Relationship between Body Mass Index and Physical Activity among Children from Low-Income Communities in Gqeberha, South Africa: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Ethics Statements
2.4. Anthropometric Measures
2.5. Physical Activity
2.6. Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bennett, J.E.; Stevens, G.A.; Mathers, C.D.; Bonita, R.; Rehm, J.; Kruk, M.E.; Riley, L.M.; Dain, K.; Kengne, A.P.; Chalkidou, K.; et al. NCD Countdown 2030: Worldwide trends in non-communicable disease mortality and progress towards Sustainable Development Goal target 3.4. Lancet 2018, 392, 1072–1088. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bradshaw, D.; Nannan, N.N.; Wyk, V.P.-V.; Laubscher, R.; Groenewald, P.; E Dorrington, R. Burden of disease in South Africa: Protracted transitions driven by social pathologies. South Afr. Med. J. 2019, 109, 69–76. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Bank. Gini Coefficient by Country 2022. Available online: https://worldpopulationreview.com/country-rankings/gini-coefficient-by-country (accessed on 22 November 2022).
- Rossouw, H.A.; Grant, C.C.; Viljoen, M. Overweight and obesity in children and adolescents: The South African problem. South Afr. J. Sci. 2012, 108, 1–7. [Google Scholar] [CrossRef]
- Monyeki, M.A.; Awotidebe, A.; Strydom, G.L.; De Ridder, J.H.; Mamabolo, R.L.; Kemper, H.C.G. The Challenges of Underweight and Overweight in South African Children: Are We Winning or Losing the Battle? A Systematic Review. Int. J. Environ. Res. Public Health 2015, 12, 1156–1173. [Google Scholar] [CrossRef] [Green Version]
- Pretorius, S.S.; Neophytou, N.; Watson, E.D. Anthropometric profiles of 8–11 year old children from a low-income setting in South Africa. BMC Public Health 2019, 19, 314. [Google Scholar] [CrossRef] [Green Version]
- Development Initiatives. 2018 Global Nutrition Report: Shining a Light to Spur Action on Nutrition; Development Initiatives: Bristol, UK, 2018. [Google Scholar]
- May, J.; Witten, C.; Lake, L. South African Child Gauge 2020; The Children’s Institute, University of Cape Town: Cape Town, South Africa, 2022. [Google Scholar]
- Pendergast, F.J.; Livingstone, K.M.; Worsley, A.; McNaughton, S.A. Correlates of meal skipping in young adults: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 125. [Google Scholar] [CrossRef] [Green Version]
- Wrottesley, S.V.; Pedro, T.M.; Fall, C.H.; A Norris, S. A review of adolescent nutrition in South Africa: Transforming adolescent lives through nutrition initiative. South Afr. J. Clin. Nutr. 2020, 33, 94–132. [Google Scholar] [CrossRef]
- Okeyo, A.P.; Seekoe, E.; De Villiers, A.; Faber, M.; Nel, J.H.; Steyn, N.P. Dietary Practices and Adolescent Obesity in Secondary School Learners at Disadvantaged Schools in South Africa: Urban–Rural and Gender Differences. Int. J. Environ. Res. Public Health 2020, 17, 5864. [Google Scholar] [CrossRef]
- Caleyachetty, R.; Thomas, G.N.; Kengne, A.P.; Echouffo-Tcheugui, J.B.; Schilsky, S.; Khodabocus, J.; Uauy, R. The double burden of malnutrition among adolescents: Analysis of data from the Global School-Based Student Health and Health Behavior in School-Aged Children surveys in 57 low- and middle-income countries. Am. J. Clin. Nutr. 2018, 108, 414–424. [Google Scholar] [CrossRef] [Green Version]
- Mbogori, T.; Kimmel, K.; Zhang, M.; Kandiah, J.; Wang, Y. Nutrition transition and double burden of malnutrition in Africa: A case study of four selected countries with different social economic development. AIMS Public Health 2020, 7, 425–439. [Google Scholar] [CrossRef]
- Popkin, B.M.; Ng, S.W. The nutrition transition to a stage of high obesity and noncommunicable disease prevalence dominated by ultra-processed foods is not inevitable. Obes. Rev. 2022, 23, e13366. [Google Scholar] [CrossRef]
- Jones, R.A.; Okely, A.; Caputi, P.; Cliff, D. Perceived and actual competence among overweight and non-overweight children. J. Sci. Med. Sport 2010, 13, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Shorey, S.; Ng, E.D. The Lived Experiences of Children and Adolescents with Non-Communicable Disease: A Systematic Review of Qualitative Studies. J. Pediatr. Nurs. 2020, 51, 75–84. [Google Scholar] [CrossRef] [PubMed]
- Janssen, I.; LeBlanc, A.G. Systematic review of the health benefits of physical activity and fitness in school-aged children and youth. Int. J. Behav. Nutr. Phys. Act. 2010, 7, 40. [Google Scholar] [CrossRef] [Green Version]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Healthy Active Kids Global Alliance. Global Matrix 4.0. 2022. Available online: https://www.activehealthykids.org/4-0/#:~:text=This%20Global%20Matrix%204.0%20confirms,19%20pandemic%20and%20related%20restrictions (accessed on 25 October 2022).
- Naidoo, R.; Christie, C.; Lambert, E.; Nyawose, Z.; Basset, S.; Monyeki, A.; Janse van Rensburg, C.; Cozett, C.; Naidoo, N.; Gradidge, P. Healthy Active Kids South Africa 2022 Report Card; University of Cape Town: Cape Town, South Africa, 2022. [Google Scholar]
- Muthuri, S.K.; Onywera, V.O.; Tremblay, M.S.; Broyles, S.T.; Chaput, J.-P.; Fogelholm, M.; Hu, G.; Kuriyan, R.; Kurpad, A.; Lambert, E.V.; et al. Relationships between Parental Education and Overweight with Childhood Overweight and Physical Activity in 9–11 Year Old Children: Results from a 12-Country Study. PLoS ONE 2016, 11, e0147746. [Google Scholar] [CrossRef] [Green Version]
- Telford, R.M.; Telford, R.D.; Olive, L.S.; Cochrane, T.; Davey, R. Why Are Girls Less Physically Active than Boys? Findings from the LOOK Longitudinal Study. PLoS ONE 2016, 11, e0150041. [Google Scholar] [CrossRef]
- Baran, J.; Weres, A.; Wyszyńska, J.; Pitucha, G.; Czenczek-Lewandowska, E.; Rusek, W.; Leszczak, J.; Mazur, A. 60 Minutes Per Day in Moderate to Vigorous Physical Activity as a Natural Health Protector in Young Population. Int. J. Environ. Res. Public Health 2020, 17, 8918. [Google Scholar] [CrossRef]
- Hanson, S.K.; Munthali, R.J.; Micklesfield, L.K.; Lobelo, F.; Cunningham, S.A.; Hartman, T.J.; Norris, S.A.; Stein, A.D. Longitudinal patterns of physical activity, sedentary behavior and sleep in urban South African adolescents, Birth-To-Twenty Plus cohort. BMC Pediatr. 2019, 19, 241. [Google Scholar] [CrossRef] [Green Version]
- Farooq, A.; Martin, A.; Janssen, X.; Wilson, M.G.; Gibson, A.; Hughes, A.; Reilly, J.J. Longitudinal changes in moderate-to-vigorous-intensity physical activity in children and adolescents: A systematic review and meta-analysis. Obes. Rev. 2019, 21, e12953. [Google Scholar] [CrossRef]
- Müller, I.; Smith, D.; Adams, L.; Aerts, A.; Damons, B.P.; Degen, J.; Gall, S.; Gani, Z.; Gerber, M.; Gresse, A.; et al. Effects of a School-Based Health Intervention Program in Marginalized Communities of Port Elizabeth, South Africa (the KaziBantu Study): Protocol for a Randomized Controlled Trial. JMIR Res. Protoc. 2019, 8, e14097. [Google Scholar] [CrossRef] [Green Version]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [Green Version]
- Cole, T.J.; Bellizzi, M.C.; Flegal, K.M.; Dietz, W.H. Establishing a standard definition for child overweight and obesity worldwide: International survey. BMJ 2000, 320, 1240. [Google Scholar] [CrossRef] [Green Version]
- Hills, A.P.; Emokhtar, N.; Byrne, N.M. Assessment of Physical Activity and Energy Expenditure: An Overview of Objective Measures. Front. Nutr. 2014, 1, 5. [Google Scholar] [CrossRef]
- Troiano, R.P.; Berrigan, D.; Dodd, K.W.; Mâsse, L.C.; Tilert, T.; Mcdowell, M. Physical Activity in the United States Measured by Accelerometer. Med. Sci. Sports Exerc. 2008, 40, 181–188. [Google Scholar] [CrossRef]
- Clemente, F.M.; Nikolaidis, P.T.; Martins, F.M.L.; Mendes, R.S. Physical Activity Patterns in University Students: Do They Follow the Public Health Guidelines? PLoS ONE 2016, 11, e0152516. [Google Scholar] [CrossRef]
- Kimani-Murage, E.W.; Kahn, K.; Pettifor, J.M.; Tollman, S.M.; Dunger, D.B.; Gómez-Olivé, X.F.; A Norris, S. The prevalence of stunting, overweight and obesity, and metabolic disease risk in rural South African children. BMC Public Health 2010, 10, 158. [Google Scholar] [CrossRef]
- Klaasen, R.; Noorbhai, H.; van Gent, M. Barriers to participation in sport among urban adolescents attending an international school in Cape Town, South Africa. In Proceedings of the International Festival of Sports, Exercise and Medicine Conference, Pretoria, South Africa, 29 September–2 October 2022. [Google Scholar]
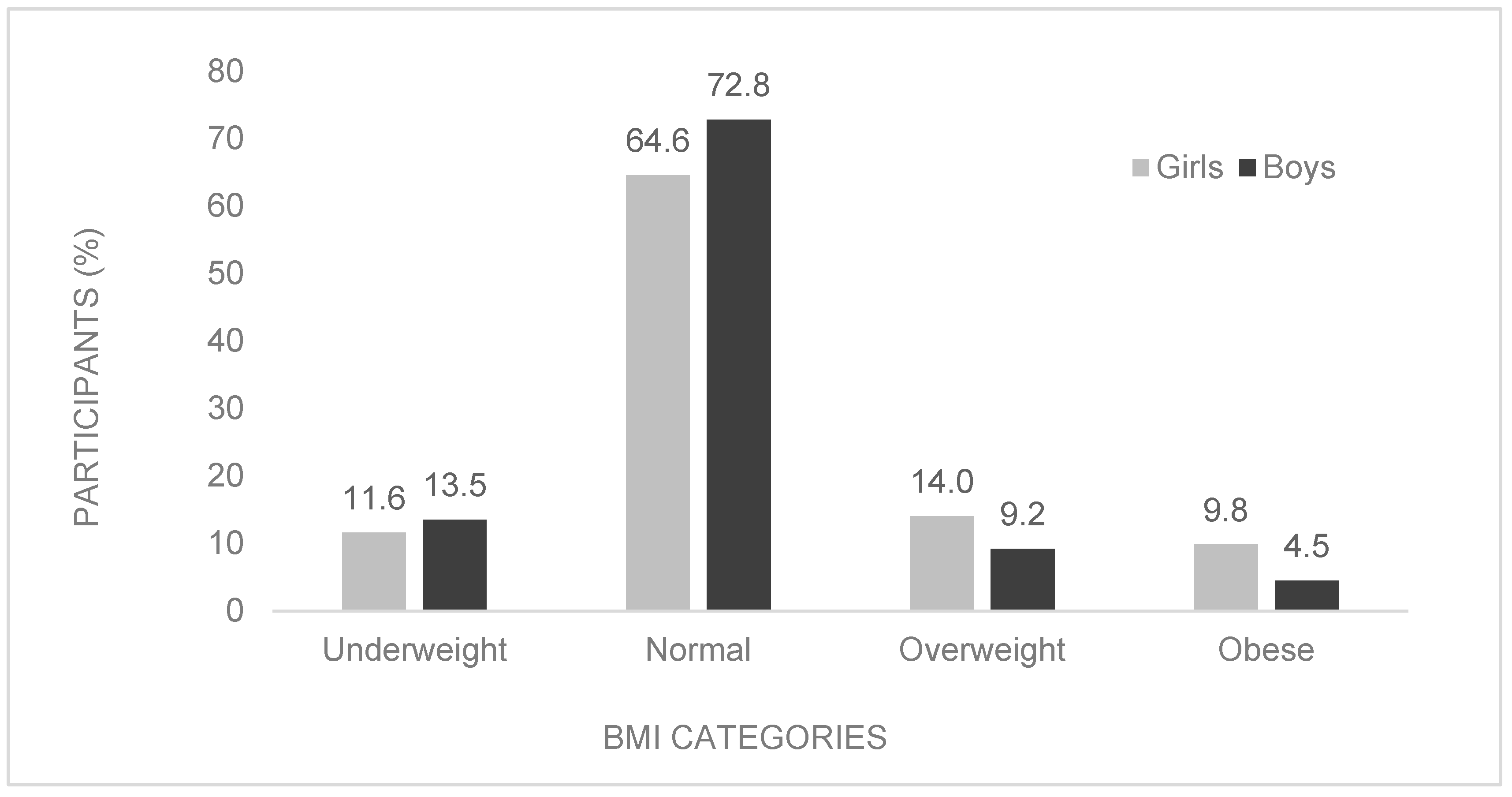

| Total (n = 975) | Boys (n = 474) | Girls (n = 501) | ||||||
|---|---|---|---|---|---|---|---|---|
| n | (SD) | n | (SD) | n | (SD) | p-Value | Cohen’s d | |
| Age (years) | 916 | 10.4 (1.2) | 467 | 10.6 (1.2) | 449 | 10.2 (1.1) | <0.001 * | 0.297 |
| Height (cm) | 927 | 139.8 (8.8) | 473 | 139.5 (8.7) | 454 | 140.2 (9.0) | 0.237 | −0.078 |
| Weight (kg) | 917 | 35.6 (10.1) | 467 | 34.5 (9.1) | 450 | 36.7 (11.0) | 0.001 * | −0.221 |
| BMI (kg/m2) | 917 | 18.0 (3.7) | 467 | 17.5 (3.2) | 450 | 18.4 (4.0) | <0.001 * | −0.250 |
| Body fat (%) | 922 | 23.64 (6.88) | 471 | 21.00 (6.37) | 451 | 26.41 (6.28) | <0.001 * | 0.85 |
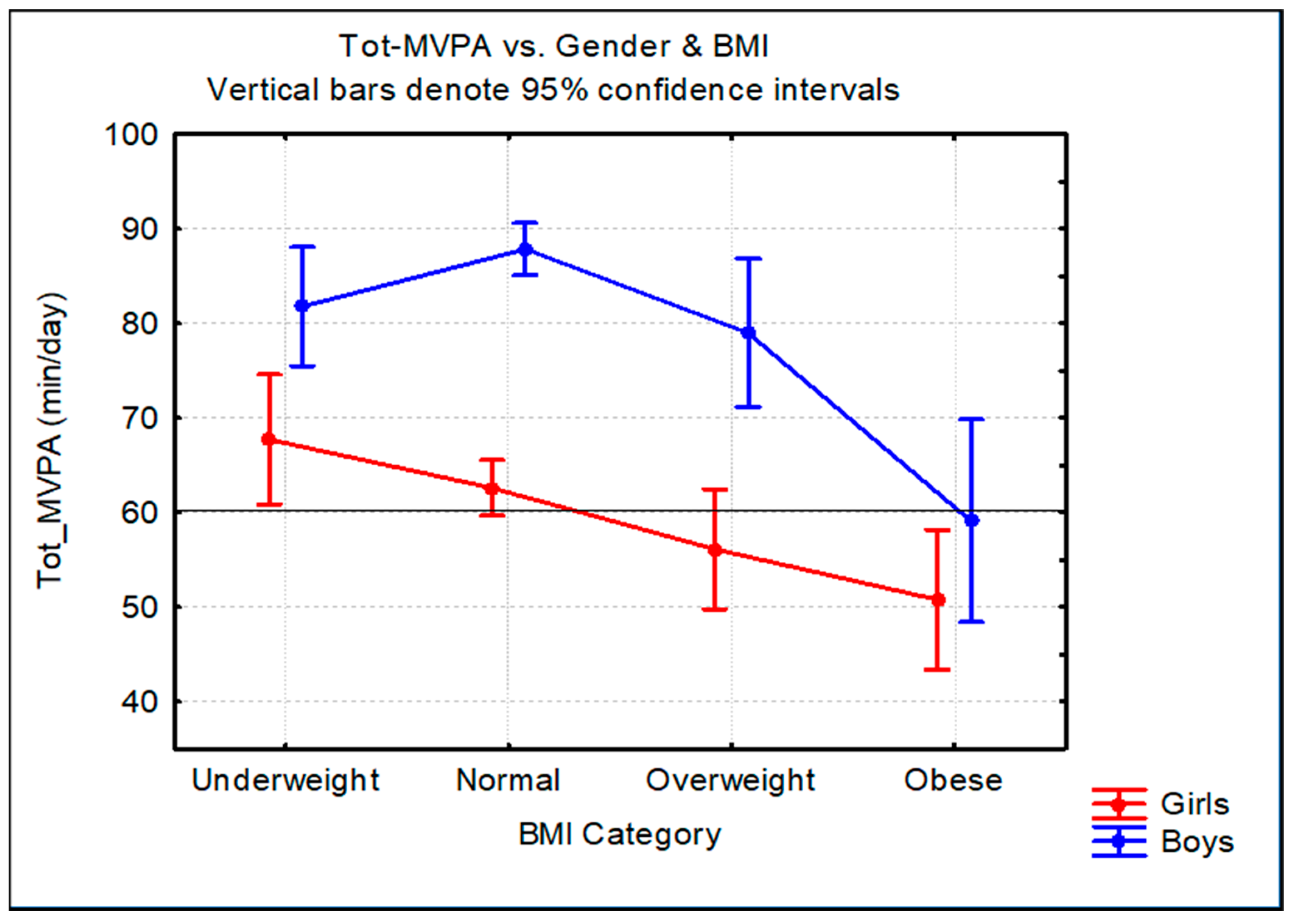
| MVPA (min/day) | 920 | 72.99 (28.25) | 464 | 84.76 (28.80) | 456 | 61.01 (21.96) | <0.001 * | −0.93 |
| Daily MVPA | ||||||||
|---|---|---|---|---|---|---|---|---|
| <60 min | ≥60 min | 95% CI | ||||||
| Sex | n | % | n | % | OR | LL | UL | p-value |
| Ov/Ob Girls | 65 | 62.5 | 39 | 37.5 | 1.78 | 1.13 | 2.80 | 0.017 * |
| Ov/Ob Boys | 26 | 43.3 | 34 | 56.7 | 3.89 | 2.18 | 6.93 | <0.0001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dolley, D.; Du Randt, R.; Pühse, U.; Gerber, M.; Bosma, J.; Aerts, A.; Adams, L.; Arnaiz, P.; Joubert, N.; Müller, I.; et al. Relationship between Body Mass Index and Physical Activity among Children from Low-Income Communities in Gqeberha, South Africa: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2023, 20, 1428. https://doi.org/10.3390/ijerph20021428
Dolley D, Du Randt R, Pühse U, Gerber M, Bosma J, Aerts A, Adams L, Arnaiz P, Joubert N, Müller I, et al. Relationship between Body Mass Index and Physical Activity among Children from Low-Income Communities in Gqeberha, South Africa: A Cross-Sectional Study. International Journal of Environmental Research and Public Health. 2023; 20(2):1428. https://doi.org/10.3390/ijerph20021428
Chicago/Turabian StyleDolley, Danielle, Rosa Du Randt, Uwe Pühse, Markus Gerber, Jacob Bosma, Ann Aerts, Larissa Adams, Patricia Arnaiz, Nandi Joubert, Ivan Müller, and et al. 2023. "Relationship between Body Mass Index and Physical Activity among Children from Low-Income Communities in Gqeberha, South Africa: A Cross-Sectional Study" International Journal of Environmental Research and Public Health 20, no. 2: 1428. https://doi.org/10.3390/ijerph20021428
APA StyleDolley, D., Du Randt, R., Pühse, U., Gerber, M., Bosma, J., Aerts, A., Adams, L., Arnaiz, P., Joubert, N., Müller, I., Nqweniso, S., Seelig, H., Steinmann, P., Utzinger, J., & Walter, C. (2023). Relationship between Body Mass Index and Physical Activity among Children from Low-Income Communities in Gqeberha, South Africa: A Cross-Sectional Study. International Journal of Environmental Research and Public Health, 20(2), 1428. https://doi.org/10.3390/ijerph20021428









