] [PubMed]
- Goodway, J.D.; Robinson, L.E.; Crowe, H. Gender differences in fundamental motor skill development in disadvantaged preschoolers from two geographical regions. Res. Q. Exerc. Sport 2010, 81, 17–24. [Google Scholar] [CrossRef]
- Hulteen, R.M.; Morgan, P.J.; Barnett, L.M.; Stodden, D.F.; Lubans, D.R. Development of foundational movement skills: A conceptual model for physical activity across the lifespan. Sports Med. 2018, 48, 1533–1540. [Google Scholar] [CrossRef]
- Story, M.; Kaphingst, K.M.; French, S. The role of child care settings in obesity prevention. Future Child. 2006, 16, 143–168. [Google Scholar] [CrossRef]
- Bureau, U.C. Who’s Minding the Kids? Child Care Arrangements: Spring 2011; US Department of Commerce, Ed.; United States Census Bureau: Washington, DC, USA, 2013.
- Figueroa, R.; An, R. Motor skill competence and physical activity in preschoolers: A review. Matern. Child Health J. 2017, 21, 136–146. [Google Scholar] [CrossRef]
- True, L.; Pfeiffer, K.A.; Dowda, M.; Williams, H.G.; Brown, W.H.; O’Neill, J.R.; Pate, R.R. Motor competence and characteristics within the preschool environment. J. Sci. Med. Sport 2017, 20, 751–755. [Google Scholar] [CrossRef]
- Early, D.M.; Iruka, I.U.; Ritchie, S.; Barbarin, O.A.; Winn, D.-M.C.; Crawford, G.M.; Frome, P.M.; Clifford, R.M.; Burchinal, M.; Howes, C. How do pre-kindergarteners spend their time? Gender, ethnicity, and income as predictors of experiences in pre-kindergarten classrooms. Early Child. Res. Q. 2010, 25, 177–193. [Google Scholar] [CrossRef]
- Yin, Z.; Ullevig, S.L.; Sosa, E.; Liang, Y.; Olmstead, T.; Howard, J.T.; Errisuriz, V.L.; Estrada, V.M.; Martinez, C.E.; He, M.; et al. Study protocol for a cluster randomized controlled trial to test “¡Míranos! Look at Us, We Are Healthy!”—An early childhood obesity prevention program. BMC Pediatr. 2019, 19, 190. [Google Scholar] [CrossRef]
- Winter, S.M.; Sass, D.A. Healthy & ready to learn: Examining the efficacy of an early approach to obesity prevention and school readiness. J. Res. Child. Educ. 2011, 25, 304–325. [Google Scholar]
- Bellows, L.L.; Davies, P.L.; Anderson, J.; Kennedy, C. Effectiveness of a physical activity intervention for Head Start preschoolers: A randomized intervention study. Am. J. Occup. Ther. 2013, 67, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Yin, Z.; Parra-Medina, D.; Cordova, A.; He, M.; Trummer, V.; Sosa, E.; Gallion, K.J.; Sintes-Yallen, A.; Huang, Y.; Wu, X.; et al. Miranos! Look at us, we are healthy! An environmental approach to early childhood obesity prevention. Child. Obes. 2012, 8, 429–439. [Google Scholar] [CrossRef] [PubMed]
- RIN 0970–AC63; 45 CFR Chapter XIII: Head Start Performance Standards. Administration for Children and Families: Washington, DC, USA, 2016; Volume 81.
- Yin, Z.; Liang, Y.; Howard, J.T.; Errisuriz, V.; Estrada, V.M.; Martinez, C.; Li, S.; Ullevig, S.L.; Sosa, E.; Olmstead, T. ¡ Míranos! a comprehensive preschool obesity prevention programme in low-income Latino children: 1-year results of a clustered randomised controlled trial. Public Health Nutr. 2023, 26, 476–487. [Google Scholar] [CrossRef]
- Region III Administration for Children and Families. I Am Moving, I Am Learning (IMIL): A Proactive Approach for Addressing Childhood Cbesity in Head Start Children: Summary Report of the First Two Years; U.S. Department of Health and Human Services (HHS): Washington, DC, USA, 2006.
- Ulrich, D.A.; Sanford, C.B. TGMD-2: Test of Gross Motor Development; Pro-Ed: Austin, TX, USA, 2000. [Google Scholar]
- Webster, E.K.; Ulrich, D.A. Evaluation of the psychometric properties of the test of gross motor development—Third edition. J. Mot. Learn. Dev. 2017, 5, 45–58. [Google Scholar] [CrossRef]
- Rey, E.; Carballo-Fazanes, A.; Varela-Casal, C.; Abelairas-Gómez, C.; ALFA-MOV Project Collaborators. Reliability of the test of gross motor development: A systematic review. PLoS ONE 2020, 15, e0236070. [Google Scholar] [CrossRef]
- Rolland-Cachera, M.; Deheeger, M.; Maillot, M.; Bellisle, F. Early adiposity rebound: Causes and consequences for obesity in children and adults. Int. J. Obes. 2006, 30, S11–S17. [Google Scholar] [CrossRef]
- Moon, R.C. Late adiposity rebound and the probability of developing and reversing childhood obesity. J. Pediatr. 2020, 216, 128–135.e123. [Google Scholar] [CrossRef]
- Dobell, A.; Pringle, A.; Faghy, M.A.; Roscoe, C.M. Fundamental movement skills and accelerometer-measured physical activity levels during early childhood: A systematic review. Children 2020, 7, 224. [Google Scholar] [CrossRef]
- Morgan, P.J.; Barnett, L.M.; Cliff, D.P.; Okely, A.D.; Scott, H.A.; Cohen, K.E.; Lubans, D.R. Fundamental movement skill interventions in youth: A systematic review and meta-analysis. Pediatrics 2013, 132, e1361–e1383. [Google Scholar] [CrossRef]
- Staiano, A.E.; Newton Jr, R.L.; Beyl, R.A.; Kracht, C.L.; Hendrick, C.A.; Viverito, M.; Webster, E.K. mHealth Intervention for Motor Skills: A Randomized Controlled Trial. Pediatrics 2022, 149, e2021053362. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Esteban, C.; Terry Andrés, J.; Méndez, I.; Morales, Á. Analysis of motor intervention program on the development of gross motor skills in preschoolers. Int. J. Environ. Res. Public Health 2020, 17, 4891. [Google Scholar] [CrossRef] [PubMed]
- Engel, A.C.; Broderick, C.R.; van Doorn, N.; Hardy, L.L.; Parmenter, B.J. Exploring the relationship between fundamental motor skill interventions and physical activity levels in children: A systematic review and meta-analysis. Sports Med. 2018, 48, 1845–1857. [Google Scholar] [CrossRef] [PubMed]
- Adamo, K.B.; Wilson, S.; Harvey, A.L.; Grattan, K.P.; Naylor, P.-J.; Temple, V.A.; Goldfield, G.S. Does intervening in childcare settings impact fundamental movement skill development? Med. Sci. Sports Exerc. 2016, 48, 926–932. [Google Scholar] [CrossRef]
- Palmer, K.K.; Chinn, K.M.; Robinson, L.E. Using achievement goal theory in motor skill instruction: A systematic review. Sports Med. 2017, 47, 2569–2583. [Google Scholar] [CrossRef]
- Pedersen, M.R.L.; Hansen, A.F. Interventions by caregivers to promote motor development in young children, the caregivers’ attitudes and benefits hereof: A scoping review. Int. J. Environ. Res. Public Health 2022, 19, 11543. [Google Scholar] [CrossRef]
- Veldman, S.L.; Jones, R.A.; Okely, A.D. Efficacy of gross motor skill interventions in young children: An updated systematic review. BMJ Open Sport Exerc. Med. 2016, 2, e000067. [Google Scholar] [CrossRef]
- Van Capelle, A.; Broderick, C.R.; van Doorn, N.; Ward, R.E.; Parmenter, B.J. Interventions to improve fundamental motor skills in pre-school aged children: A systematic review and meta-analysis. J. Sci. Med. Sport 2017, 20, 658–666. [Google Scholar] [CrossRef]
- Goodway, J.D.; Branta, C.F. Influence of a motor skill intervention on fundamental motor skill development of disadvantaged preschool children. Res. Q. Exerc. Sport 2003, 74, 36–46. [Google Scholar] [CrossRef]
- Robinson, L.E.; Stodden, D.F.; Barnett, L.M.; Lopes, V.P.; Logan, S.W.; Rodrigues, L.P.; D’Hondt, E. Motor competence and its effect on positive developmental trajectories of health. Sports Med. 2015, 45, 1273–1284. [Google Scholar] [CrossRef]
- Lubans, D.R.; Morgan, P.J.; Cliff, D.P.; Barnett, L.M.; Okely, A.D. Fundamental movement skills in children and adolescents: Review of associated health benefits. Sports Med. 2010, 40, 1019–1035. [Google Scholar] [CrossRef] [PubMed]
- Utesch, T.; Bardid, F.; Büsch, D.; Strauss, B. The relationship between motor competence and physical fitness from early childhood to early adulthood: A meta-analysis. Sports Med. 2019, 49, 541–551. [Google Scholar] [CrossRef] [PubMed]
- Kit, B.K.; Akinbami, L.J.; Isfahani, N.S.; Ulrich, D.A. Gross motor development in children aged 3–5 years, United States 2012. Matern. Child Health J. 2017, 21, 1573–1580. [Google Scholar] [CrossRef]
- Barnett, L.M.; Hnatiuk, J.A.; Salmon, J.; Hesketh, K.D. Modifiable factors which predict children’s gross motor competence: A prospective cohort study. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 129. [Google Scholar] [CrossRef] [PubMed]
- Valadi, S.; Gabbard, C. The effect of affordances in the home environment on children’s fine-and gross motor skills. Early Child Dev. Care 2020, 190, 1225–1232. [Google Scholar] [CrossRef]
- O’Connor, T.M.; Cerin, E.; Lee, R.E.; Parker, N.; Chen, T.-A.; Hughes, S.O.; Mendoza, J.A.; Baranowski, T. Environmental and cultural correlates of physical activity parenting practices among Latino parents with preschool-aged children: Ninos Activos. BMC Public Health 2014, 14, 707. [Google Scholar] [CrossRef]
- Moore, L.V.; Roux, A.V.D.; Evenson, K.R.; McGinn, A.P.; Brines, S.J. Availability of recreational resources in minority and low socioeconomic status areas. Am. J. Prev. Med. 2008, 34, 16–22. [Google Scholar] [CrossRef]
- Taylor, W.; Lou, D. Do all children have places to be active. In Disparities in Access to Physical Activity Environments in Racial and Ethnic Minority and Lower-Income Communities. Active Living Research: Research Synthesis; Robert Wood Johnson Foundation: Princeton, NJ, USA, 2011. [Google Scholar]
- Lopes, L.; Santos, R.; Coelho-e-Silva, M.; Draper, C.; Mota, J.; Jidovtseff, B.; Clark, C.; Schmidt, M.; Morgan, P.; Duncan, M. A narrative review of motor competence in children and adolescents: What we know and what we need to find out. Int. J. Environ. Res. Public Health 2021, 18, 18. [Google Scholar] [CrossRef]
- Adolph, K.E.; Hoch, J.E. Motor development: Embodied, embedded, enculturated, and enabling. Annu. Rev. Psychol. 2019, 70, 141–164. [Google Scholar] [CrossRef]
- Kopp, C.B. Development in the early years: Socialization, motor development, and consciousness. Annu. Rev. Psychol. 2011, 62, 165–187. [Google Scholar] [CrossRef]
- Colella, D.; Morano, M. Gross motor development and physical activity in kindergarten age children. Int. J. Pediatr. Obes. 2011, 6, 33–36. [Google Scholar] [CrossRef]
- Williams, H.G.; Pfeiffer, K.A.; Dowda, M.; Jeter, C.; Jones, S.; Pate, R.R. A field-based testing protocol for assessing gross motor skills in preschool children: The CHAMPS motor skills protocol (CMSP). Meas. Phys. Educ. Exerc. Sci. 2009, 13, 151. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.E.; Goodway, J.D. Instructional climates in preschool children who are at-risk. Part I: Object-control skill development. Res. Q. Exerc. Sport 2009, 80, 533–542. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.-H.; Hipp, J.A.; Marquet, O.; Alberico, C.; Fry, D.; Mazak, E.; Lovasi, G.S.; Robinson, W.R.; Floyd, M.F. Neighborhood characteristics associated with park use and park-based physical activity among children in low-income diverse neighborhoods in New York City. Prev. Med. 2020, 131, 105948. [Google Scholar] [CrossRef] [PubMed]
- Penilla, C.; Tschann, J.M.; Sanchez-Vaznaugh, E.V.; Flores, E.; Ozer, E.J. Obstacles to preventing obesity in children aged 2 to 5 years: Latino mothers’ and fathers’ experiences and perceptions of their urban environments. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 148. [Google Scholar] [CrossRef] [PubMed]
| Treatment Condition | Treatment Component | Activities | Implementers |
|---|---|---|---|
| Center-based Intervention | Physical activity, nutrition policy and environment |
| Classroom teachers and paraprofessionals |
| ¡Míranos! physical activity/gross motor program |
| Classroom teachers and paraprofessionals | |
| Supplemental health-education activities |
| Classroom teachers and paraprofessionals | |
| ¡Míranos! Staff-wellness program |
| All center staff | |
| Meal-pattern modification |
| Central kitchen staff | |
| Staff development and training |
| Center staff, curriculum development staff | |
| Home-based Intervention | Peer-led obesity education |
| Trained parent peer educators |
| Home visits |
| Family-service workers | |
| Comparison | “I Am Moving, I Am Learning” obesity-prevention curriculum |
| Control centers |
| Literacy education |
| Control centers |
| Variables | CBI + HBI (n = 92) | CBI (n = 100) | Control (n = 118) | Total (n = 310) | p Value 1 |
|---|---|---|---|---|---|
| Center size, n (%) | 0.01 | ||||
| Small | 57 (61.96) | 71 (71) | 61 (51.69) | 189 (60.97) | |
| Large | 35 (38.04) | 29 (29) | 57 (48.31) | 121 (39.03) | |
| Child age at baseline, yr | 0.49 | ||||
| Median (Q1, Q3) | 3.64 (3.39, 3.84) | 3.55 (3.36, 3.76) | 3.61 (3.31, 3.92) | 3.59 (3.33, 3.84) | |
| Mean ± SD | 3.6 ± 0.29 | 3.56 ± 0.26 | 3.6 ± 0.32 | 3.59 ± 0.29 | |
| Child sex, n (%) | 0.18 | ||||
| Male | 39 (42.39) | 35 (35) | 56 (47.46) | 130 (41.94) | |
| Female | 53 (57.61) | 65 (65) | 62 (52.54) | 180 (58.06) | |
| Child race/ethnicity, n (%) | 0.15 | ||||
| Non-H AA | 5 (5.43) | 10 (10) | 4 (3.39) | 19 (6.13) | |
| Hispanic | 78 (84.78) | 84 (84) | 109 (92.37) | 271 (87.42) | |
| Other | 9 (9.78) | 6 (6) | 5 (4.24) | 20 (6.45) | |
| Child with asthma, n (%) | 8 (8.7) | 15 (15) | 17 (14.41) | 40 (12.9) | 0.35 |
| Mother education, n (%) | 0.7 | ||||
| Less than a high-school diploma | 11 (11.96) | 12 (12) | 13 (11.02) | 36 (11.61) | |
| High-school diploma/GED | 42 (45.65) | 38 (38) | 54 (45.76) | 134 (43.23) | |
| College or technical-school degree | 27 (29.35) | 41 (41) | 40 (33.9) | 108 (34.84) | |
| N/A or missing | 12 (13.04) | 9 (9) | 11 (9.32) | 32 (10.32) | |
| Language spoken most often at home, n (%) | 0.63 | ||||
| English | 52 (56.52) | 62 (62) | 58 (49.15) | 172 (55.48) | |
| Spanish or other | 22 (23.91) | 22 (22) | 30 (25.42) | 74 (23.87) | |
| English and Spanish equally | 12 (13.04) | 11 (11) | 21 (17.8) | 44 (14.19) | |
| Not reported | 6 (6.52) | 5 (5) | 9 (7.63) | 20 (6.45) | |
| Parents not married, n (%) | 34 (36.96) | 35 (35) | 44 (37.29) | 113 (36.45) | 0.93 |
| Family members with history of diabetes, n (%) | 41 (44.57) | 43 (43) | 43 (36.44) | 127 (40.97) | 0.44 |
| Outcomes | CBI + HBI (n = 92) | CBI (n = 100) | Control (n = 118) | Total (n = 310) | p Value 1 |
|---|---|---|---|---|---|
| GMQ | |||||
| Baseline 2 | 87.2 ± 9.22 | 83.74 ± 12.17 | 84.31 ± 12.35 | 85.01 ± 11.47 | 0.41 |
| Posttest 3 | 95.09 ± 9.21 | 94.17 ± 9.46 | 89.25 ± 10.7 | 92.5 ± 10.21 | <0.001 * |
| Change 4 | 8.92 ± 10.68 | 9.36 ± 13.04 | 4.33 ±1 4.06 | 7.3 ± 12.96 | 0.02 * |
| Cohen’s d | 0.84 9 | 0.72 9 | 0.31 9 | ||
| Cohen’s d | 0.37 10 | 0.37 11 | |||
| Cohen’s d | −0.04 12 | ||||
| LS pctl | |||||
| Baseline 5 | 18.98 ± 15.34 | 23.78 ± 19.4 | 19.73 ± 17.1 | 20.73 ± 17.36 | 0.35 |
| Posttest 3 | 42.59 ± 22.39 | 42.37 ± 22.35 | 30.25 ± 19.89 | 37.65 ± 22.17 | <0.001 * |
| Change 6 | 25.13 ± 20.72 | 17.19 ± 23.92 | 10.2 ± 20.81 | 17.21 ± 22.54 | <0.001 * |
| Cohen’s d | 1.21 9 | 0.72 9 | 0.49 9 | ||
| Cohen’s d | 0.72 10 | 0.31 11 | |||
| Cohen’s d | 0.35 12 | ||||
| BS pctl | |||||
| Baseline 7 | 35.95 ± 19.76 | 30.64 ± 19.16 | 34.67 ± 19.84 | 33.76 ± 19.65 | 0.13 |
| Posttest 3 | 38.92 ± 19.84 | 37.36 ± 17.81 | 33.63 ± 19.73 | 36.35 ± 19.25 | 0.15 |
| Change 8 | 4.14 ± 23.48 | 5.36 ± 20.93 | −2.53 ± 24.7 | 1.97 ± 23.38 | 0.08 |
| Cohen’s d | 0.18 9 | 0.26 9 | −0.1 9 | ||
| Cohen’s d | 0.28 10 | 0.34 11 | |||
| Cohen’s d | −0.05 12 |
| Outcomes | CBI + HBI (n = 92) | CBI (n = 100) | Control (n = 118) | Difference (CBI + HBI−Control) | Difference (CBI−Control) | ||
|---|---|---|---|---|---|---|---|
| Mean Change (SE) | Mean Change (SE) | Mean Change (SE) | Difference (95% CI) | p Value | Difference (95% CI) | p Value | |
| GMQ 2 | 8.08 (1.48) * | 10.15 (1.43) * | 4.69 (1.32) * | 3.39 (−0.50, 7.28) | 0.09 ^ | 5.46 (1.64, 9.29) | 0.01 * |
| LS pctl 3 | 23.99 (2.48) * | 17.91 (2.53) * | 10.31 (2.31) * | 13.68 (7.04, 20.33) | <0.001 * | 7.60 (0.89, 14.31) | 0.03 * |
| BS pctl 4 | 3.32 (2.59) | 6.11 (2.52) * | −1.46 (2.32) | 4.78 (−2.04, 11.60) | 0.17 | 7.57 (0.86, 14.28) | 0.03 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Errisuriz, V.L.; Parra-Medina, D.; Liang, Y.; Howard, J.T.; Li, S.; Sosa, E.; Ullevig, S.L.; Estrada-Coats, V.M.; Yin, Z. ¡Miranos! An 8-Month Comprehensive Preschool Obesity Prevention Program in Low-Income Latino Children: Effects on Children’s Gross Motor Development. Int. J. Environ. Res. Public Health 2023, 20, 6974. https://doi.org/10.3390/ijerph20216974
Errisuriz VL, Parra-Medina D, Liang Y, Howard JT, Li S, Sosa E, Ullevig SL, Estrada-Coats VM, Yin Z. ¡Miranos! An 8-Month Comprehensive Preschool Obesity Prevention Program in Low-Income Latino Children: Effects on Children’s Gross Motor Development. International Journal of Environmental Research and Public Health. 2023; 20(21):6974. https://doi.org/10.3390/ijerph20216974
Chicago/Turabian StyleErrisuriz, Vanessa L., Deborah Parra-Medina, Yuanyuan Liang, Jeffrey T. Howard, Shiyu Li, Erica Sosa, Sarah L. Ullevig, Vanessa M. Estrada-Coats, and Zenong Yin. 2023. "¡Miranos! An 8-Month Comprehensive Preschool Obesity Prevention Program in Low-Income Latino Children: Effects on Children’s Gross Motor Development" International Journal of Environmental Research and Public Health 20, no. 21: 6974. https://doi.org/10.3390/ijerph20216974
APA StyleErrisuriz, V. L., Parra-Medina, D., Liang, Y., Howard, J. T., Li, S., Sosa, E., Ullevig, S. L., Estrada-Coats, V. M., & Yin, Z. (2023). ¡Miranos! An 8-Month Comprehensive Preschool Obesity Prevention Program in Low-Income Latino Children: Effects on Children’s Gross Motor Development. International Journal of Environmental Research and Public Health, 20(21), 6974. https://doi.org/10.3390/ijerph20216974






