Abstract
Orthodontic miniscrews (OM) are widely used in modern orthodontic clinical practice to improve skeletal anchorage and have a high safety profile. A complication at the time of OM insertion is tooth root perforation or periodontal ligament trauma. Rarely, OM injury can cause permanent damage, such as ankylosis, osteosclerosis, and loss of tooth vitality. The aim of this work was to analyze potential risks and dental complications associated with the use of OMs. A search of the PubMed, Cochrane, Web of Science, and Scopus databases was conducted without a time limit using the keywords “orthodontic mini-screw” and “dental damage”, resulting in 99 studies. After screening and eligibility, including articles obtained through a citation search, 13 articles were selected. Four studies revealed accidental injuries caused by OM. Most of the damage was localized at the root level and resolved spontaneously with restorative cement formation after prompt removal of the OM, while the pain disappeared. In some cases, irreversible nerve damage, extensive lesions to the dentin–pulp complex, and refractory periapical periodontitis occurred, requiring endodontic and/or surgical treatment. The choice of insertion site was the most important element to be evaluated during the application of OMs.
1. Introduction
The use of orthodontic miniscrews (OMs) is a valid ally in the clinical practice of orthodontics, representing a valid support in the control of anchorage during orthodontic treatment, both with fixed and removable appliances [1,2] (Figure 1).
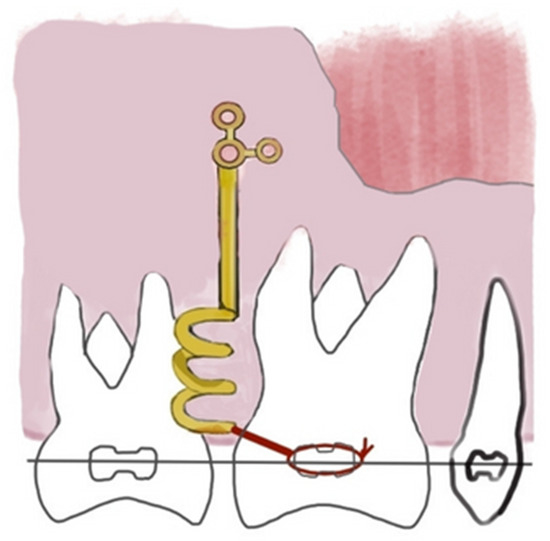
Figure 1.
Orthodontic miniscrews (OMs) are anchorage devices in orthodontic treatment.
Furthermore, OMs expand treatment options for adolescent and adult patients and are a valuable aid in reducing unwanted forces or increasing the effectiveness of orthopedic appliances, such as hybrid or bone braces [3].
Positioning is the major challenge in applying OMs. The rate of success of this technique is strictly conditioned by the site of insertion, angulations, depth of insertion, bone thickness, and design of the screw, e.g., diameter, dimension, and length [4,5,6,7,8,9,10,11,12].
A recent study evaluated the influence of the OM design of the implant surface on retention and, thus, on the success of the OM. In particular, the authors analyzed pitch, thread depth, and shape, concluding that only the first of these three factors is decisive. Implants with a denser thread show greater stability, while thread depth and thread shape are irrelevant [13].
Surgical customized 3D templates are a valuable support in enhancing the insertion accuracy and stability of OMs, reducing the risk of side-effects and failure [14]. The combined use of Cone Beam CT (CBCT) and the intraoral scan allows digital OMs positioning through a Computer-Aided Design-Computer-Aided Manufacturing (Cad-Cam) dime to guide the insertion during the clinical stage.
Although the use of Temporary Anchorage Devices (TADs) in the digital workflow reduces the occurrence of dental damage, it is still a common occurrence. The use of OMs is associated with several complications, which can occur during their insertion, use, or removal [15,16,17]. In the lower arch, the insertion of OMs without a correct evaluation of anatomic structures might determine serious damage to the mental nerve and the lingual nerve.
No significant data are reported about complications due to the perforation of the maxillary sinus by OMs insertion [18]. On the other hand, tooth root injuries are reported as the most frequent complications of OMs [19,20]. The failure of OMs stability is closely related to its proximity to the tooth root. A radiographic overlap of the body of the OM on the roots of dental elements significantly decreases the success rate from 80% in the maxilla and 75% in the mandible to 35% [21,22,23,24,25,26,27,28].
Based on the distance of the OM from the hard plate of the tooth root, three categories can be recognized: (a) category I, in which the OMs are distant and separated from the tooth root; (b) category II, in which the apex of the screw grazes the hard lamina; (c) category III, in which the body of the screw invades the lamina dura. Categories I and II are characterized by a high success rate (75%), while in category III, the stability of OMs is significantly reduced, especially at the mandibular level (35%). In addition, incorrect positioning of OMs in relation to the tooth root leads to a double complication, namely mobility and failure of the OMs and injury to the tooth element [29].
There are existing reviews about the risks associated with the insertion of OMs related to other structures such as maxillary sinus or palatine artery, while the literature is expected about the complications on teeth. It is necessary for orthodontics to widely understand the potential dental risks that can occur using OMs, to avoid them, and to improve clinical practice [30,31,32]. The aim of this review was to evaluate tooth injuries after OMs insertion, in order to understand potential risks and dental complications associated with the use of OMs [33].
2. Materials and Methods
2.1. Protocol and Registration
This review was carried out according to the recommendations of the literature search Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) and recorded in the International Prospective Register of Systematic Review (PROSPERO) with the number CRD42022380972 [34].
2.2. Search Processing
We searched without a time limitation in PubMed, Cochrane, Web of Science, and Scopus to discover publications that matched our topic. The following Boolean keywords were included in the search strategy because they closely fit the goal of our examination, which primarily focuses on the damaging effects of OMs on teeth: (“orthodontic mini-screw” AND “tooth damage”) (Table 1).

Table 1.
Database search indicator.
2.3. Inclusion and Exclusion Criteria
The inclusion criteria were (1) studies only on humans; (2) English language, (3) open-access studies; (4) clinical trials or case reports. Studies regarding tooth damage in the presence of OMs, and studies dealing with surgical procedures, complications unconnected to teeth, OMs, or any other aspect of orthodontic care were excluded.
2.4. Data Processing
Disagreements between authors on article selection were discussed and resolved.
3. Results
The electronic database search identified a total of 99 studies (PubMed n = 45, Cochrane n = 1, Web of Science n = 18, and Scopus n = 35). After removing duplicates, 53 studies remained. Six more pertinent articles were added by looking over the reference list of acceptable publications. A total of 36 articles were excluded because they were off-topic, 9 were not available, and 2 were animal studies. The study selection and process are summarized in Figure 2. After a full-text review, a total of 13 studies met the inclusion criteria. A summary of the characteristics of each study included is presented in Table 2.
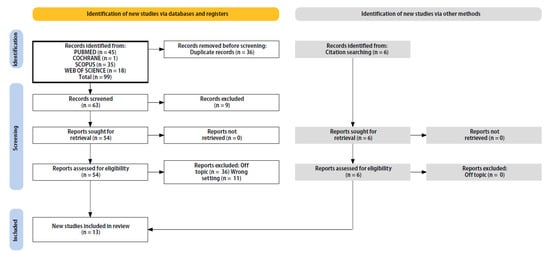
Figure 2.
Literature search Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram and database search indicators.

Table 2.
Characteristics of the included studies.
4. Discussion
Contact between the tooth root and the screw can cause trauma of the periodontal ligament or to the root, and this can lead to root resorption [48,49,50,51] (Figure 3).
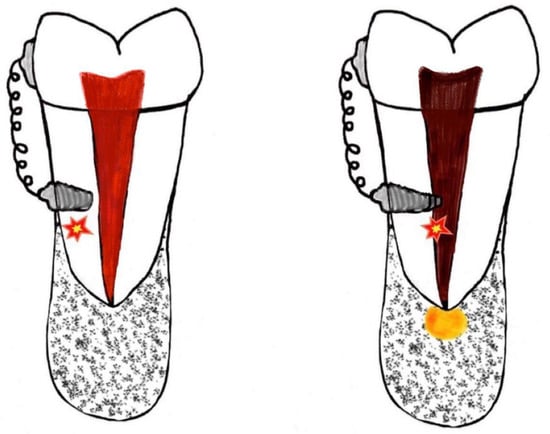
Figure 3.
Dental trauma may occur in the insertion of the OMs.
If the root is just superficially injured and there is no pulpal involvement, the injury will heal successfully by the deposition of cellular cementum once the contact has been broken [52]. In addition, a faster and complete repair takes place a few weeks after removing the screws [37]. The repair process can start as early as 7 to 10 days after the release of the force. Several studies have confirmed that 75% of the repair might be completed within 8 weeks [38], and others have demonstrated complete repair of the tooth and periodontium in 12 to 18 weeks after removal of the OM [48]. Others have demonstrated complete healing after almost 20 weeks, depending on the severity of the injury [53].
Kadioglu et al. examined the damage to the first premolars root surfaces in patients whose teeth must be extracted to correct a class II 2 division malocclusion [38]. The OM was placed near the roots of the right and left first and second premolars. The teeth of the control group that came into direct contact with the OM were extracted without the chance of repair; these teeth showed extensive damage at the root level. This study demonstrated that the injury in the root surfaces that have come into contact with the OM can be repaired through the reorganization of collagen fibers with no clinical consequences [38].
Ghanbarzadeh et al. studied the histological response of cementum, root dentin, and pulp, caused by intentional injury of the roots with self-tapping and self-drilling OMs [36]. The teeth were extracted eight weeks after the insertion of OMs, for the orthodontic treatment. Reparative cementum formation was observed in 75.4% of the teeth and there was no significant difference between the group with repair and the group with no repair regarding the formation of the restorative cement [36].
The effects of the contact of the OM with the dental root both at insertion and during orthodontic treatment have been described also by Baik et al. In both cases analyzed by the authors, the OMs were removed immediately, with pain relief, and relocated to other sites, without affecting the movement of the tooth and without loosening the screw. Cement contributed to root repair starting at 8 weeks after immediate screw or orthodontic strength removal. After approximately 12 months, there were no residual symptoms, such as ankylosis, discoloration, root canals, or pain. Orthodontic root movement in contact with the OM failed. By promptly removing the OMs, the problem of screw loosening was also avoided [40].
Lim et al. revealed that inappropriate and repeated insertion of OMs causes persistent periodontal inflammation and root damage, leading to pulp necrosis as well as refractory periapical periodontitis that necessitates surgical intervention. Accurate knowledge of the architecture and physiology of the root, tooth pulp, and periodontal tissue, as well as the benefits and restrictions of this technique, is crucial. In addition, a thorough evaluation of the damage done to both the root and the pulp and, finally, a careful consideration of the best treatment option are required [39].
The use of OMs usually never results in long-term problems. However, root injury can occasionally result in consequences such as ankylosis, osteosclerosis, and loss of tooth vitality. Ankylosis can occur if the damaged region is more than 4 mm or 20% of the root surface [37]. The close contact of dental roots appears to be the primary factor contributing to problems of surrounding teeth during implantation of OMs and following orthodontic loading [54]. Depending on the severity of the injury, a root fracture that involves the pulp tissue may cause the tooth to lose its vitality. Pulp vitality is lost when a screw penetrates the root by more than 50% of the screw’s diameter [41,55]. The periapical and surrounding periodontal tissues are destroyed as a result of the pulp necrosis that follows [37]. When the damage of root–screw contact is limited to the periodontal dental ligament (PDL), the injury is likely to be repaired with no further consequence, but if the cementum is mechanically damaged, and the dentin is exposed, multinucleated cells colonize the denuded surfaces and resorption takes place, supported by continuous stimulation [37,38,53]. Due to the persistence of continuous trauma and inflammation, a breach produced by the OM allowed outside pathogens to gain access to the PDL space and bony destruction around the roots, which ultimately resulted in pulp necrosis [35,56]. Radiological and histological testing can show injuries at the roots [37]. The loss of vitality is diagnosed with not being responsive to pulp sensitivity tests, such as cold tests and electric pulp testers. Apical radiography helps to reveal the clinical situation, at the insertion time and after the screw time removal. The insertion takes place in the attached gingiva until the drilling of the cortex [37,55,57,58]. The resulting symptoms are localized pressure and pain sensation, despite the topical anesthesia. The suspected trauma will be checked radiographically, and the clinician will screw out the fixture, in two or three turns to give relief from symptoms [48]. Once the radiographic confirmation of damage has been obtained, a root perforation can be treated through the access cavity. The treatment of a perforation concerns an intracanal approach. In case of failure of the conventional endodontic treatment, a surgical repair is indicated [35,37,43]. The surgical approach involves the creation of a bone window and consequent sealing of the perforation site with material such as mineral trioxide aggregate (MTA). The prognosis strongly depends on the treatment of bacterial infections at the perforation site [35,43].
The endodontic management of tooth damage after the insertion of OMs was analyzed by McCabe et al. The authors showed a case of accidental OM tip fracture during the insertion and included near the tooth (element 1.6) [41]. More than 1 week later, a sinus tract over 1.6 was noted, but the tooth responded positively to sensitivity testing. The retained screw was surgically removed and the 1.6 tooth seemed to be asymptomatic for 9 months until the end of orthodontic treatment when the fistula reappeared. The patient referred a history of pain that was made worse by cold. To percussion, the tooth was just mildly sensitive. The mobility was normal and periodontal probing was 3 mm interproximal to 1 mm buccally and lingually. Intraoral radiography showed a lesion in proximity to mesiobuccally and palatal roots. The endodontic treatment of MB and MB2 needed an apicectomy below the perforation. A 5-year follow-up revealed a favorable outcome with no signs and symptoms. It is crucial to obtain periapical radiographs of the intended implant location. Intraoral radiographs are not typically performed by most orthodontists. However, a two-dimensional picture cannot be used to determine the precise location of the roots. In addition, this report shows the favorable outcome of a iatrogenic perforation caused by the insertion of OMs [41].
Histological examinations, through specific coloration, e.g., blue of toluidine, allow for understanding the mechanisms of damage and repair lining the root, with details about cementum, PDL, and bone [54]. If the defect on the root surface is repaired, histological examination revealed woven bone at the insertion site and positive staining due to the activity of cementoblasts, which starts after the screw removal at the earliest 12 weeks, and lasts up for 18 or 20 weeks [54]. Through high-powered observation, Ahmed et al. found that the newly formed concrete was strongly oriented irregularly in confront to the normal healing and brownish red hemosiderin in pigmentation in several areas of the repaired cement [35]. The inner layer of Dentin Pulp Complex (DPC), following the “S” shaped dentinal tubules, revealed abnormal deposition of pre-dentine along normal uninvolved root surfaces. The DPC exposed an hematophilic area, indicating a more maturing, old, or new predentine and an eosinophilic area referring to a newly deposit predentine. The histological examination detected an increased level of predentine in the site of the OMs insertion and an irregular orientation in the external surface of dentin, while the internal zone presented numerous globular vacuolar spaces with a completely irregular outline. In the external fascia of the predentine, hemosiderin pigments were also detected. The formation of cementum around the dentin is believed to be due to two causes, i.e., the engulfment of cementum particles during the repair process and the differentiation of the periodontal ligament cells into cementum-producing cells. The presence of irregular vacuoles in the internal surface of neodentin indicates an injury of the pulp due to OMs insertion. The hyperproduction of hemosiderin in the predentine is the reflection of abnormal bleeding at the site of the trauma by OMs insertion, which may be related to the release of metal ions, e.g., vanadium and aluminum, and to altered pH [35]. However, the resorption process will end on its own if there is no additional stimulation, and a phase of healing with tissue similar to cementum will begin [37,59]. These issues result from the placement of OM in the alveolar process between roots, which needs a crucial pre-evaluation [25]. During inter-radicular placement, the clinician may change accidentally the angle of insertion, significantly increasing the risk of damage. Indeed, the available space between roots is more in the apical zone, but without attached gingiva. Thus, the clinician must remain in the “safe zones”: allowing 2 mm from the root, at least 1.0 to 5.0 mm [35]. Specifically, in the upper arch, the OM placement over the greater palatine artery increases the risk of palatal root contact and loss of biomechanical control [38,48,60,61]. In the lower arch, we could see nerve involvement, and the clinical recommendation is to use a short retromolar OM, In this case, many authors have reported measurements with screws no longer than 8 mm, and placed them in the buccal retromolar region below the anterior ramus, for the mandibular site [48,62] (Figure 4).
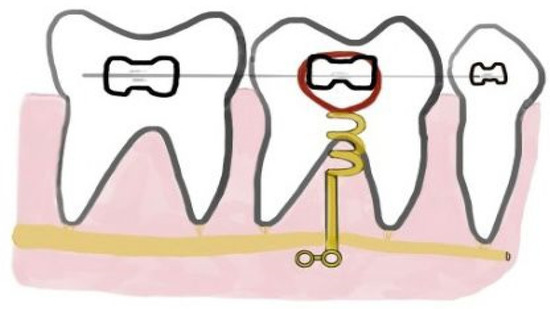
Figure 4.
Attention to the insertion of orthodontic miniscrew (OMs) in the presence of the inferior alveolar nerve.
Hwang et al. described the root injury arising from the placement of OMs in a mandibular incisor and the management of this complication [37]. One of the two inserted OMs, between the central and lateral incisors, inserted to obtain anterior sector intrusion pierced the root of the right lateral incisor. After detecting no vitality of the tooth and considering the radiolucency in the apical area on X-ray, apicectomy was performed, closing the perforation through the application of MTA [37,63]. The degree of root injury was related to the degree of injury. When the screw–root interface was restricted to the area of the periodontal ligament, the injury could be healed without further sequelae [37,64]. If the cementum was mechanically destroyed and dentin was revealed, multinucleated cells would colonize the surfaces and resorption would begin. Without additional stimulation, the reabsorption phenomenon stopped spontaneously, and cement-like tissue occurred within 2 to 3 weeks [37,65]. However, an irreversible reaction could have resulted when the affected zone was large or the injury was deep, so endodontic and surgical treatment was performed, and the perforation of the root was treated with MTA [37,66].
The major limitation of this review concerns the quantity and quality of the articles included in the study. Currently, in the literature, the number of studies concerning adverse effects and complications of OM is low and of a low methodological level: most articles analyze a very limited number of cases and do not include adequate control groups.
This review aimed to investigate the damage caused by OMs by focusing only on teeth damage. This choice was made considering that there are already reviews in the literature dealing with the damage of OMs to other tissues in the oral cavity, such as the maxillary sinus, or the general risks due to the insertion of OMs. With the exception to pay more attention during insertion, no other procedure for optimal OMs placement can be obtained. More consisting randomized controlled trials are needed to provide evidence-based guidelines to clinicians.
5. Conclusions
Anchorage control is one of the most challenging problems in orthodontics. It is achieved with OMs, which have been used frequently because they prevent unintended tooth movement and reduce the dependence on patient cooperation, increasing the predictability of achieving treatment goals. During orthodontic treatment, the choice of an appropriate site for OMs placement is more important than the insertion technique. Site selection requires recognition of the anatomy of the tooth roots and pulp, the distance between the tooth roots, and the physiology of the structures surrounding the tooth, such as the periodontal complex. Placement of OMs is a critical procedure, and even if preventive measures are taken, such as an apical radiograph before screw placement, root damage can occur. Screw–tooth contact does arise, but the incidence of clinically relevant injury seems to be low. When screw–root contact injury is limited to the periodontal structures, the lesion is usually repaired without further consequences. In many cases, cement healing was observed after the injury was intentionally caused on the tooth, and the two approaches to placing the OMs, self-tapping and self-drilling, showed no relevant differences in the healing process. Healing was achieved by eliminating continuous contact with the tooth and was achieved by prompt removal of the screws or springs tipping of the screw. In case of extensive damage to the dental root and iatrogenic perforations, endodontic and surgical treatment had to be performed to manage this complication. Despite the lack of clinically significant damage in the patients examined, clinicians must be prudent in the placement of OMs. More accurate planning of OMs placement is required to minimize the risk of root damage.
Finally, the results showed that whether the insertion of OMs is performed accurately, dental complications in most cases are minor and sometimes resolve spontaneously. Therefore, the application of OMs was found to be a safe procedure with few adverse effects. This turns out to be important in orthodontics where miniscrews are a very valuable tool for the resolution of even complex cases.
However, considering the low number of patients analyzed in this review, further studies are necessary in the future to investigate and analyze the topic more comprehensively and to draw up a list of evidence-based clinical recommendations.
Author Contributions
Conceptualization, A.M.I., A.D.I., G.M., S.C., F.P., F.L., A.P. and C.D.P.; methodology, G.P., E.d.R., V.C., S.C., S.S., M.C. and A.N.; software, F.I. and G.D.; validation, F.L., I.R.B., D.D.V., M.C.F., F.P., F.I. and G.D.; formal analysis, A.D.I., F.P., A.P., G.M.T., I.F., D.D.V., F.I. and G.D.; resources, A.D.I., A.M.I., G.M., S.S., C.D.P., A.N., M.C. and V.S.; data curation, P.A., I.R.B., E.d.R., F.L., F.I., V.S. and G.D.; writing—original draft preparation, A.D.I., A.M.I., S.S., E.d.R., F.P., D.D.V., A.N., F.I. and G.D.; writing—review and editing, P.A., A.P., V.C., S.S., M.C., I.F., M.C.F., G.P., I.R.B. and A.P.; visualization, G.P, C.D.P., F.L., A.P. and I.R.B.; supervision, A.D.I., A.M.I., F.P., G.M., D.D.V., F.I. and G.D.; project administration, I.R.B., S.S., G.M.T., F.L., F.I. and G.D. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
We thank the following for their cooperation: Antonio Scarano, Gregorio Paduanelli, Biagio Rapone, and Antonio Mancini.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| CBCT | Computer-Aided Design—Computer-Aided Manufacturing |
| DPC | Dentin Pulp Complex |
| OM | Orthodontic miniscrew |
| OMs | Orthodontic miniscrews |
| PDL | Periodontal dental ligament |
| SEM | Scanning Electron Microscopy |
| TAD | Temporary Anchorage Devices |
| TC | Tac Cone Beam |
References
- Antoszewska-Smith, J.; Sarul, M.; Łyczek, J.; Konopka, T.; Kawala, B. Effectiveness of Orthodontic Miniscrew Implants in Anchorage Reinforcement during En-Masse Retraction: A Systematic Review and Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2017, 151, 440–455. [Google Scholar] [CrossRef]
- Adina, S.; Dipalma, G.; Bordea, I.R.; Lucaciu, O.; Feurdean, C.; Inchingolo, A.D.; Septimiu, R.; Malcangi, G.; Cantore, S.; Martin, D.; et al. Orthopedic Joint Stability Influences Growth and Maxillary Development: Clinical Aspects. J. Biol. Regul. Homeost. Agents 2020, 34, 747–756. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Ferrara, I.; Viapiano, F.; Netti, A.; Campanelli, M.; Buongiorno, S.; Latini, G.; Carpentiere, V.; Ciocia, A.M.; Ceci, S.; et al. Rapid Maxillary Expansion on the Adolescent Patient: Systematic Review and Case Report. Children 2022, 9, 1046. [Google Scholar] [CrossRef]
- Nucera, R.; Costa, S.; Bellocchio, A.M.; Barbera, S.; Drago, S.; Silvestrini, A.; Migliorati, M. Evaluation of Palatal Bone Depth, Cortical Bone, and Mucosa Thickness for Optimal Orthodontic Miniscrew Placement Performed According to the Third Palatal Ruga Clinical Reference. Eur. J. Orthod. 2022, 44, 530–536. [Google Scholar] [CrossRef]
- Aiello, D.; Nucera, R.; Costa, S.; Figliuzzi, M.M.; Paduano, S. A Simplified Digital Approach to the Treatment of a Postpuberty Patient with a Class III Malocclusion and Bilateral Crossbite. Case Rep. Dent. 2021, 2021, 3883187. [Google Scholar] [CrossRef] [PubMed]
- Inchingolo, F.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; Tarullo, A.; Inchingolo, A.D.; Dipalma, G.; Podo Brunetti, S.; Tarullo, A.; Cagiano, R. Combined Occlusal and Pharmacological Therapy in the Treatment of Temporo-Mandibular Disorders. Eur. Rev. Med. Pharmacol. Sci. 2011, 15, 1296–1300. [Google Scholar] [PubMed]
- Lee, D.; Park, J.H.; Bay, R.C.; Choi, S.; Chae, J. Cortical Bone Thickness and Bone Density Effects on Miniscrew Success Rates: A Systematic Review and Meta-analysis. Orthod. Craniofac. Res. 2021, 24, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, M.V.; Codrington, J.; Fletcher, L.; Dreyer, C.W.; Sampson, W.J. The Influence of Miniscrew Insertion Torque. Eur. J. Orthod. 2018, 40, 37–44. [Google Scholar] [CrossRef]
- Golshah, A.; Gorji, K.; Nikkerdar, N. Effect of Miniscrew Insertion Angle in the Maxillary Buccal Plate on Its Clinical Survival: A Randomized Clinical Trial. Prog. Orthod. 2021, 22, 22. [Google Scholar] [CrossRef]
- Yoon, J.-H.; Cha, J.-Y.; Choi, Y.J.; Park, W.-S.; Han, S.-S.; Lee, K.-J. Simulation of Miniscrew-Root Distance Available for Molar Distalization Depending on the Miniscrew Insertion Angle and Vertical Facial Type. PLoS ONE 2020, 15, e0239759. [Google Scholar] [CrossRef]
- Janson, G.; Gigliotti, M.P.; Estelita, S.; Chiqueto, K. Influence of Miniscrew Dental Root Proximity on Its Degree of Late Stability. Int. J. Oral Maxillofac. Surg. 2013, 42, 527–534. [Google Scholar] [CrossRef]
- Alkadhimi, A.; Al-Awadhi, E.A. Miniscrews for Orthodontic Anchorage: A Review of Available Systems. J. Orthod. 2018, 45, 102–114. [Google Scholar] [CrossRef]
- Jedliński, M.; Janiszewska-Olszowska, J.; Mazur, M.; Grocholewicz, K.; Suárez Suquía, P.; Suárez Quintanilla, D. How Does Orthodontic Mini-Implant Thread Minidesign Influence the Stability? Systematic Review with Meta-Analysis. J. Clin. Med. 2022, 11, 5304. [Google Scholar] [CrossRef] [PubMed]
- Jedliński, M.; Janiszewska-Olszowska, J.; Mazur, M.; Ottolenghi, L.; Grocholewicz, K.; Galluccio, G. Guided Insertion of Temporary Anchorage Device in Form of Orthodontic Titanium Miniscrews with Customized 3D Templates—A Systematic Review with Meta-Analysis of Clinical Studies. Coatings 2021, 11, 1488. [Google Scholar] [CrossRef]
- Papageorgiou, S.N.; Zogakis, I.P.; Papadopoulos, M.A. Failure Rates and Associated Risk Factors of Orthodontic Miniscrew Implants: A Meta-Analysis. Am. J. Orthod. Dentofac. Orthop. 2012, 142, 577–595.e7. [Google Scholar] [CrossRef]
- Dimonte, M.; Inchingolo, F.; Minonne, A.; Arditi, G.; Dipalma, G. Bone SPECT in Management of Mandibular Condyle Hyperplasia. Report of a Case and Review of Literature. Minerva Stomatol. 2004, 53, 281–285. [Google Scholar] [PubMed]
- Inchingolo, F.; Ballini, A.; Cagiano, R.; Inchingolo, A.D.; Serafini, M.; De Benedittis, M.; Cortelazzi, R.; Tatullo, M.; Marrelli, M.; Inchingolo, A.M.; et al. Immediately Loaded Dental Implants Bioactivated with Platelet-Rich Plasma (PRP) Placed in Maxillary and Mandibular Region. Clin. Ther. 2015, 166, e146–e152. [Google Scholar] [CrossRef]
- Chauhan, P.; Garg, A.; Mittal, R.; Kumar, H. A Comparative Evaluation of Fracture Resistance of Endodontically Treated Teeth Using Four Different Intraorifice Barriers: An In Vitro Study. J. Conserv. Dent. 2019, 22, 420–424. [Google Scholar] [CrossRef]
- Kuroda, S.; Sugawara, Y.; Deguchi, T.; Kyung, H.-M.; Takano-Yamamoto, T. Clinical Use of Miniscrew Implants as Orthodontic Anchorage: Success Rates and Postoperative Discomfort. Am. J. Orthod. Dentofac. Orthop. 2007, 131, 9–15. [Google Scholar] [CrossRef]
- Kuroda, S.; Yamada, K.; Deguchi, T.; Hashimoto, T.; Kyung, H.-M.; Yamamoto, T.T. Root Proximity Is a Major Factor for Screw Failure in Orthodontic Anchorage. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S68–S73. [Google Scholar] [CrossRef]
- Cantarella, D.; Savio, G.; Grigolato, L.; Zanata, P.; Berveglieri, C.; Lo Giudice, A.; Isola, G.; Del Fabbro, M.; Moon, W. A New Methodology for the Digital Planning of Micro-Implant-Supported Maxillary Skeletal Expansion. Med. Devices 2020, 13, 93–106. [Google Scholar] [CrossRef]
- Inchingolo, A.D.; Malcangi, G.; Semjonova, A.; Inchingolo, A.M.; Patano, A.; Coloccia, G.; Ceci, S.; Marinelli, G.; Di Pede, C.; Ciocia, A.M.; et al. Oralbiotica/Oralbiotics: The Impact of Oral Microbiota on Dental Health and Demineralization: A Systematic Review of the Literature. Children 2022, 9, 1014. [Google Scholar] [CrossRef]
- Tartaglia, G.M.; Mapelli, A.; Maspero, C.; Santaniello, T.; Serafin, M.; Farronato, M.; Caprioglio, A. Direct 3D Printing of Clear Orthodontic Aligners: Current State and Future Possibilities. Materials 2021, 14, 1799. [Google Scholar] [CrossRef]
- Farronato, M.; Maspero, C.; Abate, A.; Grippaudo, C.; Connelly, S.T.; Tartaglia, G.M. 3D Cephalometry on Reduced FOV CBCT: Skeletal Class Assessment through AF-BF on Frankfurt Plane—Validity and Reliability through Comparison with 2D Measurements. Eur. Radiol. 2020, 30, 6295–6302. [Google Scholar] [CrossRef] [PubMed]
- Jeong, D.-M.; Oh, S.H.; Choo, H.; Choi, Y.-S.; Kim, S.-H.; Lee, J.-S.; Hwang, E.-H. Root Proximity of the Anchoring Miniscrews of Orthodontic Miniplates in the Mandibular Incisal Area: Cone-Beam Computed Tomographic Analysis. Korean J. Orthod. 2021, 51, 231–240. [Google Scholar] [CrossRef] [PubMed]
- Miyazawa, K.; Kawaguchi, M.; Tabuchi, M.; Goto, S. Accurate Pre-Surgical Determination for Self-Drilling Miniscrew Implant Placement Using Surgical Guides and Cone-Beam Computed Tomography. Eur. J. Orthod. 2010, 32, 735–740. [Google Scholar] [CrossRef] [PubMed]
- Bae, M.-J.; Kim, J.-Y.; Park, J.-T.; Cha, J.-Y.; Kim, H.-J.; Yu, H.-S.; Hwang, C.-J. Accuracy of Miniscrew Surgical Guides Assessed from Cone-Beam Computed Tomography and Digital Models. Am. J. Orthod. Dentofac. Orthop. 2013, 143, 893–901. [Google Scholar] [CrossRef]
- Cassetta, M.; Altieri, F.; Di Giorgio, R.; Barbato, E. Palatal Orthodontic Miniscrew Insertion Using a CAD-CAM Surgical Guide: Description of a Technique. Int. J. Oral Maxillofac. Surg. 2018, 47, 1195–1198. [Google Scholar] [CrossRef] [PubMed]
- Piras, D.; Garau, V.; Scalas, M.; Carini, F. Miniviti Ortodontiche: Protocollo Chirurgico Orthodontic Mini-Screws: Surgical Technique. Eur. J. Implant. Prosthodont. 2008, 1, 34. [Google Scholar]
- Mohammed, H.; Wafaie, K.; Rizk, M.Z.; Almuzian, M.; Sosly, R.; Bearn, D.R. Role of Anatomical Sites and Correlated Risk Factors on the Survival of Orthodontic Miniscrew Implants: A Systematic Review and Meta-Analysis. Prog. Orthod. 2018, 19, 36. [Google Scholar] [CrossRef]
- Poggio, P.M.; Incorvati, C.; Velo, S.; Carano, A. “Safe Zones”: A Guide for Miniscrew Positioning in the Maxillary and Mandibular Arch. Angle Orthod. 2006, 76, 191–197. [Google Scholar] [CrossRef]
- Jones, J.P.; Elnagar, M.H.; Perez, D.E. Temporary Skeletal Anchorage Techniques. Oral Maxillofac. Surg. Clin. North Am. 2020, 32, 27–37. [Google Scholar] [CrossRef] [PubMed]
- Truong, V.M.; Kim, S.; Kim, J.; Lee, J.W.; Park, Y.-S. Revisiting the Complications of Orthodontic Miniscrew. BioMed Res. Int. 2022, 2022, 8720412. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, V.K.S.; Krishnaswamy, N.R.; Thavarajah, R. Miniscrew Implant Fracture and Effects of Such Retained Tip on Dentin-Pulp Complex: A Histological Report. Dent. Traumatol. 2016, 32, 161–165. [Google Scholar] [CrossRef]
- Ghanbarzadeh, M.; Heravi, F.; Abrishamchi, R.; Shafaee, H.; Ghazi, N.; Heravi, P.; Ghanbarzadeh, H. Cementum and Dentin Repair Following Root Damage Caused by the Insertion of Self-Tapping and Self-Drilling Miniscrews. J. Orthod. Sci. 2017, 6, 91–96. [Google Scholar] [CrossRef]
- Hwang, Y.-C.; Hwang, H.-S. Surgical Repair of Root Perforation Caused by an Orthodontic Miniscrew Implant. Am. J. Orthod. Dentofac. Orthop. 2011, 139, 407–411. [Google Scholar] [CrossRef]
- Kadioglu, O.; Büyükyilmaz, T.; Zachrisson, B.U.; Maino, B.G. Contact Damage to Root Surfaces of Premolars Touching Miniscrews during Orthodontic Treatment. Am. J. Orthod. Dentofac. Orthop. 2008, 134, 353–360. [Google Scholar] [CrossRef] [PubMed]
- Lim, G.; Kim, K.-D.; Park, W.; Jung, B.-Y.; Pang, N.-S. Endodontic and Surgical Treatment of Root Damage Caused by Orthodontic Miniscrew Placement. J. Endod. 2013, 39, 1073–1077. [Google Scholar] [CrossRef]
- Baik, U.; Kook, Y.-A.; Tanaka, O.M.; Kim, K.B. Root Contact with Miniscrews during Mesiodistal Movement of the Molar. J. World Fed. Orthod. 2014, 3, e95–e100. [Google Scholar] [CrossRef]
- McCabe, P.; Kavanagh, C. Root Perforation Associated with the Use of a Miniscrew Implant Used for Orthodontic Anchorage: A Case Report. Int. Endod. J. 2012, 45, 678–688. [Google Scholar] [CrossRef] [PubMed]
- Maino, B.G.; Weiland, F.; Attanasi, A.; Zachrisson, B.U.; Buyukyilmaz, T. Root Damage and Repair after Contact with Miniscrews. J. Clin. Orthod. 2007, 41, 762–766, quiz 750. [Google Scholar]
- Ahmed, V.K.S.; Rooban, T.; Krishnaswamy, N.R.; Mani, K.; Kalladka, G. Root Damage and Repair in Patients with Temporary Skeletal Anchorage Devices. Am. J. Orthod. Dentofac. Orthop. 2012, 141, 547–555. [Google Scholar] [CrossRef]
- Hourfar, J.; Bister, D.; Lisson, J.A.; Ludwig, B. Incidence of Pulp Sensibility Loss of Anterior Teeth after Paramedian Insertion of Orthodontic Mini-Implants in the Anterior Maxilla. Head Face Med. 2017, 13, 1. [Google Scholar] [CrossRef]
- Yerawadekar, S.A.; Rahalkar, J.S.; Darda, M.; Sarode, S.C.; Sarode, G.S. Histological Evaluation of Root Repair after Damage Due to Intentional Contact with Orthodontic Micro-Screw Implants: An In Vivo Study. JCDR 2018, 12, 1–4. [Google Scholar] [CrossRef]
- Shinohara, A.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Root Proximity and Inclination of Orthodontic Mini-Implants after Placement: Cone-Beam Computed Tomography Evaluation. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Çelik Güler, Ö.; Malkoç, S. Effects of Orthodontic Force on Root Surface Damage Caused by Contact with Temporary Anchorage Devices and on the Repair Process. Korean J. Orthod. 2019, 49, 106. [Google Scholar] [CrossRef]
- Kravitz, N.D.; Kusnoto, B. Risks and Complications of Orthodontic Miniscrews. Am. J. Orthod. Dentofac. Orthop. 2007, 131, S43–S51. [Google Scholar] [CrossRef]
- Watanabe, H.; Deguchi, T.; Hasegawa, M.; Ito, M.; Kim, S.; Takano-Yamamoto, T. Orthodontic Miniscrew Failure Rate and Root Proximity, Insertion Angle, Bone Contact Length, and Bone Density: Failure Factors for Orthodontic Miniscrew. Orthod. Craniofacial Res. 2013, 16, 44–55. [Google Scholar] [CrossRef]
- Ikenaka, R.; Koizumi, S.; Otsuka, T.; Yamaguchi, T. Effects of Root Contact Length on the Failure Rate of Anchor Screw. J. Oral Sci. 2022, 64, 232–235. [Google Scholar] [CrossRef]
- Chen, Y.-H.; Chang, H.-H.; Chen, Y.-J.; Lee, D.; Chiang, H.-H.; Jane Yao, C.-C. Root Contact during Insertion of Miniscrews for Orthodontic Anchorage Increases the Failure Rate: An Animal Study. Clin. Oral Implant. Res. 2008, 19, 99–106. [Google Scholar] [CrossRef]
- Inchingolo, F.; Martelli, F.S.; Gargiulo Isacco, C.; Borsani, E.; Cantore, S.; Corcioli, F.; Boddi, A.; Nguyễn, K.C.D.; De Vito, D.; Aityan, S.K.; et al. Chronic Periodontitis and Immunity, towards the Implementation of a Personalized Medicine: A Translational Research on Gene Single Nucleotide Polymorphisms (SNPs) Linked to Chronic Oral Dysbiosis in 96 Caucasian Patients. Biomedicines 2020, 8, 115. [Google Scholar] [CrossRef] [PubMed]
- Dao, V.; Renjen, R.; Prasad, H.S.; Rohrer, M.D.; Maganzini, A.L.; Kraut, R.A. Cementum, Pulp, Periodontal Ligament, and Bone Response after Direct Injury with Orthodontic Anchorage Screws: A Histomorphologic Study in an Animal Model. J. Oral Maxillofac. Surg. 2009, 67, 2440–2445. [Google Scholar] [CrossRef] [PubMed]
- Asscherickx, K.; Vannet, B.V.; Wehrbein, H.; Sabzevar, M.M. Root Repair after Injury from Mini-Screw. Clin. Oral Implant. Res. 2005, 16, 575–578. [Google Scholar] [CrossRef] [PubMed]
- Gopikrishna, V.; Pradeep, G.; Venkateshbabu, N. Assessment of Pulp Vitality: A Review. Int. J. Paediatr. Dent. 2009, 19, 3–15. [Google Scholar] [CrossRef]
- Chauhan, R.; Rasaratnam, L.; Alani, A.; Djemal, S. Adult Dental Trauma: What Should the Dental Practitioner Know? Prim. Dent. J. 2016, 5, 70–81. [Google Scholar] [CrossRef]
- Alghaithy, R.A.; Qualtrough, A.J.E. Pulp Sensibility and Vitality Tests for Diagnosing Pulpal Health in Permanent Teeth: A Critical Review. Int. Endod. J. 2017, 50, 135–142. [Google Scholar] [CrossRef]
- Han, G.; Hu, M.; Zhang, Y.; Jiang, H. Pulp Vitality and Histologic Changes in Human Dental Pulp after the Application of Moderate and Severe Intrusive Orthodontic Forces. Am. J. Orthod. Dentofac. Orthop. 2013, 144, 518–522. [Google Scholar] [CrossRef] [PubMed]
- Brisceno, C.E.; Rossouw, P.E.; Carrillo, R.; Spears, R.; Buschang, P.H. Healing of the Roots and Surrounding Structures after Intentional Damage with Miniscrew Implants. Am. J. Orthod. Dentofac. Orthop. 2009, 135, 292–301. [Google Scholar] [CrossRef]
- Cantore, S.; Ballini, A.; De Vito, D.; Martelli, F.S.; Georgakopoulos, I.; Almasri, M.; Dibello, V.; Altini, V.; Farronato, G.; Dipalma, G.; et al. Characterization of Human Apical Papilla-Derived Stem Cells. J. Biol. Regul. Homeost. Agents 2017, 31, 901–910. [Google Scholar]
- Yi, J.; Ge, M.; Li, M.; Li, C.; Li, Y.; Li, X.; Zhao, Z. Comparison of the Success Rate between Self-Drilling and Self-Tapping Miniscrews: A Systematic Review and Meta-Analysis. Eur. J. Orthod. 2017, 39, 287–293. [Google Scholar] [CrossRef]
- Son, S.; Motoyoshi, M.; Uchida, Y.; Shimizu, N. Comparative Study of the Primary Stability of Self-Drilling and Self-Tapping Orthodontic Miniscrews. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 480–485. [Google Scholar] [CrossRef]
- Aminoshariae, A.; Hartwell, G.R.; Moon, P.C. Placement of Mineral Trioxide Aggregate Using Two Different Techniques. J. Endod. 2003, 29, 679–682. [Google Scholar] [CrossRef]
- Fabbroni, G.; Aabed, S.; Mizen, K.; Starr, D.G. Transalveolar Screws and the Incidence of Dental Damage: A Prospective Study. Int. J. Oral Maxillofac. Surg. 2004, 33, 442–446. [Google Scholar] [CrossRef] [PubMed]
- Tronstad, L. Root Resorption—Etiology, Terminology and Clinical Manifestations. Endod. Dent. Traumatol. 1988, 4, 241–252. [Google Scholar] [CrossRef] [PubMed]
- Holland, R.; Filho, J.A.; de Souza, V.; Nery, M.J.; Bernabé, P.F.; Dezan, E., Jr. Mineral Trioxide Aggregate Repair of Lateral Root Perforations. J. Endod. 2001, 27, 281–284. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).