Current Discoveries and Future Implications of Eating Disorders
Abstract
1. Introduction
2. Methods
3. Current Discoveries of Eating Disorders
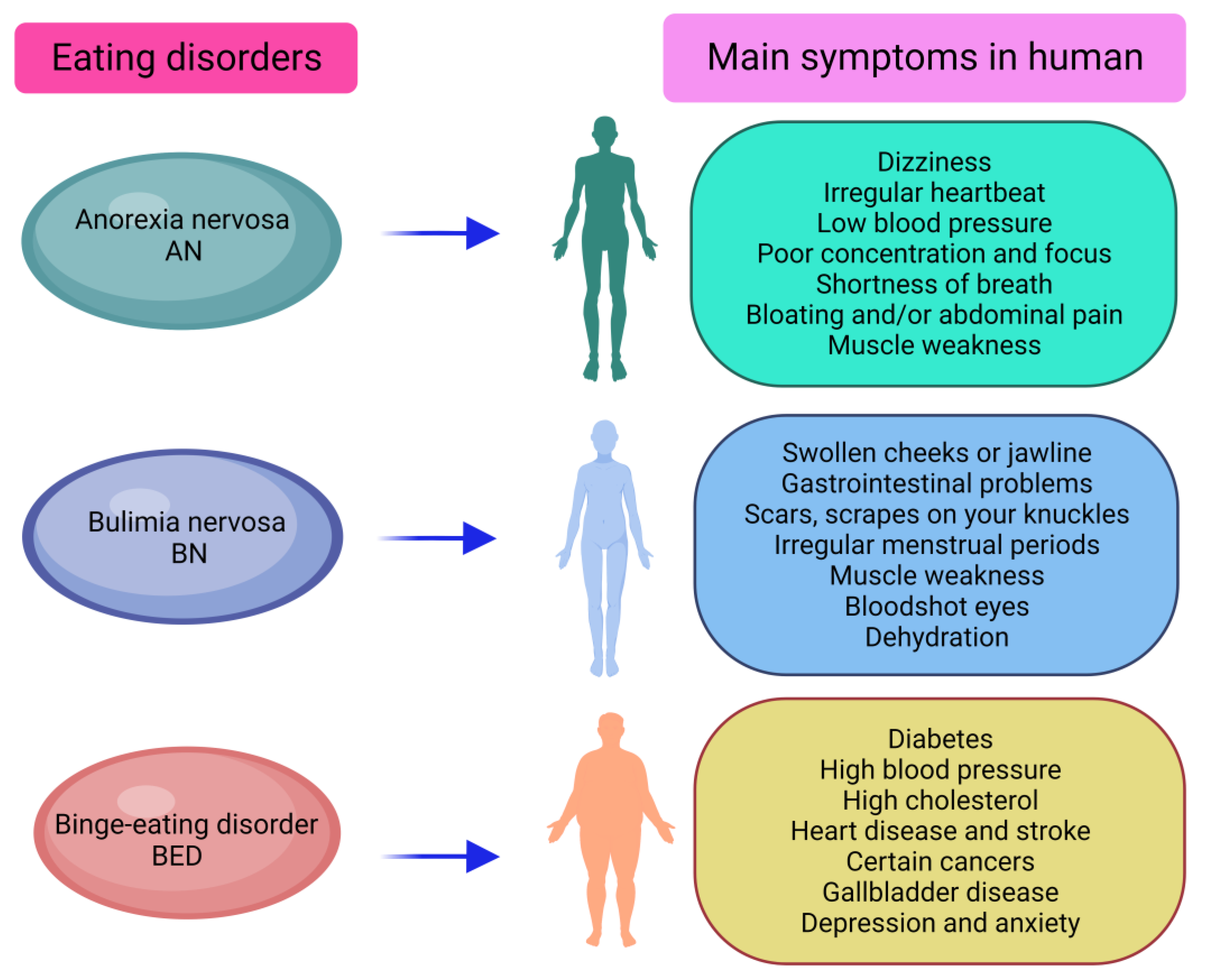
3.1. Anorexia Nervosa (AN)
3.2. Bulimia Nervosa (BN)
3.3. Binge Eating Disorder (BED)
3.4. Treatments of Eating Disorders
4. Discussion
4.1. Limitations of the Current Eating Disorders Research
4.2. Future Direction of Eating Disorder Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Diaz-Marsa, M.; Alberdi-Paramo, I.; Niell-Galmes, L. Nutritional supplements in eating disorders. Actas Esp. Psiquiatr. 2017, 45, 26–36. [Google Scholar]
- Zipfel, S.; Schmidt, U.; Giel, K.E. The hidden burden of eating disorders during the COVID-19 pandemic. Lancet Psychiatry 2022, 9, 9–11. [Google Scholar] [CrossRef]
- Azzeh, M.; Peachey, G.; Loney, T. Prevalence of High-Risk Disordered Eating Amongst Adolescents and Young Adults in the Middle East: A Scoping Review. Int. J. Env. Res. Public. Health 2022, 19, 5234. [Google Scholar] [CrossRef]
- Rantala, M.J.; Luoto, S.; Krama, T.; Krams, I. Eating Disorders: An Evolutionary Psychoneuroimmunological Approach. Front. Psychol. 2019, 10, 2200. [Google Scholar] [CrossRef]
- van Eeden, A.E.; van Hoeken, D.; Hoek, H.W. Incidence, prevalence and mortality of anorexia nervosa and bulimia nervosa. Curr. Opin. Psychiatry 2021, 34, 515–524. [Google Scholar] [CrossRef]
- Hotzy, F.; Risch, L.; Motteli, S. Nutritional Needs in Mental Healthcare: Study Protocol of a Prospective Analytic Observational Study Assessing Nutritional Status, Eating Behavior and Barriers to Healthy Eating in Psychiatric Inpatients and Outpatients Compared to Healthy Adults. Front. Psychiatry 2022, 13, 906234. [Google Scholar] [CrossRef]
- Coelho, J.S.; Lee, T.; Karnabi, P.; Burns, A.; Marshall, S.; Geller, J.; Lam, P.Y. Eating disorders in biological males: Clinical presentation and consideration of sex differences in a pediatric sample. J. Eat. Disord. 2018, 6, 40. [Google Scholar] [CrossRef] [PubMed]
- Ragnhildstveit, A.; Slayton, M.; Jackson, L.K.; Brendle, M.; Ahuja, S.; Holle, W.; Moore, C.; Sollars, K.; Seli, P.; Robison, R. Ketamine as a Novel Psychopharmacotherapy for Eating Disorders: Evidence and Future Directions. Brain Sci. 2022, 12, 382. [Google Scholar] [CrossRef] [PubMed]
- Petropoulou, A.; Bakounaki, G.; Grammatikopoulou, M.G.; Bogdanos, D.P.; Goulis, D.G.; Vassilakou, T. Eating Disorders and Disordered Eating Behaviors in Cystic Fibrosis: A Neglected Issue. Children 2022, 9, 915. [Google Scholar] [CrossRef] [PubMed]
- Olguin, P.; Fuentes, M.; Gabler, G.; Guerdjikova, A.I.; Keck, P.E., Jr.; McElroy, S.L. Medical comorbidity of binge eating disorder. Eat. Weight. Disord. 2017, 22, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Cena, H.; Vandoni, M.; Magenes, V.C.; Di Napoli, I.; Marin, L.; Baldassarre, P.; Luzzi, A.; De Pasquale, F.; Zuccotti, G.; Calcaterra, V. Benefits of Exercise in Multidisciplinary Treatment of Binge Eating Disorder in Adolescents with Obesity. Int. J. Env. Res. Public. Health 2022, 19, 8300. [Google Scholar] [CrossRef] [PubMed]
- Rendina-Ruedy, E.; Smith, B.J. Common Dietary Modifications in Preclinical Models to Study Skeletal Health. Front. Endocrinol 2022, 13, 932343. [Google Scholar] [CrossRef] [PubMed]
- Fontana, L.; Garzia, E.; Marfia, G.; Galiano, V.; Miozzo, M. Epigenetics of functional hypothalamic amenorrhea. Front. Endocrinol 2022, 13, 953431. [Google Scholar] [CrossRef] [PubMed]
- Frostad, S. Are the Effects of Malnutrition on the Gut Microbiota-Brain Axis the Core Pathologies of Anorexia Nervosa? Microorganisms 2022, 10, 1486. [Google Scholar] [CrossRef] [PubMed]
- Freizinger, M.; Recto, M.; Jhe, G.; Lin, J. Atypical Anorexia in Youth: Cautiously Bridging the Treatment Gap. Children 2022, 9, 837. [Google Scholar] [CrossRef] [PubMed]
- Pedreira, C.C.; Maya, J.; Misra, M. Functional hypothalamic amenorrhea: Impact on bone and neuropsychiatric outcomes. Front. Endocrinol 2022, 13, 953180. [Google Scholar] [CrossRef]
- Keeler, J.L.; Patsalos, O.; Chung, R.; Schmidt, U.; Breen, G.; Treasure, J.; Hubertus, H.; Dalton, B. Short communication: Serum levels of brain-derived neurotrophic factor and association with pro-inflammatory cytokines in acute and recovered anorexia nervosa. J. Psychiatr. Res. 2022, 150, 34–39. [Google Scholar] [CrossRef]
- Reyes-Haro, D. Glial cells in anorexia. Front. Cell Neurosci. 2022, 16, 983577. [Google Scholar] [CrossRef]
- Djogo, T.; Robins, S.C.; Schneider, S.; Kryzskaya, D.; Liu, X.; Mingay, A.; Gillon, C.J.; Kim, J.H.; Storch, K.F.; Boehm, U.; et al. Adult NG2-Glia Are Required for Median Eminence-Mediated Leptin Sensing and Body Weight Control. Cell Metab. 2016, 23, 797–810. [Google Scholar] [CrossRef]
- Frintrop, L.; Liesbrock, J.; Paulukat, L.; Johann, S.; Kas, M.J.; Tolba, R.; Heussen, N.; Neulen, J.; Konrad, K.; Herpertz-Dahlmann, B.; et al. Reduced astrocyte density underlying brain volume reduction in activity-based anorexia rats. World J. Biol. Psychiatry 2018, 19, 225–235. [Google Scholar] [CrossRef]
- Giel, K.; Zipfel, S.; Hallschmid, M. Oxytocin and Eating Disorders: A Narrative Review on Emerging Findings and Perspectives. Curr. Neuropharmacol. 2018, 16, 1111–1121. [Google Scholar] [CrossRef]
- Lafrance, V.; Inoue, W.; Kan, B.; Luheshi, G.N. Leptin modulates cell morphology and cytokine release in microglia. Brain Behav. Immun. 2010, 24, 358–365. [Google Scholar] [CrossRef]
- Cai, X.; Liu, H.; Feng, B.; Yu, M.; He, Y.; Liu, H.; Liang, C.; Yang, Y.; Tu, L.; Zhang, N.; et al. A D2 to D1 shift in dopaminergic inputs to midbrain 5-HT neurons causes anorexia in mice. Nat. Neurosci. 2022, 25, 646–658. [Google Scholar] [CrossRef] [PubMed]
- Sutton Hickey, A.K.; Duane, S.C.; Mickelsen, L.E.; Karolczak, E.O.; Shamma, A.M.; Skillings, A.; Li, C.; Krashes, M.J. AgRP neurons coordinate the mitigation of activity-based anorexia. Mol. Psychiatry 2022, 28, 1622–1635. [Google Scholar] [CrossRef] [PubMed]
- Plata-Salaman, C.R.; Sonti, G.; Borkoski, J.P.; Wilson, C.D.; French-Mullen, J.M. Anorexia induced by chronic central administration of cytokines at estimated pathophysiological concentrations. Physiol. Behav. 1996, 60, 867–875. [Google Scholar] [CrossRef]
- Casper, R.C. Restlessness and an Increased Urge to Move (Drive for Activity) in Anorexia Nervosa May Strengthen Personal Motivation to Maintain Caloric Restriction and May Augment Body Awareness and Proprioception: A Lesson From Leptin Administration in Anorexia Nervosa. Front. Psychol. 2022, 13, 885274. [Google Scholar] [PubMed]
- Hebebrand, J.; Hildebrandt, T.; Schlogl, H.; Seitz, J.; Denecke, S.; Vieira, D.; Gradl-Dietsch, G.; Peters, T.; Antel, J.; Lau, D.; et al. The role of hypoleptinemia in the psychological and behavioral adaptation to starvation: Implications for anorexia nervosa. Neurosci. Biobehav. Rev. 2022, 141, 104807. [Google Scholar] [CrossRef]
- Shobeiri, P.; Kalantari, A.; Teixeira, A.L.; Rezaei, N. Shedding light on biological sex differences and microbiota-gut-brain axis: A comprehensive review of its roles in neuropsychiatric disorders. Biol. Sex. Differ. 2022, 13, 12. [Google Scholar] [CrossRef] [PubMed]
- Russell, G. Bulimia nervosa: An ominous variant of anorexia nervosa. Psychol. Med. 1979, 9, 429–448. [Google Scholar] [CrossRef]
- Castillo, M.; Weiselberg, E. Bulimia Nervosa/Purging Disorder. Curr. Probl. Pediatr. Adolesc. Health Care 2017, 47, 85–94. [Google Scholar] [CrossRef]
- Wang, H.R.; Hu, S.W.; Zhang, S.; Song, Y.; Wang, X.Y.; Wang, L.; Li, Y.Y.; Yu, Y.M.; Liu, H.; Liu, D.; et al. KCNQ Channels in the Mesolimbic Reward Circuit Regulate Nociception in Chronic Pain in Mice. Neurosci. Bull. 2021, 37, 597–610. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Bi, K.; An, J.; Li, M.; Li, K.; Kong, Q.M.; Li, X.N.; Lu, Q.; Si, T.M. Abnormal structural brain network and hemisphere-specific changes in bulimia nervosa. Transl. Psychiatry 2019, 9, 206. [Google Scholar] [CrossRef] [PubMed]
- Berner, L.A.; Simmons, A.N.; Wierenga, C.E.; Bischoff-Grethe, A.; Paulus, M.P.; Bailer, U.F.; Kaye, W.H. Altered anticipation and processing of aversive interoceptive experience among women remitted from bulimia nervosa. Neuropsychopharmacology 2019, 44, 1265–1273. [Google Scholar] [CrossRef]
- Monteleone, P.; Martiadis, V.; Colurcio, B.; Maj, M. Leptin secretion is related to chronicity and severity of the illness in bulimia nervosa. Psychosom. Med. 2002, 64, 874–879. [Google Scholar] [PubMed]
- Brewerton, T.D.; Lesem, M.D.; Kennedy, A.; Garvey, W.T. Reduced plasma leptin concentrations in bulimia nervosa. Psychoneuroendocrinology 2000, 25, 649–658. [Google Scholar] [CrossRef] [PubMed]
- Jimerson, D.C.; Mantzoros, C.; Wolfe, B.E.; Metzger, E.D. Decreased serum leptin in bulimia nervosa. J. Clin. Endocrinol. Metab. 2000, 85, 4511–4514. [Google Scholar] [CrossRef]
- Hu, Y.; Kang, Q.; Chen, C.; Guo, L.; Chen, J. Increased plasma asprosin levels are associated with overeating and loss of control in drug-free bulimia nervosa. Eat. Weight. Disord. 2022, 27, 2783–2789. [Google Scholar] [CrossRef]
- Mihov, Y.; Treyer, V.; Akkus, F.; Toman, E.; Milos, G.; Ametamey, S.M.; Johayem, A.; Hasler, G. Metabotropic glutamate receptor 5 in bulimia nervosa. Sci. Rep. 2020, 10, 6374. [Google Scholar] [CrossRef]
- Qiu, A.; Adler, M.; Crocetti, D.; Miller, M.I.; Mostofsky, S.H. Basal ganglia shapes predict social, communication, and motor dysfunctions in boys with autism spectrum disorder. J. Am. Acad. Child. Adolesc. Psychiatry 2010, 49, 539–551, 551.e1-4. [Google Scholar]
- Berner, L.A.; Wang, Z.; Stefan, M.; Lee, S.; Huo, Z.; Cyr, M.; Marsh, R. Subcortical Shape Abnormalities in Bulimia Nervosa. Biol. Psychiatry Cogn. Neurosci. Neuroimaging 2019, 4, 1070–1079. [Google Scholar] [CrossRef]
- Lecomte, A.; Zerrouk, A.; Sibeoni, J.; Khan, S.; Revah-Levy, A.; Lachal, J. The role of food in family relationships amongst adolescents with bulimia nervosa: A qualitative study using photo-elicitation. Appetite 2019, 141, 104305. [Google Scholar] [CrossRef]
- Hudson, J.I.; Hiripi, E.; Pope, H.G., Jr.; Kessler, R.C. The prevalence and correlates of eating disorders in the National Comorbidity Survey Replication. Biol. Psychiatry 2007, 61, 348–358. [Google Scholar] [CrossRef]
- di Giacomo, E.; Aliberti, F.; Pescatore, F.; Santorelli, M.; Pessina, R.; Placenti, V.; Colmegna, F.; Clerici, M. Disentangling binge eating disorder and food addiction: A systematic review and meta-analysis. Eat. Weight. Disord. 2022, 27, 1963–1970. [Google Scholar] [CrossRef]
- Hilker, I.; Sanchez, I.; Steward, T.; Jimenez-Murcia, S.; Granero, R.; Gearhardt, A.N.; Rodriguez-Munoz, R.C.; Dieguez, C.; Crujeiras, A.B.; Tolosa-Sola, I.; et al. Food Addiction in Bulimia Nervosa: Clinical Correlates and Association with Response to a Brief Psychoeducational Intervention. Eur. Eat. Disord. Rev. 2016, 24, 482–488. [Google Scholar] [CrossRef] [PubMed]
- Imperatori, C.; Fabbricatore, M.; Vumbaca, V.; Innamorati, M.; Contardi, A.; Farina, B. Food Addiction: Definition, measurement and prevalence in healthy subjects and in patients with eating disorders. Riv. Psichiatr. 2016, 51, 60–65. [Google Scholar] [PubMed]
- Cao, X.; Xu, P.; Oyola, M.G.; Xia, Y.; Yan, X.; Saito, K.; Zou, F.; Wang, C.; Yang, Y.; Hinton, A., Jr.; et al. Estrogens stimulate serotonin neurons to inhibit binge-like eating in mice. J. Clin. Investig. 2014, 124, 4351–4362. [Google Scholar] [CrossRef] [PubMed]
- Val-Laillet, D.; Aarts, E.; Weber, B.; Ferrari, M.; Quaresima, V.; Stoeckel, L.E.; Alonso-Alonso, M.; Audette, M.; Malbert, C.H.; Stice, E. Neuroimaging and neuromodulation approaches to study eating behavior and prevent and treat eating disorders and obesity. Neuroimage Clin. 2015, 8, 1–31. [Google Scholar] [CrossRef]
- Xu, P.; He, Y.; Cao, X.; Valencia-Torres, L.; Yan, X.; Saito, K.; Wang, C.; Yang, Y.; Hinton, A., Jr.; Zhu, L.; et al. Activation of Serotonin 2C Receptors in Dopamine Neurons Inhibits Binge-like Eating in Mice. Biol. Psychiatry 2017, 81, 737–747. [Google Scholar] [CrossRef]
- Zhang, X.; van den Pol, A.N. Rapid binge-like eating and body weight gain driven by zona incerta GABA neuron activation. Science 2017, 356, 853–859. [Google Scholar] [CrossRef]
- Hildebrandt, B.A.; Ahmari, S.E. Breaking It Down: Investigation of Binge Eating Components in Animal Models to Enhance Translation. Front. Psychiatry 2021, 12, 728535. [Google Scholar] [CrossRef]
- Mineo, D.; Cacace, F.; Mancini, M.; Vannelli, A.; Campanelli, F.; Natale, G.; Marino, G.; Cardinale, A.; Calabresi, P.; Picconi, B.; et al. Dopamine drives binge-like consumption of a palatable food in experimental Parkinsonism. Mov. Disord. 2019, 34, 821–831. [Google Scholar] [CrossRef] [PubMed]
- Prins, K.; Huisman, M.; McLuskey, A.; Mies, R.; Karels, B.; Delhanty, P.J.D.; Visser, J.A. Ghrelin deficiency sex-dependently affects food intake, locomotor activity, and adipose and hepatic gene expression in a binge-eating mouse model. Am. J. Physiol. Endocrinol. Metab. 2022, 322, E494–E507. [Google Scholar] [CrossRef] [PubMed]
- Micioni Di Bonaventura, E.; Botticelli, L.; Del Bello, F.; Giorgioni, G.; Piergentili, A.; Quaglia, W.; Cifani, C.; Micioni Di Bonaventura, M.V. Assessing the role of ghrelin and the enzyme ghrelin O-acyltransferase (GOAT) system in food reward, food motivation, and binge eating behavior. Pharmacol. Res. 2021, 172, 105847. [Google Scholar] [CrossRef]
- Burmester, V.; Graham, E.; Nicholls, D. Physiological, emotional and neural responses to visual stimuli in eating disorders: A review. J. Eat. Disord. 2021, 9, 23. [Google Scholar] [CrossRef]
- Yu, Y.; Miller, R.; Groth, S.W. A literature review of dopamine in binge eating. J. Eat. Disord. 2022, 10, 11. [Google Scholar] [CrossRef]
- Alboni, S.; Micioni Di Bonaventura, M.V.; Benatti, C.; Giusepponi, M.E.; Brunello, N.; Cifani, C. Hypothalamic expression of inflammatory mediators in an animal model of binge eating. Behav. Brain Res. 2017, 320, 420–430. [Google Scholar] [CrossRef]
- Abbott, S.; Dindol, N.; Tahrani, A.A.; Piya, M.K. Binge eating disorder and night eating syndrome in adults with type 2 diabetes: A systematic review. J. Eat. Disord. 2018, 6, 36. [Google Scholar] [CrossRef]
- Harris, S.R.; Carrillo, M.; Fujioka, K. Binge-Eating Disorder and Type 2 Diabetes: A Review. Endocr. Pract. 2021, 27, 158–164. [Google Scholar] [CrossRef]
- Bryant, E.; Spielman, K.; Le, A.; Marks, P.; Touyz, S.; Maguire, S. Screening, assessment and diagnosis in the eating disorders: Findings from a rapid review. J. Eat. Disord. 2022, 10, 78. [Google Scholar] [CrossRef]
- Riva, G.; Malighetti, C.; Serino, S. Virtual reality in the treatment of eating disorders. Clin. Psychol. Psychother. 2021, 28, 477–488. [Google Scholar] [CrossRef] [PubMed]
- Quansah Amissah, R.; Basha, D.; Bukhtiyarova, O.; Timofeeva, E.; Timofeev, I. Neuronal activities during palatable food consumption in the reward system of binge-like eating female rats. Physiol. Behav. 2021, 242, 113604. [Google Scholar] [CrossRef] [PubMed]
- Abdelaal, M.; le Roux, C.W.; Docherty, N.G. Morbidity and mortality associated with obesity. Ann. Transl. Med. 2017, 5, 161. [Google Scholar] [CrossRef] [PubMed]
- Boye, K.S.; Ford, J.H.; Thieu, V.T.; Lage, M.J.; Terrell, K.A. The Association Between Obesity and the 5-Year Prevalence of Morbidity and Mortality Among Adults with Type 2 Diabetes. Diabetes Ther. 2023, 14, 709–721. [Google Scholar] [CrossRef]
- Lenz, M.; Richter, T.; Muhlhauser, I. The morbidity and mortality associated with overweight and obesity in adulthood: A systematic review. Dtsch. Arztebl. Int. 2009, 106, 641–648. [Google Scholar]
- Sambandam, S.; Bokhari, S.; Tsai, S.; Nathan, V.S.; Senthil, T.; Lanier, H.; Huerta, S. Morbidity and Mortality in Non-Obese Compared to Different Classes of Obesity in Patients Undergoing Transtibial Amputations. J. Clin. Med. 2022, 12, 267. [Google Scholar] [CrossRef] [PubMed]
- Rekkers, M.E.; Aardenburg, L.; Scheffers, M.; van Elburg, A.A.; van Busschbach, J.T. Shifting the Focus: A Pilot Study on the Effects of Positive Body Exposure on Body Satisfaction, Body Attitude, Eating Pathology and Depressive Symptoms in Female Patients with Eating Disorders. Int. J. Env. Res. Public. Health 2022, 19, 11794. [Google Scholar] [CrossRef]
- Navarro-Tapia, E.; Almeida-Toledano, L.; Sebastiani, G.; Serra-Delgado, M.; Garcia-Algar, O.; Andreu-Fernandez, V. Effects of Microbiota Imbalance in Anxiety and Eating Disorders: Probiotics as Novel Therapeutic Approaches. Int. J. Mol. Sci. 2021, 22, 2351. [Google Scholar] [CrossRef]
- Palmieri, S.; Mansueto, G.; Scaini, S.; Caselli, G.; Sapuppo, W.; Spada, M.M.; Sassaroli, S.; Ruggiero, G.M. Repetitive Negative Thinking and Eating Disorders: A Meta-Analysis of the Role of Worry and Rumination. J. Clin. Med. 2021, 10, 2448. [Google Scholar] [CrossRef]
- Barnes, R.D.; Ivezaj, V.; Martino, S.; Pittman, B.P.; Paris, M.; Grilo, C.M. Examining motivational interviewing plus nutrition psychoeducation for weight loss in primary care. J. Psychosom. Res. 2018, 104, 101–107. [Google Scholar] [CrossRef]
- Yohn, S.E.; Galbraith, J.; Calipari, E.S.; Conn, P.J. Shared Behavioral and Neurocircuitry Disruptions in Drug Addiction, Obesity, and Binge Eating Disorder: Focus on Group I mGluRs in the Mesolimbic Dopamine Pathway. ACS Chem. Neurosci. 2019, 10, 2125–2143. [Google Scholar] [CrossRef]
- Manasse, S.M.; Espel, H.M.; Forman, E.M.; Ruocco, A.C.; Juarascio, A.S.; Butryn, M.L.; Zhang, F.; Lowe, M.R. The independent and interacting effects of hedonic hunger and executive function on binge eating. Appetite 2015, 89, 16–21. [Google Scholar] [CrossRef]
- Sultson, H.; Kreegipuu, K.; Akkermann, K. Exploring the role of momentary positive and negative affect in overeating and binge eating: Evidence for different associations among men and women. Appetite 2022, 168, 105758. [Google Scholar] [CrossRef]
- Guerdjikova, A.I.; Mori, N.; Casuto, L.S.; McElroy, S.L. Novel pharmacologic treatment in acute binge eating disorder-role of lisdexamfetamine. Neuropsychiatr. Dis. Treat. 2016, 12, 833–841. [Google Scholar] [CrossRef]
- Schneider, E.; Martin, E.; Rotshtein, P.; Qureshi, K.L.; Chamberlain, S.R.; Spetter, M.S.; Dourish, C.T.; Higgs, S. The effects of lisdexamfetamine dimesylate on eating behaviour and homeostatic, reward and cognitive processes in women with binge-eating symptoms: An experimental medicine study. Transl. Psychiatry 2022, 12, 9. [Google Scholar] [CrossRef]
- Heal, D.J.; Gosden, J. What pharmacological interventions are effective in binge-eating disorder? Insights from a critical evaluation of the evidence from clinical trials. Int. J. Obes. 2022, 46, 677–695. [Google Scholar] [CrossRef] [PubMed]
- Heal, D.J.; Smith, S.L. Prospects for new drugs to treat binge-eating disorder: Insights from psychopathology and neuropharmacology. J. Psychopharmacol. 2022, 36, 680–703. [Google Scholar] [CrossRef] [PubMed]
- Romano, A.; Micioni Di Bonaventura, M.V.; Gallelli, C.A.; Koczwara, J.B.; Smeets, D.; Giusepponi, M.E.; De Ceglia, M.; Friuli, M.; Micioni Di Bonaventura, E.; Scuderi, C.; et al. Oleoylethanolamide decreases frustration stress-induced binge-like eating in female rats: A novel potential treatment for binge eating disorder. Neuropsychopharmacology 2020, 45, 1931–1941. [Google Scholar] [CrossRef] [PubMed]
- Dakanalis, A.; Clerici, M.; Stice, E. Prevention of eating disorders: Current evidence-base for dissonance-based programmes and future directions. Eat. Weight. Disord. 2019, 24, 597–603. [Google Scholar] [CrossRef]
- Touyz, S.; Hay, P. The future of eating disorders research: An editorial. J. Eat. Disord. 2022, 10, 10. [Google Scholar] [CrossRef]
- Jagielska, G.; Kacperska, I. Outcome, comorbidity and prognosis in anorexia nervosa. Psychiatr. Pol. 2017, 51, 205–218. [Google Scholar] [CrossRef]
- Chatelet, S.; Wang, J.; Gjoertz, M.; Lier, F.; Monney Chaubert, C.; Ambresin, A.E. Factors associated with weight gain in anorexia nervosa inpatients. Eat. Weight. Disord. 2020, 25, 939–950. [Google Scholar] [CrossRef] [PubMed]
- Van Huysse, J.L.; Smith, K.; Mammel, K.A.; Prohaska, N.; Rienecke, R.D. Early weight gain predicts treatment response in adolescents with anorexia nervosa enrolled in a family-based partial hospitalization program. Int. J. Eat. Disord. 2020, 53, 606–610. [Google Scholar] [CrossRef]
- Loomes, R.; Bryant-Waugh, R. Widening the reach of family-based interventions for Anorexia Nervosa: Autism-adaptations for children and adolescents. J. Eat. Disord. 2021, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Monteleone, A.M.; Pellegrino, F.; Croatto, G.; Carfagno, M.; Hilbert, A.; Treasure, J.; Wade, T.; Bulik, C.M.; Zipfel, S.; Hay, P.; et al. Treatment of eating disorders: A systematic meta-review of meta-analyses and network meta-analyses. Neurosci. Biobehav. Rev. 2022, 142, 104857. [Google Scholar] [CrossRef] [PubMed]
- Leppanen, J.; Cardi, V.; Ng, K.W.; Paloyelis, Y.; Stein, D.; Tchanturia, K.; Treasure, J. The effects of intranasal oxytocin on smoothie intake, cortisol and attentional bias in anorexia nervosa. Psychoneuroendocrinology 2017, 79, 167–174. [Google Scholar] [CrossRef]
- Schwenzer, C.; Voelz, C.; Kogel, V.; Schlosser, A.; Herpertz-Dahlmann, B.; Beyer, C.; Seitz, J.; Trinh, S. Fear and food: Anxiety-like behavior and the susceptibility to weight loss in an activity-based anorexia rat model. Clin. Transl. Sci. 2022, 15, 889–898. [Google Scholar] [CrossRef]
- Sorrentino, D.; Mucci, A.; Merlotti, E.; Galderisi, S.; Maj, M. Modified nutritional counselling to increase motivation to treatment in anorexia nervosa. Eur. Psychiatry 2005, 20, 186–187. [Google Scholar] [CrossRef]
- Gruber, M.; Konig, D.; Holzhauser, J.; Castillo, D.M.; Bluml, V.; Jahn, R.; Leser, C.; Werneck-Rohrer, S.; Werneck, H. Parental feeding practices and the relationship with parents in female adolescents and young adults with eating disorders: A case control study. PLoS ONE 2020, 15, e0242518. [Google Scholar] [CrossRef]
- Cassioli, E.; Rossi, E.; Vizzotto, C.; Malinconi, V.; Vignozzi, L.; Ricca, V.; Castellini, G. Avoidant Attachment Style Moderates the Recovery of Healthy Sexuality in Women With Anorexia Nervosa Treated With Enhanced Cognitive Behavior Therapy (CBT-E): A 2-Year Follow-Up Study. J. Sex. Med. 2022, 19, 347–355. [Google Scholar] [CrossRef]
- Catone, G.; Salerno, F.; Muzzo, G.; Lanzara, V.; Gritti, A. Association between anorexia nervosa and other specified eating or feeding disorders and paranoia in adolescents: What factors are involved? Riv. Psichiatr. 2021, 56, 100–106. [Google Scholar]
- Powers, P.S.; Bruty, H. Pharmacotherapy for eating disorders and obesity. Child. Adolesc. Psychiatr. Clin. N. Am. 2009, 18, 175–187. [Google Scholar] [CrossRef]
- Dalle Grave, R.; El Ghoch, M.; Sartirana, M.; Calugi, S. Cognitive Behavioral Therapy for Anorexia Nervosa: An Update. Curr. Psychiatry Rep. 2016, 18, 2. [Google Scholar] [CrossRef]
- Kaa, B.S.; Bunemann, J.M.N.; Clausen, L. A benchmark study of a combined individual and group anorexia nervosa therapy program. Nord. J. Psychiatry 2022, 77, 447–454. [Google Scholar] [CrossRef]
- de Vos, J.; Houtzager, L.; Katsaragaki, G.; van de Berg, E.; Cuijpers, P.; Dekker, J. Meta analysis on the efficacy of pharmacotherapy versus placebo on anorexia nervosa. J. Eat. Disord. 2014, 2, 27. [Google Scholar] [CrossRef]
- Berner, L.A.; Brown, T.A.; Lavender, J.M.; Lopez, E.; Wierenga, C.E.; Kaye, W.H. Neuroendocrinology of reward in anorexia nervosa and bulimia nervosa: Beyond leptin and ghrelin. Mol. Cell Endocrinol. 2019, 497, 110320. [Google Scholar] [CrossRef]
- Harrington, B.C.; Jimerson, M.; Haxton, C.; Jimerson, D.C. Initial evaluation, diagnosis, and treatment of anorexia nervosa and bulimia nervosa. Am. Fam. Physician 2015, 91, 46–52. [Google Scholar] [PubMed]
- Agras, W.S.; Bohon, C. Cognitive Behavioral Therapy for the Eating Disorders. Annu. Rev. Clin. Psychol. 2021, 17, 417–438. [Google Scholar] [CrossRef]
- Stabouli, S.; Erdine, S.; Suurorg, L.; Jankauskiene, A.; Lurbe, E. Obesity and Eating Disorders in Children and Adolescents: The Bidirectional Link. Nutrients 2021, 13, 4321. [Google Scholar] [CrossRef] [PubMed]
- Bello, N.T.; Yeomans, B.L. Safety of pharmacotherapy options for bulimia nervosa and binge eating disorder. Expert. Opin. Drug Saf. 2018, 17, 17–23. [Google Scholar] [CrossRef] [PubMed]
- Crow, S.J. Pharmacologic Treatment of Eating Disorders. Psychiatr. Clin. North. Am. 2019, 42, 253–262. [Google Scholar] [CrossRef]
- Klein, D.A.; Sylvester, J.E.; Schvey, N.A. Eating Disorders in Primary Care: Diagnosis and Management. Am. Fam. Physician 2021, 103, 22–32. [Google Scholar]
- Denman, E.; Parker, E.K.; Ashley, M.A.; Harris, D.M.; Halaki, M.; Flood, V.; Stefoska-Needham, A. Understanding training needs in eating disorders of graduating and new graduate dietitians in Australia: An online survey. J. Eat. Disord. 2021, 9, 27. [Google Scholar] [CrossRef] [PubMed]
- Hay, P.; Palavras, M.A.; da Luz, F.Q.; Dos Anjos Garnes, S.; Sainsbury, A.; Touyz, S.; Appolinario, J.C.; Claudino, A.M. Physical and mental health outcomes of an integrated cognitive behavioural and weight management therapy for people with an eating disorder characterized by binge eating and a high body mass index: A randomized controlled trial. BMC Psychiatry 2022, 22, 355. [Google Scholar] [CrossRef] [PubMed]
- Brownley, K.A.; Berkman, N.D.; Peat, C.M.; Lohr, K.N.; Cullen, K.E.; Bann, C.M.; Bulik, C.M. Binge-Eating Disorder in Adults: A Systematic Review and Meta-analysis. Ann. Intern. Med. 2016, 165, 409–420. [Google Scholar] [CrossRef] [PubMed]
- Mathisen, T.F.; Rosenvinge, J.H.; Friborg, O.; Vrabel, K.; Bratland-Sanda, S.; Pettersen, G.; Sundgot-Borgen, J. Is physical exercise and dietary therapy a feasible alternative to cognitive behavior therapy in treatment of eating disorders? A randomized controlled trial of two group therapies. Int. J. Eat. Disord. 2020, 53, 574–585. [Google Scholar] [CrossRef] [PubMed]
- Walenda, A.; Bogusz, K.; Kopera, M.; Jakubczyk, A.; Wojnar, M.; Kucharska, K. Emotion regulation in binge eating disorder. Psychiatr. Pol. 2021, 55, 1433–1448. [Google Scholar] [CrossRef]
- Schneider, E.; Higgs, S.; Dourish, C.T. Lisdexamfetamine and binge-eating disorder: A systematic review and meta-analysis of the preclinical and clinical data with a focus on mechanism of drug action in treating the disorder. Eur. Neuropsychopharmacol. 2021, 53, 49–78. [Google Scholar] [CrossRef]
- Costa, M.B.; Melnik, T. Effectiveness of psychosocial interventions in eating disorders: An overview of Cochrane systematic reviews. Einstein 2016, 14, 235–277. [Google Scholar] [CrossRef]
- Karam, A.M.; Fitzsimmons-Craft, E.E.; Tanofsky-Kraff, M.; Wilfley, D.E. Interpersonal Psychotherapy and the Treatment of Eating Disorders. Psychiatr. Clin. 2019, 42, 205–218. [Google Scholar] [CrossRef]
- Forrest, L.N.; Franko, D.L.; Thompson-Brenner, H.; Grilo, C.M. Examining changes in binge-eating disorder network centrality and structure in patients treated with cognitive-behavioral therapy versus interpersonal psychotherapy. Int. J. Eat. Disord. 2022, 56, 944–955. [Google Scholar] [CrossRef]
- Grilo, C.M.; Reas, D.L.; Mitchell, J.E. Combining Pharmacological and Psychological Treatments for Binge Eating Disorder: Current Status, Limitations, and Future Directions. Curr. Psychiatry Rep. 2016, 18, 55. [Google Scholar] [CrossRef] [PubMed]
- Garvey, W.T.; Mechanick, J.I.; Brett, E.M.; Garber, A.J.; Hurley, D.L.; Jastreboff, A.M.; Nadolsky, K.; Pessah-Pollack, R.; Plodkowski, R. Reviewers of the AACEOCPG American Association of Clinical Endocrinologists and American College of Endocrinology Comprehensive Clinical Practice Guidelines for Medical Care of Patients with Obesity. Endocr. Pract. 2016, 22 (Suppl. S3), 1–203. [Google Scholar] [CrossRef] [PubMed]
- Safer, D.L.; Adler, S.; Dalai, S.S.; Bentley, J.P.; Toyama, H.; Pajarito, S.; Najarian, T. A randomized, placebo-controlled crossover trial of phentermine-topiramate ER in patients with binge-eating disorder and bulimia nervosa. Int. J. Eat. Disord. 2020, 53, 266–277. [Google Scholar] [CrossRef] [PubMed]
- Adams, G.; Turner, H.; Hoskins, J.; Robinson, A.; Waller, G. Effectiveness of a brief form of group dialectical behavior therapy for binge-eating disorder: Case series in a routine clinical setting. Int. J. Eat. Disord. 2021, 54, 615–620. [Google Scholar] [CrossRef]
- Carter, J.C.; Kenny, T.E.; Singleton, C.; Van Wijk, M.; Heath, O. Dialectical behavior therapy self-help for binge-eating disorder: A randomized controlled study. Int. J. Eat. Disord. 2020, 53, 451–460. [Google Scholar] [CrossRef]
- Lammers, M.W.; Vroling, M.S.; Crosby, R.D.; van Strien, T. Dialectical behavior therapy compared to cognitive behavior therapy in binge-eating disorder: An effectiveness study with 6-month follow-up. Int. J. Eat. Disord. 2022, 55, 902–913. [Google Scholar] [CrossRef] [PubMed]
- Duan, H.; Zhu, L.; Li, M.; Zhang, X.; Zhang, B.; Fang, S. Comparative efficacy and acceptability of selective serotonin reuptake inhibitor antidepressants for binge eating disorder: A network meta-analysis. Front. Pharmacol. 2022, 13, 949823. [Google Scholar] [CrossRef]
- Amodeo, G.; Cuomo, A.; Bolognesi, S.; Goracci, A.; Trusso, M.A.; Piccinni, A.; Neal, S.M.; Baldini, I.; Federico, E.; Taddeucci, C.; et al. Pharmacotherapeutic strategies for treating binge eating disorder. Evidence from clinical trials and implications for clinical practice. Expert Opin. Pharmacother. 2019, 20, 679–690. [Google Scholar] [CrossRef]
- Spalding, W.M.; Bertoia, M.L.; Bulik, C.M.; Seeger, J.D. Treatment characteristics among patients with binge-eating disorder: An electronic health records analysis. Postgrad. Med. 2022, 135, 254–264. [Google Scholar] [CrossRef]
- Guerdjikova, A.I.; Williams, S.; Blom, T.J.; Mori, N.; McElroy, S.L. Combination Phentermine-Topiramate Extended Release for the Treatment of Binge Eating Disorder: An Open-Label, Prospective Study. Innov. Clin. Neurosci. 2018, 15, 17–21. [Google Scholar]
- Fardouly, J.; Crosby, R.D.; Sukunesan, S. Potential benefits and limitations of machine learning in the field of eating disorders: Current research and future directions. J. Eat. Disord. 2022, 10, 66. [Google Scholar] [CrossRef] [PubMed]
- Haghshomar, M.; Shobeiri, P.; Brand, S.; Rossell, S.L.; Akhavan Malayeri, A.; Rezaei, N. Changes of symptoms of eating disorders (ED) and their related psychological health issues during the COVID-19 pandemic: A systematic review and meta-analysis. J. Eat. Disord. 2022, 10, 51. [Google Scholar] [CrossRef] [PubMed]
- Gorrell, S.; Reilly, E.E.; Brosof, L.; Le Grange, D. Use of Telehealth in the Management of Adolescent Eating Disorders: Patient Perspectives and Future Directions Suggested from the COVID-19 Pandemic. Adolesc. Health Med. Ther. 2022, 13, 45–53. [Google Scholar] [CrossRef] [PubMed]
| Eating Disorder | Treatments (Non-Drug) | Medications |
|---|---|---|
| Anorexia nervosa (AN) | Short-term hospitalization [80,81,82]. | There is no single effective drug approved for the treatment of anorexia nervosa. |
| Home-based therapy is the evidence-based treatment for teenagers with anorexia [83,84]. | Anti-anxiety medications help anorectics to comply with nutritional rehabilitation programs [85,86]. | |
| Nutritional counseling: Nutritional counseling is the main line of nutritional recovery and is designed to teach anorexics about their body’s need for food and essential nutrients [87,88,89]. | Antipsychotics are also recommended in selected AN patients, who are not to eat in spite of ongoing anti-anxiety medications [90,91]. | |
| Individual therapy: Anticipatory behavior therapy, specifically augmentative cognitive–behavioral therapy, contributes to adults [92,93]. | Altered regulation of the hormone leptin may play role in the persistence of anorexia nervosa [94,95]. | |
| Bulimia nervosa (BN) | Psychotherapy: Also called talk therapy, this type of counseling can include cognitive–behavioral therapy, family-based therapy, and interpersonal psychotherapy [96,97,98]. | Antidepressants, such as selective serotonin re-uptake inhibitors (SSRIs) (including Celexa, Lexapro, Prozac, and Zoloft) in combination with psychological therapies, are now a mainstay in bulimia therapy [99,100,101]. |
| Dietitian support and nutritional education: A nutritionist can design a meal plan to help develop healthy eating habits 102,103]. | No medications are approved to treat bulimia nervosa. | |
| Binge eating disorder (BED) | Cognitive–behavioral therapy (CBT): CBT is highly effective in reducing the number of binge eating episodes in individuals [104,105,106]. | Lisdexamfetamine dimesylate (LDX) is currently the only drug approved by the FDA for the treatment of binge eating disorder [73,74,107]. |
| Interpersonal psychotherapy: It can help reduce binge eating triggered by bad communication abilities and relationships [108,109,110]. | Weight loss drugs: Xenical, Contrave, Qsymia, etc. [111,112,113]. | |
| The act of dialectic behavior therapy: It reduces the desire to overeat through studying behavioral skills that can help regulate emotions and perfect relationships with other people [114,115,116]. | Topiramate (Topamax), an anticonvulsant antidepressant [117,118,119,120]. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Feng, B.; Harms, J.; Chen, E.; Gao, P.; Xu, P.; He, Y. Current Discoveries and Future Implications of Eating Disorders. Int. J. Environ. Res. Public Health 2023, 20, 6325. https://doi.org/10.3390/ijerph20146325
Feng B, Harms J, Chen E, Gao P, Xu P, He Y. Current Discoveries and Future Implications of Eating Disorders. International Journal of Environmental Research and Public Health. 2023; 20(14):6325. https://doi.org/10.3390/ijerph20146325
Chicago/Turabian StyleFeng, Bing, Jerney Harms, Emily Chen, Peiyu Gao, Pingwen Xu, and Yanlin He. 2023. "Current Discoveries and Future Implications of Eating Disorders" International Journal of Environmental Research and Public Health 20, no. 14: 6325. https://doi.org/10.3390/ijerph20146325
APA StyleFeng, B., Harms, J., Chen, E., Gao, P., Xu, P., & He, Y. (2023). Current Discoveries and Future Implications of Eating Disorders. International Journal of Environmental Research and Public Health, 20(14), 6325. https://doi.org/10.3390/ijerph20146325






