Development and Validation of Protocol Based on Brazilian Dietary Guidelines for Adults with Diabetes Mellitus Who Attended Primary Health Care
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol Format Definition
2.2. Definition of the Instrument for the Assessment of Food Consumption Markers
2.3. Extracting Recommendations from Brazilian Dietary Guidelines
2.4. Evidence Systematization on the Food and Nutrition Needs of Adults with DM
2.5. Development of Dietary Guidelines Recommendations for Adults with DM
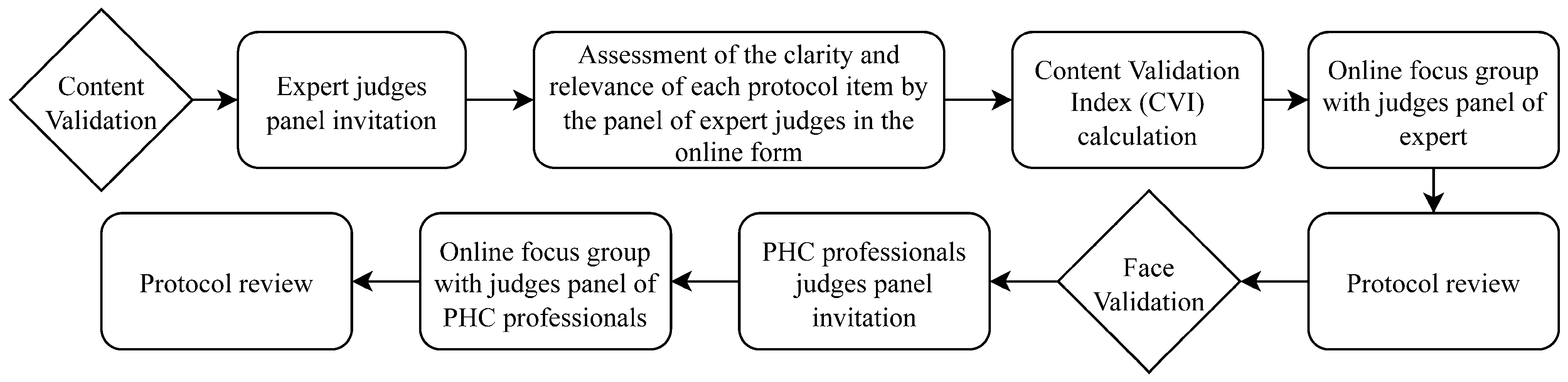
2.6. Validation of the Protocol
2.6.1. Content Validation
2.6.2. Face Validation
2.7. Data Analysis
2.8. Ethics Aspects
3. Results
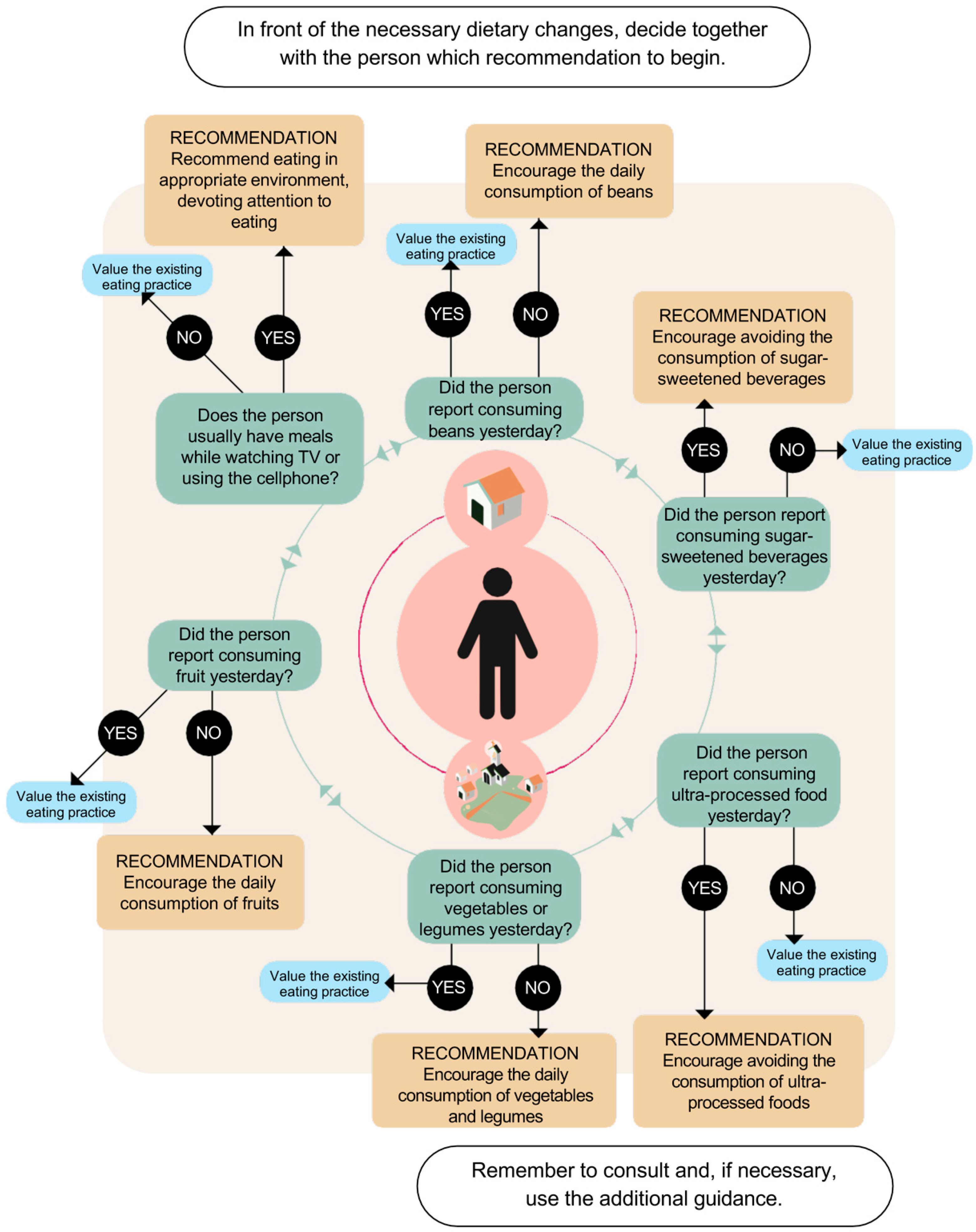
3.1. Development of the Protocol
- Recommendation 1—Encourage the daily consumption of beans.
- Recommendation 2—Advise the avoidance of sugar-sweetened beverages.
- Recommendation 3—Advise the avoidance of ultra-processed foods.
- Recommendation 4—Advise the daily consumption of vegetables.
- Recommendation 5—Encourage the daily consumption of fruits.
- Recommendation 6—Encourage the person to eat in appropriate environments and with attention.
3.2. Content Validation
3.3. Face Validation
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| PHC | Primary Health Care |
| DM | Diabetes Mellitus |
| DGBP | Dietary Guidelines for Brazilian Population |
| FHS | Family Health Strategy |
| SUS | Brazilian Unified Health System (In Portuguese: Sistema Único De Saúde) |
| CVI | Content Validity Index |
| VIGITEL | Surveillance System for Risk and Protection Factors for Chronic Diseases by Telephone Survey (In Portuguese: Sistema de Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico) |
References
- Alberti, K.G.; Zimmet, P.Z. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: Diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef]
- International-Diabetes-Federation. IDF Diabetes Atlas, 10th ed.; International Diabetes Federation: Brussels, Belgium, 2021. [Google Scholar]
- Facilitating Behavior Change and Well-Being to Improve Health Outcomes: Standards of Medical Care in Diabetes—2020. Diabetes Care 2020, 43, S48–S65. [CrossRef] [PubMed]
- Ministério da Saúde do Brasil. Estratégias Para o Cuidado da Pessoa com Doença Crônica: Diabetes Mellitus: Cadernos de Atenção Básica; Ministério da Saúde do Brasil: Brasília, Brazil, 2013; ISBN 9788533420595.
- Ministério da Saúde do Brasil. Guia Alimentar para a População Brasileira, 2nd ed.; Ministério da Saúde do Brasil: Brasília, Brazil, 2014.
- Monteiro, C.A.; Cannon, G.; Lawrence, M.; Louzada, M.L.C.; Machado, P.P. Ultra-Processed Foods, Diet Quality, and Health Using the NOVA Classification System; FAO: Rome, Italy, 2019; pp. 6–12. [Google Scholar]
- Louzada, M.L.D.C.; Tramontt, C.R.; de Jesus, J.G.L.; Rauber, F.; Hochberg, J.R.B.; Santos, T.S.S.; Jaime, P.C. Developing a protocol based on the Brazilian Dietary Guidelines for individual dietary advice in the primary healthcare: Theoretical and methodological bases. Fam. Med. Community Health 2022, 10, e001276. [Google Scholar] [CrossRef] [PubMed]
- Sociedade Brasileira de Diabetes. Diretrizes da Sociedade Brasileira de Diabetes (SBD): 2019–2020; Sociedade Brasileira de Diabetes: São Paulo, Brazil, 2019. [Google Scholar]
- Brouwers, M.C.; Kerkvliet, K.; Spithof, K. The AGREE Reporting Checklist: A Tool to Improve Reporting of Clinical Practice Guidelines. BMJ 2016, 352, i1152. [Google Scholar] [CrossRef] [PubMed]
- Berg, S. Snowball sampling. In Encyclopedia of Statistical Sciences; John Wiley and Sons, Inc.: New York, NY, USA, 1988; Volume 8, pp. 528–532. [Google Scholar]
- Bardin, L. Content Analysis, 5th ed.; Almedina Brasil: São Paulo, Brazil, 2008. [Google Scholar]
- Streiner, D.L.; Norman, G.R.; Cairney, J. Health Measurement Scales: A Practical Guide to Their Development and Use, 5th ed.; Oxford University Press: Oxford, UK, 2015; p. 399. [Google Scholar]
- Rubio, D.M.; Berg-Weger, M.; Tebb, S.S.; Lee, E.S.; Rauch, S. Objectifying content validity: Conducting a content validity study in social work research. Soc. Work Res. 2003, 27, 94–104. [Google Scholar] [CrossRef]
- Ministério da Saúde do Brasil. Formulário de Marcadores de Consumo Alimentar na Atenção Básica; Ministério da Saúde do Brasil: Brasília, Brazil, 2015.
- Ministério da Saúde do Brasil. Orientações para Avaliação de Marcadores de Consumo Alimentar na Atenção Básica; Ministério da Saúde do Brasil: Brasília, Brazil, 2015.
- Ministério da Saúde do Brasil. Orientação Alimentar de Pessoas Adultas com Diabetes Mellitus; Ministério da Saúde do Brasil: Brasília, Brazil, 2022.
- Jesus, J.G.L.; Tramontt, C.R.; Santos, T.S.S.; Rauber, F.; Louzada, M.L.C.; Jaime, P.C. Dietary guidelines for the elderly in Primary Health Care: Development and validation of a protocol based on the Food Guide for the Brazilian Population. Rev. Bras. Geriatr. Gerontol. 2021, 24, e210157. [Google Scholar] [CrossRef]
- Ministério da Saúde do Brasil. Política Nacional de Atenção Básica PNAB; Portaria No 2436, de 21 de setembro de 2017; Ministério da Saúde do Brasil: Brasília, Brazil, 2017.
- Ministério da Saúde do Brasil. Matriz para Organização dos Cuidados em Alimentação e Nutrição na Atenção Primária à Saúde, 1st ed.; Ministério da Saúde do Brasil: Brasília, Brazil, 2022.
- Baldissera, R.; Issler, R.M.S.; Giugliani, E.R.J. Efetividade da Estratégia Nacional para Alimentação Complementar Saudável na melhoria da alimentação complementar de lactentes em um município do Sul do Brasil. Cad. Saúde Pública 2016, 32, e0010131. [Google Scholar] [CrossRef] [PubMed]
- Bortolini, G.A.; de Oliveira, T.F.V.; da Silva, S.A.; Santin, R.D.C.; de Medeiros, O.L.; Spaniol, A.M.; Pires, A.C.L.; Alves, M.F.M.; Faller, L.D.A. Feeding and nutrition efforts in the context of primary healthcare in Brazil. Pan Am. J. Public Health 2020, 44, e39. [Google Scholar] [CrossRef]
- Sociedade Brasileira de Diabetes. Manual de Contagem de Carboidratos para Pessoas com Diabetes; Sociedade Brasileira de Diabetes: São Paulo, Brazil, 2016. [Google Scholar]
- Moradi, S.; Entezari, M.H.; Mohammadi, H.; Jayedi, A.; Lazaridi, A.-V.; Kermani, M.A.H.; Miraghajani, M. Ultra-processed food consumption and adult obesity risk: A systematic review and dose-response meta-analysis. Crit. Rev. Food Sci. Nutr. 2021, 63, 249–260. [Google Scholar] [CrossRef] [PubMed]
- Pagliai, G.; Dinu, M.; Madarena, M.P.; Bonaccio, M.; Iacoviello, L.; Sofi, F. Consumption of ultra-processed foods and health status: A systematic review and meta-Analysis. Brit. J. Nutr. 2021, 125, 308–318. [Google Scholar] [CrossRef] [PubMed]
- Delpino, F.M.; Figueiredo, L.M.; Bielemann, R.M.; da Silva, B.G.C.; dos Santos, F.S.; Mintem, G.C.; Flores, T.R.; Arcêncio, R.A.; Nunes, B.P. Ultra-processed food and risk of type 2 diabetes: A systematic review and meta-analysis of longitudinal studies. Int. J. Epidemiol. 2022, 51, 1120–1141. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Fan, Y.; Zhang, X.; Hou, W.; Tang, Z. Fruit and vegetable intake and risk of type 2 diabetes mellitus: Meta-analysis of prospective cohort studies. BMJ Open 2014, 4, e005497. [Google Scholar] [CrossRef] [PubMed]
- Tabesh, M.; Hariri, M.; Askari, G.; Ghiasvand, R.; Tabesh, M.; Heydari, A.; Darvishi, L.; Khorvash, F. The Relationship Between Vegetables and Fruits Intake and Glycosylated Hemoglobin Values, Lipids Profiles and Nitrogen Status in Type II Inactive Diabetic Patients. Int. J. Prev. Med. 2013, 4, S63–S67. [Google Scholar] [PubMed]
- Browne, J.L.; Ventura, A.; Mosely, K.; Speight, J. ‘I call it the blame and shame disease’: A qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open 2013, 3, e003384. [Google Scholar] [CrossRef] [PubMed]
- Holmes-Truscott, E.; Ventura, A.D.; Thuraisingam, S.; Pouwer, F.; Speight, J. Psychosocial moderators of the impact of diabetes stigma: Results from the second diabetes miles—Australia (MILES-2) Study. Diabetes Care 2020, 43, 2651–2659. [Google Scholar] [CrossRef] [PubMed]
- Dickinson, J.K. The experience of diabetes-related language in diabetes care. Diabetes Spectr. 2018, 31, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Speight, J.; Skinner, T.C.; Dunning, T.; Black, T.; Kilov, G.; Lee, C.; Scibilia, R.; Johnson, G. Our language matters: Improving communication with and about people with diabetes. A position statement by Diabetes Australia. Diabetes Res. Clin. Pract. 2021, 173, e108655. [Google Scholar] [CrossRef]
- Dickinson, J.K.; Guzman, S.J.; Maryniuk, M.D.; O’brian, C.A.; Kadohiro, J.K.; Jackson, R.A.; D’hondt, N.; Montgomery, B.; Close, K.L.; Funnell, M.M. The use of language in diabetes care and education. Diabetes Care 2017, 40, 1790–1799. [Google Scholar] [CrossRef] [PubMed]
- Polonsky, W.H.; Capehorn, M.; Belton, A.; Down, S.; Alzaid, A.; Gamerman, V.; Nagel, F.; Lee, J.; Edelman, S. Physician–patient communication at diagnosis of type 2 diabetes and its links to patient outcomes: New results from the global IntroDia® study. Diabetes Res. Clin. Pract. 2017, 127, 265–274. [Google Scholar] [CrossRef] [PubMed]
| Content Validity Index (CVI) | |||
|---|---|---|---|
| Component | Clarity (Min-Max.) | Relevance (Min-Max.) | Average CVI |
| Introductory Text | 1.00 | 0.94 | 0.97 |
| How to use the protocol? | 1.00 | 1.00 | 1.00 |
| Flowchart | 1.00 | 1.00 | 1.00 |
| Recommendation 1—Consumption of beans | |||
| Guideline | 0.94 | 0.94 | 0.94 |
| Suggestion for variations | 1.00 | 1.00 | 1.00 |
| Reason | 1.00 | 1.00 | 1.00 |
| Obstacles | 1.00 | 1.00 | 1.00 |
| Recommendation 2—Sugar-sweetened beverages | |||
| Guideline | 1.00 | 1.00 | 1.00 |
| Suggestion for variations | 1.00 | 1.00 | 1.00 |
| Reason | 1.00 | 1.00 | 1.00 |
| Obstacles | 1.00 | 1.00 | 1.00 |
| Recommendation 3—Ultra-processed food | |||
| Guideline | 1.00 | 1.00 | 1.00 |
| Suggestion for variations | 0.94 | 0.94 | 0.94 |
| Reason | 1.00 | 1.00 | 1.00 |
| Obstacles | 1.00 | 1.00 | 1.00 |
| Recommendation 4—Legumes and vegetables | |||
| Guideline | 1.00 | 1.00 | 1.00 |
| Suggestion for variations | 0.94 | 0.94 | 0.94 |
| Reason | 1.00 | 1.00 | 1.00 |
| Obstacles and strategies | 1.00 | 1.00 | 1.00 |
| Recommendation 5—Fruits | |||
| Guideline | 1.00 | 1.00 | 1.00 |
| Suggestion for variations | 1.00 | 1.00 | 1.00 |
| Reason | 1.00 | 1.00 | 1.00 |
| Obstacles and strategies | 1.00 | 1.00 | 1.00 |
| Recommendation 6—Appropriate environments | |||
| Guideline | 1.00 | 1.00 | 1.00 |
| Reason | 1.00 | 1.00 | 1.00 |
| Strategies | 1.00 | 1.00 | 1.00 |
| Final messages | |||
| Additional guidance | 0.89 | 0.94 | 0.92 |
| Valuing the practice | 1.00 | 1.00 | 1.00 |
| Total-Content Validation Index (tCVI) | 0.99 | ||
| Recommendations | Emerging Topics | Sub-Topic Supported the Reformulation |
|---|---|---|
| Introduction | Contextualization | -Emphasize the high prevalence of overweight and obesity in the Brazilian population with diabetes according to a recent national Brazilian survey (in Portuguese: Sistema de Vigilância de Fatores de Risco e Proteção para Doenças Crônicas por Inquérito Telefônico (VIGITEL)). |
| PHC flow care | -Highlight the importance of the lines of care, which trace the individual care flow, and reinforce the Health Care Network available in the care of the person with diabetes. | |
| Diabetes Complications | -Include the risk reduction in DM complications, in addition to only glycemic management, as an advantage of the protocol implementation. | |
| Carbohydrate counting | -Inclusion request, considering the PHC reality in the orientation of persons who perform or have doubts about carbohydrate counting and its relationship with the use of insulin. | |
| How to use the protocol? | Food consumption markers form | -Assistance in locating food consumption markers within the PHC Information System. |
| People’s autonomy in their care process | -Valuing and strengthening adequate and healthy practices that a person with DM already has. | |
| Diabetes stigma | -Relevance of health care professionals in preventing DM stigma when treating people with DM. | |
| Equity | -Strengthening feasible guidelines and being attentive to cultural and socioeconomic issues. | |
| Flowchart | -Reinforcing that the process must be collaborative, between the professional and the person, from the decision of which dietary recommendation begins. | |
| Sugar-sweetened beverages | Diet, light, and zero | -Insertion of examples, considering the relevance of strengthening that such foods are ultra-processed, and their consumption is not recommended. |
| Consumption | -Encouraging the gradual substitution of chocolate-sugar beverages to cocoa powder. | |
| Foods | -Discouraging the consumption of sweeteners, due to their classification as ultra-processed food. | |
| Ultra-processed food | Foods | -Expanding examples of ultra-processed food. |
| Foods | -Expanding examples of different types of cereal according to their carbohydrate content and their association with other foods and culinary preparations. | |
| Consumption | -Reinforcing the non-stimulating of dessert consumption, but for those with this habit, recommended to substitute ultra-processed food for unprocessed or minimally processed options. | |
| Consumption | -Reinforcing the lower impact of consumption of sweet culinary preparations right after meals on blood glucose, rather than their isolated consumption. -Stimulating the avoidance or reduction in the consumption of ultra-processed sweet foods. | |
| Consumption | -Including vegetarian culinary preparations as substitutes for ultra-processed food, considering the different contexts and food preferences. | |
| Consumption | -Reinforcing the importance of analyzing food labels for adequate and healthy food choices. | |
| Foods | -Expanding examples of unprocessed food as substitutes for ultra-processed food. | |
| Legumes and vegetables | Regional foods | -Expanding examples of regional foods. |
| Consumption | -Reinforcing the consumption of foods that grow under the ground (roots) in the context of healthy eating. | |
| Consumption | -Demystifying the impossibility of consuming two foods from the root and tubercle group in the same meal, however, recommend reducing the portion of each of these foods. | |
| Food access | -Reinforcing avoiding eating at places with a predominance of ultra-processed food. | |
| Fruits | Glycemia management | -Including examples of food rich in dietary fiber to combine with fruits for better glycemic control. |
| Consumption | -Including practical strategies to stimulate fruit intake daily. | |
| Appropriate environments | Equity | -Considering the different socioeconomic realities with a view to providing feasible guidelines. |
| Final messages | Fad Diets | -Inclusion of the impacts and damages of long periods of fasting on blood glucose. |
| Low-carb Diets | -Reinforcing the low adherence to a low-carb diet in long-term periods and the low high-quality evidence of their safety. | |
| Glycemic management | -Reinforcing the strategy of associating different food groups in the same meal to promote a better glycemic control. | |
| Food ingredients | -Expanding the regional food examples. | |
| Hypoglycemia episodes | -Reinforcing the investigation of possible causes for the hypoglycemia episodes. -Reinforcement of the importance of maintaining medication with adequate dosages and meal planning. -Encouraging carbohydrate counting as a strategy to decrease the risk of hypoglycemia. | |
| Hypoglycemia episodes | -Insertion of guidelines for the management of hypoglycemic episodes. |
| Recommendations | Emerging Topics | Sub-Topic That Supported the Reformulation |
|---|---|---|
| How to use the protocol | The autonomy of people with DM in their care process | -Reinforce valorization and encourage active participation throughout their care process. |
| Food ingredients | -Encouraging and providing strategies for people with DM to access unprocessed and minimally processed foods, regardless of socioeconomic status. | |
| Ultra-processed foods | Culinary preparations | -Expanding the examples of regional culinary preparations to replace ultra-processed foods. -Reinforcing the inclusion of protein-rich foods in culinary preparations, to improve glycemic control. |
| Final Messages | Fads diets | -Elucidation of the impact and potential harm of restrictive diets for people with DM. |
| Food production and access | -Encouraging people with DM to make a vegetable garden in their homes or communities. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Araújo, M.M.; Pizato, N.; Rodrigues, L.S.; de Andrade, L.S.; de Moraes, V.D.; de Carvalho, K.M.B.; Dutra, E.S.; Botelho, P.B.; Gonçalves, V.S.S. Development and Validation of Protocol Based on Brazilian Dietary Guidelines for Adults with Diabetes Mellitus Who Attended Primary Health Care. Int. J. Environ. Res. Public Health 2023, 20, 5784. https://doi.org/10.3390/ijerph20105784
Araújo MM, Pizato N, Rodrigues LS, de Andrade LS, de Moraes VD, de Carvalho KMB, Dutra ES, Botelho PB, Gonçalves VSS. Development and Validation of Protocol Based on Brazilian Dietary Guidelines for Adults with Diabetes Mellitus Who Attended Primary Health Care. International Journal of Environmental Research and Public Health. 2023; 20(10):5784. https://doi.org/10.3390/ijerph20105784
Chicago/Turabian StyleAraújo, Maísa Miranda, Nathalia Pizato, Lorrany Santos Rodrigues, Laila Santos de Andrade, Verena Duarte de Moraes, Kênia Mara Baiocchi de Carvalho, Eliane Said Dutra, Patrícia Borges Botelho, and Vivian Siqueira Santos Gonçalves. 2023. "Development and Validation of Protocol Based on Brazilian Dietary Guidelines for Adults with Diabetes Mellitus Who Attended Primary Health Care" International Journal of Environmental Research and Public Health 20, no. 10: 5784. https://doi.org/10.3390/ijerph20105784
APA StyleAraújo, M. M., Pizato, N., Rodrigues, L. S., de Andrade, L. S., de Moraes, V. D., de Carvalho, K. M. B., Dutra, E. S., Botelho, P. B., & Gonçalves, V. S. S. (2023). Development and Validation of Protocol Based on Brazilian Dietary Guidelines for Adults with Diabetes Mellitus Who Attended Primary Health Care. International Journal of Environmental Research and Public Health, 20(10), 5784. https://doi.org/10.3390/ijerph20105784








