The Burden of Pediatric Visual Impairment and Ocular Diagnoses in Barbados
Abstract
1. Introduction
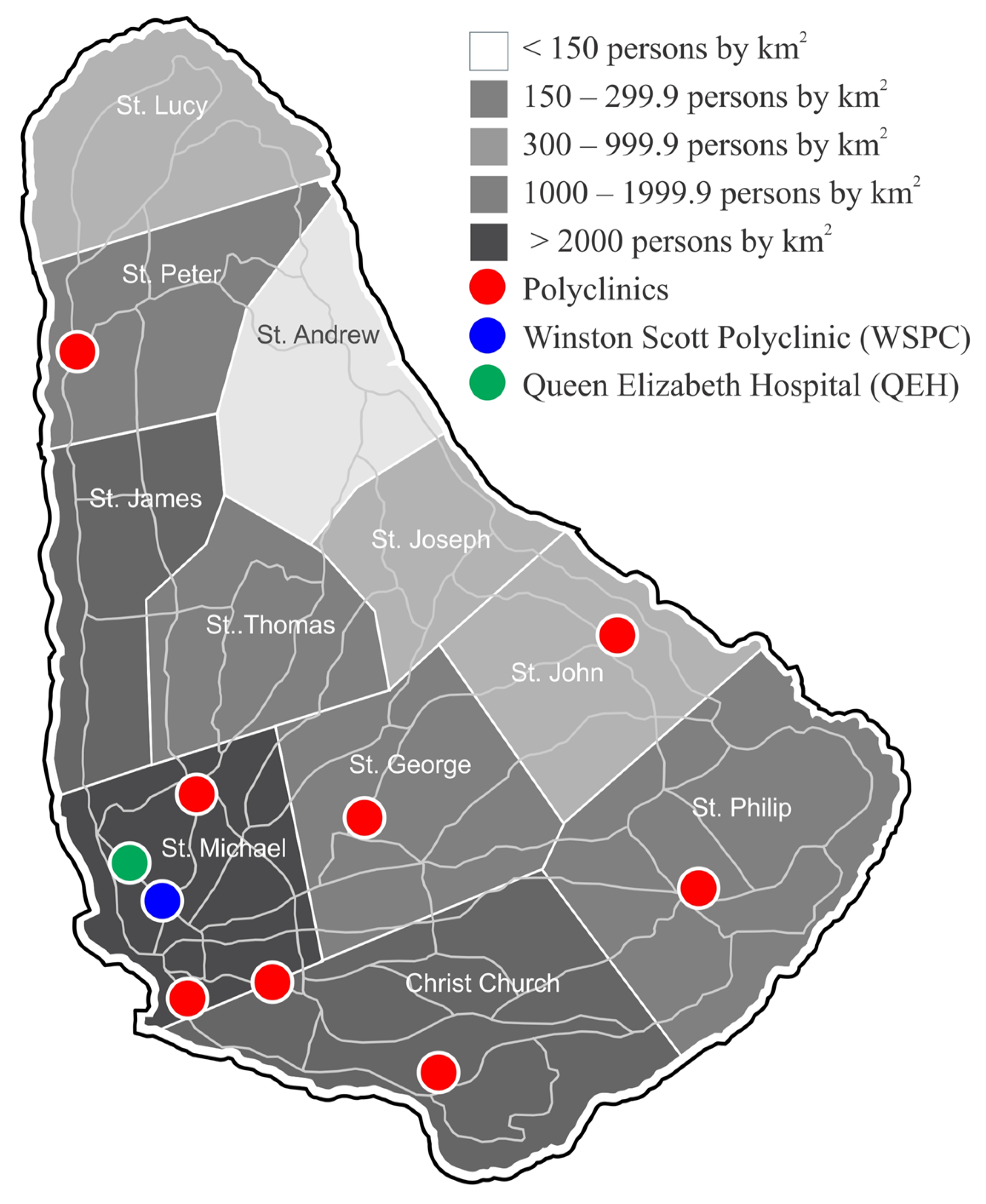
2. Materials and Methods
3. Results
Visual Impairment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rahi, J.S.; Cable, N.; British Childhood Visual Impairment Study Group. Severe visual impairment and blindness in children in the UK. Lancet 2003, 362, 1359–1365. [Google Scholar] [CrossRef]
- USAID’s Child Blindness Program. Available online: https://www.usaid.gov/childblindness (accessed on 8 February 2022).
- World Health Organization. Blindness and Deafness Unit & International Agency for the Prevention of Blindness. In Proceedings of the Preventing Blindness in Children: Report of a WHO/IAPB Scientific Meeting, Hyderabad, India, 13–17 April 1999; Licence: CC BY-NC-SA 3.0 IGO. Available online: https://apps.who.int/iris/handle/10665/66663 (accessed on 8 February 2022).
- Institute for Health Metrics and Evaluation. Health Data.org. Available online: https://vizhub.healthdata.org/gbd-compare/ (accessed on 9 February 2022).
- Heijthuijsen, A.A.M.; Beunders, V.A.A.; Jiawan, D.; de Mesquita-Voigt, A.-M.B.; Pawiroredjo, J.; Mourits, M.; Tanck, M.; Verhoeff, J.; Saeed, P. Causes of severe visual impairment and blindness in children in the Republic of Suriname. Br. J. Ophthalmol. 2013, 97, 812–815. [Google Scholar] [CrossRef]
- Moriarty, B.J. Childhood blindness in Jamaica. Br. J. Ophthalmol. 1988, 72, 65–67. [Google Scholar] [CrossRef]
- Saunders, A. Health Ministry to Ramp Up Coverage for MMR. Jamaica Information Service. 2012. Available online: https://jis.gov.jm/health-ministry-to-ramp-up-coverage-for-mmr/ (accessed on 21 November 2019).
- Das Gupta, M.; Engelman, R.; Levy, J.; Luchsinger, G.; Merrick, T.; Rosen, J. The Power of 1.8 Billion Adolescents, Youth and the Transformation of the Future. United Nations Population Fund. 2014. Available online: https://www.unfpa.org/sites/default/files/pub-pdf/EN-SWOP14-Report_FINAL-web.pdf (accessed on 6 August 2023).
- Data Warehouse. Unicef Data. 29 March 2021. Available online: https://data.unicef.org/resources/data_explorer/unicef_f/?ag=UNICEF&df=GLOBAL_DATAFLOW&ver=1.0&dq=JAM.CME_MRY0T4.&startPeriod=1970&endPeriod=2022 (accessed on 16 February 2022).
- Barbados Population 2022 (Live). Barbados Population 2022 (Demographics, Maps, Graphs). (n.d.). Available online: https://worldpopulationreview.com/countries/barbados-population (accessed on 8 February 2022).
- Barbados. The World Bank. (n.d.). Available online: https://data.worldbank.org/country/barbados (accessed on 18 May 2022).
- Barbados—Market Overview. International Trade Administration. 25 September 2021. Available online: https://www.trade.gov/country-commercial-guides/barbados-market-overview (accessed on 26 May 2022).
- World Health Organization. Vision Impairment and Blindness; World Health Organization: Geneva, Switzerland, 2021; Licence: CC BY-NC-SA 3.0 IGO; Available online: https://www.who.int/news-room/fact-sheets/detail/blindness-and-visual-impairment (accessed on 6 June 2022).
- Leske, M.C.; Connell, A.M.; Schachat, A.P.; Hyman, L. The Barbados Eye Study. Prevalence of open angle glaucoma. Arch. Ophthalmol. 1994, 112, 821–829. [Google Scholar] [CrossRef]
- Friedburg, D.; Klöppel, K. Early correction of hyperopia and astigmatism in children leads to better development of visual acuity. Klin. Monatsblatter Augenheilkd. 1996, 209, 21–24. (In German) [Google Scholar] [CrossRef]
- Ma, X.; Zhou, Z.; Yi, H.; Pang, X.; Shi, Y.; Chen, Q.; Meltzer, M.E.; le Cessie, S.; He, M.; Rozelle, S.; et al. Effect of providing free glasses on children’s educational outcomes in China: Cluster randomized controlled trial. BMJ 2014, 349, g5740. [Google Scholar] [CrossRef] [PubMed]
- Miyazaki, D.; Fukagawa, K.; Okamoto, S.; Fukushima, A.; Uchio, E.; Ebihara, N.; Shoji, J.; Namba, K.; Shimizu, Y. Epidemiological aspects of allergic conjunctivitis. Allergol. Int. 2020, 69, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Palmares, J.; Delgado, L.; Cidade, M.; Quadrado, M.J.; Filipe, H.P.; Season Study Group. Allergic conjunctivitis: A national cross-sectional study of clinical characteristics and quality of life. Eur. J. Ophthalmol. 2010, 20, 257–264. [Google Scholar] [CrossRef] [PubMed]
- Hashemi, H.; Khabazkhoob, M.; Yazdani, N.; Ostadimoghaddam, H.; Norouzirad, R.; Amanzadeh, K.; Miraftab, M.; Derakhshan, A.; Yekta, A. The prevalence of keratoconus in a young population in Mashhad, Iran. Ophthalmic Physiol. Opt. 2014, 34, 519–527. [Google Scholar] [CrossRef] [PubMed]
- Agaje, B.G.; Delelegne, D.; Abera, E.; Desta, K.; Girum, M.; Mossie, M.; Eshetu, D.; Hirigo, A.T. Strabismus prevalence and associated factors among pediatric patients in southern Ethiopia: A cross-sectional study. J. Int. Med. Res. 2020, 48, 2. [Google Scholar] [CrossRef] [PubMed]
- Borchert, M.S.; Varma, R.; Cotter, S.A.; Tarczy-Hornoch, K.; McKean-Cowdin, R.; Lin, J.; Multi-Ethnic Pediatric Eye Disease Study and the Baltimore Pediatric Eye Disease Study Groups. Risk factors for hyperopia and myopia in preschool children the multi-ethnic pediatric eye disease and Baltimore pediatric eye disease studies. Ophthalmology 2011, 118, 1966–1973. [Google Scholar] [CrossRef] [PubMed]
- O’Neill, A. Barbados—Infant Mortality Rate 2009–2019. Statista. 5 January 2022. Available online: https://www.statista.com/statistics/806666/infant-mortality-in-barbados/ (accessed on 18 May 2022).
- Rondaris, M.V.A. The Public Health Approach for Retinopathy of Prematurity. Philipp. J. Ophthalmol. 2013, 38, 61–63. [Google Scholar]
- O’Neill, A. Suriname—Infant Mortality Rate 2009–2019. Statista. 2 February 2022. Available online: https://www.statista.com/statistics/807790/infant-mortality-in-suriname/ (accessed on 6 June 2022).
- Service Specification. GOV.UK. (n.d.). Available online: https://www.gov.uk/government/publications/child-vision-screening/service-specification (accessed on 7 October 2022).
- Grossman, D.C.; Curry, S.J.; Owens, D.K.; Barry, M.J.; Davidson, K.W.; Doubeni, C.A.; Epling, J.W.; Kemper, A.R.; Krist, A.H.; Kurth, A.E.; et al. Vision Screening in Children Aged 6 Months to 5 years: US Preventive Services Task Force Recommendation Statement. JAMA 2017, 318, 836–844. [Google Scholar] [PubMed]
- Vision Screening Recommendations (2014, May). AAPOS Member Resources. Available online: https://aapos.org/members/vision-screening-guidelines (accessed on 6 August 2023).
- Leon, A.; Donahue, S.P.; Morrison, D.G.; Estes, R.L.; Li, C. The age-dependent effect of anisometropia magnitude on anisometropic amblyopia severity. J. AAPOS 2008, 12, 150–1560. [Google Scholar] [CrossRef] [PubMed]
- Longmuir, S.Q.; Pfeifer, W.; Leon, A.; Olson, R.J.; Short, L.; Scott, W.E. Nine-year Results of a Volunteer Lay Network Photoscreening Program of 147 809 Children Using a PhotoScreener in Iowa. Ophthalmology 2010, 117, 1869–1875. [Google Scholar] [CrossRef] [PubMed]
- Committee on Practice and Ambulatory Medicine; Section on Ophthalmology; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Eye examination in infants, children, and young adults by pediatricians. Pediatrics 2003, 111, 902–907. [Google Scholar] [CrossRef]
- Donahue, S.P.; Baker, C.N.; Simon, G.R. Procedures for the Evaluation of the Visual System by Pediatricians; American Academy of Pediatrics: Washington, DC, USA, 2016; Available online: https://publications.aap.org/pediatrics/article/137/1/e20153597/52806/Procedures-for-the-Evaluation-of-the-Visual-System?autologincheck=redirected (accessed on 16 January 2023).
- Guidelines for School-Based Eye Health Programmes. (n.d). Available online: https://www.globalpartnership.org/sites/default/files/2017-09-ship-guidelines-vision-screening.pdf (accessed on 5 August 2023).
- School Eye Health Guidelines. The International Agency for the Prevention of Blindness. 28 February 2022. Available online: https://www.iapb.org/learn/resources/school-eye-health-guidelines/ (accessed on 5 August 2023).
- Thorisdottir, R.L.; Faxén, T.; Blohmé, J.; Sheikh, R.; Malmsjö, M. The impact of vision screening in preschool children on visual function in the Swedish adult population. Acta Ophthalmol. 2019, 97, 793–797. [Google Scholar] [CrossRef]
- Kaur, K.; Kannusamy, V.; Mouttapa, F.; Gurnani, B.; Venkatesh, R.; Khadia, A. To assess the accuracy of Plusoptix S12-C photoscreener in detecting amblyogenic risk factors in children aged 6 months to 6 years in remote areas of South India. Indian J. Ophthalmol. 2020, 68, 2186–2189. [Google Scholar] [PubMed]
- Schmidt, P.; Maguire, M.; Dobson, V.; Quinn, G.; Ciner, E.; Cyert, L.; Kulp, M.T.; Moore, B.; Orel-Bixler, D.; Redford, M.; et al. Comparison of preschool vision screening tests as administered by licensed eye care professionals in the vision in preschoolers study. Ophthalmology 2004, 111, 637–650. [Google Scholar] [PubMed]
- Ademola-Popoola, D.S.; Olatunji, V.A.; Obajolowo, T.S.; Akande, T.M.; Mokuolu, O.A. Outcome of vision screening by community health workers at immunization outlets in Nigeria to support access to early visual evaluation in children aged 0–2 years. Taiwan J. Ophthalmol. 2021, 11, 77–85. [Google Scholar] [CrossRef] [PubMed]
| World Health Organization Category of Visual Impairment | Best Corrected Visual Acuity in the Better Eye |
|---|---|
| Normal Vision | Better than 6/12 |
| Mild visual impairment | 6/12–6/18 |
| Moderate visual impairment | <6/18–6/60 |
| Severe visual impairment | <6/60–3/60 |
| Blindness | Worse than 3/60 |
| Origin of First Referral to Eye Clinic | Number of Children (n) | Percentage (%) |
|---|---|---|
| Schools Eye Service | 1467 | 44.8 |
| Interdepartmental (QEH) referral | 292 | 8.9 |
| Polyclinic referral | 201 | 6.1 |
| Private pediatrician | 98 | 2.9 |
| Self-referral | 48 | 1.5 |
| Private ophthalmologist | 36 | 1.1 |
| Accident and Emergency Department (QEH) | 19 | 0.6 |
| Unknown/undocumented | 1117 | 34.1 |
| Total | 3278 | 100.0 |
| WHO Category for Visual Impairment | Number of Children (n) | Percentage (%) |
|---|---|---|
| Mild | 62 | 77.5 |
| Moderate | 16 | 20.0 |
| Severe | 0 | 0 |
| Blindness | 2 | 2.5 |
| Total | 80 | 100.0 |
| Age Group | ||
| Preschool (0–<5) | 31 | 38.75 |
| School age (5–<12) | 42 | 52.50 |
| Older children (12–18) | 7 | 8.75 |
| Total | 80 | 100.00 |
| Disease Entity/Diagnosis | Number of Children (n) |
|---|---|
| Refractive Error * | 70 |
| Strabismus * | 22 |
| Allergic Eye Disease * | 16 |
| Amblyopia | 50 |
| Corneal Disease *: | |
| ● Keratoconus | 2 |
| ● Dry eye disease | 1 |
| ● Corneal abrasion | 1 |
| Glaucoma *: | |
| ● Primary open angle glaucoma | 3 |
| ● Juvenile open angle glaucoma | 1 |
| Cataract *: | |
| ● Congenital cataract | 2 |
| Uveitis *: | |
| ● Traumatic iritis | 1 |
| Retinal Diseases: | |
| ● Retinitis pigmentosa | 1 |
| Other: | |
| ● Nystagmus | 3 |
| ● Bilateral aphakia * | 1 |
| ● Ectopia lentis * | 1 |
| ● Unknown | 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Da Silva, K.; Dowell, M.; Savatovsky, E.J.; Grosvenor, D.; Callender, D.; Campbell, M.H.; Hambleton, I.; Vanner, E.A.; Grajewski, A.L.; Chang, T.C. The Burden of Pediatric Visual Impairment and Ocular Diagnoses in Barbados. Int. J. Environ. Res. Public Health 2023, 20, 6554. https://doi.org/10.3390/ijerph20166554
Da Silva K, Dowell M, Savatovsky EJ, Grosvenor D, Callender D, Campbell MH, Hambleton I, Vanner EA, Grajewski AL, Chang TC. The Burden of Pediatric Visual Impairment and Ocular Diagnoses in Barbados. International Journal of Environmental Research and Public Health. 2023; 20(16):6554. https://doi.org/10.3390/ijerph20166554
Chicago/Turabian StyleDa Silva, Kirsten, Michelle Dowell, Eleonore J. Savatovsky, Dawn Grosvenor, David Callender, Michael H. Campbell, Ian Hambleton, Elizabeth A. Vanner, Alana L. Grajewski, and Ta Chen Chang. 2023. "The Burden of Pediatric Visual Impairment and Ocular Diagnoses in Barbados" International Journal of Environmental Research and Public Health 20, no. 16: 6554. https://doi.org/10.3390/ijerph20166554
APA StyleDa Silva, K., Dowell, M., Savatovsky, E. J., Grosvenor, D., Callender, D., Campbell, M. H., Hambleton, I., Vanner, E. A., Grajewski, A. L., & Chang, T. C. (2023). The Burden of Pediatric Visual Impairment and Ocular Diagnoses in Barbados. International Journal of Environmental Research and Public Health, 20(16), 6554. https://doi.org/10.3390/ijerph20166554






