“Students Moving Together”, Tailored Exercise for Students Facing Mental Health Challenges—A Pilot Feasibility Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Sample Size
2.4. Tailored Group Exercise Intervention
2.5. Measurements
2.5.1. Feasibility
2.5.2. Mental Health and Physical Fitness
2.6. Statistical Analysis
3. Results
3.1. Sample Characteristics
3.2. Feasibility Analyses
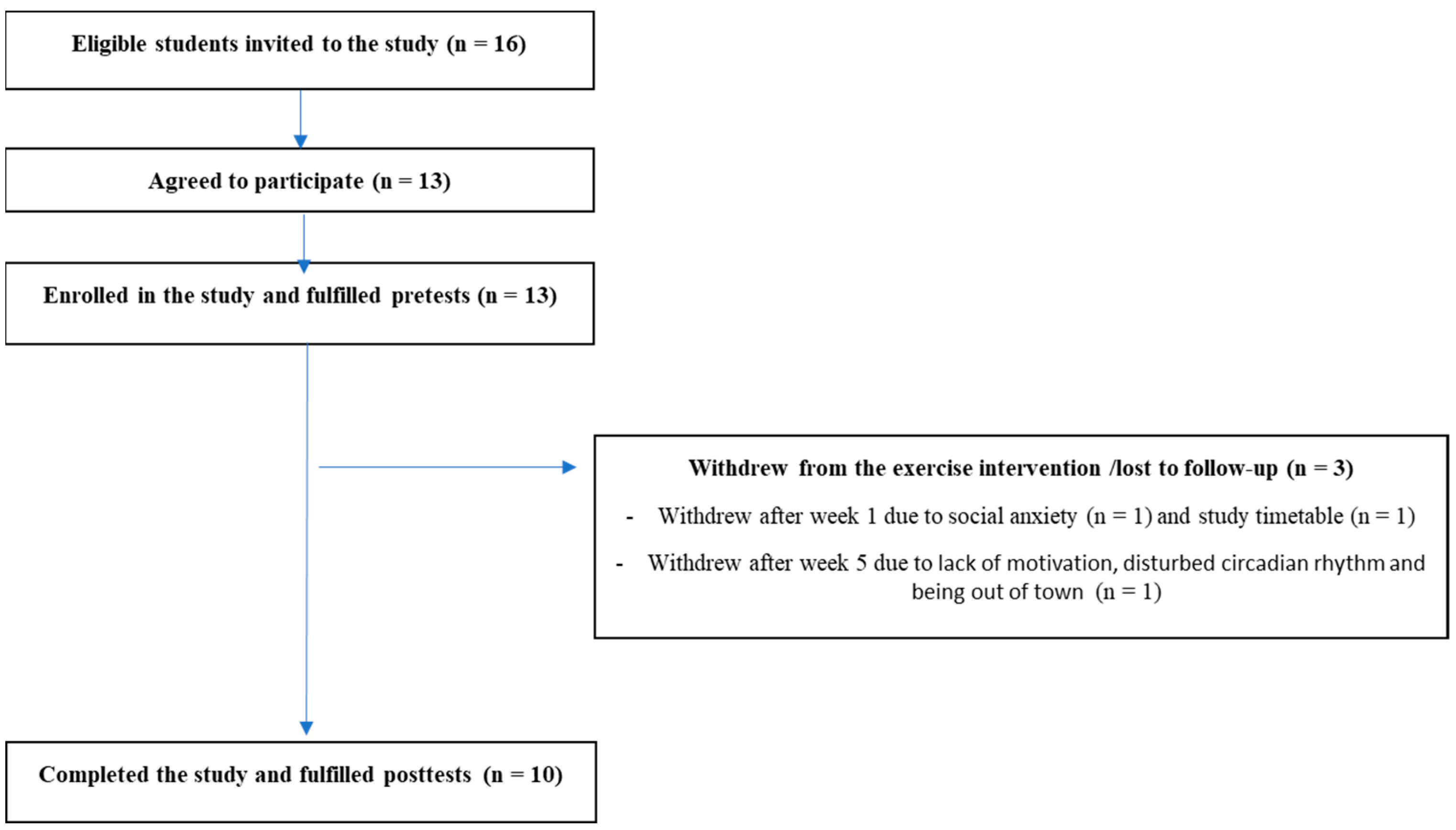
3.2.1. Recruitment
3.2.2. Dropouts
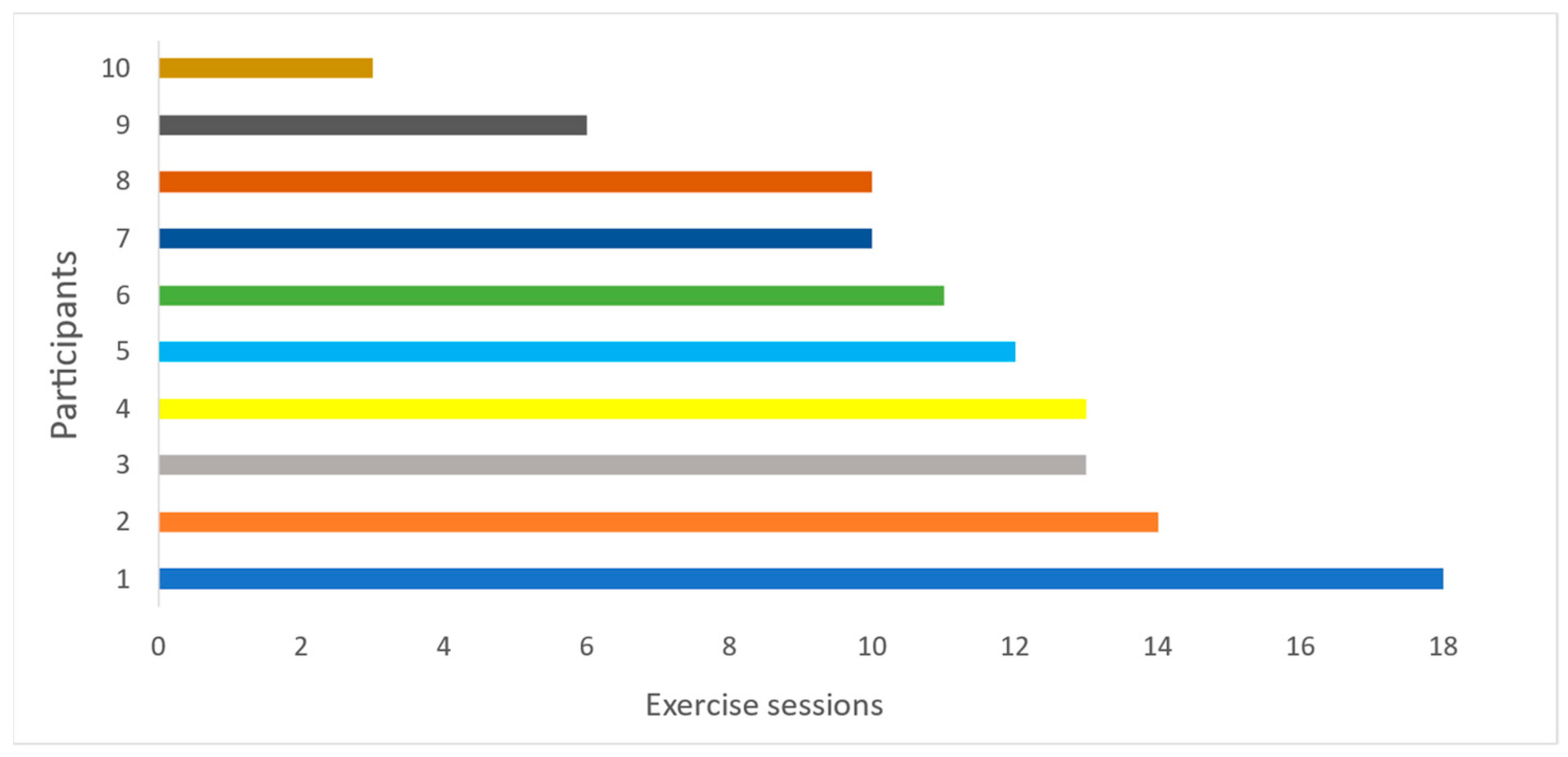
3.2.3. Attendance
3.2.4. Adverse Events
3.3. Preliminary Effectiveness
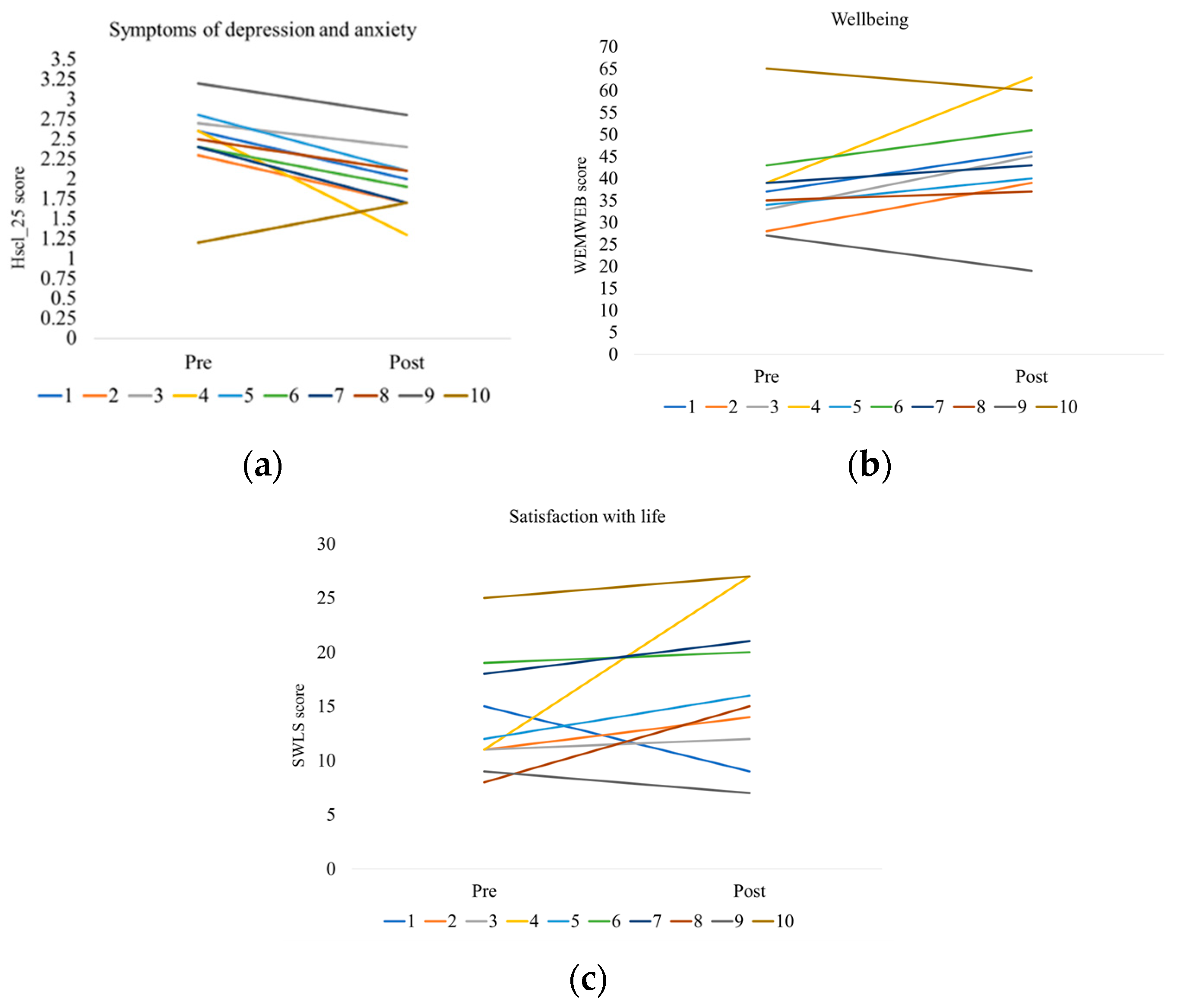
3.3.1. Mental Health, Well-Being, and Satisfaction with Life
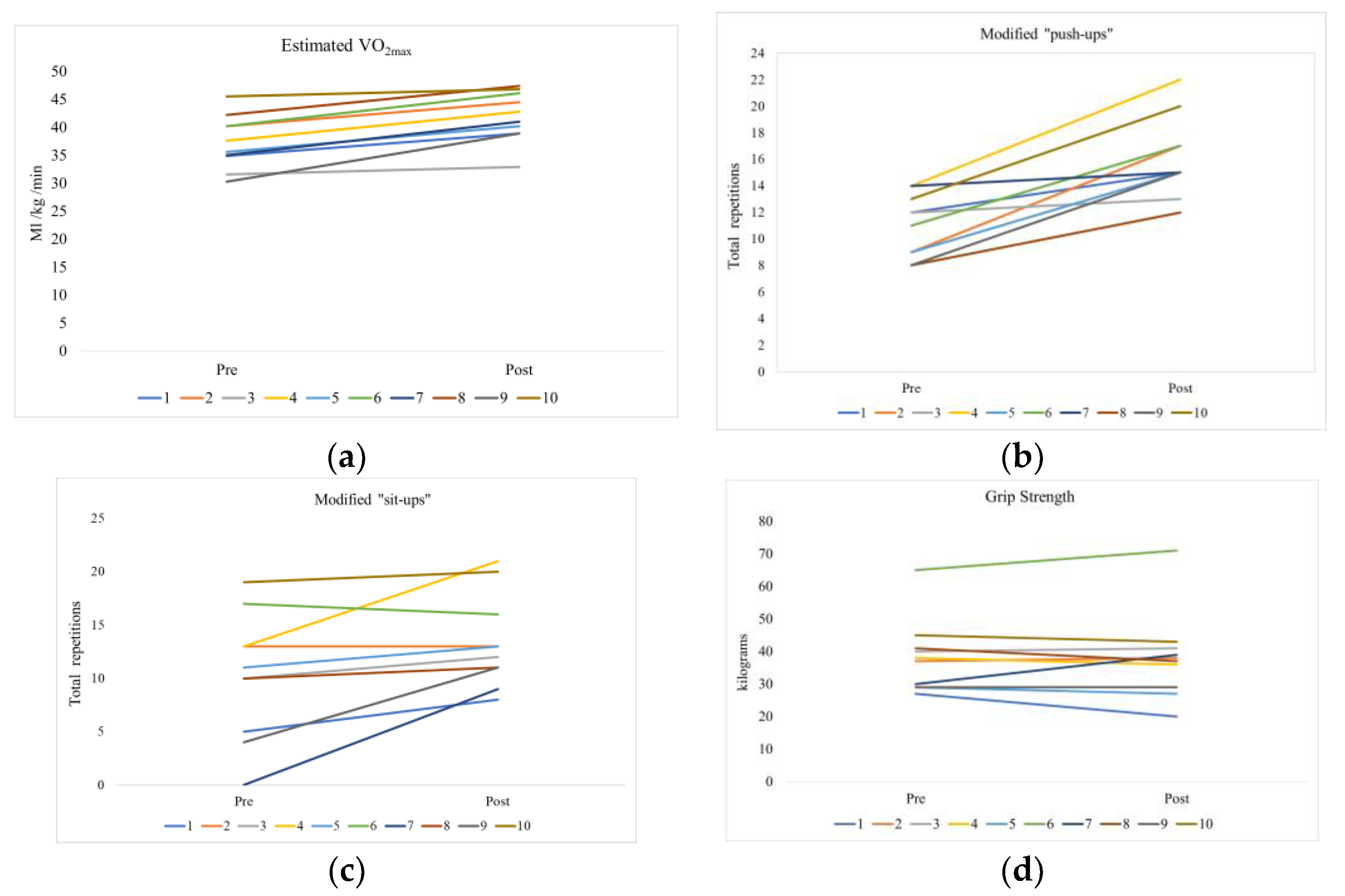
3.3.2. Physical Fitness
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. Mental Disorders, Key Facts. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 30 April 2021).
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1.9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, B.; Borg, M. Recovery Tradisjoner, Fornyelser og Praksiser, 1st ed.; Gyldendal Norsk Forlag AS: Oslo, Norway, 2017. [Google Scholar]
- Topor, A. Hva Hjelper? Veier til Bedring fra Alvorlige Psykiske Problemer; Kommuneforlaget: Oslo, Norway, 2011. [Google Scholar]
- Martinsen, E.W. Fysisk aktivitet og psykiske lidelser. In Fysisk Aktivitet og Helse. Fra Begrepsforståelse til Implementering av Kunnskap, 1st ed.; Klungland Torstveit, M., Lohne-Seiler, H., Berntsen, S., Anderssen, S.A., Eds.; Cappelen Damm Akademisk: Oslo, Norway, 2018; pp. 245–268. [Google Scholar]
- Sivertsen, B.; Johansen, M.S. Studentenes Helse- og Trivselsundersøkelse 2022. Hovedrapport 2022; Folkehelseinstituttet: Oslo, Norway, 2022; ISBN 978-82-691382-2-1. [Google Scholar]
- Mordal, S.; Ness, o. Hva vet vi om Studenters Psykiske Helse og Livskvalitet?—En Litteraturgjennomgang av Skandinaviske Studenters Psykiske Helse og Livskvalitet, og Hvilke Tiltak og Intervensjoner som har Vist Effekt; IPLs rapportserie. Nr. 2/2021; NTNU Institutt for Pedagogikk og Livslang Læring: Oslo, Norway, 2021; ISSN 2535-7142. [Google Scholar]
- Lien, L. Hva kan leger og psykologer lære av historiene? In Et Bedre liv. Historier, Erfaringer og Forskning om Recovery ved Rusmiddelmisbruk og Psykiske Helseproblemer; Landheim, A.W., Wiig, F.L., Brendbekken, M., Brodahl, M., Biong, S., Eds.; Gyldendal Akademisk: Copenhagen, Denmark, 2016; pp. 168–170. [Google Scholar]
- Lauveng, A. Vi må slutte og behandle samtidig rus og psykisk lidelse—Vi skal behandle mennesker. In Et Bedre liv. Historier, Erfaringer og Forskning om Recovery ved Rusmiddelmisbruk og Psykiske Helseproblemer; Landheim, A.W., Wiig, F.L., Brendbekken, M., Brodahl, M., Biong, S., Eds.; Gyldendal Akademisk: Copenhagen, Denmark, 2016; pp. 171–173. [Google Scholar]
- Schuch, F.B.; Stubbs, B. The Role of Exercise in Preventing and Treating Depression. Curr. Sports Med. Rep. 2019, 18, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Firth, J.; Rosenbaum, S.; Ward, P.; Reichert, T.; Bagatini, N.C.; Bgeginski, R.; Stubbs, B. Physical activity and sedentary behavior in people with major depressive disorder: A systematic review and meta-analysis. J. Affect. Disord. 2017, 210, 139–150. [Google Scholar] [CrossRef] [PubMed]
- Schuch, F.B.; Vancampfort, D.; Richards, J.; Rosenbaum, S.; Ward, P.B.; Stubbs, B. Exercise as a treatment for depression: A meta-analysis adjusting for publication bias. J. Psychiatr. Res. 2016, 77, 42–51. [Google Scholar] [CrossRef]
- Schuch, F.B.; Vancampfort, D.; Rosenbaum, S.; Richards, J.; Ward, P.B.; Stubbs, B. Exercise improves physical and psychological quality of life in people with depression: A meta-analysis including the evaluation of control group response. Psychiatry Res. 2016, 241, 47–54. [Google Scholar] [CrossRef]
- Krogh, J.; Hjorthoj, C.; Speyer, H.; Gluud, C.; Nordentoft, M. Exercise for patients with major depression: A systematic review with meta-analysis and trial sequential analysis. BMJ Open 2017, 7, e014820. [Google Scholar] [CrossRef]
- Kvam, S.; Kleppe, C.L.; Nordhus, I.H.; Hovland, A. Exercise as a treatment for depression: A meta-analysis. J. Affect. Disord. 2016, 202, 67–86. [Google Scholar] [CrossRef]
- Singh, B.; Olds, T.; Curtis, R.; Dumuid, D.; Virgara, R.; Watson, A.; Szeto, K.; O’Connor, E.; Ferguson, T.; Eglitis, E.; et al. Effectiveness of physical activity interventions for improving depression, anxiety and distress: An overview of systematic reviews. Br. J. Sports Med. 2023. [Google Scholar] [CrossRef]
- Henriksson, M.; Wall, A.; Nyberg, J.; Adiels, M.; Lundin, K.; Bergh, Y.; Eggertsen, R.; Danielsson, L.; Kuhn, H.G.; Westerlund, M.; et al. Effects of exercise on symptoms of anxiety in primary care patients: A randomized controlled trial. J. Affect. Disord. 2022, 297, 26–34. [Google Scholar] [CrossRef]
- Stubbs, B.; Vancampfort, D.; Rosenbaum, S.; Ward, P.B.; Richards, J.; Ussher, M.; Schuch, F.B. Challenges Establishing the Efficacy of Exercise as an Antidepressant Treatment: A Systematic Review and Meta-Analysis of Control Group Responses in Exercise Randomised Controlled Trials. Sports Med. 2016, 46, 699–713. [Google Scholar] [CrossRef]
- Bartley, C.A.; Hay, M.; Bloch, M.H. Meta-analysis: Aerobic exercise for the treatment of anxiety disorders. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2013, 45, 34–39. [Google Scholar] [CrossRef]
- Herring, M.P.; O’Connor, P.J.; Dishman, R.K. The effect of exercise training on anxiety symptoms among patients: A systematic review. Arch. Intern. Med. 2010, 170, 321–331. [Google Scholar] [CrossRef] [PubMed]
- Stonerock, G.L.; Hoffman, B.M.; Smith, P.J.; Blumenthal, J.A. Exercise as Treatment for Anxiety: Systematic Review and Analysis. Ann. Behav. Med. 2015, 49, 542–556. [Google Scholar] [CrossRef]
- Hallgren, M.; Vancampfort, D.; Giesen, E.S.; Lundin, A.; Stubbs, B. Exercise as treatment for alcohol use disorders: Systematic review and meta-analysis. Br. J. Sports Med. 2017, 51, 1058–1064. [Google Scholar] [CrossRef] [PubMed]
- Wang, D.; Wang, Y.; Wang, Y.; Li, R.; Zhou, C. Impact of Physical Exercise on Substance Use Disorders: A Meta-Analysis. PLoS ONE 2014, 9, e110728. [Google Scholar] [CrossRef] [PubMed]
- Pearsall, R.; Smith, D.J.; Pelosi, A.; Geddes, J. Exercise therapy in adults with serious mental illness: A systematic review and meta-analysis. BMC Psychiatry 2014, 14, 117. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, S.; Tiedemann, A.; Sherrington, C.; Curtis, J.; Ward, P.B. Physical activity interventions for people with mental illness: A systematic review and meta-analysis. J. Clin. Psychiatry 2014, 75, 964–974. [Google Scholar] [CrossRef] [PubMed]
- Firth, J.; Cotter, J.; Elliott, R.; French, P.; Yung, A.R. A systematic review and meta-analysis of exercise interventions in schizophrenia patients. Psychol. Med. 2015, 45, 1343–1361. [Google Scholar] [CrossRef]
- Firth, J.; Stubbs, B.; Rosenbaum, S.; Vancampfort, D.; Malchow, B.; Schuch, F.; Elliott, R.; Nuechterlein, K.H.; Yung, A.R. Aerobic Exercise Improves Cognitive Functioning in People with Schizophrenia: A Systematic Review and Meta-Analysis. Schizophr. Bull. 2017, 43, 546–556. [Google Scholar] [CrossRef]
- Dauwan, M.; Begemann, M.J.H.; Heringa, S.M.; Sommer, I.E. Exercise Improves Clinical Symptoms, Quality of Life, Global Functioning, and Depression in Schizophrenia: A Systematic Review and Meta-analysis. Schizophr. Bull. 2015, 42, 588–599. [Google Scholar] [CrossRef]
- Vancampfort, D.; Firth, J.; Schuch, F.B.; Rosenbaum, S.; De Hert, M.; Mugisha, J.; Probst, M.; Stubbs, B. Physical activity and sedentary behavior in people with bipolar disorder: A systematic review and meta-analysis. J. Affect. Disord. 2016, 201, 145–152. [Google Scholar] [CrossRef] [PubMed]
- Hodgson, M.H.; McCulloch, H.P.; Fox, K.R. The experiences of people with severe and enduring mental illness engaged in a physical activity programme integrated into the mental health service. Ment. Health Phys. Act. 2011, 4, 23–29. [Google Scholar] [CrossRef]
- Crone, D.; Guy, H. ‘I know it is only exercise, but to me it is something that keeps me going’: A qualitative approach to understanding mental health service users’ experiences of sports therapy. Int. J. Ment. Health Nurs. 2008, 17, 197–207. [Google Scholar] [CrossRef] [PubMed]
- Chapman, J.J.; Fraser, S.J.; Brown, W.J.; Burton, N.W. Physical activity preferences, motivators, barriers and attitudes of adults with mental illness. J. Ment. Health 2016, 25, 448–454. [Google Scholar] [CrossRef]
- Fogarty, M.; Happell, B. Exploring the benefits of an exercise program for people with schizophrenia: A qualitative study. Issues Ment. Health Nurs. 2005, 26, 341–351. [Google Scholar] [CrossRef]
- Danielsen, K.K.; Oydna, M.H.; Strommer, S.; Haugjord, K. “It’s More Than Just Exercise”: Tailored Exercise at a Community-Based Activity Center as a Liminal Space along the Road to Mental Health Recovery and Citizenship. Int. J. Environ. Res. Public Health 2021, 18, 10516. [Google Scholar] [CrossRef]
- Song, J.; Liu, Z.Z.; Huang, J.; Wu, J.S.; Tao, J. Effects of aerobic exercise, traditional Chinese exercises, and meditation on depressive symptoms of college student: A meta-analysis of randomized controlled trials. Medicine 2021, 100, e23819. [Google Scholar] [CrossRef]
- Huang, J.; Nigatu, Y.T.; Smail-Crevier, R.; Zhang, X.; Wang, J. Interventions for common mental health problems among university and college students: A systematic review and meta-analysis of randomized controlled trials. J. Psychiatr. Res. 2018, 107, 1–10. [Google Scholar] [CrossRef]
- Karlsson, B.; Borg, M. Psykisk Helsearbeid. Humane og Sosiale Perspektiver og Praksiser; Gyldendal: Copenhagen, Denmark, 2013. [Google Scholar]
- Cappelen, A.V.; Charness, G.; Ekström, M.; Gneezy, U.; Tungodden, B. Exercise Improves Academic Performance; DP SAM;8/2017; Department of Economics, Norwegian School of Economics: Bergen, Norway, 2017; ISSN 0804-6824. [Google Scholar]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A.; PAFS Consensus Group. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016, 2, 64. [Google Scholar] [CrossRef]
- Schulz, K.F.; Altman, D.G.; Moher, D.; Group, C. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. PLoS Med. 2010, 7, e1000251. [Google Scholar] [CrossRef]
- Hoffmann, T.C.; Glasziou, P.P.; Boutron, I.; Milne, R.; Perera, R.; Moher, D.; Altman, D.G.; Barbour, V.; Macdonald, H.; Johnston, M.; et al. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ 2014, 348, g1687. [Google Scholar] [CrossRef]
- El-Kotob, R.; Giangregorio, L.M. Pilot and feasibility studies in exercise, physical activity, or rehabilitation research. Pilot Feasibility Stud. 2018, 4, 137. [Google Scholar] [CrossRef] [PubMed]
- Billingham, S.A.; Whitehead, A.L.; Julious, S.A. An audit of sample sizes for pilot and feasibility trials being undertaken in the United Kingdom registered in the United Kingdom Clinical Research Network database. BMC Med. Res. Methodol. 2013, 13, 104. [Google Scholar] [CrossRef]
- Sim, J.; Lewis, M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J. Clin. Epidemiol. 2012, 65, 301–308. [Google Scholar] [CrossRef]
- Hertzog, M.A. Considerations in determining sample size for pilot studies. Res. Nurs. Health 2008, 31, 180–191. [Google Scholar] [CrossRef]
- Vindbjerg, E.; Carlsson, J.; Mortensen, E.L.; Makransky, G.; Nielsen, T. A Rasch-based validity study of the Harvard Trauma Questionnaire. J. Affect. Disord. 2020, 277, 697–705. [Google Scholar] [CrossRef]
- Derogatis, L.R.; Lipman, R.S.; Rickels, K.; Uhlenhuth, E.H.; Covi, L. The Hopkins Symptom Checklist (HSCL): A self-report symptom inventory. Behav. Sci. 1974, 19, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.; Friede, T.; Putz, R.; Ashdown, J.; Martin, S.; Blake, A.; Adi, Y.; Parkinson, J.; Flynn, P.; Platt, S.; et al. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): Validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health 2011, 11, 487. [Google Scholar] [CrossRef] [PubMed]
- Taggart, F.; Friede, T.; Weich, S.; Clarke, A.; Johnson, M.; Stewart-Brown, S. Cross cultural evaluation of the Warwick-Edinburgh Mental Well-being Scale (WEMWBS)—A mixed methods study. Health Qual. Life Outcomes 2013, 11, 27. [Google Scholar] [CrossRef]
- Diener, E.; Emmons, R.A.; Larsen, R.J.; Griffin, S. The Satisfaction with Life Scale. J. Pers. Assess. 1985, 49, 71–75. [Google Scholar] [CrossRef]
- Kjell, O.N.E.; Diener, E. Abbreviated Three-Item Versions of the Satisfaction with Life Scale and the Harmony in Life Scale Yield as Strong Psychometric Properties as the Original Scales. J. Pers. Assess. 2021, 103, 183–194. [Google Scholar] [CrossRef] [PubMed]
- Pavot, W.; Diener, E.; Colvin, C.R.; Sandvik, E. Further validation of the Satisfaction with Life Scale: Evidence for the cross-method convergence of well-being measures. J. Pers. Assess. 1991, 57, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Andersen, L.B.; Andersen, T.E.; Andersen, E.; Anderssen, S.A. An intermittent running test to estimate maximal oxygen uptake: The Andersen test. J. Sports Med. Phys. Fit. 2008, 48, 434–437. [Google Scholar]
- Migueles, J.H.; Cadenas-Sanchez, C.; Ekelund, U.; Delisle Nystrom, C.; Mora-Gonzalez, J.; Lof, M.; Labayen, I.; Ruiz, J.R.; Ortega, F.B. Accelerometer Data Collection and Processing Criteria to Assess Physical Activity and Other Outcomes: A Systematic Review and Practical Considerations. Sports Med. 2017, 47, 1821–1845. [Google Scholar] [CrossRef]
- Tomkinson, G.R.; Carver, K.D.; Atkinson, F.; Daniell, N.D.; Lewis, L.K.; Fitzgerald, J.S.; Lang, J.J.; Ortega, F.B. European normative values for physical fitness in children and adolescents aged 9–17 years: Results from 2,779,165 Eurofit performances representing 30 countries. Br. J. Sports Med. 2018, 52, 1445–14563. [Google Scholar] [CrossRef]
- Suni, J.H.; Oja, P.; Miilunpalo, S.I.; Pasanen, M.E.; Vuori, I.M.; Bos, K. Health-related fitness test battery for middle-aged adults: Associations with physical activity patterns. Int. J. Sports Med. 1999, 20, 183–191. [Google Scholar] [CrossRef]
- Castro-Pinero, J.; Artero, E.G.; Espana-Romero, V.; Ortega, F.B.; Sjostrom, M.; Suni, J.; Ruiz, J.R. Criterion-related validity of field-based fitness tests in youth: A systematic review. Br. J. Sports Med. 2010, 44, 934–943. [Google Scholar] [CrossRef]
- Joseph, K.L.; Dagfinrud, H.; Hagen, K.B.; Norden, K.R.; Fongen, C.; Wold, O.M.; Hinman, R.S.; Nelligan, R.K.; Bennell, K.L.; Tveter, A.T. The AktiWeb study: Feasibility of a web-based exercise program delivered by a patient organisation to patients with hip and/or knee osteoarthritis. Pilot Feasibility Stud. 2022, 8, 150. [Google Scholar] [CrossRef]
- Grasaas, E.; Helseth, S.; Fegran, L.; Stinson, J.; Smastuen, M.; Lalloo, C.; Haraldstad, K. App-based intervention among adolescents with persistent pain: A pilot feasibility randomized controlled trial. Pilot Feasibility Stud. 2022, 8, 158. [Google Scholar] [CrossRef]
- Vancampfort, D.; Sanchez, C.P.R.; Hallgren, M.; Schuch, F.; Firth, J.; Rosenbaum, S.; Van Damme, T.; Stubbs, B. Dropout from exercise randomized controlled trials among people with anxiety and stress-related disorders: A meta-analysis and meta-regression. J. Affect. Disord. 2021, 282, 996–1004. [Google Scholar] [CrossRef]
- Lawlor, D.A.; Hopker, S.W. The effectiveness of exercise as an intervention in the management of depression: Systematic review and meta-regression analysis of randomised controlled trials. BMJ 2001, 322, 763–767. [Google Scholar] [CrossRef]
- Rethorst, C.D.; Wipfli, B.M.; Landers, D.M. The antidepressive effects of exercise: A meta-analysis of randomized trials. Sports Med. 2009, 39, 491–511. [Google Scholar] [CrossRef]
- Krogh, J.; Nordentoft, M.; Sterne, J.A.; Lawlor, D.A. The effect of exercise in clinically depressed adults: Systematic review and meta-analysis of randomized controlled trials. J. Clin. Psychiatry 2011, 72, 529–538. [Google Scholar] [CrossRef] [PubMed]
- Helsedirektoratet. Fysisk Aktivitet i Forebygging og Behandling. Voksne og Eldre—Generelle Råd. Available online: https://www.helsedirektoratet.no/faglige-rad/fysisk-aktivitet-i-forebygging-og-behandling/voksne-og-eldre (accessed on 17 August 2023).
- WHO. WHO Guidelines on Physical Activity and Sedentary Behaviour: At a Glance; World Health Organization: Geneva, Switzerland, 2020; ISBN 9789240014886. [Google Scholar]
- Laursen, T.M.; Musliner, K.L.; Benros, M.E.; Vestergaard, M.; Munk-Olsen, T. Mortality and life expectancy in persons with severe unipolar depression. J. Affect. Disord. 2016, 193, 203–207. [Google Scholar] [CrossRef]
- Laursen, T.M.; Wahlbeck, K.; Hallgren, J.; Westman, J.; Osby, U.; Alinaghizadeh, H.; Gissler, M.; Nordentoft, M. Life expectancy and death by diseases of the circulatory system in patients with bipolar disorder or schizophrenia in the Nordic countries. PLoS ONE 2013, 8, e67133. [Google Scholar] [CrossRef]
- Nordentoft, M.; Wahlbeck, K.; Hallgren, J.; Westman, J.; Osby, U.; Alinaghizadeh, H.; Gissler, M.; Laursen, T.M. Excess mortality, causes of death and life expectancy in 270,770 patients with recent onset of mental disorders in Denmark, Finland and Sweden. PLoS ONE 2013, 8, e55176. [Google Scholar] [CrossRef]
- Wahlbeck, K.; Westman, J.; Nordentoft, M.; Gissler, M.; Laursen, T.M. Outcomes of Nordic mental health systems: Life expectancy of patients with mental disorders. Br. J. Psychiatry J. Ment. Sci. 2011, 199, 453–458. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; Cohen, D.; Bobes, J.; Cetkovich-Bakmas, M.; Leucht, S.; Ndetei, D.M.; Newcomer, J.W.; Uwakwe, R.; Asai, I.; Moller, H.J.; et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 2011, 10, 138–151. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.; Happell, B. The high prevalence of poor physical health and unhealthy lifestyle behaviours in individuals with severe mental illness. Issues Ment. Health Nurs. 2011, 32, 589–597. [Google Scholar] [CrossRef]
- Warburton, D.E.R.; Bredin, S.S.D. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef] [PubMed]
- Farholm, A. Motivation and Physical Activity in Individuals with Severe Mental Illness. Ph.D. Thesis, Norges Idrettshøgskole, Oslo, Norway, 2017. [Google Scholar]
- Lundstrom, S.; Jormfeldt, H.; Hedman Ahlstrom, B.; Skarsater, I. Health-related lifestyle and perceived health among people with severe mental illness: Gender differences and degree of sense of coherence. Arch. Psychiatr. Nurs. 2019, 33, 182–188. [Google Scholar] [CrossRef]
- Vancampfort, D.; Firth, J.; Schuch, F.B.; Rosenbaum, S.; Mugisha, J.; Hallgren, M.; Probst, M.; Ward, P.B.; Gaughran, F.; De Hert, M.; et al. Sedentary behavior and physical activity levels in people with schizophrenia, bipolar disorder and major depressive disorder: A global systematic review and meta-analysis. World Psychiatry 2017, 16, 308–315. [Google Scholar] [CrossRef]
- Solmi, M.; Radua, J.; Olivola, M.; Croce, E.; Soardo, L.; Salazar de Pablo, G.; Il Shin, J.; Kirkbride, J.B.; Jones, P.; Kim, J.H.; et al. Age at onset of mental disorders worldwide: Large-scale meta-analysis of 192 epidemiological studies. Mol. Psychiatry 2022, 27, 281–295. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Amminger, G.P.; Aguilar-Gaxiola, S.; Alonso, J.; Lee, S.; Ustun, T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 2007, 20, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Kessler, R.C.; Angermeyer, M.; Anthony, J.C.; De Graaf, R.O.N.; Demyttenaere, K.; Gasquet, I.; De Girolamo, G.; Gluzman, S.; Gureje, O.Y.E.; Haro, J.M.; et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the World Health Organization’s World Mental Health Survey Initiative. World Psychiatry 2007, 6, 168–176. [Google Scholar] [PubMed]
| Demographics | |
| Age, years, mean (SD) | 24.5 (5.1) |
| Female, n (%) | 9 (69.2%) |
| Mental health | |
| Symptoms of depression and anxiety | |
| Hscl_25, mean (SD) | 2.5 (0.5) |
| Hscl_25 (<1.75), n (%) | 12 (92.3%) |
| Well-being | |
| WEMWBS, mean (SD) | 37.2 (9.4) |
| WEMWEB (≤14), n (%) | 0 (0%) |
| Satisfaction with life | |
| SWLS, mean (SD) | 13.3 (4.8) |
| SWLS (>31), n (%) | 0 (0%) |
| Pre-Test (n = 10) | Post-Test (n = 10) | Mean Change (95% CI) | p-Value | |
|---|---|---|---|---|
| Symptoms of depression and anxiety (Hscl_25) | 2.5 (0.5) | 1.9 (0.4) | 0.5 (0.2, 0.8) | 0.008 1 |
| Well-being (WEMWEB) | 38.0 (10.7) | 44.2 (12.3) | 6.2 (−12.8, 0.3) | 0.58 1 |
| Satisfaction with life (SWLS) | 13.9 (5.3) | 16.8 (6.9) | 2.9 (−7.0, 1.2) | 0.15 1 |
| Pre-Test (n = 10) | Post-Test (n = 10) | Mean Change (95% CI) | p-Value | |
|---|---|---|---|---|
| Cardiorespiratory fitness: | ||||
| 20 m shuttle run test (meters) | 698 (94.5) | 840 (94.3) | 142 (95.1, 189.0) | <0.001 1 |
| Estimated VO2maks (mL/kg/min) | 37.3 (4.7) | 42.0 (4.5) | 4.7 (3.1, 6.2) | <0.001 1 |
| Muscular endurance/strength: | ||||
| Modified push-ups (max reps) | 11.0 (2.4) | 16.1 (3) | 5.1 (3.2, 7.0) | 0.01 1 |
| Sit-ups (max reps) | 10.2 (5.9) | 13.4 (4.4) | 3.2 (0.7, 5.7) | 0.02 1 |
| Grip strength (kg) | 38.1 (11.2) | 38.1 (13.6) | 0.0 (−3.3, 3.3) | 1.00 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Danielsen, K.K.; Cabral, D.; Sveaas, S.H. “Students Moving Together”, Tailored Exercise for Students Facing Mental Health Challenges—A Pilot Feasibility Study. Int. J. Environ. Res. Public Health 2023, 20, 6639. https://doi.org/10.3390/ijerph20176639
Danielsen KK, Cabral D, Sveaas SH. “Students Moving Together”, Tailored Exercise for Students Facing Mental Health Challenges—A Pilot Feasibility Study. International Journal of Environmental Research and Public Health. 2023; 20(17):6639. https://doi.org/10.3390/ijerph20176639
Chicago/Turabian StyleDanielsen, Kjersti Karoline, Danielle Cabral, and Silje Halvorsen Sveaas. 2023. "“Students Moving Together”, Tailored Exercise for Students Facing Mental Health Challenges—A Pilot Feasibility Study" International Journal of Environmental Research and Public Health 20, no. 17: 6639. https://doi.org/10.3390/ijerph20176639
APA StyleDanielsen, K. K., Cabral, D., & Sveaas, S. H. (2023). “Students Moving Together”, Tailored Exercise for Students Facing Mental Health Challenges—A Pilot Feasibility Study. International Journal of Environmental Research and Public Health, 20(17), 6639. https://doi.org/10.3390/ijerph20176639






