Adherence and Effect of Home-Based Rehabilitation with Telemonitoring Support in Patients with Chronic Non-Specific Low Back Pain: A Pilot Study
Abstract
1. Introduction
2. Materials and Methods
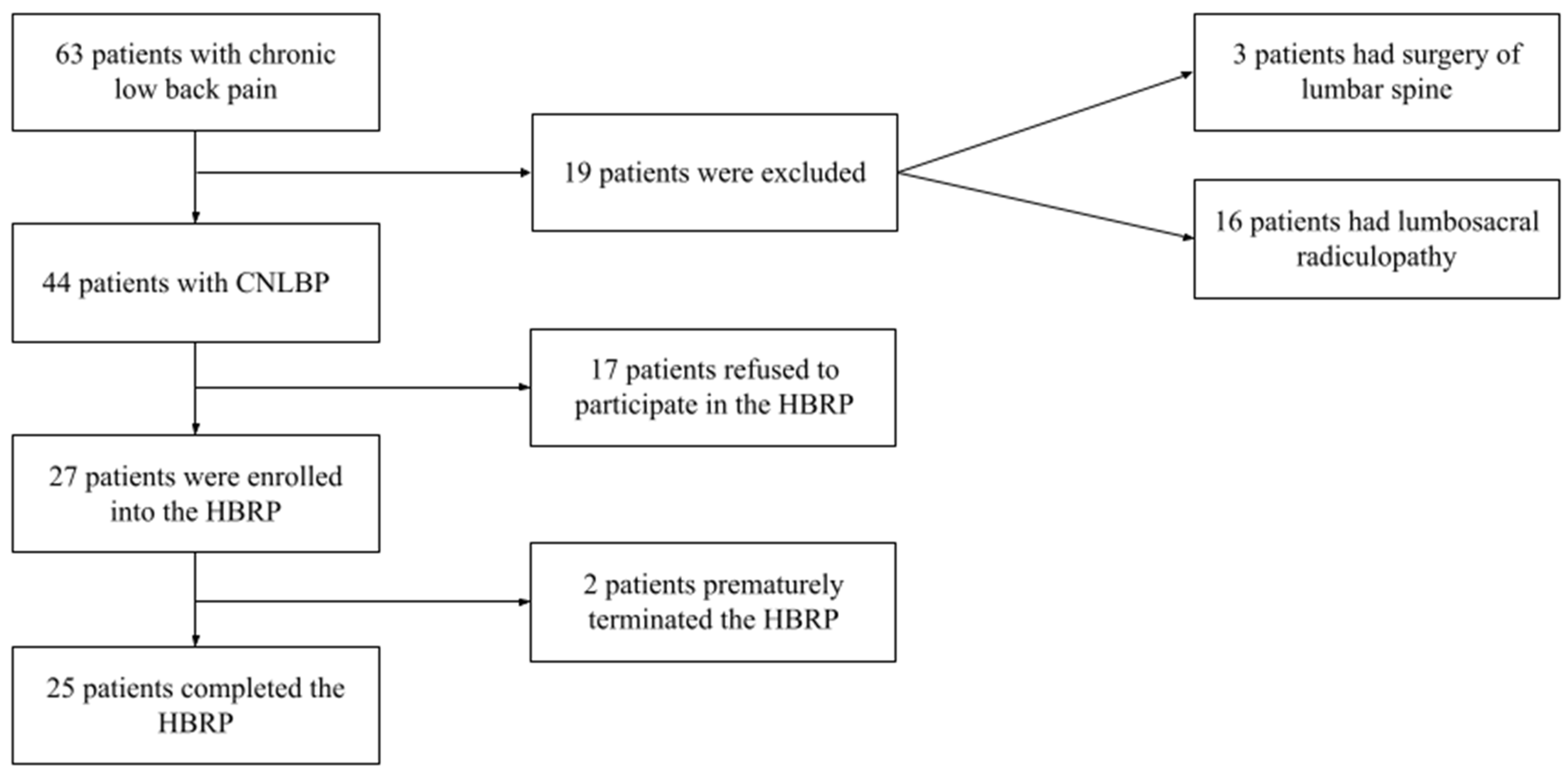
2.1. Participants
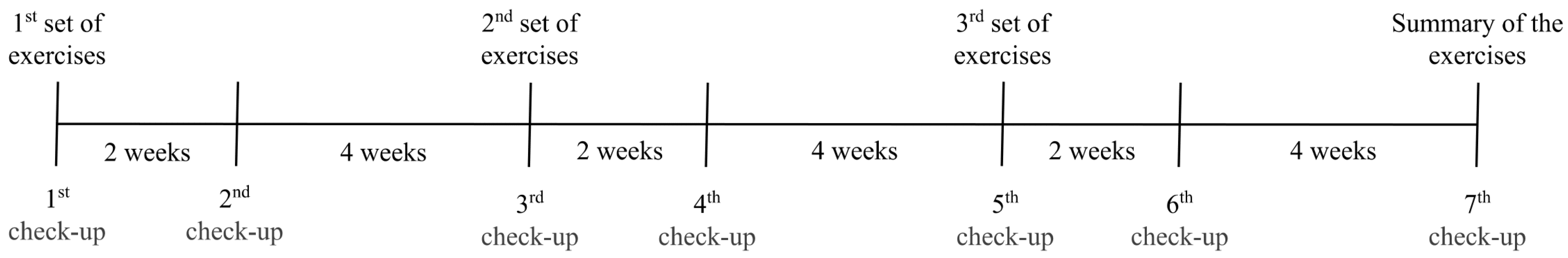
2.2. Procedures
2.2.1. Neurological Clinical Evaluation and Patient-Oriented Outcomes
2.2.2. Functional Assessment of Trunk Muscles
2.2.3. Home-Based Rehabilitation Programme
2.3. Compliance and Telemonitoring
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. Adherence to a Home-Based Rehabilitation Programme and Patient Satisfaction
3.3. Changes in Pain, Disability, and Functional Tests after the HBRP
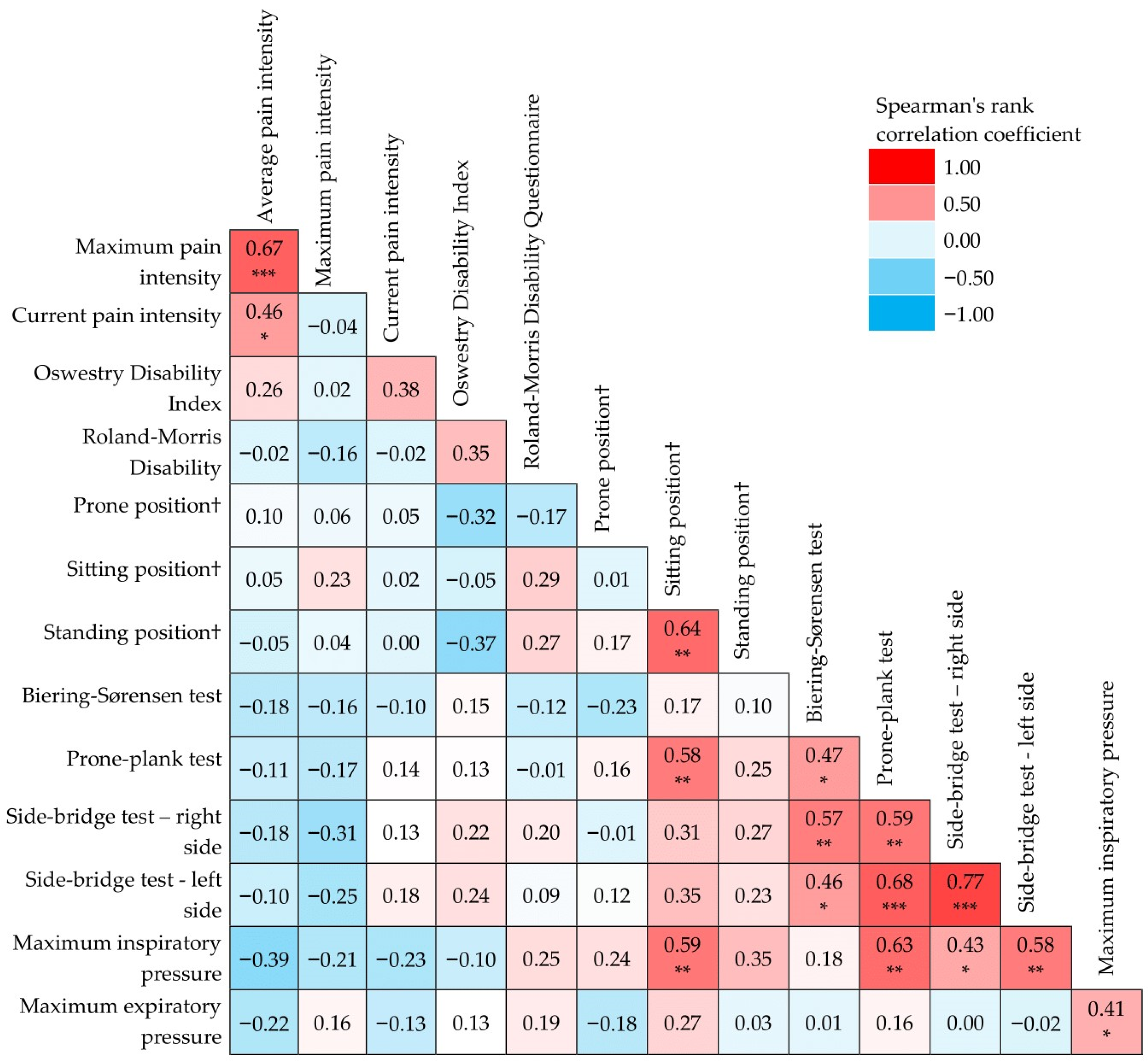
3.4. Correlation of Relative Changes in Particular Parameters after the HBRP
4. Discussion
4.1. Adherence
4.2. Satisfaction and Beliefs
4.3. Changes in Pain, Disability, and Functional Tests after the HBRP
4.4. Correlations in Changes of Particular Parameters
4.5. Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Saragiotto, B.T.; Maher, C.G.; Yamato, T.P.; Costa, L.O.; Menezes Costa, L.C.; Ostelo, R.W.; Macedo, L.G. Motor Control Exercise for Chronic Non-specific Low-back Pain. Cochrane Database Syst. Rev. 2016, 2016, CD012004. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, O.; Brox, J.I.; Cedraschi, C.; Hildebrandt, J.; Klaber-Moffett, J.; Kovacs, F.; Mannion, A.F.; Reis, S.; Staal, J.B.; Ursin, H.; et al. Chapter 4. European Guidelines for the Management of Chronic Nonspecific Low Back Pain. Eur. Spine J. 2006, 15 (Suppl. S2), S192–S300. [Google Scholar] [CrossRef]
- Panjabi, M.M. A Hypothesis of Chronic Back Pain: Ligament Subfailure Injuries Lead to Muscle Control Dysfunction. Eur. Spine J. 2006, 15, 668–676. [Google Scholar] [CrossRef] [PubMed]
- Agten, A.; Verbrugghe, J.; Stevens, S.; Boomgaert, L.; O Eijnde, B.; Timmermans, A.; Vandenabeele, F. Feasibility, Accuracy and Safety of a Percutaneous Fine-Needle Biopsy Technique to Obtain Qualitative Muscle Samples of the Lumbar Multifidus and Erector Spinae Muscle in Persons with Low Back Pain. J. Anat. 2018, 233, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Mannion, A.F. Fibre Type Characteristics and Function of the Human Paraspinal Muscles: Normal Values and Changes in Association with Low Back Pain. J. Electromyogr. Kinesiol. 1999, 9, 363–377. [Google Scholar] [CrossRef] [PubMed]
- Adams, M.A.; Hutton, W.C. Has the Lumbar Spine a Margin of Safety in Forward Bending? Clin. Biomech. 1986, 1, 3–6. [Google Scholar] [CrossRef]
- Kalichman, L.; Carmeli, E.; Been, E. The Association between Imaging Parameters of the Paraspinal Muscles, Spinal Degeneration, and Low Back Pain. BioMed Res. Int. 2017, 2017, 2562957. [Google Scholar] [CrossRef]
- Hildebrandt, M.; Fankhauser, G.; Meichtry, A.; Luomajoki, H. Correlation between Lumbar Dysfunction and Fat Infiltration in Lumbar Multifidus Muscles in Patients with Low Back Pain. BMC Musculoskelet. Disord. 2017, 18, 12. [Google Scholar] [CrossRef]
- Freeman, M.D.; Woodham, M.A.; Woodham, A.W. The Role of the Lumbar Multifidus in Chronic Low Back Pain: A Review. PM R 2010, 2, 142–146, quiz 1 p following 167. [Google Scholar] [CrossRef]
- Padwal, J.; Berry, D.B.; Hubbard, J.C.; Zlomislic, V.; Allen, R.T.; Garfin, S.R.; Ward, S.R.; Shahidi, B. Regional Differences between Superficial and Deep Lumbar Multifidus in Patients with Chronic Lumbar Spine Pathology. BMC Musculoskelet. Disord. 2020, 21, 764. [Google Scholar] [CrossRef]
- Steele, J.; Fisher, J.; Perrin, C.; Conway, R.; Bruce-Low, S.; Smith, D. Does Change in Isolated Lumbar Extensor Muscle Function Correlate with Good Clinical Outcome? A Secondary Analysis of Data on Change in Isolated Lumbar Extension Strength, Pain, and Disability in Chronic Low Back Pain. Disabil. Rehabil. 2019, 41, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Steele, J.; Bruce-Low, S.; Smith, D. A Reappraisal of the Deconditioning Hypothesis in Low Back Pain: Review of Evidence from a Triumvirate of Research Methods on Specific Lumbar Extensor Deconditioning. Curr. Med. Res. Opin. 2014, 30, 865–911. [Google Scholar] [CrossRef]
- Frizziero, A.; Pellizzon, G.; Vittadini, F.; Bigliardi, D.; Costantino, C. Efficacy of Core Stability in Non-Specific Chronic Low Back Pain. J. Funct. Morphol. Kinesiol. 2021, 6, 37. [Google Scholar] [CrossRef] [PubMed]
- Corp, N.; Mansell, G.; Stynes, S.; Wynne-Jones, G.; Morsø, L.; Hill, J.C.; van der Windt, D.A. Evidence-Based Treatment Recommendations for Neck and Low Back Pain across Europe: A Systematic Review of Guidelines. Eur. J. Pain 2021, 25, 275–295. [Google Scholar] [CrossRef] [PubMed]
- Akuthota, V.; Ferreiro, A.; Moore, T.; Fredericson, M. Core Stability Exercise Principles. Curr. Sports Med. Rep. 2008, 7, 39–44. [Google Scholar] [CrossRef]
- Panjabi, M.M. The Stabilizing System of the Spine. Part I. Function, Dysfunction, Adaptation, and Enhancement. J. Spinal Disord. 1992, 5, 383–389; discussion 397. [Google Scholar] [CrossRef]
- Panjabi, M.M. The Stabilizing System of the Spine. Part II. Neutral Zone and Instability Hypothesis. J. Spinal Disord. 1992, 5, 390–396; discussion 397. [Google Scholar] [CrossRef]
- Janssens, L.; Brumagne, S.; McConnell, A.K.; Hermans, G.; Troosters, T.; Gayan-Ramirez, G. Greater Diaphragm Fatigability in Individuals with Recurrent Low Back Pain. Respir. Physiol. Neurobiol. 2013, 188, 119–123. [Google Scholar] [CrossRef]
- Janssens, L.; Brumagne, S.; Polspoel, K.; Troosters, T.; McConnell, A. The Effect of Inspiratory Muscles Fatigue on Postural Control in People with and without Recurrent Low Back Pain. Spine 2010, 35, 1088–1094. [Google Scholar] [CrossRef]
- Parreira, P.; Heymans, M.W.; van Tulder, M.W.; Esmail, R.; Koes, B.W.; Poquet, N.; Lin, C.-W.C.; Maher, C.G. Back Schools for Chronic Non-Specific Low Back Pain. Cochrane Database Syst. Rev. 2017, 8, CD011674. [Google Scholar] [CrossRef]
- Forssell, M.Z. The Back School. Spine 1981, 6, 104–106. [Google Scholar] [CrossRef] [PubMed]
- Seron, P.; Oliveros, M.-J.; Gutierrez-Arias, R.; Fuentes-Aspe, R.; Torres-Castro, R.C.; Merino-Osorio, C.; Nahuelhual, P.; Inostroza, J.; Jalil, Y.; Solano, R.; et al. Effectiveness of Telerehabilitation in Physical Therapy: A Rapid Overview. Phys. Ther. 2021, 101, pzab053. [Google Scholar] [CrossRef] [PubMed]
- Meystre, S. The Current State of Telemonitoring: A Comment on the Literature. Telemed. J. E-Health 2005, 11, 63–69. [Google Scholar] [CrossRef] [PubMed]
- Quentin, C.; Bagheri, R.; Ugbolue, U.C.; Coudeyre, E.; Pélissier, C.; Descatha, A.; Menini, T.; Bouillon-Minois, J.-B.; Dutheil, F. Effect of Home Exercise Training in Patients with Nonspecific Low-Back Pain: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 8430. [Google Scholar] [CrossRef] [PubMed]
- Mbada, C.E.; Olaoye, M.I.; Dada, O.O.; Ayanniyi, O.; Johnson, O.E.; Odole, A.C.; Ishaya, G.P.; Omole, O.J.; Makinde, M.O. Comparative Efficacy of Clinic-Based and Telerehabilitation Application of Mckenzie Therapy in Chronic Low-Back Pain. Int. J. Telerehabil. 2019, 11, 41–58. [Google Scholar] [CrossRef] [PubMed]
- Fairbank, J.C.; Couper, J.; Davies, J.B.; O’Brien, J.P. The Oswestry Low Back Pain Disability Questionnaire. Physiotherapy 1980, 66, 271–273. [Google Scholar]
- Roland, M.; Morris, R. A Study of the Natural History of Back Pain. Part I: Development of a Reliable and Sensitive Measure of Disability in Low-Back Pain. Spine 1983, 8, 141–144. [Google Scholar] [CrossRef]
- Vlažná, D.; Krkoška, P.; Kuhn, M.; Dosbaba, F.; Batalik, L.; Vlčková, E.; Voháňka, S.; Adamová, B. Assessment of Lumbar Extensor Muscles in the Context of Trunk Function, a Pilot Study in Healthy Individuals. Appl. Sci. 2021, 11, 9518. [Google Scholar] [CrossRef]
- Peek, K.; Carey, M.; Mackenzie, L.; Sanson-Fisher, R. Patient Adherence to an Exercise Program for Chronic Low Back Pain Measured by Patient-Report, Physiotherapist-Perception and Observational Data. Physiother. Theory Pract. 2019, 35, 1304–1313. [Google Scholar] [CrossRef]
- Dhondt, E.; Van Oosterwijck, J.; Cagnie, B.; Adnan, R.; Schouppe, S.; Van Akeleyen, J.; Logghe, T.; Danneels, L. Predicting Treatment Adherence and Outcome to Outpatient Multimodal Rehabilitation in Chronic Low Back Pain. J. Back Musculoskelet. Rehabil. 2020, 33, 277–293. [Google Scholar] [CrossRef]
- Kolt, G.S.; McEvoy, J.F. Adherence to Rehabilitation in Patients with Low Back Pain. Man. Ther. 2003, 8, 110–116. [Google Scholar] [CrossRef]
- Ben Salah Frih, Z.; Fendri, Y.; Jellad, A.; Boudoukhane, S.; Rejeb, N. Efficacy and Treatment Compliance of a Home-Based Rehabilitation Programme for Chronic Low Back Pain: A Randomized, Controlled Study. Ann. Phys. Rehabil. Med. 2009, 52, 485–496. [Google Scholar] [CrossRef] [PubMed]
- Murphy, M.H.; Lahart, I.; Carlin, A.; Murtagh, E. The Effects of Continuous Compared to Accumulated Exercise on Health: A Meta-Analytic Review. Sports Med. 2019, 49, 1585–1607. [Google Scholar] [CrossRef] [PubMed]
- Medina-Mirapeix, F.; Escolar-Reina, P.; Gascón-Cánovas, J.J.; Montilla-Herrador, J.; Jimeno-Serrano, F.J.; Collins, S.M. Predictive Factors of Adherence to Frequency and Duration Components in Home Exercise Programs for Neck and Low Back Pain: An Observational Study. BMC Musculoskelet. Disord. 2009, 10, 155. [Google Scholar] [CrossRef]
- Anar, S.Ö. The Effectiveness of Home-Based Exercise Programs for Low Back Pain Patients. J. Phys. Ther. Sci. 2016, 28, 2727–2730. [Google Scholar] [CrossRef]
- Escolar-Reina, P.; Medina-Mirapeix, F.; Gascón-Cánovas, J.J.; Montilla-Herrador, J.; Jimeno-Serrano, F.J.; de Oliveira Sousa, S.L.; del Baño-Aledo, M.E.; Lomas-Vega, R. How Do Care-Provider and Home Exercise Program Characteristics Affect Patient Adherence in Chronic Neck and Back Pain: A Qualitative Study. BMC Health Serv. Res. 2010, 10, 60. [Google Scholar] [CrossRef] [PubMed]
- Ostelo, R.W.J.G.; Deyo, R.A.; Stratford, P.; Waddell, G.; Croft, P.; Von Korff, M.; Bouter, L.M.; de Vet, H.C. Interpreting Change Scores for Pain and Functional Status in Low Back Pain: Towards International Consensus Regarding Minimal Important Change. Spine 2008, 33, 90–94. [Google Scholar] [CrossRef] [PubMed]
- Bruce-Low, S.; Smith, D.; Burnet, S.; Fisher, J.; Bissell, G.; Webster, L. One Lumbar Extension Training Session per Week Is Sufficient for Strength Gains and Reductions in Pain in Patients with Chronic Low Back Pain Ergonomics. Ergonomics 2012, 55, 500–507. [Google Scholar] [CrossRef]
- Welch, N.; Moran, K.; Antony, J.; Richter, C.; Marshall, B.; Coyle, J.; Falvey, E.; Franklyn-Miller, A. The Effects of a Free-Weight-Based Resistance Training Intervention on Pain, Squat Biomechanics and MRI-Defined Lumbar Fat Infiltration and Functional Cross-Sectional Area in Those with Chronic Low Back. BMJ Open Sport Exerc. Med. 2015, 1, e000050. [Google Scholar] [CrossRef]
- Storheim, K.; Holm, I.; Gunderson, R.; Brox, J.I.; Bø, K. The Effect of Comprehensive Group Training on Cross-Sectional Area, Density, and Strength of Paraspinal Muscles in Patients Sick-Listed for Subacute Low Back Pain. J. Spinal Disord. Tech. 2003, 16, 271–279. [Google Scholar] [CrossRef] [PubMed]
- Steele, J.; Bruce-Low, S.; Smith, D.; Jessop, D.; Osborne, N. Isolated Lumbar Extension Resistance Training Improves Strength, Pain, and Disability, but Not Spinal Height or Shrinkage (“Creep”) in Participants with Chronic Low Back Pain. Cartilage 2020, 11, 160–168. [Google Scholar] [CrossRef] [PubMed]
- Huijnen, I.P.J.; Verbunt, J.A.; Wittink, H.M.; Smeets, R.J.E.M. Physical Performance Measurement in Chronic Low Back Pain: Measuring Physical Capacity or Pain-Related Behaviour? Eur. J. Physiother. 2013, 15, 103–110. [Google Scholar] [CrossRef]
| Variable | Patients Started HBRP (n = 27) | Patients Completed HBRP (n = 25) | |
|---|---|---|---|
| Sex | Female [n (%)] | 12 (44.4) | 10 (40.0) |
| Male [n (%)] | 15 (55.6) | 15 (60.0) | |
| Age [years] | 49.0 (26; 68) | 49.0 (26; 68) | |
| Height [cm] | 175.0 (160.0; 188.0) | 176.0 (160.0; 188.0) | |
| Weight [kg] | 79.0 (56.0; 118.0) | 80.0 (56.0; 118.0) | |
| BMI [kg/m2] | 25.8 (19.4; 35.2) | 25.8 (19.4; 35.2) | |
| Education | Primary education [n (%)] | 10 (37.1) | 9 (36.0) |
| Secondary education [n (%)] | 8 (29.6) | 8 (32.0) | |
| Tertiary education [n (%)] | 9 (33.3) | 8 (32.0) | |
| Duration of CNLBP [weeks] | 96.0 (13.0; 1664.0) | 96.0 (13.0; 1664.0) | |
| Use of analgesic medication for CNLBP [n (%)] | 15 (55.6) | 13 (52.0) | |
| Use of central muscle relaxants [n (%)] | 4 (14.8) | 4 (16.0) | |
| Patients Using Exercise Diary (n = 7) | Patients Using Mobile Application (n = 18) | Group Difference (p) | |
|---|---|---|---|
| Percentage of completed records (%) | 100 (100.0; 100.0) | 97.1 (88.5; 98.9) | <0.001 |
| Exercised at least once a day (%) | 82.3 (80.1; 88.7) | 94.8 (90.8; 97.9) | <0.001 |
| Exercised twice a day (%) | 72.9 (68.2; 78.4) | 86.6 (75.3; 91.2) | <0.001 |
| No exercise on the day (%) | 17.7 (11.3; 19.9) | 5.2 (2.1; 9.2) | <0.001 |
| Question | |||||
|---|---|---|---|---|---|
| How satisfied are you with the completion of the rehabilitation programme? | Fully satisfied | Rather satisfied | Neither satisfied nor dissatisfied | Rather dissatisfied | Fully dissatisfied |
| 22 (88.0) | 3 (12.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Do you believe that this rehabilitation programme has helped you with problems associated with your lumbar spine? | I believe it | I somewhat believe it | I don’t know | I somewhat don’t believe it | I don’t believe it at all |
| 20 (80.0) | 4 (16.0) | 1 (4.0) | 0 (0.0) | 0 (0.0) |
| Variable | Patients with CNLBP (before Rehabilitation Programme) (n = 25) | Patients with CNLBP (after Rehabilitation Programme) (n = 25) | Group Difference | |
|---|---|---|---|---|
| Median (min; max) | p | |||
| Average pain intensity [NRS 0–10] | 4.0 (1.0; 8.0) | 2.0 (0.0; 5.0) | −2.0 (−4.0; 0.0) | <0.001 |
| Current pain intensity [NRS 0–10] | 2.0 (0.0; 6.0) | 1.0 (0.0; 5.0) | −1.0 (−5.0; 1.0) | 0.002 |
| Maximum pain intensity [NRS 0–10] | 7.0 (2.0; 10.0) | 3.0 (0.0; 8.0) | −3.0 (−8.0; 4.0) | <0.001 |
| Oswestry Disability Index [0–100%] | 20.0 (4.0; 31.0) | 4.0 (0.0; 15.5) | −13.0 (−24.4; −4.0) | <0.001 |
| Roland–Morris Disability Questionnaire | 7.0 (0.0; 19.0) | 1.0 (0.0; 6.0) | −6.0 (−17.0; 0.0) | <0.001 |
| Variable | Patients with CNLBP (before Rehabilitation Programme) (n = 25) | Patients with CNLBP (after Rehabilitation Programme) (n = 25) | Group Difference (p) |
|---|---|---|---|
| Use of analgesic medication for CNLBP [n (%)] | 13 (52.0) | 3 (12.0) | 0.006 † |
| Use of central muscle relaxants [n (%)] | 4 (16.0) | 1 (4.0) | 0.349 †† |
| Variable | Patients with CNLBP (before Rehabilitation Programme) (n = 25) | Patients with CNLBP (after Rehabilitation Programme) (n = 25) | Group Difference | ||
|---|---|---|---|---|---|
| Median (min; max) | p | ||||
| Maximal isometric lower back extensor strength | Prone position [kg] † | 16.6 (4.3; 24.6) | 23.4 (9.0; 34.1) | 6.5 (0.5; 13.5) | <0.001 |
| Sitting position [kg] † | 35.3 (13.5; 77.7) | 57.7 (23.0; 86.3) | 16.3 (−3.7; 37.2) | <0.001 | |
| Standing position [kg] † | 32.7 (9.7; 66.9) | 51.8 (17.0; 71.8) | 13.7 (−10.3; 41.9) | <0.001 | |
| Respiratory muscle strength | Maximum inspiratory pressure [cmH2O] †† | 83.1 (27.3; 127.0) | 91.7 (45.3; 138.7) | 11.3 (−15.3; 61.3) | 0.005 |
| Maximum expiratory pressure [cmH2O] †† | 130.3 (52.0; 245.0) | 147.7 (61.7; 267.3) | 18.7 (−17.0; 98.3) | 0.001 | |
| Trunk muscle endurance tests | Biering–Sørensen test [time (s)] | 58.0 (4.0; 204.0) | 122.0 (35.0; 247.0) | 59.0 (−4.0; 177.0) | <0.001 |
| Prone-plank test [time (s)] | 57.0 (5.0; 240.0) | 83.0 (50.0; 212.0) | 43.0 (−60.0; 112.0) | <0.001 | |
| Side-bridge test-right side [time (s)] | 25.0 (2.0; 122.0) | 58.0 (16.0; 120.0) | 35.0 (−2.0; 67.0) | <0.001 | |
| Side-bridge test-left side [time (s)] | 20.0 (2.0; 122.0) | 61.0 (17.0; 121.0) | 33.0 (−30.0; 69.0) | <0.001 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krkoska, P.; Vlazna, D.; Sladeckova, M.; Minarikova, J.; Barusova, T.; Batalik, L.; Dosbaba, F.; Vohanka, S.; Adamova, B. Adherence and Effect of Home-Based Rehabilitation with Telemonitoring Support in Patients with Chronic Non-Specific Low Back Pain: A Pilot Study. Int. J. Environ. Res. Public Health 2023, 20, 1504. https://doi.org/10.3390/ijerph20021504
Krkoska P, Vlazna D, Sladeckova M, Minarikova J, Barusova T, Batalik L, Dosbaba F, Vohanka S, Adamova B. Adherence and Effect of Home-Based Rehabilitation with Telemonitoring Support in Patients with Chronic Non-Specific Low Back Pain: A Pilot Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1504. https://doi.org/10.3390/ijerph20021504
Chicago/Turabian StyleKrkoska, Peter, Daniela Vlazna, Michaela Sladeckova, Jitka Minarikova, Tamara Barusova, Ladislav Batalik, Filip Dosbaba, Stanislav Vohanka, and Blanka Adamova. 2023. "Adherence and Effect of Home-Based Rehabilitation with Telemonitoring Support in Patients with Chronic Non-Specific Low Back Pain: A Pilot Study" International Journal of Environmental Research and Public Health 20, no. 2: 1504. https://doi.org/10.3390/ijerph20021504
APA StyleKrkoska, P., Vlazna, D., Sladeckova, M., Minarikova, J., Barusova, T., Batalik, L., Dosbaba, F., Vohanka, S., & Adamova, B. (2023). Adherence and Effect of Home-Based Rehabilitation with Telemonitoring Support in Patients with Chronic Non-Specific Low Back Pain: A Pilot Study. International Journal of Environmental Research and Public Health, 20(2), 1504. https://doi.org/10.3390/ijerph20021504







