Examining the Role of Quality of Institutionalized Healthcare on Maternal Mortality in the Dominican Republic
Abstract
1. Introduction
1.1. Quality of Care
1.2. Obstetric Violence
1.3. Potential Sociodemographic Factors Associated with MMR
1.4. Current Research
2. Methods
2.1. Variables
2.2. Pearson Correlation
2.3. Conway-Maxwell-Poisson Regression
2.4. Patient and Public Involvement
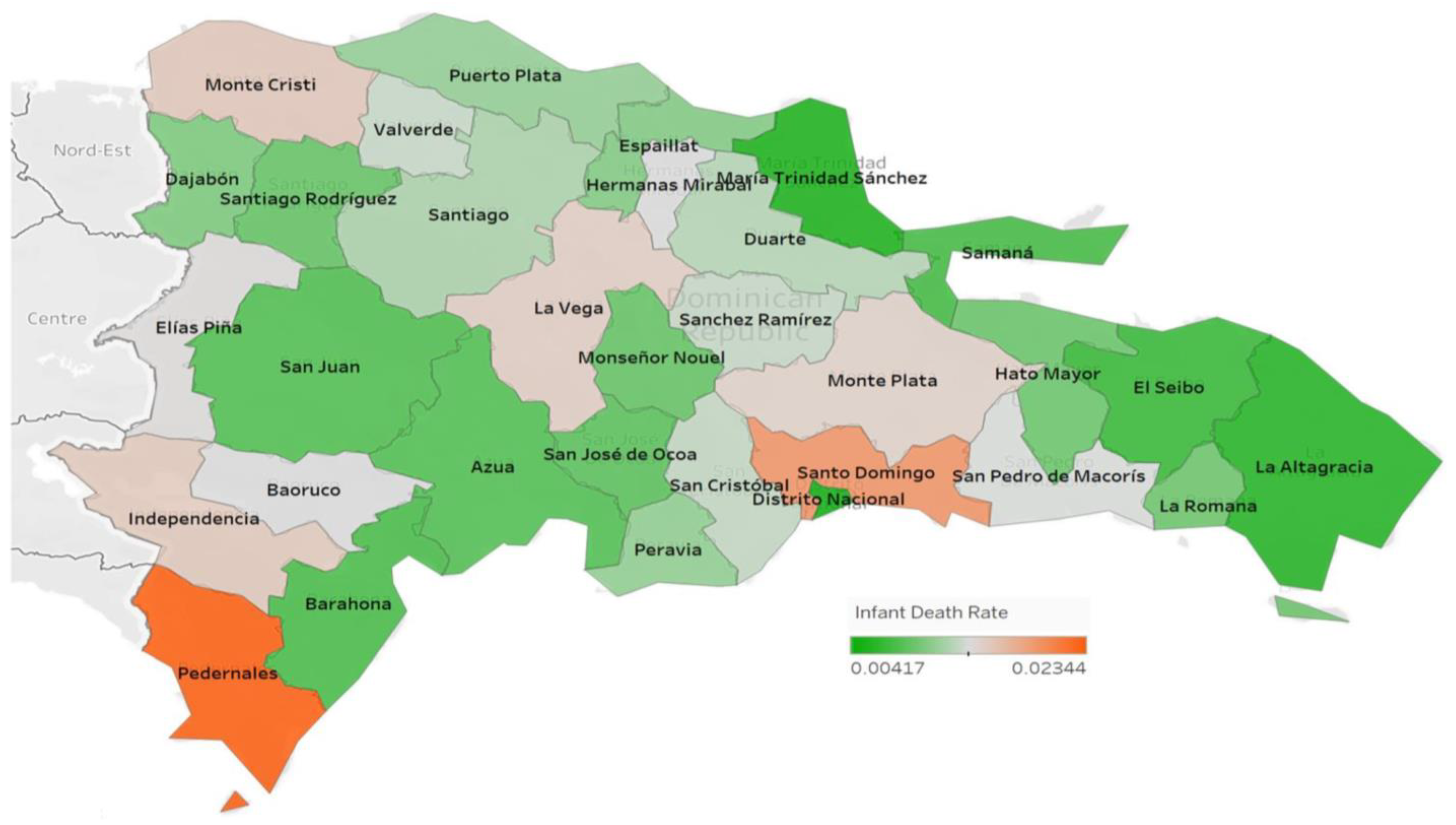
3. Results
3.1. Pearson Correlation
3.2. COM-Poisson Regression
4. Discussion
Implications for Interventions to Improve Maternal Mortality Incomes
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- UNICEF Data. Maternal Mortality Rates and Statistics. Available online: https://data.unicef.org/topic/maternal-health/maternal-mortality/ (accessed on 28 March 2022).
- World Health Organization. Ending Preventable Maternal Mortality Online Consultation for Coverage Targets for Ending Preventable Maternal Mortality. 2020. Available online: https://www.who.int/news/item/03-09-2020-ending-preventable-maternal-mortality-online-consultation-for-coverage-targets-for-ending-preventable-maternal-mortality (accessed on 5 January 2022).
- Sellers, K.F.; Raim, A. A flexible zero-inflated model to address data dispersion. Comput. Stat. Data Anal. 2016, 99, 68–80. [Google Scholar] [CrossRef]
- World Health Organization. Maternal Mortality. Available online: https://www.who.int/news-room/fact-sheets/detail/maternal-mortality (accessed on 5 January 2022).
- Gonzaga-Soriano, M.R.; Zonana-Nacach, A.; Anzaldo-Campos, M.C.; Olazarán-Gutiérrez, A. Prenatal care and hospital maternal mortality in Tijuana, Baja California, Mexico. Salud Publica Mex. 2014, 56, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Schindler, P.; Burgos, R.; Vuong, K.; Lerner, H.A.; Evangelista, E.; Rodriguez, F.J.; Peralta Polanco, L.; Foster, J. The Process of Intrapartum Care among Skilled Birth Attendants in the Dominican Republic and Maternal Perceptions of Care during Labor and Birth: A Case Report. J. Midwifery Women’s Health 2017, 62, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Savage, V.; Castro, A. Measuring mistreatment of women during childbirth: A review of terminology and methodological approaches. Reprod. Health 2017, 14, 138. [Google Scholar] [CrossRef]
- Miller, S.; Cordero, M.; Coleman, A.L.; Figueroa, J.; Brito-Anderson, S.; Dabagh, R.; Calderon, V.; Cáceres, F.; Fernandez, A.J.; Nunez, M. Quality of care in institutionalized deliveries: The paradox of the Dominican Republic. Int. J. Gynaecol. Obstet. 2003, 82, 89–103, discussion 107–108. [Google Scholar] [CrossRef]
- Castro, A.; Savage, V. Obstetric Violence as Reproductive Governance in the Dominican Republic. Med. Anthropol. 2019, 38, 123–136. [Google Scholar] [CrossRef]
- Bonnell, S.; Griggs, A.; Avila, G.; Mack, J.; Bush, R.A.; Vignato, J.; Connelly, C.D. Community Health Workers and Use of mHealth: Improving Identification of Pregnancy Complications and Access to Care in the Dominican Republic. Health Promot. Pract. 2018, 19, 331–340. [Google Scholar] [CrossRef]
- Tunçalp, O.; Stanton, C.; Castro, A.; Adanu, R.; Heymann, M.; Adu-Bonsaffoh, K.; Lattof, S.R.; Blanc, A.; Langer, A. Measuring coverage in MNCH: Validating women’s self-report of emergency cesarean sections in Ghana and the Dominican Republic. PLoS ONE 2013, 8, e60761. [Google Scholar] [CrossRef]
- Betrán, A.P.; Vindevoghel, N.; Souza, J.P.; Gülmezoglu, A.M.; Torloni, M.R. A systematic review of the Robson classification for caesarean section: What works, doesn’t work and how to improve it. PLoS ONE 2014, 9, e97769. [Google Scholar] [CrossRef]
- Austad, K.; Juarez, M.; Shryer, H.; Moratoya, C.; Rohloff, P. Obstetric care navigation: Results of a quality improvement project to provide accompaniment to women for facility-based maternity care in rural Guatemala. BMJ Qual. Saf. 2020, 29, 169–178. [Google Scholar] [CrossRef]
- Binfa, L.; Pantoja, L.; Ortiz, J.; Gurovich, M.; Cavada, G.; Foster, J. Assessment of the implementation of the model of integrated and humanised midwifery health services in Chile. Midwifery 2016, 35, 53–61. [Google Scholar] [CrossRef] [PubMed]
- Bohren, M.A.; Vogel, J.P.; Hunter, E.C.; Lutsiv, O.; Makh, S.K.; Souza, J.P.; Aguiar, C.; Saraiva Coneglian, F.; Diniz, A.L.; Tunçalp, Ö.; et al. The Mistreatment of Women during Childbirth in Health Facilities Globally: A Mixed-Methods Systematic Review. PLoS Med. 2015, 12, e1001847. [Google Scholar] [CrossRef] [PubMed]
- Sen, G.; Reddy, B.; Iyer, A. Beyond measurement: The drivers of disrespect and abuse in obstetric care. Reprod. Health Matters 2018, 26, 6–18. [Google Scholar] [CrossRef]
- Freedman, L.P.; Ramsey, K.; Abuya, T.; Bellows, B.; Ndwiga, C.; Warren, C.E.; Kujawski, S.; Moyo, W.; Kruk, M.E.; Mbaruku, G. Defining disrespect and abuse of women in childbirth: A research, policy and rights agenda. Bull. World Health Organ. 2014, 92, 915–917. [Google Scholar] [CrossRef] [PubMed]
- Castro, A.; Savage, V.; Kaufman, H. Assessing equitable care for Indigenous and Afrodescendant women in Latin America. Rev. Panam. Salud Publica 2015, 38, 96–109. [Google Scholar]
- Van Lerberghe, W.; Matthews, Z.; Achadi, E.; Ancona, C.; Campbell, J.; Channon, A.; de Bernis, L.; De Brouwere, V.; Fauveau, V.; Fogstad, H.; et al. Country experience with strengthening of health systems and deployment of midwives in countries with high maternal mortality. Lancet 2014, 384, 1215–1225. [Google Scholar] [CrossRef]
- Zacher Dixon, L. Obstetrics in a Time of Violence: Mexican Midwives Critique Routine Hospital Practices. Med. Anthropol. Q. 2015, 29, 437–454. [Google Scholar] [CrossRef]
- Babington. Perceived Social Support, Self Esteem, and Pregnancy Status among Dominican Adolescents. 2015. Available online: https://wrlc-amu.primo.exlibrisgroup.com/permalink/01WRLC_AMU/4u6ipk/cdi_proquest_miscellaneous_1675872422 (accessed on 8 July 2021).
- Human Rights Watch. Dominican Republic: Policies Fuel Teen Pregnancy. 2019. Available online: https://www.hrw.org/news/2019/06/18/dominican-republic-policies-fuel-teen-pregnancy (accessed on 12 May 2022).
- Mayor, S. Pregnancy and childbirth are leading causes of death in teenage girls in developing countries. BMJ 2004, 328, 1152. [Google Scholar] [CrossRef]
- Stack, R.J.; Meredith, A. The Impact of Financial Hardship on Single Parents: An Exploration of the Journey from Social Distress to Seeking Help. J. Fam. Econ. Issues 2018, 39, 233–242. [Google Scholar] [CrossRef]
- Wehby, G.L.; Gimenez, L.G.; López-Camelo, J.S. The impact of unemployment cycles on child and maternal health in Argentina. Int. J. Public Health 2017, 62, 197–207. [Google Scholar] [CrossRef]
- Moucheraud, C.; Worku, A.; Molla, M.; Finlay, J.E.; Leaning, J.; Yamin, A. Consequences of maternal mortality on infant and child survival: A 25-year longitudinal analysis in Butajira Ethiopia (1987–2011). Reprod. Health 2015, 12 (Suppl. 1), S4. [Google Scholar] [CrossRef] [PubMed]
- Oficina Nacional de Estadística, República Dominicana: Defunciones Infantiles Notificadas por Año, Según Región y Provincia de Residencia, 2005–2020. Available online: https://web.one.gob.do/busqueda?s=infantiles (accessed on 5 July 2021).
- Oficina Nacional de Estadística, República Dominicana: Compendio de Estadísticas Vitales 2015–2019. 2021. Available online: https://web.one.gob.do/publicaciones/2020/compendio-de-estadisticas-vitales-2015-2019/?altTemplate=publicacionOnline (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana: Población Desocupada por Sexo y Año, Según Regiones de Planificación, 2013–2019. Available online: https://web.one.gob.do/datos-y-estadisticas/temas/estadisticas-sociales/trabajo/ (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana. Población Económicamente Activa (PEA) por Sexo y Año, Según Regiones de Planificación, 2013–2019. Available online: https://www.one.gob.do/busqueda?s=Poblaci%C3%B3n+Econ%C3%B3micamente+Activa+%28PEA (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana. Número-de-Camas-del-Sector-Público-Según-Provincia-2012–2020. Available online: https://www.one.gob.do/busqueda?s=N%C3%BAmero-de-Camas-del-Sector-P%C3%BAblico-Seg%C3%BAn-Provincia (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana. Estimaciones y Proyecciones de la Población Total por año Calendario, Según Región y Provincia, 2000–2030. Available online: https://web.archive.org/web/20170102090940/http://one.gob.do/Estadisticas/8/proyecciones-de-poblacion (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana. Anuario de Estadísticas Sociodemográficas 2012. 2013. Available online: https://web.one.gob.do/media/dpnlohhv/anuariodeestad%C3%ADsticassociodemogr%C3%A1ficas2012dic2013.pdf (accessed on 12 July 2021).
- Oficina Nacional de Estadística, República Dominicana. República Dominicana: Defunciones Maternas Notificadas por año, Según Región y Provincia de Residencia, 2005–2020. Available online: https://web.one.gob.do/datos-y-estadisticas/temas/estadisticas-sociales/salud/ (accessed on 12 July 2021).
- Sellers, K.; Lotze, T.; Raim, A. COMPoissonReg: Conway-Maxwell-Poisson Regression, Version 7.0.0. 2019. Available online: http://cran.r-project.org/web/packages/COMPoissonReg/index.html (accessed on 10 January 2021).
- Vázquez-Vázquez, A.; Fewtrell, M.S.; Chan-García, H.; Batún-Marrufo, C.; Dickinson, F.; Wells, J.C. Does maternal grandmother’s support improve maternal and child nutritional health outcomes? Evidence from Merida, Yucatan, Mexico. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2021, 376, 20200035. [Google Scholar] [CrossRef] [PubMed]
- Merriel, A.; Murove, B.T.; Merriel, S.W.; Sibanda, T.; Moyo, S.; Crofts, J. Implementation of a modified obstetric early warning system to improve the quality of obstetric care in Zimbabwe. Int. J. Gynaecol. Obstet. 2017, 136, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Shields, L.E.; Wiesner, S.; Klein, C.; Pelletreau, B.; Hedriana, H.L. Use of Maternal Early Warning Trigger tool reduces maternal morbidity. Am. J. Obstet. Gynecol. 2016, 214, 527.e1–527.e6. [Google Scholar] [CrossRef]
- Lewis, G. Saving Mothers’ Lives: The continuing benefits for maternal health from the United Kingdom (UK) Confidential Enquires into Maternal Deaths. Semin. Perinatol. 2012, 36, 19–26. [Google Scholar] [CrossRef]
- Ortiz, E.I.; Herrera, E.; De La Torre, A. Extreme Maternal Morbidity: A tracer event to improve the quality of obstetric care in Latin America. Colomb. Med. 2019, 50, 286–292. [Google Scholar] [CrossRef]
- Kelly, M.E.; Duff, H.; Kelly, S.; McHugh Power, J.E.; Brennan, S.; Lawlor, B.A.; Loughrey, D.G. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: A systematic review. Syst. Rev. 2017, 6, 259. [Google Scholar] [CrossRef]
- Kawachi, I.; Berkman, L.F. Social ties and mental health. J. Urban Health 2001, 78, 458–467. [Google Scholar] [CrossRef]
- Fahmy, C. First weeks out: Social support stability and health among formerly incarcerated men. Soc. Sci. Med. 2021, 282, 114141. [Google Scholar] [CrossRef]
- Benavides, Q.; Doshi, M.; Valentín-Cortés, M.; Militzer, M.; Quiñones, S.; Kraut, R.; Rion, R.; Bryce, R.; Lopez, W.D.; Fleming, P.J. Immigration law enforcement, social support, and health for Latino immigrant families in Southeastern Michigan. Soc. Sci. Med. 2021, 280, 114027. [Google Scholar] [CrossRef]
- de la Haye, K.; Bell, B.M.; Salvy, S.J. The role of maternal social networks on the outcomes of a home-based childhood obesity prevention pilot intervention. J. Soc. Struct. 2019, 20, 7–28. [Google Scholar] [CrossRef] [PubMed]
- Okonofua, F. Maternal near-miss morbidity: Is this evidence of maternal health quality in sub-Saharan Africa? BJOG 2019, 126, 762. [Google Scholar] [CrossRef] [PubMed]
- Haddad, S.M.; Cecatti, J.G.; Souza, J.P.; Sousa, M.H.; Parpinelli, M.A.; Costa, M.L.; Pacagnella, R.C.; Brum, I.R.; Moraes Filho, O.B.; Feitosa, F.E.; et al. Applying the maternal near miss approach for the evaluation of quality of obstetric care: A worked example from a Multicenter Surveillance Study. BioMed Res. Int. 2014, 2014, 989815. [Google Scholar] [CrossRef] [PubMed]
- Rojas-Suarez, J.; Suarez, N.; Ateka-Barrutia, O. Developing obstetric medicine training in Latin America. Obstet. Med. 2017, 10, 16–20. [Google Scholar] [CrossRef]
- Vacaflor, C.H. Obstetric violence: A new framework for identifying challenges to maternal healthcare in Argentina. Reprod. Health Matters 2016, 24, 65–73. [Google Scholar] [CrossRef]

| Minimum | Maximum | Median | Mean | Std. Deviation | |
|---|---|---|---|---|---|
| MMR | 0.435 | 2.04 | 0.865 | 0.926 | 0.362 |
| Infant deaths | 0.638 | 5.38 | 2.96 | 2.98 | 0.935 |
| Unemployment rate | 143.4 | 1112.0 | 568.2 | 619.0 | 274.3 |
| Teen birth rate | 32.3 | 388.9 | 216.7 | 214.4 | 71.8 |
| Single mother birth rate | 419.5 | 1479.3 | 834.6 | 865.8 | 217.9 |
| Bed rate | 4.54 | 6.58 | 9.38 | 12.4 | 18.4 |
| Sex of child rate | 9021.9 | 10,679.4 | 10,395.1 | 10,350.5 | 282.4 |
| Vaginal birth rate | 2590.0 | 8056.0 | 5858.5 | 5957.6 | 1190.0 |
| MMR | Teen Birth Rate | Un- Employment Rate | Single Mother Birth Rate | Sex of Child | Bed Rate | Vaginal Birth Rate | Infant Death Rate | Birth Rate | |
|---|---|---|---|---|---|---|---|---|---|
| MMR | −0.249 | −0.206 | −0.299 | −0.311 | 0.112 | 0.514 | 0.539 | −0.299 | |
| Teen birth rate | 0.169 | −0.022 | 0.738 | 0.067 | 0.340 | −0.076 | −0.366 | 0.706 | |
| Un- employment rate | 0.258 | 0.905 | −0.047 | 0.112 | 0.071 | −0.333 | −0.383 | −0.0386 | |
| Single mother birth rate | 0.096 | 0.000 | 0.800 | 0.251 | 0.164 | −0.051 | −0.529 | 0.982 | |
| Sex of child rate | 0.083 | 0.715 | 0.543 | 0.166 | −0.024 | −0.238 | −0.385 | 0.227 | |
| Bed rate 2020 | 0.541 | 0.057 | 0.701 | 0.371 | 0.896 | −0.070 | −0.047 | 0.196 | |
| Vaginal birth rate | 0.003 | 0.680 | 0.062 | 0.781 | 0.190 | 0.702 | 0.425 | −0.0789 | |
| Infant death rate | 0.001 | 0.040 | 0.030 | 0.002 | 0.030 | 0.797 | 0.015 | −0.522 | |
| Birth rate | 0.0962 | 6.48 × 10−6 | 0.834 | 0 | 0.211 | 0.283 | 0.668 | 0.002 |
| Coefficients: | ||||
|---|---|---|---|---|
| Estimate (Log Scale) | Std. Error | z Value | Pr (>|t|) | |
| (Intercept) | −11.7347 | 2.8316 | −4.144 | 3.41 × 10−5 |
| Teen birth rate | −9.8370 | 8.2326 | −1.195 | 0.232128 |
| Unemployment rate | 1.6980 | 1.7900 | 0.949 | 0.342821 |
| Single mother birth rate | −9.5072 | 3.6353 | −2.615 | 0.008917 |
| Sex of child rate | 3.8285 | 2.5806 | 1.484 | 0.137925 |
| Bed rate | 172.6341 | 161.6696 | 1.068 | 0.285602 |
| Vaginal birth rate | 1.4974 | 0.4218 | 3.550 | 0.000385 |
| Infant death rate | 24.7191 | 13.6387 | 1.812 | 0.069920 |
| (Dispersion parameter for Poisson family taken to be 1) | ||||
| Coefficients: | ||||
|---|---|---|---|---|
| Estimate | Std. Error | Z Statistics | p Value | |
| (Intercept) | −5.5387 | 1.4233 | −3.8913 | 9.97 × 10−5 |
| Teen birth rate | 2.2327 | 4.8370 | 0.4616 | 0.6444 |
| Unemployment rate | −4.5737 | 0.8780 | −5.2090 | 1.898 × 10−7 |
| Single mother birth rate | −15.3186 | 1.4121 | −10.8479 | 2.041 × 10−27 |
| Sex of Child Rate | 0.5055 | 1.3343 | 0.3788 | 0.7048 |
| Bed rate | −0.0366 | 94.5633 | −0.0004 | 0.9997 |
| Vaginal birth rate | 0.9538 | 0.3091 | 3.0857 | 0.002031 |
| MMR | 0.0186 | 880.4206 | 0.0000 | 1 |
| Dispersion intercept | −0.0534 | 0.0270 | −1.9795 | 0.04776 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Jesus, M.; Sullivan, N.; Hopman, W.; Martinez, A.; Glenn, P.D., II; Msopa, S.; Milligan, B.; Doney, N.; Howell, W.; Sellers, K.; et al. Examining the Role of Quality of Institutionalized Healthcare on Maternal Mortality in the Dominican Republic. Int. J. Environ. Res. Public Health 2023, 20, 6413. https://doi.org/10.3390/ijerph20146413
De Jesus M, Sullivan N, Hopman W, Martinez A, Glenn PD II, Msopa S, Milligan B, Doney N, Howell W, Sellers K, et al. Examining the Role of Quality of Institutionalized Healthcare on Maternal Mortality in the Dominican Republic. International Journal of Environmental Research and Public Health. 2023; 20(14):6413. https://doi.org/10.3390/ijerph20146413
Chicago/Turabian StyleDe Jesus, Maria, Nora Sullivan, William Hopman, Alex Martinez, Paul David Glenn, II, Saviour Msopa, Brooke Milligan, Noah Doney, William Howell, Kimberly Sellers, and et al. 2023. "Examining the Role of Quality of Institutionalized Healthcare on Maternal Mortality in the Dominican Republic" International Journal of Environmental Research and Public Health 20, no. 14: 6413. https://doi.org/10.3390/ijerph20146413
APA StyleDe Jesus, M., Sullivan, N., Hopman, W., Martinez, A., Glenn, P. D., II, Msopa, S., Milligan, B., Doney, N., Howell, W., Sellers, K., & Jackson, M. C. (2023). Examining the Role of Quality of Institutionalized Healthcare on Maternal Mortality in the Dominican Republic. International Journal of Environmental Research and Public Health, 20(14), 6413. https://doi.org/10.3390/ijerph20146413






