Presence of Depression Is Associated with Functional Impairment in Middle-Aged and Elderly Chinese Adults with Vascular Disease/Diabetes Mellitus—A Cross-Sectional Study
Abstract
1. Introduction
2. Methods
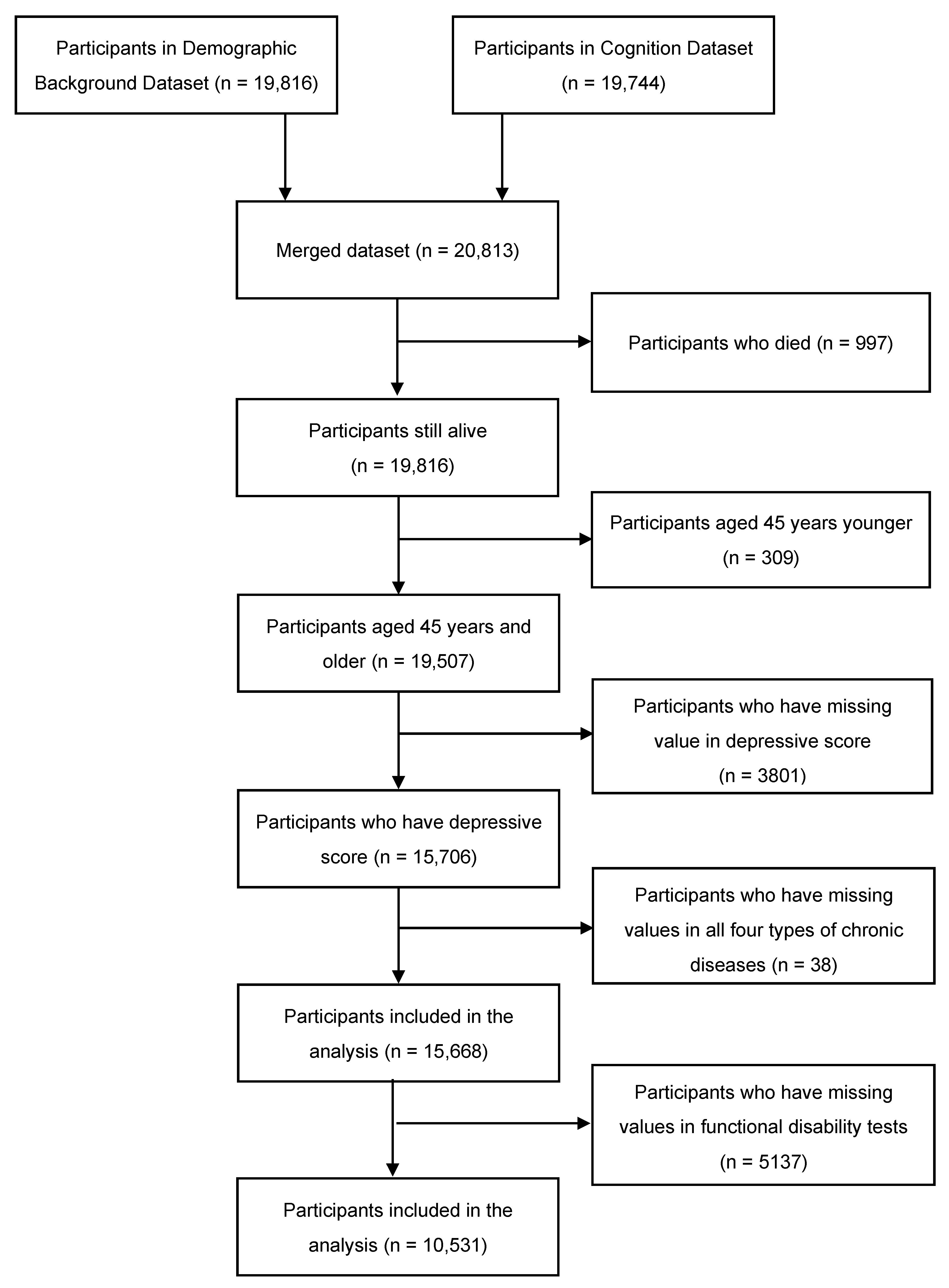
2.1. Subjects
2.2. Measures
2.2.1. Vascular Diseases/Diabetes Mellitus and Depression
2.2.2. Functional Impairment
2.2.3. Covariates
2.3. Statistical Analysis
3. Results
3.1. Sociodemographic Characteristics of Subjects
3.2. The Association between Depression and Vascular Diseases/Diabetes Mellitus
3.3. Functional Impairment According to Groups
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cherbuin, N.; Kim, S.; Anstey, K.J. Dementia risk estimates associated with measures of depression: A systematic review and meta-analysis. BMJ Open 2015, 5, e008853. [Google Scholar] [CrossRef]
- Löwe, B.; Spitzer, R.L.; Williams, J.B.; Mussell, M.; Schellberg, D.; Kroenke, K. Depression, anxiety and somatization in primary care: Syndrome overlap and functional impairment. Gen. Hosp. Psychiatry 2008, 30, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Manning, K.J.; Preciado-Pina, J.; Wang, L.; FitzGibbon, K.; Chan, G.; Steffens, D.C. Cognitive variability, brain aging, and cognitive decline in late-life major depression. Int. J. Geriatr. Psychiatry 2020, 36, 665–676. [Google Scholar] [CrossRef] [PubMed]
- The Emerging Risk Factors Collaboration; Sarwar, N.; Gao, P.; Seshasai, S.R.; Gobin, R.; Kaptoge, S.; Di Angelantonio, E.; Ingelsson, E.; Lawlor, D.A.; Selvin, E.; et al. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: A collaborative meta-analysis of 102 prospective studies. Lancet 2010, 375, 2215–2222. [Google Scholar] [CrossRef] [PubMed]
- Frasure-Smith, N.; Lespérance, F. Depression and cardiac risk: Present status and future directions. Heart 2009, 96, 173–176. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S.; Meyers, B.S.; Young, R.C.; Campbell, S.; Silbersweig, D.; Charlson, M. ‘Vascular Depression’ Hypothesis. Arch. Gen. Psychiatry 1997, 54, 915–922. [Google Scholar] [CrossRef]
- Thomas, A. Depression and vascular disease: What is the relationship? J. Affect. Disord. 2004, 79, 81–95. [Google Scholar] [CrossRef]
- Larson, S.L.; Owens, P.L.; Ford, D.; Eaton, W. Depressive Disorder, Dysthymia, and Risk of Stroke: Thirteen-year follow-up from the Baltimore epidemiologic catchment area study. Stroke 2001, 32, 1979–1983. [Google Scholar] [CrossRef]
- Meijer, A.; Conradi, H.J.; Bos, E.H.; Thombs, B.D.; van Melle, J.P.; de Jonge, P. Prognostic association of depression following myocardial infarction with mortality and cardiovascular events: A meta-analysis of 25 years of research. Gen. Hosp. Psychiatry 2011, 33, 203–216. [Google Scholar] [CrossRef]
- Knopman, D.; Boland, L.; Mosley, T.; Howard, G.; Liao, D.; Szklo, M.; McGovern, P.; Folsom, A. Cardiovascular risk factors and cognitive decline in middle-aged adults. Neurology 2001, 56, 42–48. [Google Scholar] [CrossRef]
- Ballard, C.; McKeith, I.; O’Brien, J.; Kalaria, R.; Jaros, E.; Ince, P.; Perry, R. Neuropathological Substrates of Dementia and Depression in Vascular Dementia, with a Particular Focus on Cases with Small Infarct Volumes. Dement. Geriatr. Cogn. Disord. 2000, 11, 59–65. [Google Scholar] [CrossRef] [PubMed]
- den Ouden, M.E.M.; Schuurmans, M.J.; Mueller-Schotte, S.; Bots, M.L.; van der Schouw, Y. Do subclinical vascular abnormalities precede impaired physical ability and ADL disability? Exp. Gerontol. 2014, 58, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Connolly, D.; Garvey, J.; McKee, G. Factors associated with ADL/IADL disability in community dwelling older adults in the Irish longitudinal study on ageing (TILDA). Disabil. Rehabil. 2016, 39, 809–816. [Google Scholar] [CrossRef] [PubMed]
- Lestari, S.K.; Ng, N.; Kowal, P.; Santosa, A. Diversity in the Factors Associated with ADL-Related Disability among Older People in Six Middle-Income Countries: A Cross-Country Comparison. Int. J. Environ. Res. Public Health 2019, 16, 1341. [Google Scholar] [CrossRef]
- Köhler, S.; Buntinx, F.; Palmer, K.; van den Akker, M. Depression, Vascular Factors, and Risk of Dementia in Primary Care: A Retrospective Cohort Study. J. Am. Geriatr. Soc. 2015, 63, 692–698. [Google Scholar] [CrossRef]
- Leys, D.; Hénon, H.; Pasquier, F. White Matter Changes and Poststroke Dementia. Dement. Geriatr. Cogn. Disord. 1998, 9, 25–29. [Google Scholar] [CrossRef] [PubMed]
- Rosen, W.G. Verbal fluency in aging and dementia. J. Clin. Neuropsychol. 1980, 2, 135–146. [Google Scholar] [CrossRef]
- Brach, J.S.; Solomon, C.; Naydeck, B.L.; Sutton-Tyrrell, K.; Enright, P.L.; Jenny, N.S.; Chaves, P.M.; Newman, A.B.; for the Cardiovascular Health Study Research Group. Incident Physical Disability in People with Lower Extremity Peripheral Arterial Disease: The Role of Cardiovascular Disease. J. Am. Geriatr. Soc. 2008, 56, 1037–1044. [Google Scholar] [CrossRef]
- Fong, J.H. Disability incidence and functional decline among older adults with major chronic diseases. BMC Geriatr. 2019, 19, 323. [Google Scholar] [CrossRef]
- Giltay, E.J.; Zitman, F.G.; Kromhout, D. Cardiovascular Risk Profile and Subsequent Disability and Mental Well-being: The Zutphen Elderly Study. Am. J. Geriatr. Psychiatry 2008, 16, 874–882. [Google Scholar] [CrossRef]
- Kamper, A.M.; Stott, D.J.; Hyland, M.; Murray, H.M.; Ford, I. Predictors of functional decline in elderly people with vascular risk factors or disease. Age Ageing 2005, 34, 450–455. [Google Scholar] [CrossRef] [PubMed]
- Luo, H.; Li, J.; Zhang, Q.; Cao, P.; Ren, X.; Fang, A.; Liao, H.; Liu, L. Obesity and the onset of depressive symptoms among middle-aged and older adults in China: Evidence from the CHARLS. BMC Public Health 2018, 18, 909. [Google Scholar] [CrossRef] [PubMed]
- Björgvinsson, T.; Kertz, S.J.; Bigda-Peyton, J.S.; McCoy, K.L.; Aderka, I.M. Psychometric Properties of the CES-D-10 in a Psychiatric Sample. Assessment 2013, 20, 429–436. [Google Scholar] [CrossRef]
- Katz, S.; Ford, A.B.; Moskowitz, R.W.; Jackson, B.A.; Jaffe, M.W. Studies of Illness in the Aged. The index of Adl: A standardized measure of biological and phychological funcation. JAMA 1963, 185, 914–919. [Google Scholar] [CrossRef] [PubMed]
- Lawton, M.P.; Brody, E.M. Assessment of older people: Self-maintaining and instrumental activities of daily living. Gerontologist 1969, 9, 179–186. [Google Scholar] [CrossRef]
- Lee, Y.; Smofsky, A.; Nykoliation, P.; Allain, S.J.; Lewis-Daly, L.; Schwartz, J.; Pollack, J.H.; Tarride, J.-E.; McIntyre, R.S. Cognitive Impairment Mediates Workplace Impairment in Adults with Type 2 Diabetes Mellitus: Results from the Motivaction Study. Can. J. Diabetes 2018, 42, 289–295. [Google Scholar] [CrossRef]
- Wong, E.; Backholer, K.; Gearon, E.; Harding, J.; Freak-Poli, R.; Stevenson, C.; Peeters, A. Diabetes and risk of physical disability in adults: A systematic review and meta-analysis. Lancet Diabetes Endocrinol. 2013, 1, 106–114. [Google Scholar] [CrossRef]
- Kuo, H.-K.; Al Snih, S.; Kuo, Y.-F.; Raji, M.A. Chronic inflammation, albuminuria, and functional disability in older adults with cardiovascular disease: The National Health and Nutrition Examination Survey, 1999–2008. Atherosclerosis 2012, 222, 502–508. [Google Scholar] [CrossRef]
- Armenian, H.K.; Pratt, L.A.; Gallo, J.; Eaton, W.W. Psychopathology as a Predictor of Disability: A Population-based Follow-up Study in Baltimore, Maryland. Am. J. Epidemiol. 1998, 148, 269–275. [Google Scholar] [CrossRef]
- McIntyre, R.S.; Cha, D.S.; Soczynska, J.K.; Woldeyohannes, H.O.; Gallaugher, L.A.; Kudlow, P.; Alsuwaidan, M.; Baskaran, A. Cognitive deficits and functional outcomes in major depressive disorder: Determinants, substrates, and treatment interventions. Depress. Anxiety 2013, 30, 515–527. [Google Scholar] [CrossRef]
- Steffens, D.C.; Potter, G.G. Geriatric depression and cognitive impairment. Psychol. Med. 2007, 38, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Alexopoulos, G.S. Mechanisms and treatment of late-life depression. Transl. Psychiatry 2019, 9, 188. [Google Scholar] [CrossRef] [PubMed]
- Rosenblat, J.D.; Cha, D.S.; Mansur, R.B.; McIntyre, R.S. Inflamed moods: A review of the interactions between inflammation and mood disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2014, 53, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Taylor, W.D.; Aizenstein, H.J.; Alexopoulos, G.S. The vascular depression hypothesis: Mechanisms linking vascular disease with depression. Mol. Psychiatry 2013, 18, 963–974. [Google Scholar] [CrossRef]
| Characteristics | Total | Hypertension | Diabetes Mellitus | Myocardial Infarction | Stroke | Unexposed ** |
|---|---|---|---|---|---|---|
| Total (n, %) | 10,531 | 1692 (14.6) | 834 (5.8) | 1082 (7.9) | 691 (4.5) | 4519 (42.9) |
| Age (years; Mean ± SD) | 61.8 ± 9.4 | 62.0 ± 8.8 | 62.4 ± 9.0 | 65.1 ± 8.2 | 60.5 ± 9.3 | |
| Gender (n, %) | ||||||
| Male | 899 (53.1) | 395 (47.4) | 464 (42.9) | 360 (52.1) | 1917 (42.4) | |
| Female | 793 (46.9) | 439 (52.6) | 618 (57.1) | 331 (47.9) | 2602 (57.6) | |
| Education level (n, %) | ||||||
| Illiterate | 315 (18.6) | 172 (20.6) | 215 (19.9) | 147 (21.3) | 998 (22.1) | |
| Primary school and below | 752 (44.4) | 354 (42.5) | 453 (41.9) | 302 (43.7) | 2132 (47.2) | |
| Junior high school or above | 615 (37.0) | 308 (36.9) | 414 (38.2) | 242 (35.0) | 1389 (30.7) | |
| Mariral status (n, %) | ||||||
| Married/cohabitating | 1458 (86.2) | 733 (87.9) | 937 (86.6) | 566 (81.9) | 3959 (87.6) | |
| Divorced/separated/widowed/never married | 234 (13.8) | 101 (12.1) | 145 (13.4) | 125 (18.1) | 560 (12.4) | |
| Drinking * (n, %) | ||||||
| Drink more than once a month | 480 (28.4) | 190 (22.8) | 232 (21.5) | 131 (19.0) | 1146 (25.4) | |
| Drink less than once a month | 1212 (71.6) | 644 (77.2) | 850 (78.5) | 560 (81) | 3373 (74.6) | |
| Smoking (n, %) | ||||||
| Yes | 489 (28.9) | 196 (23.5) | 242 (22.4) | 158 (22.9) | 1219 (27.0) | |
| No | 898 (53.1) | 508 (60.9) | 664 (61.4) | 373 (54.0) | 2787 (61.7) | |
| Quit | 305 (18.0) | 130 (15.6) | 176 (16.2) | 160 (23.1) | 513 (11.4) | |
| Depression (n, %) | ||||||
| Yes | 710 (42.0) | 354 (42.4) | 503 (46.5) | 346 (50.1) | 1897 (42.0) | |
| No | 982 (58.0) | 480 (57.6) | 579 (53.5) | 345 (49.9) | 2622 (58.0) |
| Vascular Diseases | Depressive Scores (Mean ± SD) | OR * (95% CI) | ||
|---|---|---|---|---|
| Have Diseases | Not Have Diseases | t | ||
| Hypertension | 9.17 ± 0.17 | 8.03 ± 0.06 | 6.75 *** | 1.39 (1.25, 1.54) *** |
| Diabetes mellitus | 9.56 ± 0.25 | 8.29 ± 0.05 | 5.5 *** | 1.32 (1.14, 1.52) *** |
| Myocardial infarction | 10.04 ± 0.21 | 8.01 ± 0.06 | 10.09 *** | 1.67 (1.48, 1.90) *** |
| Stroke | 10.87 ± 0.27 | 8.28 ± 0.05 | 10.3 *** | 1.80 (1.54, 2.10) *** |
| Unexposed | 10.32 ± 0.17 | 9.16 ± 0.01 | 5.89 *** | 1.32 (1.18, 1.48) *** |
| Functional Assessment (Independent n, %) | Total | Hypertension | Diabetes Mellitus | Myocardial Infarction | Stroke | Unexposed |
|---|---|---|---|---|---|---|
| 10,531 | n = 1256 | n = 644 | n = 899 | n = 590 | n = 4519 | |
| Activity of daily living (n, %) | ||||||
| Total independent | 924 (73.6) | 455 (70.7) | 630 (70.1) | 344 (58.3) | 3738 (82.7) | |
| Dressing | 1149 (91.5) | 586 (91.0) | 827 (92.0) | 494 (83.7) | 4272 (94.5) | |
| Bathing or showering | 1118 (89.0) | 573 (89.0) | 808 (89.9) | 465 (78.8) | 4277 (94.6) | |
| Eating | 1228 (97.8) | 625 (97.0) | 873 (97.1) | 546 (92.5) | 4455 (98.6) | |
| Getting into or out of bed | 1143 (91.0) | 575 (89.3) | 817 (90.9) | 495 (83.9) | 4289 (94.9) | |
| Using the toilet | 1044 (83.1) | 531 (82.5) | 720 (80.1) | 437 (74.1) | 4070 (90.1) | |
| Controlling urination and defecation | 1186 (94.4) | 612 (95.0) | 834 (92.8) | 527 (89.3) | 4371 (96.7) | |
| Instrumental activities of daily living (n, %) | ||||||
| Total independent | 820 (65.3) | 403 (62.6) | 581 (64.6) | 284 (48.1) | 3451 (76.4) | |
| Household chores | 1012 (80.6) | 500 (77.6) | 716 (79.6) | 393 (66.6) | 4028 (89.1) | |
| Preparing hot meals | 1080 (86.0) | 547 (84.9) | 782 (87.0) | 438 (74.2) | 4183 (92.6) | |
| Shopping for groceries | 1123 (89.4) | 571 (88.7) | 795 (88.4) | 469 (79.5) | 4275 (94.6) | |
| Making phone calls | 1057 (84.2) | 545 (84.6) | 761 (84.6) | 463 (78.5) | 3961 (87.7) | |
| Taking medications | 1178 (93.8) | 593 (92.1) | 829 (92.2) | 524 (88.8) | 4363 (96.5) | |
| Managing money | 1097 (87.3) | 545 (84.6) | 764 (85.0) | 449 (76.1) | 4110 (90.9) | |
| Diseases | UOR (95% CI) | p-Value | AOR * (95% CI) | p-Value |
|---|---|---|---|---|
| Activity of daily living (ADL) | ||||
| Hypertentiosn | 1.45 (1.26, 1.67) | <0.001 | 1.37 (1.19, 1.58) | <0.001 |
| Diabetes | 1.45 (1.22, 1.73) | <0.001 | 1.43 (1.19, 1.72) | <0.001 |
| Myocardial infarction | 1.62 (1.39, 1.89) | <0.001 | 1.57 (1.35, 1.84) | <0.001 |
| Stroke | 2.54 (2.14, 3.01) | <0.001 | 2.32 (1.95, 2.77) | <0.001 |
| Exposed | 1.63 (1.42, 1.86) | <0.001 | 1.55 (1.35, 1.78) | <0.001 |
| Depression | 2.91 (2.65, 3.20) | <0.001 | 2.95 (2.68, 3.25) | <0.001 |
| Instrumental activity of daily living (IADL) | ||||
| Hypertension | 1.48 (1.30, 1.68) | <0.001 | 1.43 (1.25, 1.64) | <0.001 |
| Diabetes | 1.44 (1.22, 1.70) | <0.001 | 1.43 (1.20, 1.70) | <0.001 |
| Myocardial infarction | 1.43 (1.24, 1.66) | <0.001 | 1.41 (1.21, 1.64) | <0.001 |
| Stroke | 2.68 (2.27, 3.17) | <0.001 | 2.57 (2.15, 3.06) | <0.001 |
| Exposed | 1.58 (1.40, 1.79) | <0.001 | 1.55 (1.37, 1.77) | <0.001 |
| Depression | 3.10 (2.85, 3.38) | <0.001 | 3.10 (2.83, 3.40) | 0.001 |
| Variables | n | UOR (95% CI) | p-Value | AOR * (95% CI) | p-Value |
|---|---|---|---|---|---|
| Depression by hypertension | |||||
| Both | 620 | 4.16 (3.43, 5.04) | <0.001 | 3.86 (3.03, 4.93) | <0.001 |
| Depression only | 2687 | 3.01 (2.64, 3.44) | <0.001 | 2.93 (2.47, 3.46) | <0.001 |
| Hypertension only | 636 | 1.42 (1.13, 1.80) | 0.003 | 1.37 (1.01, 1.85) | 0.042 |
| Unexposed | 3410 | REF | REF | ||
| Depression by diabetes | |||||
| Both | 322 | 4.20 (3.32, 5.32) | <0.001 | 3.80 (2.84, 5.08) | <0.001 |
| Depression only | 4007 | 2.87 (2.59, 3.18) | <0.001 | 2.82 (2.46, 3.23) | <0.001 |
| Diabetes only | 322 | 1.30 (0.97, 1.75) | 0.083 | 1.30 (0.90, 1.89) | 0.169 |
| Unexposed | 4945 | REF | REF | ||
| Depression by myocardial infarction | |||||
| Both | 459 | 3.95 (3.21, 4.86) | <0.001 | 3.60 (2.79, 4.66) | <0.001 |
| Depression only | 3433 | 2.85 (2.55, 3.19) | <0.001 | 2.78 (2.40, 3.21) | <0.001 |
| Myocardial infarction only | 440 | 1.78 (1.40, 2.27) | <0.001 | 1.65 (1.21, 2.25) | 0.001 |
| Unexposed | 4458 | REF | REF | ||
| Depression by stroke | |||||
| Both | 317 | 7.19 (5.69, 9.08) | <0.001 | 6.62 (4.91, 8.91) | <0.001 |
| Depression only | 4335 | 2.87 (2.60, 3.17) | <0.001 | 2.80 (2.45, 3.18) | <0.001 |
| Stroke only | 273 | 2.32 (1.76, 3.07) | <0.001 | 2.32 (1.61, 3.34) | <0.001 |
| Unexposed | 5359 | REF | REF | ||
| Variables | n | UOR (95% CI) | p-Value | AOR *(95% CI) | p-Value |
|---|---|---|---|---|---|
| Depression by hypertension | |||||
| Both | 620 | 4.47 (3.73, 5.36) | <0.001 | 4.30 (3.55, 5.19) | <0.001 |
| Depression only | 2687 | 3.17 (2.82, 3.57) | <0.001 | 3.17 (2.80, 3.59) | <0.001 |
| Hypertension only | 636 | 1.45 (1.18, 1.78) | <0.001 | 1.38 (1.12, 1.72) | 0.003 |
| Unexposed | 3410 | REF | REF | ||
| Depression by diabetes | |||||
| Both | 322 | 4.50 (3.58, 5.66) | <0.001 | 4.38 (3.44, 5.58) | <0.001 |
| Depression only | 4007 | 2.99 (2.72, 3.29) | <0.001 | 2.30 (2.72, 3.31) | <0.001 |
| Diabetes only | 322 | 1.25 (0.95, 1.63) | 0.108 | 1.27 (0.96, 1.68) | 0.092 |
| Unexposed | 4945 | REF | REF | ||
| Depression by myocardial infarction | |||||
| Both | 459 | 4.19 (3.43, 5.10) | <0.001 | 4.14 (3.37, 5.10) | <0.001 |
| Depression only | 3433 | 2.91 (2.63, 3.22) | <0.001 | 2.94 (2.64, 3.27) | <0.001 |
| Myocardial infarction only | 440 | 1.22 (0.96, 1.55) | 0.104 | 1.20 (0.93, 1.53) | 0.155 |
| Unexposed | 4458 | REF | REF | ||
| Depression by stroke | |||||
| Both | 317 | 8.16 (6.41, 10.38) | <0.001 | 7.72 (6.00, 9.92) | <0.001 |
| Depression only | 4335 | 3.08 (2.81, 3.38) | <0.001 | 3.07 (2.79, 3.38) | <0.001 |
| Stroke only | 273 | 2.54 (1.97, 3.28) | <0.001 | 2.36 (1.81, 3.08) | <0.001 |
| Unexposed | 5359 | REF | REF | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhao, Y.; Zhang, Y.; Teopiz, K.M.; Lui, L.M.W.; McIntyre, R.S.; Cao, B. Presence of Depression Is Associated with Functional Impairment in Middle-Aged and Elderly Chinese Adults with Vascular Disease/Diabetes Mellitus—A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 1602. https://doi.org/10.3390/ijerph20021602
Zhao Y, Zhang Y, Teopiz KM, Lui LMW, McIntyre RS, Cao B. Presence of Depression Is Associated with Functional Impairment in Middle-Aged and Elderly Chinese Adults with Vascular Disease/Diabetes Mellitus—A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1602. https://doi.org/10.3390/ijerph20021602
Chicago/Turabian StyleZhao, Yuxiao, Yueying Zhang, Kayla M. Teopiz, Leanna M. W. Lui, Roger S. McIntyre, and Bing Cao. 2023. "Presence of Depression Is Associated with Functional Impairment in Middle-Aged and Elderly Chinese Adults with Vascular Disease/Diabetes Mellitus—A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 2: 1602. https://doi.org/10.3390/ijerph20021602
APA StyleZhao, Y., Zhang, Y., Teopiz, K. M., Lui, L. M. W., McIntyre, R. S., & Cao, B. (2023). Presence of Depression Is Associated with Functional Impairment in Middle-Aged and Elderly Chinese Adults with Vascular Disease/Diabetes Mellitus—A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(2), 1602. https://doi.org/10.3390/ijerph20021602







