A Comparison of Objectively Measured Free-Living Physical Behaviour in Adults with and without Lower Limb Amputation
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Equipment
2.3. Participants
2.4. Recruitment
2.5. Procedures
- ActivPAL3 monitor with four nitrile waterproof sleeves and four Tegaderm™ adhesive patches.
- Activity monitor information sheet with verbal, visual and written guidance including a link to an online researcher-led demonstration video showing how to attach and remove the monitor on the non-amputated side.
- Participant activities of daily living diary.
- Participant demographic questionnaire.
- Return address, postage paid, padded envelope identifiable by unique participant ID marked on outer.
2.6. Secondary Data Collection—Comparison Group Participants without LLA
2.7. Matching Procedure
2.8. Primary and Secondary Data Processing (All Data)
- Start time and stop time (date and hours and minutes);
- Total number of steps;
- Time spent sitting/lying, standing and stepping (decimal proportion of one-hour increments);
- Sit-to-stand transitions;
- Energy expenditure (METs/hour);
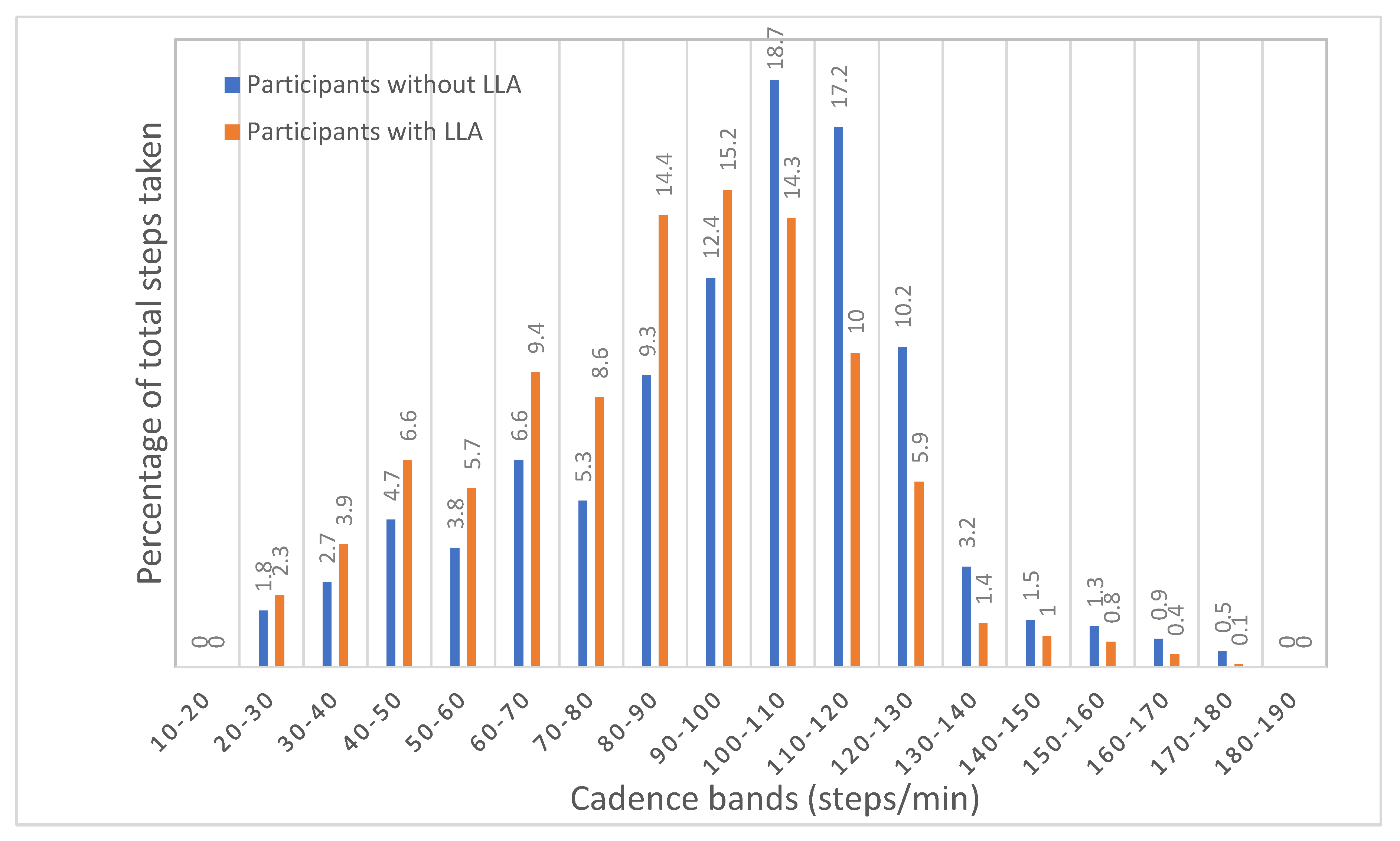
- Total steps within 24 cadence bands in increments of 10 steps·min−1 (i.e., 1–10 steps·min−1, 10–20 steps·min−1, … up to > 240 steps·min−1).
2.9. Statistical Analysis
3. Results
3.1. Participants
3.2. Physical Behaviour of Participants with Lower Limb Absence
3.3. Physical Behaviour of Participants with and without LLA
4. Discussion
4.1. Physical Behaviour of Participants with Lower Limb Absence
4.2. Comparison of Participants with and without Lower Limb Absence
4.3. Strengths, Limitations and Future Work
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Dillingham, T.R.; Pezzin, L.E.; Shore, A.D. Reamputation, mortality, and health care costs among persons with dysvascular lower-limb amputations. Arch. Phys. Med. Rehabil. 2005, 86, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Toumi, A.; Simoneau-Buessinger, É.; Bassement, J.; Barbier, F.; Gillet, C.; Allard, P.; Leteneur, S. Standing posture and balance modalities in unilateral transfemoral and transtibial amputees. J. Bodyw. Mov. Ther. 2021, 27, 634–639. [Google Scholar] [CrossRef] [PubMed]
- Davie-Smith, F.; Coulter, E.; Kennon, B.; Wyke, S.; Paul, L. Factors influencing quality of life following lower limb amputation for peripheral arterial occlusive disease: A systematic review of the literature. Prosthet. Orthot. Int. 2017, 41, 537–547. [Google Scholar] [CrossRef] [PubMed]
- McDonald, C.L.; Westcott-McCoy, S.; Weaver, M.R.; Haagsma, J.; Kartin, D. Global prevalence of traumatic non-fatal limb amputation. Prosthet. Orthot. Int. 2021, 45, 105–114. [Google Scholar] [CrossRef]
- Fortington, L.V.; Geertzen, J.H.B.; van Netten, J.J.; Postema, K.; Rommers, G.M.; Dijkstra, P.U. Short- and long-term mortality rates after a lower limb amputation. Eur. J. Vasc. Endovasc. Surg. 2013, 46, 124–131. [Google Scholar] [CrossRef]
- Luza, L.P.; da Silva, D.R.P.; Ferreira, E.G.; Pires, G.K.W.; Filho, P.J.B.G.; da Silva, R. Physical activity among people with lower limb amputation in Brazil. J. Phys. Act. Health 2021, 18, 1269–1276. [Google Scholar] [CrossRef]
- Sederberg, M.; Tarkhan, A.; Ray, L.S.; Lee, E.S.; Lin, C. Physical activity in adults with an amputation as assessed with a self-reported exercise vital sign. Phys. Med. Rehabil. 2020, 12, 861–869. [Google Scholar] [CrossRef]
- Wong, C.K.; Rissland, M.S.; Madagan, D.M.; Jones, K.N. A scoping review of physical activity in people with lower limb loss: 10,000 steps per day? Phys. Ther. 2021, 101, 1–10. [Google Scholar] [CrossRef]
- Deans, S.; Burns, D.; McGarry, A.; Murray, K.; Mutrie, N. Motivations and barriers to prosthesis users’ participation in physical activity, exercise and sport: A review of the literature. Prosthet. Orthot. Int. 2012, 36, 260–269. [Google Scholar] [CrossRef]
- Bouzas, S.; Molina, A.J.; Fernández-Villa, T.; Miller, K.; Sanchez-Lastra, M.A.; Ayán, C. Effects of exercise on the physical fitness and functionality of people with amputations: Systematic review and meta-analysis. Disabil. Health J. 2021, 14, 100976. [Google Scholar] [CrossRef]
- Schafer, Z.A.; Perry, J.L.; Vanicek, N. A personalised exercise programme for individuals with lower limb amputation reduces falls and improves gait biomechanics: A block randomised controlled trial. Gait Posture 2018, 63, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Department of Health and Social Care. Physical Activity Guidelines: UK Chief Medical Officers’ Report. 2019. Available online: https://www.gov.uk/government/publications/physical-activity-guidelines-uk-chief-medical-officers-report (accessed on 30 March 2023).
- World Health Organisation. Guidelines on physical activity and sedentary behaviour. Br. J. Sport. Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Smith, B.; Kirby, N.; Skinner, B.; Wightman, L. Physical Activity for General Health Benefits in Disabled Adults: Summary of a Rapid Evidence Review for the UK Chief Medical Officers’ Update of the Physical Activity Guidelines; Public Health England: London, UK, 2018.
- Redfield, M.T.; Cagle, J.C.; Hafner, B.J.; Sanders, J.E. Classifying prosthetic use via accelerometery in persons with transtibial amputations. J. Rehabil. Res. Dev. 2013, 50, 1201–1212. [Google Scholar] [CrossRef] [PubMed]
- Rowe, D.A.; McMinn, D.; Peacock, L.; Buis, A.W.P.; Sutherland, R.; Henderson, E.; Hewitt, A. Cadence, energy expenditure, and gait symmetry during music-prompted and self-regulated walking in adults with unilateral transtibial amputation. J. Phys. Act. Health 2014, 11, 320–329. [Google Scholar] [CrossRef]
- Stepien, J.M.; Cavenett, S.; Taylor, L.; Crotty, M. Activity levels among lower-limb amputees: Self-report versus step activity monitor. Arch. Phys. Med. Rehabil. 2007, 88, 896–900. [Google Scholar] [CrossRef]
- Klute, G.K.; Berge, J.S.; Orendurff, M.S.; Williams, R.M.; Czerniecki, J.M. Prosthetic intervention effects on activity of lower-extremity amputees. Arch. Phys. Med. Rehabil. 2006, 87, 717–722. [Google Scholar] [CrossRef]
- Bourke, A.K.; Ihlen, E.A.F.; Helbostad, J.L. Validation of the activPAL3 in free-living and laboratory scenarios for the measurement of physical activity, stepping, and transitions in older adults. J. Meas. Phys. Behav. 2019, 2, 58–65. [Google Scholar] [CrossRef]
- Deans, S.; Kirk, A.; McGarry, A.; Rowe, D. Reliability and criterion-related validity of the activPAL™ accelerometer when measuring physical activity and sedentary behaviour in adults with lower limb absence. J. Meas. Phys. Behav. 2020, 3, 244–252. [Google Scholar] [CrossRef]
- Sellers, C.; Dall, P.; Grant, M.; Stansfield, B. Agreement of the activPAL3 and activPAL for characterising posture and stepping in adults and children. Gait Posture 2016, 48, 209–214. [Google Scholar] [CrossRef]
- Sellers, C.; Dall, P.; Grant, M.; Stansfield, B. Validity and reliability of the activPAL3 for measuring posture and stepping in adults and young people. Gait Posture 2016, 43, 42–47. [Google Scholar] [CrossRef]
- Reid, N.; Eakin, E.; Henwood, T.; Keogh, J.W.L.; Senior, H.E.; Gardiner, P.A.; Healy, G.N. Objectively measured activity patterns among adults in residential aged care. Int. J. Environ. Res. Public Health 2013, 10, 6783–6798. [Google Scholar] [CrossRef] [PubMed]
- Edwardson, C.L.; Winkler, E.A.H.; Bodicoat, D.H.; Yates, T.; Davies, M.J.; Dunstan, D.W.; Healy, G.N. Considerations when using the activPAL monitor in field-based research with adult populations. J. Sport Health Sci. 2017, 6, 162–178. [Google Scholar] [CrossRef] [PubMed]
- Dall, P.M.; McCrorie, P.R.W.; Granat, M.H.; Stansfield, B.W. Step accumulation per minute epoch is not the same as cadence for free-living adults. Med. Sci. Sport. Exerc. 2013, 45, 1995–2001. [Google Scholar] [CrossRef] [PubMed]
- Iveson, A.M.J.; Abaraogu, U.O.; Dall, P.M.; Granat, M.H.; Ellis, B.E. Walking behaviour of individuals with Intermittent Claudication compared to matched controls: Does location matter? Int. J. Environ. Res. Public Health 2023, 20, 5816. [Google Scholar] [CrossRef]
- United National Institute for Prosthetics and Orthotics Development. Limbless Statistics Annual Reports: A Repository for Quantitative Information on the UK Limbless Population Referred for Prosthetics Treatment. Limbless Statistics. 2011. Available online: http://www.limbless-statistics.org/ (accessed on 30 March 2023).
- Miller, M.J.; Jones, J.; Anderson, C.B.; Christiansen, C.L. Factors influencing participation in physical activity after dysvascular amputation: A qualitative meta-synthesis. Disabil. Rehabil. 2019, 41, 3141–3150. [Google Scholar] [CrossRef]
- Rowe, D.A.; Welk, G.J.; Heil, D.P.; Mahar, M.T.; Kemble, C.D.; Calabró, M.A.; Camenisch, K. Stride rate recommendations for moderate-intensity walking. Med. Sci. Sport. Exerc. 2011, 43, 312–318. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Sisson, S.B.; Collova, T.; Lee, S.M.; Swan, P.D. Pedometer-determined step count guidelines for classifying walking intensity in a young ostensibly healthy population. Can. J. Appl. Physiol. 2005, 30, 666–676. [Google Scholar] [CrossRef]
- Tudor-Locke, C.; Rowe, D.A. Using cadence to study free-living ambulatory behaviour. Sport. Med. 2012, 42, 381–398. [Google Scholar] [CrossRef]
- Slaght, J.; Sénéchal, M.; Hrubeniuk, T.J.; Mayo, A.; Bouchard, D.R. Walking cadence to exercise at moderate intensity for adults: A systematic review. J. Sport. Med. 2017, 2017, 4641203. [Google Scholar] [CrossRef]
- Waters, R.L.; Perry, J.; Antonelli, D.; Hislop, H. Energy cost of walking of amputees: The influence of level of amputation. J. Bone Jt. Surg. 1976, 58, 42–46. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; Egerton, T.; Leask, C.; Stamatakis, E. Meta-analysis of the relationship between breaks in sedentary behavior and cardiometabolic health. Obesity 2015, 23, 1800–1810. [Google Scholar] [CrossRef] [PubMed]
- Owen, N.; Healy, G.N.; Matthews, C.E.; Dunstan, D.W. Too much sitting: The population health science of sedentary behaviour. Exerc. Sport Sci. Rev. 2010, 38, 105–113. [Google Scholar] [CrossRef] [PubMed]
- Bohannon, R.W. Daily sit-to-stands performed by adults: A systematic review. J. Phys. Ther. Sci. 2015, 27, 939–942. [Google Scholar] [CrossRef] [PubMed]
- Dall, P.M.; Skelton, D.A.; Dontje, M.L.; Coulter, E.H.; Stewart, S.; Cox, S.R.; Shaw, R.J.; Čukić, I.; Fitzsimons, C.F.; Greig, C.A.; et al. Characteristics of a protocol to collect objective physical activity/sedentary behaviour data in a large study: Seniors USP (Understanding Sedentary Patterns). J. Meas. Phys. Behav. 2018, 1, 26–31. [Google Scholar] [CrossRef] [PubMed]
- Buis, A.W.P.; Dumbleton, T.; Murray, K.D.; McHugh, B.F.; McKay, G.; Sexton, S. Measuring the daily stepping activity of people with transtibial amputation using the activPAL™ activity monitor. J. Prosthet. Orthot. 2014, 26, 43–47. [Google Scholar] [CrossRef]

| Characteristic | All (N = 57) | Male (n = 40) | Female (n = 17) | |
|---|---|---|---|---|
| Age (years) 1 | 57.39 ± 12.09 | 59.40 ± 10.85 | 52.65 ± 13.82 | |
| Height (m) 1 | 1.73 ± 0.10 | 1.77 ± 0.07 | 1.63 ± 0.07 | |
| Body mass (kg) 1 | 81.48 ± 16.99 | 87.58 ± 14.67 | 67.14 ± 13.17 | |
| Body mass index (kg/m2) 1 | 27.14 ± 4.54 | 27.94 ± 4.26 | 25.27 ± 4.76 | |
| Level | Transtibial | 40 | 27 | 13 |
| Transfemoral | 17 | 13 | 4 | |
| Side | Right | 29 | 22 | 7 |
| Left | 28 | 18 | 10 | |
| Cause of limb absence | Trauma | 28 | 22 | 6 |
| Cancer | 8 | 3 | 5 | |
| Infection | 8 | 6 | 2 | |
| Congenital | 5 | 3 | 2 | |
| PAD | 7 | 5 | 2 | |
| Thrombosis | 1 | 1 | 0 | |
| Employment status | Retired | 28 | 22 | 6 |
| Full-time | 18 | 13 | 5 | |
| Part-time | 9 | 4 | 5 | |
| Unemployed | 2 | 1 | 1 | |
| Wheelchair user | No | 40 | 31 | 9 |
| Yes | 17 | 9 | 8 | |
| Measurement | All (N = 57) | Male (n = 40) | Female (n = 17) |
|---|---|---|---|
| Age (years) 1 | 57.86 ± 14.10 | 59.92 ± 13.48 | 53.00 ± 14.73 |
| Height (metres) 1 | 1.72 ± 0.10 | 1.77 ± 0.07 | 1.61 ± 0.06 |
| Body mass (kilograms) 1 | 75.94 ± 10.99 | 79.61 ± 10.14 | 67.30 ± 7.69 |
| Body mass index (kg/m2) 1 | 25.74 ± 3.22 | 25.80 ± 3.42 | 25.58 ± 2.79 |
| Variable | All (N = 57) | Male (n = 40) | Female (n = 17) |
|---|---|---|---|
| Time awake (h) | 14.88 ± 0.98 | 14.98 ± 0.98 | 14.66 ± 0.95 |
| Time awake (%) | 62.02 ± 4.07 | 62.42 ± 4.08 | 61.07 ± 3.98 |
| Time asleep (h) | 9.12 ± 0.98 | 9.02 ± 0.98 | 9.34 ± 0.95 |
| Time asleep (%) | 37.98 ± 4.07 | 37.57 ± 4.09 | 38.93 ± 3.98 |
| Time sitting/lying (h) | 10.44 ± 10.99 | 10.61 ± 1.91 | 10.03 ± 1.58 |
| Time sitting/lying (%) | 70.45 ± 12.92 | 71.35 ± 14.28 | 68.35 ± 8.98 |
| Time standing (h) | 3.19 ± 1.43 | 3.10 ± 1.58 | 3.42 ± 1.01 |
| Time standing (%) | 21.24 ± 8.91 | 20.37 ± 9.66 | 23.30 ± 6.65 |
| Time stepping (h) | 1.25 ± 0.82 | 1.27 ± 0.91 | 1.21 ± 0.59 |
| Time stepping (%) | 8.31 ± 5.13 | 8.29 ± 5.56 | 8.35 ± 4.11 |
| Daily step count | 5569 ± 4083 | 5677 ± 4535 | 5316 ± 2852 |
| Number of daily sit-to-stand transitions | 57 ± 20.00 | 54 ± 20.00 | 65 ± 20.00 |
| Daily energy expenditure (METs/h) 1 | 7.32 ± 2.39 | 7.46 ± 2.70 | 6.97 ± 1.45 |
| Activity Variable | Transtibial (n = 40) | Transfemoral (n = 17) |
|---|---|---|
| Time awake (h) | 14.91 ± 0.98 | 14.82 ± 0.99 |
| Time awake (%) | 62.12 ± 4.10 | 61.77 ± 4.12 |
| Time asleep (h) | 9.09 ± 0.98 | 9.17 ± 0.99 |
| Time asleep (%) | 37.87 ± 4.09 | 38.23 ± 4.12 |
| Time sitting/lying (h) | 10.25 ± 1.92 | 10.90 ± 1.55 |
| Time sitting/lying (%) | 69.06 ± 13.60 | 73.72 ± 10.83 |
| Time standing (h) | 3.32 ± 1.49 | 2.89 ± 1.29 |
| Time standing (%) | 22.06 ± 9.21 | 19.32 ± 8.11 |
| Time stepping (h) | 1.34 ± 0.90 | 1.04 ± 0.58 |
| Time stepping (%) | 8.88 ± 5.56 | 6.95 ± 3.74 |
| Daily step count | 6085 ± 4449 | 4356 ± 2809 |
| Number of daily sit-to-stand transitions | 60 ± 21 | 50 ± 15 |
| Daily energy expenditure (METs/h) 1 | 7.56 ± 2.56 | 6.75 ± 1.89 |
| Variable | Trauma (n = 28) | Cancer (n = 8) | Infection (n = 8) | Congenital (n = 5) | Circulatory (n = 8) 1 |
|---|---|---|---|---|---|
| Time awake (h) | 14.84 ± 0.97 | 15.47 ± 0.76 | 14.70 ± 0.84 | 14.65 ± 1.54 | 14.78 ± 0.96 |
| Time awake (%) | 61.84 ± 4.03 | 64.47 ± 3.15 | 61.25 ± 3.48 | 61.05 ± 6.41 | 61.57 ± 3.98 |
| Time asleep (h) | 9.16 ± 0.97 | 8.53 ± 0.76 | 9.30 ± 0.84 | 9.35 ± 1.54 | 9.22 ± 0.96 |
| Time asleep (%) | 38.16 ± 4.06 | 35.53 ± 3.15 | 38.75 ± 3.48 | 38.95 ± 6.41 | 38.43 ± 3.98 |
| Time sitting/lying (h) | 9.75 ± 1.74 | 10.59 ± 1.95 | 10.99 ± 1.46 | 10.59 ± 1.61 | 12.07 ± 1.48 |
| Time sitting/lying (%) | 66.07 ± 12.87 | 68.63 ± 13.15 | 74.64 ± 7.53 | 72.87 ± 13.13 | 81.89 ± 10.71 |
| Time standing (h) | 3.57 ± 1.37 | 3.47 ± 1.47 | 2.65 ± 0.74 | 2.94 ± 1.96 | 2.28 ± 1.52 |
| Time standing (%) | 23.88 ± 8.39 | 22.28 ± 9.01 | 18.17 ± 5.51 | 19.35 ± 11.32 | 15.24 ± 9.79 |
| Time stepping (h) | 1.52 ± 0.92 | 1.41 ± 0.73 | 1.05 ± 0.50 | 1.12 ± 0.50 | 0.42 ± 0.21 |
| Time stepping (%) | 10.05 ± 5.56 | 9.09 ± 4.60 | 7.19 ± 3.44 | 7.78 ± 3.84 | 2.87 ± 1.45 |
| Daily step count | 6817 ±4607 | 6376 ±3583 | 4536 ±2552 | 5449 ±2790 | 1502 ± 778 |
| Number of daily sit-to-stand transitions | 61 ± 20 | 58 ± 20 | 54 ± 13 | 61 ± 26 | 46 ± 22 |
| Daily energy expenditure (METs/h) 2 | 7.72 ± 2.80 | 8.51 ± 1.87 | 6.64 ± 1.47 | 7.02 ± 1.89 | 5.59 ± 1.26 |
| Variable | Statistic | LLA N = 57 | CG N = 57 | Percentage Difference % LLA vs. CG 2 | df | t | p |
|---|---|---|---|---|---|---|---|
| Time sitting/lying (h) | M | 11.73 | 10.41 | 13 | 56 | −3.42 | <0.001 * |
| SD | 1.99 | 1.38 | |||||
| Time standing (h) | M | 3.07 | 3.98 | 23 | 56 | 2.29 | <0.001 * |
| SD | 1.38 | 1.11 | |||||
| Time stepping (h) | M | 1.20 | 1.75 | 31 | 56 | 3.31 | <0.001 * |
| SD | 0.75 | 0.49 | |||||
| Step count | M | 5340 | 8715 | 39 | 56 | 3.22 | <0.001 * |
| SD | 3613 | 2639 | |||||
| Sit-to-stand transitions | M | 54 | 48 | 12 | 56 | 1.80 | 0.107 |
| SD | 20 | 11 | |||||
| Energy expenditure (MET/h) 1 | M | 22.53 | 24.13 | 20 | 56 | 2.08 | <0.001 * |
| SD | 1.66 | 1.21 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Deans, S.; Kirk, A.; McGarry, A.; Rowe, D.A.; Dall, P.M. A Comparison of Objectively Measured Free-Living Physical Behaviour in Adults with and without Lower Limb Amputation. Int. J. Environ. Res. Public Health 2023, 20, 6198. https://doi.org/10.3390/ijerph20136198
Deans S, Kirk A, McGarry A, Rowe DA, Dall PM. A Comparison of Objectively Measured Free-Living Physical Behaviour in Adults with and without Lower Limb Amputation. International Journal of Environmental Research and Public Health. 2023; 20(13):6198. https://doi.org/10.3390/ijerph20136198
Chicago/Turabian StyleDeans, Sarah, Alison Kirk, Anthony McGarry, David A. Rowe, and Philippa M. Dall. 2023. "A Comparison of Objectively Measured Free-Living Physical Behaviour in Adults with and without Lower Limb Amputation" International Journal of Environmental Research and Public Health 20, no. 13: 6198. https://doi.org/10.3390/ijerph20136198
APA StyleDeans, S., Kirk, A., McGarry, A., Rowe, D. A., & Dall, P. M. (2023). A Comparison of Objectively Measured Free-Living Physical Behaviour in Adults with and without Lower Limb Amputation. International Journal of Environmental Research and Public Health, 20(13), 6198. https://doi.org/10.3390/ijerph20136198







