Feasibility and First Experiences from an Online Kidney School for Patients with Chronic Kidney Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting and Participants
2.2. Data Collection
2.2.1. Assessment of Feasibility
2.2.2. Qualitative Data Collection
2.2.3. Quantitative Data Collection
2.2.4. Kidney Knowledge Questionnaire
2.2.5. Telehealth Usability Questionnaire
2.3. Statistics
3. Results
3.1. Feasibility
3.2. Qualitative Results
3.2.1. Over-Arching Theme: Evolution of the Online Kidney School over Time
“It’s not that they have to be able to answer specific questions. They have to have an understanding of what kidney disease means and what treatment options there are … generally speaking”.(Participant no. 3)
3.2.2. Sub-Themes
Concerns and Perceived Barriers
“…I can see it as a disadvantage, if we find out that they (ed. Participants) don’t get just as much out of being online, as they do when they are physically present”.(Participant no. 1)
“And the oldest we’ve had online, he was eighty-nine and he was just so; ”well, I’ll manage this!” and then he managed to get online, though we had neither camera nor sound from him and he wasn’t able to ask any questions, but he could take part … like, he could take part …He could hear XX’s lesson and he told (ed. us) that he got a lot out of it. It wasn’t a problem for him”.(Participant no. 1)
“That was a bigger worry (..), in relation to whether they (ed. Participants) were able to connect. On the other hand, there were just many things that happened at once because so much was converted to online and there were many ways of doing things, so the possibility was there. But of course, what system should we choose? And was it available to them at home? And how many of them (ed. Participants) even had the opportunity to get onto the system from their home?”(Participant no. 4)
“You don’t have quite the same sense of who you’re speaking to and how it’s being received… Not the same as sitting in a room with them face-to-face...”(Participant no. 3)
Facilitators
“And we’ve had some classes that were really small because people backed out anyway, until I realised that if I call them and say ‘now I have a class, are you on?’ and they said ‘nah, I don’t really know’ and then I could take care of it there and then and say ‘Listen here, I think you should try. We have good experience with it and (..) if you don’t get through, well then, we’ll find another solution for you’ and then it was like they were kind of ’well, OK then, I’ll try”.(Participant no. 1)
“And some of what we found out, was that, it was good to hold some short breaks (…) and also ask, (..) ‘What do you think about this?’ To kind of get people included because otherwise you’ll just sort of sit there at home in your living room and hide and maybe not participate in the same way as you would have done. (…) So, we’re getting smarter each time we hold it”.(Participant no. 1)
”You got a bit of a surprise when you called them and afterwards (ed., found) that there were actually a lot who were interested in it. (…). But it was an eye opener when you called around and found out that (..) some simply said that ‘I have a relative that can help’”.(Participant no. 4)
3.2.3. Benefits and Future Possibilities for the Kidney School
“Yeah, so it’s actually opened up for something new, because most often, it’s a wife or a husband who joins in. Now it was other relatives, you know, like children or the like, that logged on from other places”.(Participant no. 4)
“We could be more flexible as well, also if there is a patient who doesn’t have the opportunity to come in but would like to have it online, then you can hook them up to the physical, can’t you?”(Participant no. 2)
3.3. Quantitative Results
3.3.1. Kidney Knowledge Questionnaire
3.3.2. Telehealth Usability Questionnaire
3.4. Merging Interpretation of Results
3.4.1. Kidney Knowledge Questionnaire and Qualitative Results
3.4.2. Telehealth Usability Questionnaire and Qualitative Results
3.4.3. Benefits and Future Possibilities for the Kidney School
4. Discussion
4.1. Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Interview Guide for the Focus Group Discussion
| Why did you choose to reorganise the kidney school to an online kidney school? What considerations did you take into account in connection with re-organising the lessons? |
How have you experienced teaching via a screen? How is that type of teaching different from teaching face-to-face? |
How have you experienced your own development in relation to carrying out the teaching online? What advantages and disadvantages did you experience with use of an online kidney school? |
What do you prefer and why? With any comments for suggestions for improvements. Is this something you would recommend to others? |
How did the technical side of things function in the online kidney school? We have read in the literature that more opposition is experienced among healthcare professionals than patients to the use of technology. Do you recognise this phenomenon? What would you prefer? And why?
|
Appendix B. Kidney Knowledge Questionnaire
- What is the name of the treatment option that rinses waste material from your blood?
- (a)
- Catalyst
- (b)
- Dialysis
- (c)
- Osmosis
- (d)
- Diuresis
- Which answer regarding MMU (maximal medical uraemic treatment) is correct?
- (a)
- Dialysis treatment starts only when there is total kidney failure
- (b)
- Treatment focuses on quality of life rather than length of life
- (c)
- Is largely a treatment for younger people without previous illness
- (d)
- Means that one does not receive any further treatment
- Which answer relating to peritoneal dialysis is correct?
- (a)
- Peritoneal dialysis is carried out at the hospital
- (b)
- Dialysis is performed via the peritoneum
- (c)
- Carried out in daytime only
- (d)
- The peritoneal dialysis catheter can be removed
- Which haemodialysis access method does not exist?
- (a)
- Graft
- (b)
- Tunnelled catheter
- (c)
- Fistula
- (d)
- Tube in the peritoneum
- Which answer regarding home haemodialysis is correct?
- (a)
- The teaching program takes place at home
- (b)
- After 2 weeks one automatically starts dialysis at home
- (c)
- We recommend a minimum of 15 h dialysis weekly
- (d)
- The more dialysis I receive, the more medicine I have to take
- Which answer regarding haemodialysis at the hospital is correct?
- (a)
- Carried out 5 times a week
- (b)
- Only during daytime
- (c)
- You have a dialysis nurse who is assigned to you
- (d)
- Dialysis takes at least 4 h
- Which symptom is not a typical uraemic one (waste build-up symptom)?
- (a)
- Tiredness
- (b)
- Tummy sickness
- (c)
- Itching skin
- (d)
- Pain over the kidneys
- Which answer regarding kidney transplantation is correct?
- (a)
- One must not be older than 50 years to come into consideration for transplantation
- (b)
- One can only be transplanted if one knows somebody who will donate a kidney
- (c)
- A new kidney will last a lifetime
- (d)
- Transplantation—if possible—is the best treatment option for kidney failure
- What is not recommended in relation to kidney failure?
- (a)
- Exercising regularly
- (b)
- Quitting smoking
- (c)
- Eating more salt
- (d)
- Vaccination
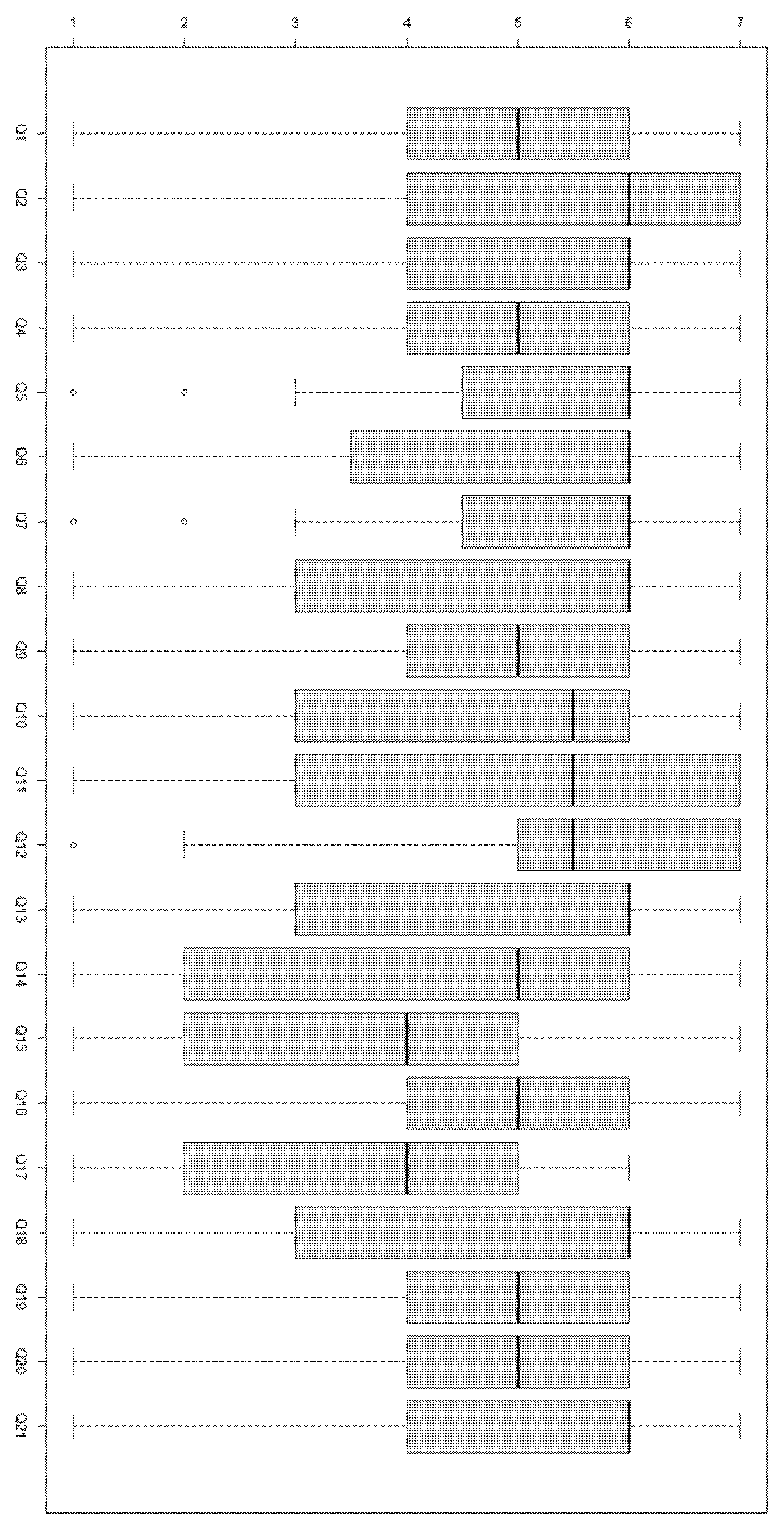
Appendix C. Boxplot of TUQ Responses for Each Question, Used for Data Assessment
References
- Warner, M.M.; Tong, A.; Campbell, K.L.; Kelly, J.T. Patients’ Experiences and Perspectives of Telehealth Coaching with a Dietitian to Improve Diet Quality in Chronic Kidney Disease: A Qualitative Interview Study. J. Acad. Nutr. Diet. 2019, 119, 1362–1374. [Google Scholar] [CrossRef] [PubMed]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2012 Clinical Practice Guidelines for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. Suppl. 2013, 3, 1–150. [Google Scholar]
- Devoe, D.J.; Wong, B.; James, M.T.; Ravani, P.; Oliver, M.J.; Barnieh, L.; Roberts, D.J.; Pauly, R.; Manns, B.J.; Kappel, J.; et al. Patient Education and Peritoneal Dialysis Modality Selection: A Systematic Review and Meta-analysis. Am. J. Kidney Dis. 2016, 68, 422–433. [Google Scholar] [CrossRef]
- Dansk Nefrologisk Selskabs. Dansk Nefrologisk Selskabs Landsregister. Årsrapport 2021, version 1.0; Regionernes Kliniske Kvalitetsudviklingsprogram: Aarhus, Denmark, 2021; p. 2.
- Narva, A.S.; Norton, J.M.; Boulware, L.E. Educating Patients about CKD: The Path to Self-Management and Patient-Centered Care. Clin. J. Am. Soc. Nephrol. 2016, 11, 694–703. [Google Scholar] [CrossRef] [PubMed]
- Cavanaugh, K.L.; Merkin, S.S.; Plantinga, L.C.; Fink, N.E.; Sadler, J.H.; Powe, N.R. Accuracy of patients’ reports of comorbid disease and their association with mortality in ESRD. Am. J. Kidney Dis. 2008, 52, 118–127. [Google Scholar] [CrossRef] [PubMed]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Denmark Shuts Down Schools and Universities to Fight Coronavirus Pandemic. TheLocaldk. 2020. Available online: https://www.thelocal.dk/20200311/denmark-to-shut-all-schools-and-universities-to-fight-virus/ (accessed on 30 June 2022).
- Programme WTGT. Tuberculosis: Global Task Force on Digital Health. World Health Organization. 2015. Available online: https://www.who.int/news-room/questions-and-answers/item/tuberculosis-global-task-force-on-digital-health (accessed on 30 June 2022).
- Patient Education. American Academy of Family Physicians. Am. Fam. Physician 2000, 62, 1712–1714. [Google Scholar]
- Fetters, M.D.; Curry, L.A.; Creswell, J.W. Achieving integration in mixed methods designs-principles and practices. Health Serv. Res. 2013, 48, 2134–2156. [Google Scholar] [CrossRef]
- Malterud, K. Focus Groups as Research Method for Medicine and Health Sciences; Scandinavian University Press: Oslo, Norway, 2012. [Google Scholar]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- O’Grady, L.A.; Witteman, H.; Wathen, C.N. The experiential health information processing model: Supporting collaborative web-based patient education. BMC Med. Inform. Decis. Mak. 2008, 8, 58. [Google Scholar] [CrossRef]
- Salmon, G.; Nie, M.; Edirisingha, P. Developing a five-stage model of learning in Second Life. Educ. Res. 2010, 52, 169–182. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Devins, G.M.; Binik, Y.M.; Mandin, H.; Letourneau, P.; Hollomby, D.J.; Barre, P.E.; Prichard, S. The Kidney Disease Questionnaire: A test for measuring patient knowledge about end-stage renal disease. J. Clin. Epidemiol. 1990, 43, 297–307. [Google Scholar] [CrossRef] [PubMed]
- Parmanto, B.; Lewis, A.N., Jr.; Graham, K.M.; Bertolet, M.H. Development of the Telehealth Usability Questionnaire (TUQ). Int. J. Telerehabil. 2016, 8, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Wild, D.; Grove, A.; Martin, M.; Eremenco, S.; McElroy, S.; Verjee-Lorenz, A.; Erikson, P.; ISPOR Task Force for Translation and Cultural Adaptation. Principles of Good Practice for the Translation and Cultural Adaptation Process for Patient-Reported Outcomes (PRO) Measures: Report of the ISPOR Task Force for Translation and Cultural Adaptation. Value Health 2005, 8, 94–104. [Google Scholar] [CrossRef] [PubMed]
- Morony, S.; Flynn, M.; McCaffery, K.J.; Jansen, J.; Webster, A.C. Readability of Written Materials for CKD Patients: A Systematic Review. Am. J. Kidney Dis. 2015, 65, 842–850. [Google Scholar] [CrossRef] [PubMed]
- Schultz, A.N.O.; Kampmann, J.D.; Kidholm, K.; Moos, C.; Bauer, E.H. mHealth education for patients with chronic kidney disease: Protocol for a scoping review. BMJ Open 2022, 12, e061226. [Google Scholar] [CrossRef]
- Allida, S.; Du, H.; Xu, X.; Prichard, R.; Chang, S.; Hickman, L.D.; Davidson, P.M.; Inglis, S.C. mHealth education interventions in heart failure. Cochrane Database Syst. Rev. 2020, 7, CD011845. [Google Scholar]
- Easom, A.M.; Shukla, A.M.; Rotaru, D.; Ounpraseuth, S.; Shah, S.V.; Arthur, J.M.; Singh, M. Home run-results of a chronic kidney disease Telemedicine Patient Education Study. Clin. Kidney J. 2020, 13, 867–872. [Google Scholar] [CrossRef]
- Dubin, R.; Rubinsky, A. A Digital Modality Decision Program for Patients With Advanced Chronic Kidney Disease. JMIR Form. Res. 2019, 3, e12528. [Google Scholar] [CrossRef]
- Kaiser, P.; Pipitone, O.; Franklin, A.; Jackson, D.R.; Moore, E.A.; Dubuque, C.R.; Peralta, C.A.; De Mory, A.C. A virtual multidisciplinary care program for management of advanced chronic kidney disease: Matched cohort study. J. Med. Internet Res. 2020, 22, e17194. [Google Scholar] [CrossRef] [PubMed]
- Ladin, K.; Porteny, T.; Perugini, J.M.; Gonzales, K.M.; Aufort, K.E.; Levine, S.K.; Wong, J.B.; Isakova, T.; Rifkin, D.; Gordon, E.J.; et al. Perceptions of Telehealth vs. In-Person Visits Among Older Adults with Advanced Kidney Disease, Care Partners, and Clinicians. JAMA Netw. Open 2021, 4, e2137193. [Google Scholar] [CrossRef] [PubMed]
- Barkai, G.; Gadot, M.; Amir, H.; Menashe, M.; Shvimer-Rothschild, L.; Zimlichman, E. Patient and clinician experience with a rapidly implemented large-scale video consultation program during COVID-19. Int. J. Qual. Health Care 2021, 33, mzaa165. [Google Scholar] [CrossRef] [PubMed]
- Schrauben, S.J.; Appel, L.; Rivera, E.; Lora, C.M.; Lash, J.P.; Chen, J.; Hamm, L.L.; Fink, J.C.; Go, A.S.; Townsend, R.R.; et al. Mobile Health (mHealth) Technology: Assessment of Availability, Acceptability, and Use in CKD. Am. J. Kidney Dis. 2021, 77, 941–950. [Google Scholar] [CrossRef]
- Meuleman, Y.; Brinke, L.T.; Kwakernaak, A.J.; Vogt, L.; Rotmans, J.; Bos, W.J.W.; Van Der Boog, P.J.M.; Navis, G.; Van Montfrans, G.A.; Hoekstra, T.; et al. Perceived Barriers and Support Strategies for Reducing Sodium Intake in Patients with Chronic Kidney Disease: A Qualitative Study. Int. J. Behav. Med. 2015, 22, 530–539. [Google Scholar] [CrossRef] [PubMed]
- Clarke, A.L.; Young, H.M.L.; Hull, K.L.; Hudson, N.; Burton, J.O.; Smith, A.C. Motivations and barriers to exercise in chronic kidney disease: A qualitative study. Nephrol. Dial. Transplant. 2015, 30, 1885–1892. [Google Scholar] [CrossRef]
- Reinhard, S.C.; Given, B.; Petlick, N.H.; Bemis, A. Supporting Family Caregivers in Providing Care. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Advances in Patient Safety; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Etics Ncohr. What to Notify? National Commitee on Health Research Etics. 2019. Available online: https://en.nvk.dk/how-to-notify/what-to-notify (accessed on 7 July 2022).
- Wma Declaration of Helsinki–Ethical Principles for Medical Research Involving Human Subjects [Internet]. 2018. Available online: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ (accessed on 26 March 2019).

| Demographics | KKQ | TUQ | |
|---|---|---|---|
| Pre (n = 48) | Post (n = 24) | Post (n = 21) | |
| Male % (n) Female % (n) | 69% (33) 31% (15) | 79% (19) 21% (5) | 76% (16) 24% (5) |
| Age median [IQR] (n) | 69 [10.0] (45) | 69 [15.0] (21) | 69 [10.75] (18) |
Completed questionnaire
| 65% (31) 35% (17) | 57% (13) 43% (10) | 55% (11) 45% (9) |
| Statements 1 | Domain | Strongly Agree | Agree | Somewhat Agree | Neither Agree Nor Disagree | Somewhat Disagree | Disagree | Strongly Disagree | Not Relevant | Number of Responders | Median 2 [IQR] | Domain Median 2 [IQR] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Responders | ||||||||||||
| 1 | Usefulness | 4 | 5 | 3 | 6 | 1 | 1 | 1 | 0 | 21 | 5.0 [2.0] | 5.0 [2.0] |
| 2 | 7 | 4 | 2 | 4 | 0 | 3 | 1 | 0 | 21 | 6.0 [3.0] | ||
| 3 | 4 | 7 | 3 | 2 | 1 | 3 | 1 | 0 | 21 | 6.0 [2.0] | ||
| 4 | Ease of Use | 4 | 4 | 5 | 3 | 2 | 1 | 1 | 0 | 20 | 5.0 [2.0] | 6.0 [2.0] |
| 5 | 3 | 9 | 2 | 1 | 2 | 1 | 1 | 0 | 19 | 6.0 [1.5] | ||
| 6 | 4 | 8 | 0 | 2 | 1 | 3 | 1 | 0 | 19 | 6.0 [2.5] | ||
| 7 | 4 | 8 | 2 | 2 | 1 | 1 | 1 | 0 | 19 | 6.0 [1.5] | ||
| 8 | 4 | 7 | 0 | 2 | 1 | 3 | 1 | 0 | 18 | 6.0 [2.75] | ||
| 9 | 3 | 5 | 4 | 2 | 2 | 1 | 1 | 0 | 18 | 5.0 [2.0] | ||
| 10 | Effectiveness | 2 | 7 | 3 | 1 | 2 | 1 | 2 | 0 | 18 | 5.5 [2.75] | 6.0 [3.0] |
| 11 | 5 | 4 | 2 | 1 | 2 | 3 | 1 | 0 | 18 | 5.5 [3.75] | ||
| 12 | 5 | 4 | 5 | 0 | 0 | 3 | 1 | 0 | 18 | 5.5 [1.75] | ||
| 13 | 4 | 7 | 2 | 0 | 2 | 2 | 1 | 0 | 18 | 6.0 [2.5] | ||
| 14 | 4 | 4 | 2 | 2 | 1 | 4 | 1 | 0 | 18 | 5.0 [3.75] | ||
| 15 | Reliability | 1 | 3 | 4 | 2 | 1 | 6 | 1 | 0 | 18 | 4.0 [3.0] | 5.0 [4.0] |
| 16 | 1 | 6 | 6 | 1 | 0 | 3 | 1 | 0 | 18 | 5.0 [1.75] | ||
| 17 | 0 | 2 | 2 | 3 | 0 | 2 | 2 | 6 | 17 | 4.0 [3.0] | ||
| 18 | Satisfaction | 4 | 5 | 1 | 0 | 3 | 3 | 1 | 0 | 17 | 6.0 [3.0] | 5.0 [3.0] |
| 19 | 2 | 5 | 4 | 2 | 0 | 2 | 2 | 0 | 17 | 5.0 [2.0] | ||
| 20 | 3 | 5 | 3 | 2 | 0 | 2 | 2 | 0 | 17 | 5.0 [2.0] | ||
| 21 | 3 | 6 | 3 | 1 | 0 | 3 | 1 | 0 | 17 | 6.0 [2.0] | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ørsted Schultz, A.N.; Petersen, S.R.; Fibieger, T.; Kampmann, J.D.; Bauer, E.H. Feasibility and First Experiences from an Online Kidney School for Patients with Chronic Kidney Disease. Int. J. Environ. Res. Public Health 2023, 20, 864. https://doi.org/10.3390/ijerph20010864
Ørsted Schultz AN, Petersen SR, Fibieger T, Kampmann JD, Bauer EH. Feasibility and First Experiences from an Online Kidney School for Patients with Chronic Kidney Disease. International Journal of Environmental Research and Public Health. 2023; 20(1):864. https://doi.org/10.3390/ijerph20010864
Chicago/Turabian StyleØrsted Schultz, Anders Nikolai, Stefan Rowald Petersen, Tove Fibieger, Jan Dominik Kampmann, and Eithne Hayes Bauer. 2023. "Feasibility and First Experiences from an Online Kidney School for Patients with Chronic Kidney Disease" International Journal of Environmental Research and Public Health 20, no. 1: 864. https://doi.org/10.3390/ijerph20010864
APA StyleØrsted Schultz, A. N., Petersen, S. R., Fibieger, T., Kampmann, J. D., & Bauer, E. H. (2023). Feasibility and First Experiences from an Online Kidney School for Patients with Chronic Kidney Disease. International Journal of Environmental Research and Public Health, 20(1), 864. https://doi.org/10.3390/ijerph20010864






