Exploration of the Experiences of Persons in the Traumatic Spinal Cord Injury Population in Relation to Chronic Pain Management
Abstract
1. Introduction
2. Materials and Methods
2.1. The Inclusion Criteria for the Study Are Listed Below
- Adult (older than 18 years)
- Diagnosis: traumatic spinal cord injury
- Injury occurring in the last five years, i.e., April 2016–April 2021
- Injury occurring in the Cape Metropolitan region of the Western Cape
2.2. Participants
2.3. Data Collection
- What are the medications’ names that you are currently using? Prompts: how many times do you take it in a day? (Only when you have pain or as prescribed, for example three times a day)
- How else do you manage your pain? Prompts: nonpharmacological (name the type of nonpharmacological treatment and how often it is performed).
- Are you satisfied with your pain management? Prompts: Does the medication take your pain away or improve your pain? How long does the pain stay away for?
- How do you cope with your pain? Prompts: What do you do to ease your pain other than the management described above?
- What education did you receive regarding pain and pain management?
- What advice would you give to health professionals about pain management?
2.4. Data Analysis
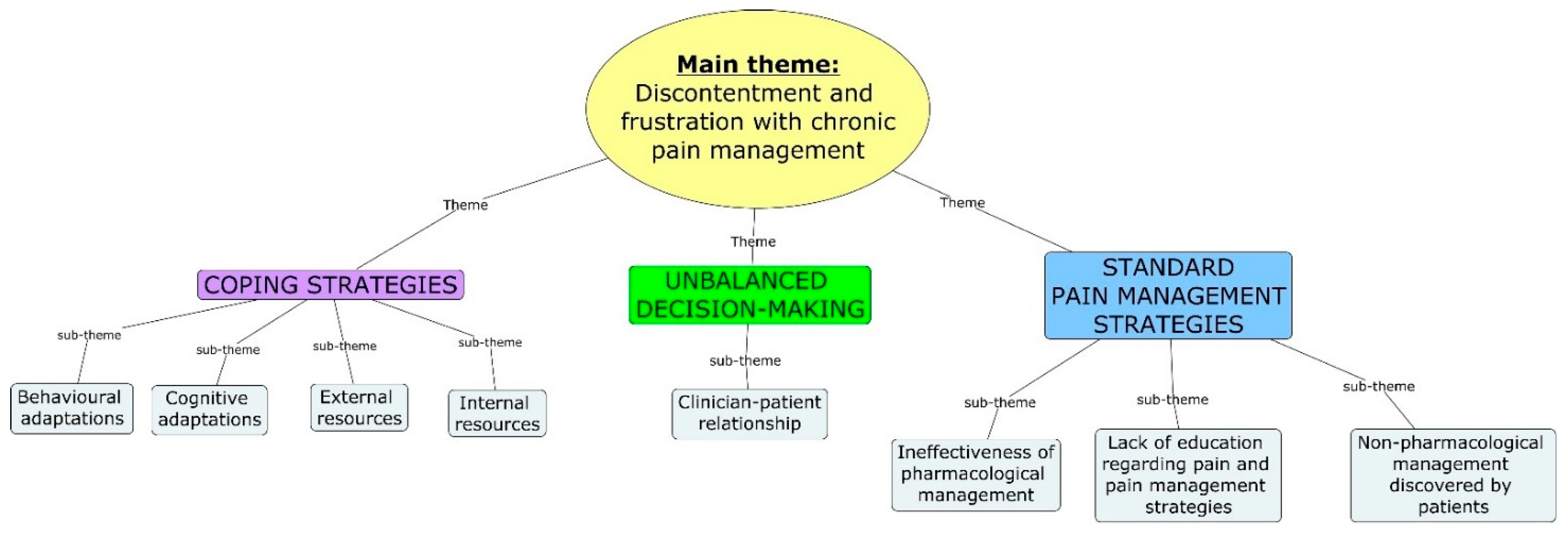
3. Results
3.1. Standard Pain Management Strategies
3.1.1. Ineffectiveness of Pharmacological Management
“It only helps for a short period of time”.(P1)
“It doesn’t take my pain away because like if I drink those medications for some minutes I start to feel the pain again”.(P5)
3.1.2. Nonpharmacological Management Discovered by Patients
“Then when I do the exercises … it helps the pain because why it [exercises] can get the area that I’m exercising, that I’m moving my body”.(P8)
One participant was prescribed calipers for his lower limbs in order to aid mobility and when describing their use, the participant mentioned “If I put those things I don’t feel pain because the blood will be circulating.”(P5)
“The relieve is just for a few hours and then it is back again”.(P3)
“So the moment I go to sleep then the pain is gone”.(P2)
“So he said go see a physiotherapist and since I see the physiotherapist then the pain doesn’t come so much.”(P1)
3.1.3. A Lack of Education Regarding Pain and Pain Management Strategies
“They didn’t teach me anything”.(P3)
“He just only give me the medication”.(P6)
“Like I said after the operation I didn’t see the surgeon and he didn’t come and explain to me what they did, what they saw and what was wrong and what did they put in. I didn’t have any of that information”.(P4)
“It’s the nerves. I think the nerves is getting irritated because why it’s now not moving or anything so now it’s just getting the spasms”.(P13)
“…they said I mustn’t stop my pain tablets, I mustn’t stop the nerve tablets, you know, they said it’s very important to take them but the pain will never go away. And one thing in particular I can remember what they said to me was that I must listen music in my ears to distract me from the pain, that’s all they educate me about, that’s all that they teached me”.(P8)
“No. We were actually just talking about everyday things. But nothing about that [pain education]”.(P4)
“Nothing my dear”.(P8)
“I’m not satisfied because even if I have those tablets, I keep on feeling the pain”.(P5)
“I take the tablets like every day so the pain don’t happen often”.(P13)
3.2. Unbalanced Decision-Making
Clinician–Patient Relationship
“When I told him about this pains in the leg and that, I told him I am the one feeling the pains not you, so he can’t tell me that he cannot make my…how can I say, he can’t make the dosage higher, he must listen to me because it’s me sitting in this wheelchair, it’s not you, so they must listen to their patients man, so that the patients can explain to them thoroughly what is going on so that they can understand what they have to do to help the patient”.(P13)
“That is why I stopped asking the doctor to actually look at these things because for it feels like they don’t really take note of it”.(P4)
“I can say try to give more physio to the patient and see what is the outcome of it. That is the best option I can see”.(P2)
“You know what, to be honest with you, I think the doctors can get, they can do better to help us with our pain, really you know, really they can do better”.(P8)
3.3. Coping Strategies
3.3.1. Behavioural and Cognitive Adaptations
“You see when I lay on my back and I put my legs up that is when the pain starts. So I don’t lay on my back anymore, I just lay on my sides”.(P1)
“I have accepted that I will live with these pains for the rest of my life”.(P11)
“I try to focus on something else. I try to read; I would try to play with Jojo [cat] or what I do is, I try to sing”.(P4)
3.3.2. Internal Resources
“My dear I’m praying a lot my dear. What keeps me going is to live a righteous life and to be strong in my faith you know, my God is really strengthening me and he’s giving me the peace … I’m always happy, irrespective my pain you know, so if you ask me what is keeping me going, it’s my faith in God my dear”.(P8)
“I think I lean on myself and my own strength because I know there is a lot that I can handle”.(P4)
3.3.3. External Resources
“I am just grateful to my wife and children because they are the only one who knows exactly what I go through, even though at times I snap at them or fight with my wife because this life and pains are emotionally consuming me”.(P11)
“I have a sister and with her, she keeps me going man, like when I don’t want to stand up, she say hu uh, kom, kom, ruk jou reg (Afrikaans to English translation: “no, pull yourself together”)… like I have a very supportive family so they are always there to uplift and to motivate me, you know there is that time when you think like yoh I don’t have lus today or so man, but they don’t give me time to think of that”.(P13)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Golestani, A.; Shobeiri, P.; Sadeghi-Naini, M.; Jazayeri, S.B.; Maroufi, S.F.; Ghodsi, Z.; Ohadi, M.A.; Mohammadi, E.; Rahimi-Movaghar, V.; Ghodsi, S.M. Epidemiology of traumatic spinal cord injury in developing countries from 2009 to 2020: A systematic review and meta-analysis. Neuroepidemiology 2022, 56, 219–239. [Google Scholar] [CrossRef] [PubMed]
- Joseph, C.; Delcarme, A.; Vlok, I.; Wahman, K.; Phillips, J.; Nilsson Wikmar, L. Incidence and aetiology of traumatic spinal cord injury in Cape Town, South Africa: A prospective, population-based study. Spinal Cord 2015, 53, 692–696. [Google Scholar] [CrossRef] [PubMed]
- Hunt, C.; Moman, R.; Peterson, A.; Wilson, R.; Covington, S.; Mustafa, R.; Murad, M.H.; Hooten, W.M. Prevalence of chronic pain after spinal cord injury: A systematic review and meta-analysis. Reg. Anesth. Pain Med. 2021, 46, 328–336. [Google Scholar] [CrossRef] [PubMed]
- Andresen, S.R.; Biering-Sørensen, F.; Hagen, E.M.; Nielsen, J.F.; Bach, F.W.; Finnerup, N.B. Pain, spasticity and quality of life in individuals with traumatic spinal cord injury in Denmark. Spinal Cord 2016, 54, 973–979. [Google Scholar] [CrossRef]
- Avluk, O.C.; Gurcay, E.; Gurcay, A.G.; Karaahmet, O.Z.; Tamkan, U.; Cakci, A. Effects of chronic pain on function, depression, and sleep among patients with traumatic spinal cord injury. Ann. Saudi Med. 2014, 34, 211–216. [Google Scholar] [CrossRef]
- Felix, E.R.; Cardenas, D.D.; Bryce, T.N.; Charlifue, S.; Lee, T.K.; MacIntyre, B.; Mulroy, S.; Taylor, H. Prevalence and impact of neuropathic and nonneuropathic pain in chronic spinal cord injury. Arch. Phys. 2022, 103, 729–737. [Google Scholar] [CrossRef]
- Finnerup, N.B. Pain in patients with spinal cord injury. Pain 2013, 154, S71–S76. [Google Scholar] [CrossRef]
- Colloca, L.; Ludman, T.; Bouhassira, D.; Baron, R.; Dickenson, A.H.; Yarnitsky, D.; Freeman, R.; Truini, A.; Attal, N.; Finnerup, N.B.; et al. Neuropathic pain. Nat. Rev. Dis. 2017, 3, 17002. [Google Scholar] [CrossRef]
- Rekand, T.; Hagen, E.M.; Grønning, M. Chronic pain following spinal cord injury. Tidsskr. Nor. Legeforen. 2012, 132, 974–979. [Google Scholar] [CrossRef] [PubMed]
- Wagner Anke, A.G.; Stenehjem, A.E.; Kvalvik Stanghelle, J. Pain and life quality within 2 years of spinal cord injury. Paraplegia 1995, 33, 555–559. [Google Scholar] [CrossRef][Green Version]
- Siddall, P.J.; Middleton, J.W. A proposed algorithm for the management of pain following spinal cord injury. Spinal Cord 2006, 44, 67–77. [Google Scholar] [CrossRef] [PubMed]
- Karran, E.L.; Fryer, C.E.; Middleton, J.W.; Moseley, G.L. Pain and pain management experiences following spinal cord injury–a mixed methods study of Australian community-dwelling adults. Disabil. Rehabil. 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Löfgren, M.; Norrbrink, C. “But I know what works”—Patients’ experience of spinal cord injury neuropathic pain management. Disabil. Rehabil. 2012, 34, 2139–2147. [Google Scholar] [CrossRef]
- Norrbrink, C.; Löfgren, M.; Hunter, J.; Ellis, J. Patients’ perspectives on pain. Top. Spinal Cord Inj. Rehabil. 2012, 18, 50–56. [Google Scholar] [CrossRef][Green Version]
- Norrbrink, C.; Löfgren, M. Needs and requests–patients and physicians voices about improving the management of spinal cord injury neuropathic pain. Disabil. Rehabil. 2016, 38, 151–158. [Google Scholar] [CrossRef]
- Murphy, D.; Reid, D.B. Pain treatment satisfaction in spinal cord injury. Spinal Cord 2001, 39, 44–46. [Google Scholar] [CrossRef] [PubMed]
- Baastrup, C.; Finnerup, N.B. Pharmacological management of neuropathic pain following spinal cord injury. CNS Drugs 2008, 22, 455–475. [Google Scholar] [CrossRef]
- Henwood, P.; Ellis, J.A. Chronic neuropathic pain in spinal cord injury: The patient’s perspective. Pain Res. Manag. 2004, 9, 39–45. [Google Scholar] [CrossRef]
- Widerström-Noga, E.G.; Felix, E.R.; Cruz-Almeida, Y.; Turk, D.C. Psychosocial subgroups in persons with spinal cord injuries and chronic pain. Arch. Phys. M. 2007, 88, 1628–1635. [Google Scholar] [CrossRef]
- Bernardi, M.; Catania, G.; Lambert, A.; Tridello, G.; Luzzani, M. Knowledge and attitudes about cancer pain management: A national survey of Italian oncology nurses. Eur. J. Oncol. Nurs. 2007, 11, 272–279. [Google Scholar] [CrossRef]
- Rahimi-Madiseh, M.; Tavakol, M.; Dennick, R. A quantitative study of Iranian nursing students’ knowledge and attitudes towards pain: Implication for education. Int. J. Nurs. Pract. 2010, 16, 478–483. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.T.; Bowman, J.M.; Eason, F.R. Assessment of nurses’ attitudes and knowledge regarding pain management. J. Contin. Educ. Nurs. 1999, 30, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Engel, G.L. The need for a new medical model: A challenge for biomedicine. Science 1977, 196, 129–136. [Google Scholar] [CrossRef] [PubMed]
- Waddell, G. Volvo award in clinical sciences. A new clinical model for the treatment of low-back pain. Spine 1987, 12, 632–644. [Google Scholar] [CrossRef]
- Madasa, V.; Boggenpoel, B.; Phillips, J.; Joseph, C. Mortality and secondary complications four years after traumatic spinal cord injury in Cape Town, South Africa. Spinal Cord Ser. Cases 2020, 6, 84. [Google Scholar] [CrossRef] [PubMed]
- Colorafi, K.J.; Evans, B. Qualitative descriptive methods in health science research. Health Environ. Res. Des. J. 2016, 9, 16–25. [Google Scholar] [CrossRef]
- Jensen, M.P.; Widerström-Noga, E.; Richards, J.S.; Finnerup, N.B.; Biering-Sørensen, F.; Cardenas, D.D. Reliability and validity of the International Spinal Cord Injury Basic Pain Data Set items as self-report measures. Spinal Cord 2010, 48, 230–238. [Google Scholar] [CrossRef]
- Austin, Z.; Sutton, J. Qualitative research: Getting started. Can. J. Hosp. Pharm. 2014, 67, 436. [Google Scholar] [CrossRef]
- Shenton, A.K. Strategies for ensuring trustworthiness in qualitative research projects. Educ. Inf. 2004, 22, 63–75. [Google Scholar] [CrossRef]
- Franz, S.; Schulz, B.; Wang, H.; Gottschalk, S.; Grüter, F.; Friedrich, J.; Glaesener, J.J.; Bock, F.; Schott, C.; Müller, R.; et al. Management of pain in individuals with spinal cord injury: Guideline of the German-Speaking Medical Society for Spinal Cord Injury. GMS Ger. Med. Sci. 2019, 17, 5. [Google Scholar]
- Ditor, D.S.; Latimer, A.E.; Martin Ginis, K.A.; Arbour, K.P.; McCartney, N.; Hicks, A.L. Maintenance of exercise participation in individuals with spinal cord injury: Effects on quality of life, stress and pain. Spinal Cord 2003, 41, 446–450. [Google Scholar] [CrossRef] [PubMed]
- Widerström-Noga, E.G.; Turk, D.C. Types and effectiveness of treatments used by people with chronic pain associated with spinal cord injuries: Influence of pain and psychosocial characteristics. Spinal Cord 2003, 41, 600–609. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, P.; Duff, J.; Evans, M.; Beedie, A. Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br. J. Clin. Psychol. 2003, 42, 41–52. [Google Scholar] [CrossRef] [PubMed]
- Budh, C.N.; Kowalski, J.; Lundeberg, T. A comprehensive pain management programme comprising educational, cognitive and behavioural interventions for neuropathic pain following spinal cord injury. J. Rehabil. Med. 2006, 38, 172–180. [Google Scholar] [CrossRef] [PubMed]
- Wollaars, M.M.; Post, M.W.; van Asbeck, F.W.; Brand, N. Spinal cord injury pain: The influence of psychologic factors and impact on quality of life. Clin. J. Pain 2007, 23, 383–391. [Google Scholar] [CrossRef]
- Heutink, M.; Post, M.W.; Bongers-Janssen, H.M.; Dijkstra, C.A.; Snoek, G.J.; Spijkerman, D.C.; Lindeman, E. The CONECSI trial: Results of a randomized controlled trial of a multidisciplinary cognitive behavioral program for coping with chronic neuropathic pain after spinal cord injury. Pain 2012, 153, 120–128. [Google Scholar] [CrossRef]
- Perry, K.N.; Nicholas, M.K.; Middleton, J.W. Comparison of a pain management program with usual care in a pain management center for people with spinal cord injury-related chronic pain. Clin. J. Pain 2010, 26, 206–216. [Google Scholar] [CrossRef]
- Burns, A.S.; Delparte, J.J.; Ballantyne, E.C.; Boschen, K.A. Evaluation of an interdisciplinary program for chronic pain after spinal cord injury. PM R 2013, 5, 832–838. [Google Scholar] [CrossRef]
- Adams, J.R.; Drake, R.E. Shared decision-making and evidence-based practice. Commun. Ment. Health J. 2006, 42, 87–105. [Google Scholar] [CrossRef]
- Couët, N.; Desroches, S.; Robitaille, H.; Vaillancourt, H.; Leblanc, A.; Turcotte, S.; Elwyn, G.; Légaré, F. Assessments of the extent to which health-care providers involve patients in decision making: A systematic review of studies using the OPTION instrument. Health Expect. 2015, 18, 542–561. [Google Scholar] [CrossRef]
- Elwyn, G.; Frosch, D.L.; Kobrin, S. Implementing shared decision-making: Consider all the consequences. Implement. Sci. 2015, 11, 114. [Google Scholar] [CrossRef] [PubMed]
- Lin, G.A.; Fagerlin, A. Shared decision making: State of the science. Circ. Circ. Cardiovasc. Qual. Outcomes 2014, 7, 328–334. [Google Scholar] [CrossRef] [PubMed]
- Charles, C.; Gafni, A.; Whelan, T. Shared decision-making in the medical encounter: What does it mean? (Or it takes at least two to tango). Soc. Sci. Med. 1997, 44, 681–692. [Google Scholar] [CrossRef] [PubMed]
- Joosten, E.A.; DeFuentes-Merillas, L.; De Weert, G.H.; Sensky, T.; Van Der Staak, C.P.F.; de Jong, C.A. Systematic review of the effects of shared decision-making on patient satisfaction, treatment adherence and health status. Psychother. Psychosom. 2008, 77, 219–226. [Google Scholar] [CrossRef]
- Norman, C.; Bender, J.L.; Macdonald, J.; Dunn, M.; Dunne, S.; Siu, B.; Hitzig, S.L.; Jadad, A.R.; Hunter, J. Questions that individuals with spinal cord injury have regarding their chronic pain: A qualitative study. Disabil. Rehabil. 2010, 32, 114–124. [Google Scholar] [CrossRef]
- McCracken, L.M. Learning to live with the pain: Acceptance of pain predicts adjustment in persons with chronic pain. Pain 1998, 74, 21–27. [Google Scholar] [CrossRef]
- McCracken, L.M. Behavioral constituents of chronic pain acceptance: Results from factor analysis of the Chronic Pain Acceptance Questionnaire. J. Back Musculoskelet. Rehabil. 1999, 13, 93–100. [Google Scholar] [CrossRef]
- Summers, J.D.; Rapoff, M.A.; Varghese, G.; Porter, K.; Palmer, R.E. Psychosocial factors in chronic spinal cord injury pain. Pain 1991, 47, 183–189. [Google Scholar] [CrossRef]
- Vowles, K.; Sorrell, J. Cognitive/behavioral approaches: Acceptance of chronic pain: Efficacy of a short-term group intervention. J. Pain 2004, 5, S92. [Google Scholar] [CrossRef]
- Esteve, R.; Ramírez-Maestre, C.; López-Martínez, A.E. Adjustment to chronic pain: The role of pain acceptance, coping strategies, and pain-related cognitions. Ann. Behav. Med. 2007, 33, 179–188. [Google Scholar] [CrossRef]
- Dahl, J.; Luciano, C.; Wilson, K. Acceptance and Commitment Therapy for Chronic Pain; New Harbinger Publications: Oakland, CA, USA, 2005; p. 223. [Google Scholar]
- McCaul, K.D.; Malott, J.M. Distraction and coping with pain. Psychol. Bull. 1984, 95, 516–533. [Google Scholar] [CrossRef]
- Subnis, U.B.; Starkweather, A.; Menzies, V. A current review of distraction-based interventions for chronic pain management. Eur. J. Integr. Med. 2016, 8, 715–722. [Google Scholar] [CrossRef]
- Ahmadpour, N.; Randall, H.; Choksi, H.; Gao, A.; Vaughan, C.; Poronnik, P. Virtual Reality interventions for acute and chronic pain management. Int. J. Biochem. Cell Biol. 2019, 114, 105568. [Google Scholar] [CrossRef] [PubMed]
- Pekyavas, N.O.; Ergun, N. Comparison of virtual reality exergaming and home exercise programs in patients with subacromial impingement syndrome and scapular dyskinesis: Short term effect. Acta Orthop. Traumatol. Turc. 2017, 51, 238–242. [Google Scholar] [CrossRef]
- Jones, T.; Moore, T.; Choo, J. The impact of virtual reality on chronic pain. PLoS ONE 2016, 11, e0167523. [Google Scholar] [CrossRef]
- Botella, C.; Garcia-Palacios, A.; Vizcaíno, Y.; Herrero, R.; Baños, R.M.; Belmonte, M.A. Virtual reality in the treatment of fibromyalgia: A pilot study. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 215–223. [Google Scholar] [CrossRef]
- Shiri, S.; Feintuch, U.; Weiss, N.; Pustilnik, A.; Geffen, T.; Kay, B.; Meiner, Z.; Berger, I. A virtual reality system combined with biofeedback for treating pediatric chronic headache—A pilot study. Pain Med. 2013, 14, 621–627. [Google Scholar] [CrossRef]
- Van Rensburg, H.C. South Africa’s protracted struggle for equal distribution and equitable access—Still not there. Hum. Resour. Health 2014, 12, 26. [Google Scholar] [CrossRef]
- De Villiers, K. Bridging the health inequality gap: An examination of South Africa’s social innovation in health landscape. Infect. Dis. Poverty 2021, 10, 19. [Google Scholar] [CrossRef]
- Mining Qualifications Authority. Sector Skills Plan for the Mining and Minerals Sector; A Report Submitted By the MQA to the Department of Higher Education and Training; Mining Qualifications Authority: Johannesburg, South Africa, 2011. [Google Scholar]
| Participants (P) | Gender | Age | Year of Injury | Level of Injury and ASIA Classification | The Most Common Location and Type of Pain | The Second Most Common Location and Type of Pain | The Third Most Common Location and Type of Pain | Pharmacological Management | Nonpharmacological Management |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Male | 33 | 2020 | T1, ASIA A (motor and sensory complete) | Below-level NeuP; bilateral feet | None | None | Baclofen (skeletal muscle relaxant) Triptyline (amitriptyline) (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) | Exercise |
| 2 | Male | 39 | 2017 | C5, ASIA A (motor and sensory complete) | NP; bilateral lower limbs | None | None | Baclofen (skeletal muscle relaxant) Amitriptyline (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) Panadol (analgesic for mild pain) Tramadol (analgesic for mild to moderate pain) | Wonder cream Moving around in the area with the wheelchair |
| 3 | Male | 47 | 2019 | T9, ASIA A (motor and sensory complete) | Visceral NP, stomach | Below-level NeuP; lower back | Below-level NeuP; bilateral lower limbs | Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) | Menthol rub Self-massage |
| 4 | Female | 54 | 2017 | T12, ASIA C (motor and sensory incomplete) | Below-level NeuP; Genitalia | Below-level NeuP; bilateral lower limbs | Visceral NP; throat | Ibuprofen (analgesic and anti-inflammatory) Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) | Does not use nonpharmacological management |
| 5 | Male | 36 | 2018 | T12, ASIA B (motor complete and sensory incomplete) | Below-level NeuP; bilateral lower limbs | Visceral NP; stomach | None | Baclofen (skeletal muscle relaxant) Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) Paracetamol (analgesic for mild to moderate pain) Carbamazepine (anticonvulsant medication for epilepsy and neuropathic pain) | Walking with calipers |
| 6 | Male | 61 | 2018 | C4 (ASIA classification not documented in file) | Below-level NeuP; bilateral lower limbs | None | None | Tramadol (analgesic for mild to moderate pain) Carbamazepine (anticonvulsant medication for epilepsy and neuropathic pain) | Does not use nonpharmacological management |
| 7 | Male | 30 | 2017 | C7, ASIA A (motor and sensory complete) | NP; left shoulder | NP, bilateral lower limbs | None | The participant reports that his pain is not severe enough to use medication. | The participant reports that his pain is not severe enough to use nonpharmacological management. |
| 8 | Male | 35 | 2018 | T11, ASIA A (motor and sensory complete) | Below-level NeuP; stomach | Visceral NP; bladder | None | Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) Triptyline (amitriptyline) (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) Carbamazepine (anticonvulsant medication for epilepsy and neuropathic pain) Paracetamol (analgesic for mild to moderate pain) Adco-dol (analgesic for mild pain) | Exercise |
| 9 | Male | 35 | 2018 | T12, ASIA B (motor complete, sensory incomplete) | Below-level NeuP; right lower limb | None | None | Baclofen (skeletal muscle relaxant) Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) Valium (anxiolytic medication for anxiety, seizures, alcohol withdrawal, muscle spasms, insomnia and restless leg syndrome) Amitriptyline (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) | Smoking cannabis |
| 10 | Male | 47 | 2017 | T6, ASIA classification not documented in file, however, motor complete, sensory incomplete documented) | Other NP; Head | None | None | Grandpa (analgesic for mild to moderate pain) Paracetamol (analgesic for mild to moderate pain) Carbamazepine (anticonvulsant medication for epilepsy and neuropathic pain) Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) Amitriptyline (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) | Does not use nonpharmacological management |
| 11 | Male | 47 | 2018 | C8, ASIA A (motor and sensory complete) | Below-level NeuP; left hip | NP; bilateral fingers | Below-level NeuP; left shoulder | Triptyline (amitriptyline) (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) Ibuprofen (analgesic and anti-inflammatory) Tramadol (analgesic for mild to moderate pain) | African plant called NidorellaExercise Ointment use Self-massage |
| 12 | Male | 41 | 2018 | T2, ASIA A (motor and sensory complete) | NP; upper back | None | None | Norflex (skeletal muscle relaxant) Amitriptyline (antidepressant and analgesic for various types of pain ranging from neuropathic to fibromyalgia to migraines and tension headaches) Painamol (analgesic for mild to moderate pain) | Does not use nonpharmacological management |
| 13 | Female | 21 | 2018 | T5, ASIA A (motor and sensory complete) | Below-level NeuP; genitalia | None | None | Baclofen (skeletal muscle relaxant) Pregabalin/Lyrica (analgesic specifically for neuropathic pain, anticonvulsant and anxiolytic) | Heat/Hot water bottle use |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Williams, T.-L.; Joseph, C.; Nilsson-Wikmar, L.; Phillips, J. Exploration of the Experiences of Persons in the Traumatic Spinal Cord Injury Population in Relation to Chronic Pain Management. Int. J. Environ. Res. Public Health 2023, 20, 77. https://doi.org/10.3390/ijerph20010077
Williams T-L, Joseph C, Nilsson-Wikmar L, Phillips J. Exploration of the Experiences of Persons in the Traumatic Spinal Cord Injury Population in Relation to Chronic Pain Management. International Journal of Environmental Research and Public Health. 2023; 20(1):77. https://doi.org/10.3390/ijerph20010077
Chicago/Turabian StyleWilliams, Tammy-Lee, Conran Joseph, Lena Nilsson-Wikmar, and Joliana Phillips. 2023. "Exploration of the Experiences of Persons in the Traumatic Spinal Cord Injury Population in Relation to Chronic Pain Management" International Journal of Environmental Research and Public Health 20, no. 1: 77. https://doi.org/10.3390/ijerph20010077
APA StyleWilliams, T.-L., Joseph, C., Nilsson-Wikmar, L., & Phillips, J. (2023). Exploration of the Experiences of Persons in the Traumatic Spinal Cord Injury Population in Relation to Chronic Pain Management. International Journal of Environmental Research and Public Health, 20(1), 77. https://doi.org/10.3390/ijerph20010077





