Assessing Motor Function in Frail Older Adults in Their Home Settings: Challenges, Strategies and Recommendations
Abstract
1. Introduction
2. Materials and Methods
2.1. Data
2.1.1. Pro-Home Study Design
2.1.2. Study Context and Participant Recruitment
2.2. Lower Extremity Functional Assessment
2.2.1. Selection Criteria
- Appropriateness for the target population. We needed performance-based tests that would be feasible, safe, and acceptable for community-dwelling older adults who have difficulties with daily activities such as walking or standing up. Our preliminary and pilot studies provided our study team with hands-on experiences working with community-dwelling older adults who have difficulties with daily activities such as walking or standing up. Those studies also helped us understand our target population’s health and sociodemographic characteristics [7,14,15]. Those prior experiences helped us assess what would be feasible, safe, and acceptable for the study participants.
- Sensitivity to change and responsiveness. We needed measures that could detect a meaningful or clinically important change in lower extremity motor function within or across study participants, which could be expected of the low-intensity physical activity intervention and would be sensitive to change and responsive to the intervention in the target population [16,17]. If too easy or too difficult for the target population, performance tests could produce ceiling or floor effects, where large proportions of participants would score the minimum or maximum points possible for the performance test.
- Practicality of administration. We needed performance-based tests that would be practical for trained interviewers to administer for frail older adults in their home settings. Interviewers would need to bring whatever equipment were necessary for the tests from our research office into participants’ homes. We needed tests that (1) would minimize burden (e.g., time, exertion) on study participants and interviewers, (2) could be administered safely by the trained interviewer without formal clinical training (e.g., physical therapy training), (3) would allow participants to use assistive devices (e.g., cane, walker), if needed, in some of the lower extremity motor function tests (e.g., walking or gait speed test), (4) would not require large, heavy, or special equipment, and (5) would be relatively easy for the interviewer to score.
- Measurement validity and reliability. Our priority was to select performance tests that have been developed and validated for community-dwelling older adults with functional limitations. In particular, we needed an instrument that would validly and reliably measure lower extremity motor function targeted by two moves: Seated Step-in-Place and Ankle Point and Flex.
2.2.2. Selected Instruments
2.2.2.1. Short Physical Performance Battery
- Selection Process
- Adaptations
- Prior to each SPPB subtest, the interviewer demonstrated the subtest and asked the participant, “Do you feel safe doing the measure?” The test would be conducted only when participants felt safe doing it.
- Interviewers were trained to assess the appropriateness of participants’ footwear for SPPB subtests.
- For the chair stand subtest, interviewers were instructed to position the chair against the back of a wall, to prevent the movement of the chair.
- For the balance and gait speed subtests, interviewers were instructed to stand and walk close to the participants.
- Measurement
2.2.2.2. PHAROMM
- Selection Process
- Adaptations
- Measurement
2.3. Interviewers
2.3.1. Hiring
2.3.2. Training
- Curriculum. The interviewer training curriculum, led by the research team staff, was comprised of 30 h hands-on in-person training during the first 4 weeks. It covered topics including communicating with older adults, safety, protection of human subjects, data collection, performance-based assessments, use of technology, and role plays. New interviewers shadowed experienced interviewers and conducted assessments under supervision, prior to being certified to perform these tasks independently.
- Individualized training. Each interviewer had unique strengths. Some excelled in health literacy, and others excelled in motivating and communicating with older adults, the use of electronic devices, or addressing data quality. We identified each interviewers’ strengths and areas of growth to personalize additional training and practice.
- Co-learning. A highly experienced interviewer who worked in our pilot project that developed the AROM measurement protocol helped train the new interviewers. We intentionally recruited interviewers with complementary strengths, so that interviewers would learn from each other through role playing and discussion. For example, interviewers with clinical backgrounds helped others to correctly identify anatomical landmarks. Those who administered SPPB in other studies or had experience communicating with older adults shared their experience with other team members. Once the project matured, then we could identify a lead interviewer who could carry out certain training components independently.
- Bilingual interviewer training. Interviewers completed the English curriculum described above. Once certified in English, they completed additional practice assessments, and shadowed assessments in Spanish with a bilingual lead interviewer or research staff.
- Refresher training. We provided refresher training every 6 months during the course of the study. Refresher training varied in length, based on the topic (1 to 3 h). When our project transitioned to remote operations due to the COVID-19 pandemic, these trainings focused primarily on added administrative tasks (i.e., scanning, network set up and access, etc.).
- Continuous improvement and refinement of training materials. Updating training materials was especially important for the AROM measurement we developed. To standardize assessment procedures, we wrote and refined scripts and created training videos of the assessments being carried out.
- Ensuring competency and consistency. At the beginning of the project, the interviewer trainer (a member of the research staff) would observe interviewers administering assessments to other staff and to study participants in the home. Later on, after a lead interviewer was identified, the lead interviewer would observe other interviewers and coach them, as needed, during refresher training sessions or in study participants’ homes. We also conducted a training session in which interviewers, including the lead interviewer, measured the AROM of mock participants, and received feedback based upon the results.
2.3.3. Protocol
2.3.4. Continued Communication
2.3.5. Tools to Enhance Data Collection Experience
2.4. Other Measures and Analytic Strategy
2.4.1. Participants’ Characteristics
Sociodemographic Characteristics
Motor Function Assessment
Cognitive Function Assessment
2.4.2. Interviewer Observations
Perceived Neighborhood and Home Environment
Perceived Interview Quality
2.4.3. Analytic Strategy
3. Results
3.1. Sample Characteristics
| Demographic and Health Variables | Mean or N (%) |
|---|---|
| Age | 76 (SD = 8.7; Range 61–96) |
| Female | 86 (74.1) |
| Race/Ethnicity | |
| Black/African American | 59 (50.9) |
| Hispanic 2 | 38 (32.8) |
| Non-Hispanic White | 16 (13.8) |
| Two or more races | 3 (2.6) |
| Education | |
| No formal education | 4 (3.5) |
| Less than high school | 50 (43.1) |
| High school graduate 3 | 16 (13.8) |
| Some college | 31 (26.7) |
| College graduate or above | 12 (10.3) |
| Not married currently | 87 (75.0) |
| Live alone | 54 (46.6) |
| Equipment use in daily activities | |
| Use equipment to cross a room | 73 (64.0) |
| Use equipment to get in/out of bed | 36 (31.3) |
| Chronic conditions 4 | |
| >5 health conditions | 62 (53.4) |
| Cognition 5 | |
| Scored below 1.5 SD from the SS 6 mean in: | |
| At least 1 test 6 | 67 (57.8) |
| 1 test | 29 (25.0) |
| 2 tests | 19 (16.4) |
| 3 tests | 9 (7.8) |
| 4 tests | 10 (8.6) |
| 5 tests | 0 (0) |
| Unable to complete at least 1 test 7 | 15 (12.9) |
3.2. Short Physical Performance Battery
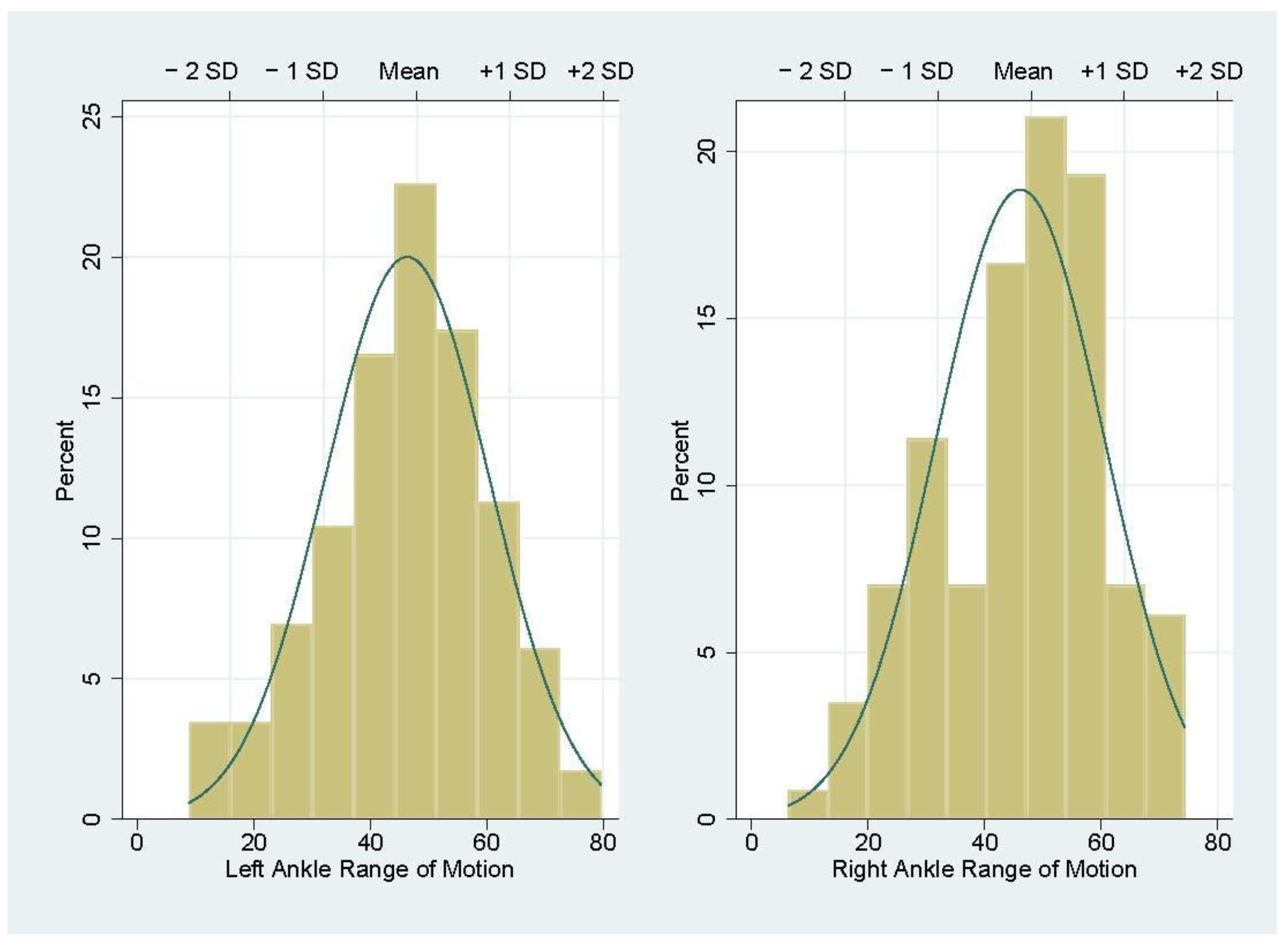
3.3. PHAROMM
3.4. Post-Visit Interviewer Perception
4. Discussion
4.1. Pro-Home Lower Extremity Motor Assessment
4.2. Recommendations
- Know your target population. Select measures appropriate for the target population, and adapt them as needed. Select measures that are more inclusive than others. For example, the SPPB gait speed subtest allows participants to use devices (i.e., cane, rolling walker, walker, rollator) which make the instrument inclusive of those who use assistive devices. Additionally, the SPPB balance tests consist of three tests that vary in the level of difficulty, so that the majority could complete at least one of the tests.
- Do not skip pretests and pilot testing. Pretesting the assessment protocol within the research team and with collaborators helps identify and address potential problems before administering to the study participants.
- Provide clear instructions and have interviewers demonstrate assessment procedures to study participants. Acknowledge that participants have different levels of educational background, health status, and cognitive or sensory function. Use a prepared script as a guide, so that interviewers can better explain and demonstrate each test. This process will help participants better understand the test procedures.
- Know the home environment in advance. Homes have different physical features (e.g., flooring, lighting, furniture, and open floor space), which may be potential safety hazards. Pro-Home interviewers used the first screening visit to assess and document the availability of space and equipment, and identified safety issues. This step helped interviewers plan for the baseline lower extremity motor function tests (e.g., identifying space for the 3 m gait speed test in the home setting, assessing the need for bringing a folding chair from the research office).
- Ask participants about their perceived safety prior to each test. Participants’ safety is a priority. An assessment should not proceed unless participants feel safe participating in it.
- Train interviewers thoroughly and continuously. Comprehensive, hands-on initial and refresher training is essential. Detailed training reveals each interviewer’s skills, strengths, and areas of growth, thus facilitating individual training plans. Having one experienced, lead interviewer train others (or newly hired interviewers) is effective and efficient.
- Develop a learning community with interviewers, office staff, students, and a senior collaborative team. Interviewers have direct contact with study participants. Valuing interviewers’ input and promoting collaboration among interviewers, office staff, and research team are critical elements for success.
- Value interviewers’ contributions and incentivize appropriately. Participants may have a wide range of motor competence, and the time spent on in-home assessment may vary, depending on participants’ health, state of mood, and the context of the assessment visit. In rare cases, interviewers may need to split an assessment session into different days. Pay interviewers by the number of hours spent on a participant instead of by case. To keep interviewers engaged throughout the studies, it is important to incentivize interviewers appropriately.
4.3. Strengths, Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Jette, A.M.; Lachman, M.; Giorgetti, M.M.; Assmann, S.F.; Harris, B.A.; Levenson, C.; Wernick, M.; Krebs, D. Exercise—It’s Never too Late: The Strong-for-Life Program. Am. J. Public Health 1999, 89, 66–72. [Google Scholar]
- Voelcker-Rehage, C. Motor-Skill Learning in Older Adults—A Review of Studies on Age-Related Differences. Eur. Rev. Aging Phys. Act. 2008, 5, 5–16. [Google Scholar] [CrossRef]
- De Cormier Plosky, W.; Ne’eman, A.; Silverman, B.C.; Strauss, D.H.; Francis, L.P.; Stein, M.A.; Bierer, B.E. Excluding People with Disabilities from Clinical Research: Eligibility Criteria Lack Clarity and Justification. Health Aff. 2022, 41, 1423–1432. [Google Scholar] [CrossRef]
- Martin Ginis, K.A.; Sharma, R.; Brears, S.L. Physical Activity and Chronic Disease Prevention: Where Is the Research on People Living with Disabilities? CMAJ 2022, 194, E338–E340. [Google Scholar] [CrossRef] [PubMed]
- Hulteen, R.M.; Terlizzi, B.; Abrams, T.C.; Sacko, R.S.; De Meester, A.; Pesce, C.; Stodden, D.F. Reinvest to Assess: Advancing Approaches to Motor Competence Measurement Across the Lifespan. Sports Med. 2023, 53, 33–50. [Google Scholar] [CrossRef] [PubMed]
- Soubra, R.; Chkeir, A.; Novella, J.-L. A Systematic Review of Thirty-One Assessment Tests to Evaluate Mobility in Older Adults. BioMed Res. Int. 2019, 2019, 1354362. [Google Scholar] [CrossRef]
- Muramatsu, N.; Yin, L.; Berbaum, M.L.; Marquez, D.X.; Jurivich, D.A.; Zanoni, J.P.; Cruz Madrid, K.Y.; Walton, S.M. Promoting Seniors’ Health with Home Care Aides: A Pilot. Gerontol. 2018, 58, 779–788. [Google Scholar] [CrossRef]
- Muramatsu, N.; Yin, L.; Berbaum, M.L.; Marquez, D.X.; Walton, S.M.; Caceres, M.; Cruz Madrid, K.Y.; Zanoni, J.P. Protocol for a Randomized Controlled Trial of Low-Intensity Physical Activity for Frail Older Adults: Promoting Seniors’ Health with Home Care Aides (Pro-Home). Contemp. Clin. Trials 2021, 104, 106362. [Google Scholar] [CrossRef]
- National Council on Aging. Evidence-Based Program Summary: Healthy Moves for Aging Well. Available online: https://www.ncoa.org/article/evidence-based-program-healthy-moves-for-aging-well (accessed on 9 April 2023).
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual, 2nd ed.; Human Kinetics: Champaign, IL, USA, 2012; ISBN 978-1-4504-1118-9. [Google Scholar]
- Community Care Program. Available online: https://ilaging.illinois.gov/programs/ccp.html (accessed on 24 June 2023).
- Coster, W.J. Making the Best Match: Selecting Outcome Measures for Clinical Trials and Outcome Studies. Am. J. Occup. Ther. 2013, 67, 162–170. [Google Scholar] [CrossRef]
- Van Swearingen, J.M.; Brach, J.S. Making Geriatric Assessment Work: Selecting Useful Measures. Phys. Ther. 2001, 81, 1233–1252. [Google Scholar] [CrossRef]
- Muramatsu, N.; Sokas, R.K.; Lukyanova, V.V.; Zanoni, J. Perceived Stress and Health among Home Care Aides: Caring for Older Clients in a Medicaid-Funded Home Care Program. J. Health Care Poor Underserved 2019, 30, 721–738. [Google Scholar] [CrossRef]
- Muramatsu, N.; Sokas, R.K.; Chakraborty, A.; Zanoni, J.P.; Lipscomb, J. Slips, Trips, and Falls Among Home Care Aides: A Mixed-Methods Study. J. Occup. Environ. Med. 2018, 60, 796–803. [Google Scholar] [CrossRef]
- Pardasaney, P.K.; Latham, N.K.; Jette, A.M.; Wagenaar, R.C.; Ni, P.; Slavin, M.D.; Bean, J.F. Sensitivity to Change and Responsiveness of Four Balance Measures for Community-Dwelling Older Adults. Phys. Ther. 2012, 92, 388–397. [Google Scholar] [CrossRef]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful Change and Responsiveness in Common Physical Performance Measures in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J. Gerontol. Ser. A: Biol. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar] [CrossRef] [PubMed]
- Guralnik, J.M.; Ferrucci, L.; Simonsick, E.M.; Salive, M.E.; Wallace, R.B. Lower-Extremity Function in Persons over the Age of 70 Years as a Predictor of Subsequent Disability. N. Engl. J. Med. 1995, 332, 556–562. [Google Scholar] [CrossRef] [PubMed]
- Bean, J.F.; Latham, N.K.; Holt, N.; Kurlinksi, L.; Ni, P.; Leveille, S.; Percac-Lima, S.; Jette, A. Which Neuromuscular Attributes Are Most Associated With Mobility Among Older Primary Care Patients? Arch. Phys. Med. Rehabil. 2013, 94, 2381–2388. [Google Scholar] [CrossRef]
- Guralnik, J. Short Physical Performance Battery (SPPB) Guide. Available online: https://sppbguide.com/ (accessed on 29 April 2023).
- Freiberger, E.; de Vreede, P.; Schoene, D.; Rydwik, E.; Mueller, V.; Frändin, K.; Hopman-Rock, M. Performance-Based Physical Function in Older Community-Dwelling Persons: A Systematic Review of Instruments. Age Ageing 2012, 41, 712–721. [Google Scholar] [CrossRef]
- Gómez, J.F.; Curcio, C.-L.; Alvarado, B.; Zunzunegui, M.V.; Guralnik, J. Validity and Reliability of the Short Physical Performance Battery (SPPB): A Pilot Study on Mobility in the Colombian Andes. Colomb. Médica 2013, 44, 165–171. [Google Scholar] [CrossRef]
- Mangione, K.K.; Craik, R.L.; McCormick, A.A.; Blevins, H.L.; White, M.B.; Sullivan-Marx, E.M.; Tomlinson, J.D. Detectable Changes in Physical Performance Measures in Elderly African Americans. Phys. Ther. 2010, 90, 921–927. [Google Scholar] [CrossRef]
- Root, M.L.; Orien, W.P.; Weed, J.H. Normal and Abnormal Function of the Foot; Clinical Biomechanics Corporation: Los Angeles, CA, USA, 1977. [Google Scholar]
- Bennell, K.L.; Talbot, R.C.; Wajswelner, H.; Techovanich, W.; Kelly, D.H.; Hall, A.J. Intra-Rater and Inter-Rater Reliability of a Weight-Bearing Lunge Measure of Ankle Dorsiflexion. Aust. J. Physiother. 1998, 44, 175–180. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Tiedemann, A.; Kwan, M.M.-S.; Latt, M.D.; Sherrington, C.; Lord, S.R. Reliability of Clinical Tests of Foot and Ankle Characteristics in Older People. J. Am. Podiatr. Med. Assoc. 2003, 93, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Weintraub, S.; Dikmen, S.S.; Heaton, R.K.; Tulsky, D.S.; Zelazo, P.D.; Bauer, P.J.; Carlozzi, N.E.; Slotkin, J.; Blitz, D.; Wallner-Allen, K.; et al. Cognition Assessment Using the NIH Toolbox. Neurology 2013, 80, S54–S64. [Google Scholar] [CrossRef]
- Cole, K.R.; Yen, C.-L.; Dudley-Javoroski, S.; Shields, R.K. NIH Toolbox Cognition Battery in Young and Older Adults: Reliability and Relationship to Adiposity and Physical Activity. J. Geriatr. Phys. Ther. 2021, 44, 51–59. [Google Scholar] [CrossRef]
- Mungas, D.; Heaton, R.; Tulsky, D.; Zelazo, P.D.; Slotkin, J.; Blitz, D.; Lai, J.-S.; Gershon, R. Factor Structure, Convergent Validity, and Discriminant Validity of the NIH Toolbox Cognitive Health Battery (NIHTB-CHB) in Adults. J. Int. Neuropsychol. Soc. 2014, 20, 579–587. [Google Scholar] [CrossRef] [PubMed]
- Weintraub, S.; Dikmen, S.S.; Heaton, R.K.; Tulsky, D.S.; Zelazo, P.D.; Slotkin, J.; Carlozzi, N.E.; Bauer, P.J.; Wallner-Allen, K.; Fox, N.; et al. The Cognition Battery of the NIH Toolbox for Assessment of Neurological and Behavioral Function: Validation in an Adult Sample. J. Int. Neuropsychol. Soc. 2014, 20, 567–578. [Google Scholar] [CrossRef]
- Scott, E.P.; Sorrell, A.; Benitez, A. Psychometric Properties of the NIH Toolbox Cognition Battery in Healthy Older Adults: Reliability, Validity, and Agreement with Standard Neuropsychological Tests. J. Int. Neuropsychol. Soc. 2019, 25, 857–867. [Google Scholar] [CrossRef]
- StataCorp Stata Statistical Software, Release 17; StataCorp LLC.: College Station, TX, USA, 2021.
- Callahan, C.M.; Unverzagt, F.W.; Hui, S.L.; Perkins, A.J.; Hendrie, H.C. Six-Item Screener to Identify Cognitive Impairment among Potential Subjects for Clinical Research. Med. Care 2002, 40, 771–781. [Google Scholar] [CrossRef]
- Teng, E.L.; Chui, H.C. The Modified Mini-Mental State (3MS) Examination. J. Clin. Psychiatry 1987, 48, 314–318. [Google Scholar] [PubMed]
- Jak, A.J.; Bondi, M.W.; Delano-Wood, L.; Wierenga, C.; Corey-Bloom, J.; Salmon, D.P.; Delis, D.C. Quantification of Five Neuropsychological Approaches to Defining Mild Cognitive Impairment. Am. J. Geriatr. Psychiatry 2009, 17, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Chaudhry, S.; Jin, L.; Meltzer, D. Use of a Self-Report-Generated Charlson Comorbidity Index for Predicting Mortality. Med. Care 2005, 43, 607. [Google Scholar] [CrossRef]
- Pahor, M.; Blair, S.N.; Espeland, M.; Fielding, R.; Gill, T.M.; Guralnik, J.M.; Hadley, E.C.; King, A.C.; Kritchevsky, S.B.; Maraldi, C.; et al. Effects of a Physical Activity Intervention on Measures of Physical Performance: Results of the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) Study. J. Gerontol. A Biol. Sci. Med. Sci. 2006, 61, 1157–1165. [Google Scholar] [CrossRef] [PubMed]
- Kudelka, J.; Geritz, J.; Welzel, J.; Hildesheim, H.; Maetzler, C.; Emmert, K.; Niemann, K.; Hobert, M.A.; Pilotto, A.; Bergmann, P.; et al. What Contributes Most to the SPPB and Its Subscores in Hospitalized Geriatric Patients: An ICF Model-Based Approach. BMC Geriatr. 2022, 22, 668. [Google Scholar] [CrossRef]
- Quadri, P.; Tettamanti, M.; Bernasconi, S.; Trento, F.; Loew, F. Lower Limb Function as Predictor of Falls and Loss of Mobility with Social Repercussions One Year after Discharge among Elderly Inpatients. Aging Clin. Exp. Res. 2005, 17, 82–89. [Google Scholar] [CrossRef]
- Brockett, C.L.; Chapman, G.J. Biomechanics of the Ankle. Orthop. Trauma 2016, 30, 232–238. [Google Scholar] [CrossRef]
- Jung, H.; Yamasaki, M. Association of Lower Extremity Range of Motion and Muscle Strength with Physical Performance of Community-Dwelling Older Women. J. Physiol. Anthropol. 2016, 35, 30. [Google Scholar] [CrossRef]
- Mecagni, C.; Smith, J.P.; Roberts, K.E.; O’Sullivan, S.B. Balance and Ankle Range of Motion in Community-Dwelling Women Aged 64 to 87 Years: A Correlational Study. Phys. Ther. 2000, 80, 1004–1011. [Google Scholar] [CrossRef]
- Takeuchi, K.; Takemura, M.; Nakamura, M.; Tsukuda, F.; Miyakawa, S. Effects of Active and Passive Warm-Ups on Range of Motion, Strength, and Muscle Passive Properties in Ankle Plantarflexor Muscles. J. Strength Cond. Res. 2021, 35, 141. [Google Scholar] [CrossRef]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short Physical Performance Battery and All-Cause Mortality: Systematic Review and Meta-Analysis. BMC Med. 2016, 14, 215. [Google Scholar] [CrossRef]
- Vasunilashorn, S.; Coppin, A.K.; Patel, K.V.; Lauretani, F.; Ferrucci, L.; Bandinelli, S.; Guralnik, J.M. Use of the Short Physical Performance Battery Score to Predict Loss of Ability to Walk 400 Meters: Analysis from the InCHIANTI Study. J. Gerontol. Ser. A 2009, 64A, 223–229. [Google Scholar] [CrossRef] [PubMed]
- Menz, H.B.; Morris, M.E.; Lord, S.R. Foot and Ankle Risk Factors for Falls in Older People: A Prospective Study. J. Gerontol. Ser. A 2006, 61, 866–870. [Google Scholar] [CrossRef] [PubMed]
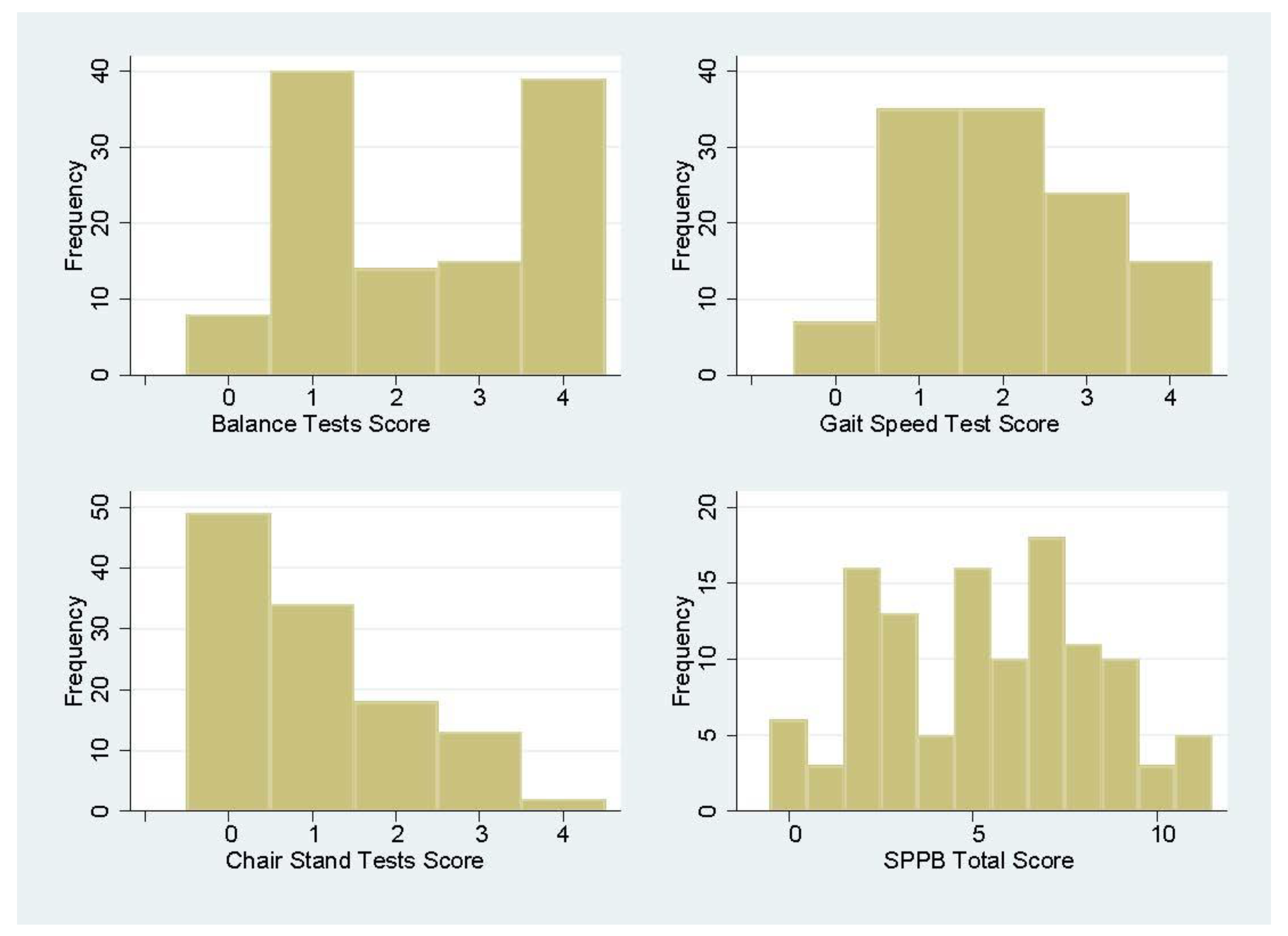
| Short Physical Performance Battery | Mean or N (%) |
|---|---|
| Missing Data | 0 (0) |
| Attempted Short Physical Performance Battery | |
| All tests | 55 (47.4) |
| Balance: Side-by-side test | 108 (93.1) |
| Semi-tandem test | 85 (73.3) |
| Tandem test | 67 (57.8) |
| Gait speed test (3 m walk) 1 | 109 (94.0) |
| Chair stand: Single stand | 75 (64.6) |
| Repeated chair stand | 70 (60.3) |
| Short Physical Performance Battery Scores | |
| Balance | 2.3 (SD = 1.4; Range 0–4) |
| Gait speed | 2.0 (SD = 1.1; Range 0–4) |
| Chair stand | 1.0 (SD = 1.1; Range 0–4) |
| Total | 5.4 (SD = 2.9; Range 0–11) |
| Neighborhood Environment and Home Settings | N (%) |
|---|---|
| Neighborhood safety | |
| Very safe | 77 (67.0) |
| Somewhat safe | 36 (31.3) |
| Not at all safe | 2 (1.7) |
| Home settings | |
| Not clean | 19 (17.4) |
| Overcrowded with furniture or objects | 13 (11.2) |
| No space for 3 m gait speed test | 5 (4.3) |
| No chair available for physical performance tests | 35 (30.2) |
| No table accessible for assessments | 27 (23.3) |
| Lighting conditions inadequate for assessments | 1 (0.9) |
| Need for a second interviewer for baseline | 10 (8.6) |
| Interviewer Observations | N (%) |
|---|---|
| Baseline assessment experience | |
| High or adequate quality | 112 (96.6) |
| Presence of others (non-participants) during visit | 76 (65.5) |
| Interviewers’ perception of participants | |
| Good or excellent understanding of questions | 107 (92.2) |
| Enjoyed the baseline assessment session 1 | 115 (99.1) |
| Assessment seemed tiring for participants (a little to very 2) | 61 (53.6) |
| Difficulty remembering questions (a little to some 3) | 44 (37.9) |
| Difficulty hearing (a little to a lot 4) | 24 (21.7) |
| Required frequent repetition of questions | 14 (12.1) |
| Appeared strained by leaning forward and/or watching interviewer’s lips very carefully | 4 (3.5) |
| Failed to react to interviewer’s questions and comments, if not watching interviewer’s lips | 2 (1.7) |
| Anticipated Challenges | Pro-Home Strategies | Recommendations |
|---|---|---|
| There are few guidelines for selecting motor function measures appropriate for frail older adults who have difficulties walking or standing. | Define selection criteria. Conduct literature review. Train interviewers. Pretest and pilot measurement protocols. | Know your target population. Do not skip pretests and pilot testing. |
| Administering motor function assessment among frail older adults is challenging, because they tend to have physical and cognitive limitations. | Develop and adapt protocol. Accommodate participants’ needs. Train interviewers. | Provide clear instructions and have interviewers demonstrate assessment procedures to study participants. |
| Home environments are potentially unfit for motor function assessment. | Assess home environment prior to the assessment visit. Bring standard equipment to assessment visit. | Know the home environment in advance. Ask participants about their perceived safety prior to each test. |
| Interviewers may encounter variations in older adults’ functional competence and home environment; the time and effort needed for each assessment visit may vary. | Identify interviewers’ skillset needed. Provide training and communicate with interviewers continuously. Pay interviewers by hour instead of by case. | Train interviewers thoroughly and continuously. Develop a learning community. Value interviewers’ contributions and incentivize appropriately. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yin, L.; Caceres, M.; Skowronski, J.; Muramatsu, N. Assessing Motor Function in Frail Older Adults in Their Home Settings: Challenges, Strategies and Recommendations. Int. J. Environ. Res. Public Health 2023, 20, 6515. https://doi.org/10.3390/ijerph20156515
Yin L, Caceres M, Skowronski J, Muramatsu N. Assessing Motor Function in Frail Older Adults in Their Home Settings: Challenges, Strategies and Recommendations. International Journal of Environmental Research and Public Health. 2023; 20(15):6515. https://doi.org/10.3390/ijerph20156515
Chicago/Turabian StyleYin, Lijuan, Maria Caceres, Jordan Skowronski, and Naoko Muramatsu. 2023. "Assessing Motor Function in Frail Older Adults in Their Home Settings: Challenges, Strategies and Recommendations" International Journal of Environmental Research and Public Health 20, no. 15: 6515. https://doi.org/10.3390/ijerph20156515
APA StyleYin, L., Caceres, M., Skowronski, J., & Muramatsu, N. (2023). Assessing Motor Function in Frail Older Adults in Their Home Settings: Challenges, Strategies and Recommendations. International Journal of Environmental Research and Public Health, 20(15), 6515. https://doi.org/10.3390/ijerph20156515






