Health Effects of Exposure to Indoor Semi-Volatile Organic Compounds in Chinese Building Environment: A Systematic Review
Abstract
1. Introduction
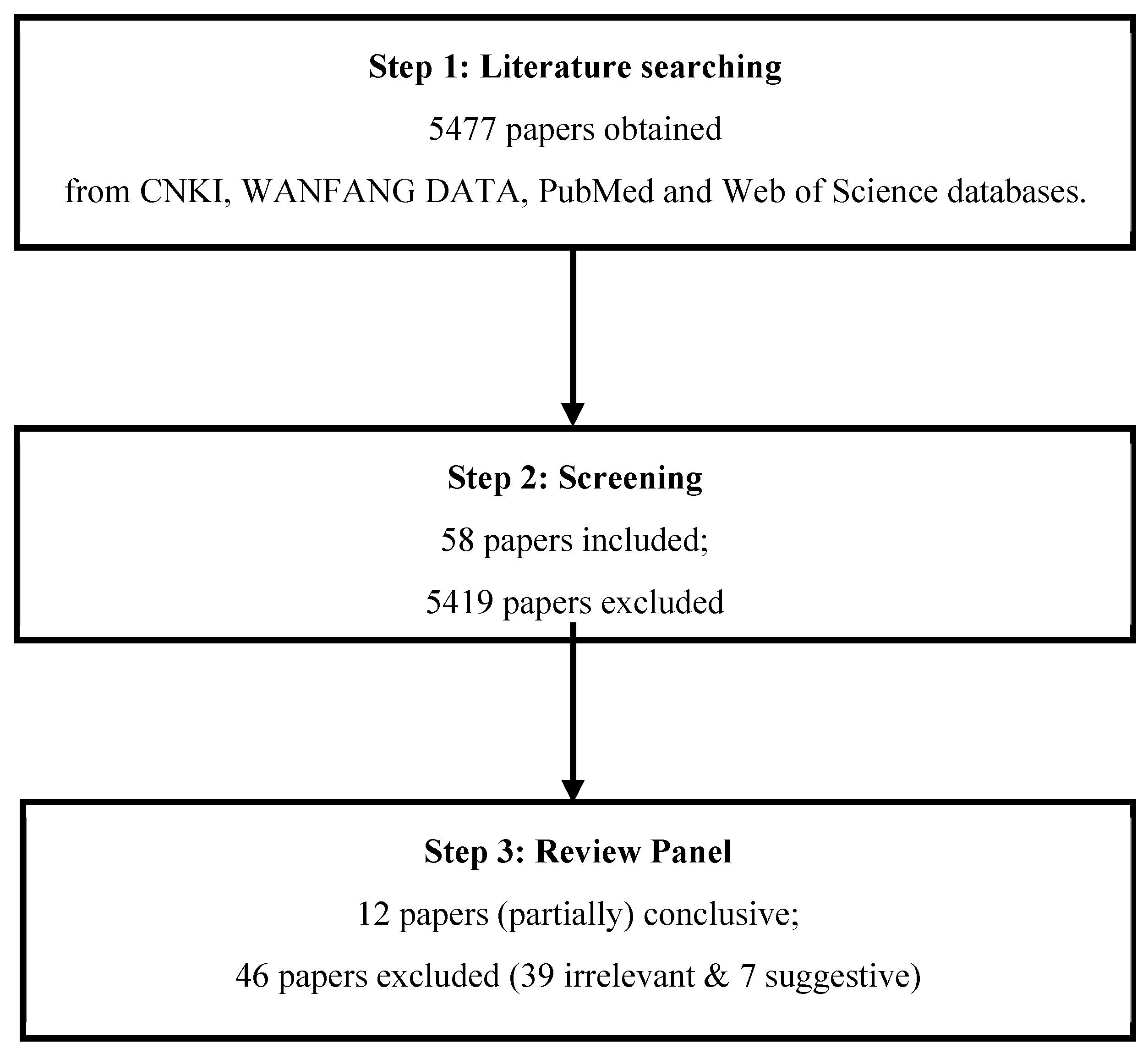
2. Materials and Methods
2.1. Literature Searching
2.2. Literature Screening
2.3. Literature Review
- Relevant and (partially) conclusive—giving sufficient information regarding exposure to indoor SVOCs and its health outcomes, and relationship between indoor SVOC exposure and its health outcomes.
- Relevant and suggestive (background)—although not conclusive, there is some suggestion that exposure to indoor SVOCs and health outcomes may be associated—or neither.
- Irrelevant—not addressing a topic covered by the review; lacking information on exposure to indoor SVOCs and its health outcomes.
3. Results and Discussion
3.1. Polycyclic Aromatic (PAHs) and Health Outcomes
3.2. Phthalates and Health Outcomes
3.3. Research Gaps and Future Considerations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- US EPA. Introduction to Indoor Air Quality. 2014. Available online: https://www.epa.gov/indoor-air-quality-iaq/introduction-indoor-air-quality (accessed on 7 December 2017).
- Lucattini, L.; Poma, G.; Covaci, A.; de Boer, J.; Lamoree, M.H.; Leonards, P.E. A review of semi-volatile organic compounds (SVOCs) in the indoor environment: Occurrence in consumer products, indoor air and dust. Chemosphere 2018, 201, 466–482. [Google Scholar] [CrossRef] [PubMed]
- Klepeis, N.E.; Nelson, W.C.; Ott, W.R.; Robinson, J.P.; Tsang, A.M.; Switzer, P.; Behar, J.V.; Hern, S.C.; Engelmann, W.H. The National Human Activity Pattern Survey (NHAPS): A resource for assessing exposure to environmental pollutants. J. Expo. Sci. Environ. Epidemiol. 2001, 11, 231–252. [Google Scholar] [CrossRef] [PubMed]
- Fan, G.; Xie, J.; Yoshino, H.; Yanagi, U.; Hasegawa, K.; Kagi, N.; Liu, J. Environmental conditions in homes with healthy and unhealthy schoolchildren in Beijing, China. Build. Environ. 2017, 112, 270–284. [Google Scholar] [CrossRef]
- Hu, J.; Li, N.; Lv, Y.; Liu, J.; Xie, J.; Zhang, H. Investigation on indoor air pollution and childhood allergies in households in six Chinese cities by subjective survey and field measurements. Int. J. Environ. Res. Public Health 2017, 14, 979. [Google Scholar] [CrossRef]
- Zhang, H.; Xie, J.; Yoshino, H.; Yanagi, U.; Hasegawa, K.; Kagi, N.; Lian, Z. Thermal and environmental conditions in Shanghai households: Risk factors for childhood health. Build. Environ. 2016, 104, 35–46. [Google Scholar] [CrossRef]
- D’Hollander, W.; Roosens, L.; Covaci, A.; Cornelis, C.; Reynders, H.; Van Campenhout, K.; de Voogt, P.; Bervoets, L. Brominated flame retardants and perfluorinated compounds in indoor dust from homes and offices in Flanders, Belgium. Chemosphere 2010, 81, 478–487. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Li, N.; Yoshino, H.; Yanagi, U.; Hasegawa, K.; Kagi, N.; He, Y.; Wei, X. Field study on indoor health risk factors in households with schoolchildren in south-central China. Build. Environ. 2017, 117, 260–273. [Google Scholar] [CrossRef]
- Waked, M.; Salameh, P. Risk factors for asthma and allergic diseases in school children across Lebanon. J. Asthma Allergy 2009, 2, 1. [Google Scholar] [CrossRef]
- Fan, G.; Xie, J.; Yoshino, H.; Zhang, H.; Li, Z.; Li, N.; Liu, J.; Lv, Y.; Zhu, S.; Yanagi, U. Common SVOCs in house dust from urban dwellings with schoolchildren in six typical cities of China and associated non-dietary exposure and health risk assessment. Environ. Int. 2018, 120, 431–442. [Google Scholar] [CrossRef]
- Xu, Y.; Zhang, J. Understanding SVOCs. ASHRAE J. 2011, 53, 121–125. [Google Scholar]
- World Health Organization. Indoor Air Quality: Organic Pollutants. In Proceedings of the Report on a WHO Meeting, Berlin, Germany, 23–27 August 1987; EURO Reports and Studies 111. World Health Organization Regional Office for Europe: Copenhagen, Denmark, 1989. [Google Scholar]
- Blanchard, O.; Glorennec, P.; Mercier, F.; Bonvallot, N.; Chevrier, C.; Ramalho, O.; Mandin, C.; Bot, B.L. Semivolatile organic compounds in indoor air and settled dust in 30 French dwellings. Environ. Sci. Technol. 2014, 48, 3959–3969. [Google Scholar] [CrossRef] [PubMed]
- Król, S.; Namieśnik, J.; Zabiegała, B. Occurrence and levels of polybrominated diphenyl ethers (PBDEs) in house dust and hair samples from Northern Poland; an assessment of human exposure. Chemosphere 2014, 110, 91–96. [Google Scholar] [CrossRef] [PubMed]
- Langer, S.; Weschler, C.J.; Fischer, A.; Bekö, G.; Toftum, J.; Clausen, G. Phthalate and PAH concentrations in dust collected from Danish homes and daycare centers. Atmos. Environ. 2010, 44, 2294–2301. [Google Scholar] [CrossRef]
- Pei, X.; Song, M.; Guo, M.; Mo, F.; Shen, X. Concentration and risk assessment of phthalates present in indoor air from newly decorated apartments. Atmos. Environ. 2013, 68, 17–23. [Google Scholar] [CrossRef]
- Rudel, R.A.; Camann, D.E.; Spengler, J.D.; Korn, L.R.; Brody, J.G. Phthalates, alkylphenols, pesticides, polybrominated diphenyl ethers, and other endocrine-disrupting compounds in indoor air and dust. Environ. Sci. Technol. 2003, 37, 4543–4553. [Google Scholar] [CrossRef]
- Wang, B.-L.; Pang, S.-T.; Sun, J.-P.; Zhang, X.-L.; Li, X.-L.; Sun, Y.-G.; Lu, X.-M.; Zhang, Q. Levels of polychlorinated biphenyls in settled house dust from urban dwellings in China and their neurodevelopmental effects on preschool-aged children. Sci. Total Environ. 2015, 505, 402–408. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.-J.; Lin, B.-G.; Liang, W.-B.; Li, L.-Z.; Chen, X.-C.; Xu, X.-Y.; Xiang, M.-d.; Huang, S. Associations between PBDEs exposure from house dust and human semen quality at an e-waste areas in South China–A pilot study. Chemosphere 2018, 198, 266–273. [Google Scholar] [CrossRef]
- Yu, Y.-X.; Pang, Y.-P.; Li, C.; Li, J.-L.; Zhang, X.-Y.; Yu, Z.-Q.; Feng, J.-L.; Wu, M.-H.; Sheng, G.-Y.; Fu, J.-M. Concentrations and seasonal variations of polybrominated diphenyl ethers (PBDEs) in in-and out-house dust and human daily intake via dust ingestion corrected with bioaccessibility of PBDEs. Environ. Int. 2012, 42, 124–131. [Google Scholar] [CrossRef]
- Zhang, Q.; Lu, X.-M.; Zhang, X.-L.; Sun, Y.-G.; Zhu, D.-M.; Wang, B.-L.; Zhao, R.-Z.; Zhang, Z.-D. Levels of phthalate esters in settled house dust from urban dwellings with young children in Nanjing, China. Atmos. Environ. 2013, 69, 258–264. [Google Scholar] [CrossRef]
- Boström, C.-E.; Gerde, P.; Hanberg, A.; Jernström, B.; Johansson, C.; Kyrklund, T.; Rannug, A.; Törnqvist, M.; Victorin, K.; Westerholm, R. Cancer risk assessment, indicators, and guidelines for polycyclic aromatic hydrocarbons in the ambient air. Environ. Health Perspect. 2002, 110, 451–488. [Google Scholar]
- Guo, Y.; Huo, X.; Wu, K.; Liu, J.; Zhang, Y.; Xu, X. Carcinogenic polycyclic aromatic hydrocarbons in umbilical cord blood of human neonates from Guiyu, China. Sci. Total Environ. 2012, 427, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Bu, Z.; Xu, X.; Xu, Q.; Mmereki, D.; Wang, J.; Cheng, Z.; Li, K.; Dong, C. Indoor polybrominated diphenyl ethers in urban China: An exposure and risk assessment based on settled dust from selected urban regions. Sci. Total Environ. 2020, 714, 136808. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Zhou, Y.; Cui, X.; Wu, X.; Yuan, J.; Xie, J.; Chen, W. Urinary polycyclic aromatic hydrocarbon metabolites and adult asthma: A case-control study. Sci. Rep. 2018, 8, 7658. [Google Scholar] [CrossRef] [PubMed]
- Chuang, J.C.; Mack, G.A.; Kuhlman, M.R.; Wilson, N.K. Polycyclic aromatic hydrocarbons and their derivatives in indoor and outdoor air in an eight-home study. Atmospheric Environment. Part B. Urban Atmos. 1991, 25, 369–380. [Google Scholar] [CrossRef]
- World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Life; World Health Organization: Geneva, Switzerland, 2002; pp. 1–248. [Google Scholar]
- Li, Z.; Zhang, L.; Ye, R.; Pei, L.; Liu, J.; Zheng, X.; Ren, A. Indoor air pollution from coal combustion and the risk of neural tube defects in a rural population in Shanxi Province, China. Am. J. Epidemiol. 2011, 174, 451–458. [Google Scholar] [CrossRef]
- Khalequzzaman, M.; Kamijima, M.; Sakai, K.; Hoque, B.A.; Nakajima, T. Indoor air pollution and the health of children in biomass-and fossil-fuel users of Bangladesh: Situation in two different seasons. Environ. Health Prev. Med. 2010, 15, 236–243. [Google Scholar] [CrossRef]
- Ahmed, F.; Hossain, S.; Hossain, S.; Fakhruddin, A.N.M.; Abdullah, A.T.M.; Chowdhury, M.A.Z.; Gan, S.H. Impact of household air pollution on human health: Source identification and systematic management approach. SN Appl. Sci. 2019, 1, 418. [Google Scholar] [CrossRef]
- Sobue, T. Association of indoor air pollution and lifestyle with lung cancer in Osaka, Japan. Int. J. Epidemiol. 1990, 19, S62–S66. [Google Scholar] [CrossRef]
- Behera, D.; Balamugesh, T. Indoor air pollution as a risk factor for lung cancer in women. JAPI 2005, 53, 190–192. [Google Scholar]
- Ezzati, M. Indoor air pollution and health in developing countries. Lancet 2005, 366, 104–106. [Google Scholar] [CrossRef]
- Ko, Y.-C.; Lee, C.-H.; Chen, M.-J.; Huang, C.-C.; Chang, W.-Y.; Lin, H.-J.; Wang, H.-Z.; Chang, P.-Y. Risk factors for primary lung cancer among non-smoking women in Taiwan. Int. J. Epidemiol. 1997, 26, 24–31. [Google Scholar] [CrossRef]
- Zhong, L.; Goldberg, M.S.; Parent, M.-É.; Hanley, J.A. Risk of developing lung cancer in relation to exposure to fumes from Chinese-style cooking. Scand. J. Work Environ. Health 1999, 25, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Duan, Y.-P.; Meng, X.-Z.; Yang, C.; Pan, Z.-Y.; Chen, L.; Yu, R.; Li, F.-T. Polybrominated diphenyl ethers in background surface soils from the Yangtze River Delta (YRD), China: Occurrence, sources, and inventory. Environ. Sci. Pollut. Res. 2010, 17, 948–956. [Google Scholar] [CrossRef] [PubMed]
- Hites, R.A. Polybrominated diphenyl ethers in the environment and in people: A meta-analysis of concentrations. Environ. Sci. Technol. 2004, 38, 945–956. [Google Scholar] [CrossRef] [PubMed]
- Tang, J.; Zhai, J.X. Distribution of polybrominated diphenyl ethers in breast milk, cord blood and placentas: A systematic review. Environ. Sci. Pollut. Res. 2017, 24, 21548–21573. [Google Scholar] [CrossRef]
- Leonetti, C.; Butt, C.M.; Hoffman, K.; Miranda, M.L.; Stapleton, H.M. Concentrations of polybrominated diphenyl ethers (PBDEs) and 2, 4, 6-tribromophenol in human placental tissues. Environ. Int. 2016, 88, 23–29. [Google Scholar] [CrossRef]
- Zhao, Y.; Ruan, X.; Li, Y.; Yan, M.; Qin, Z. Polybrominated diphenyl ethers (PBDEs) in aborted human fetuses and placental transfer during the first trimester of pregnancy. Environ. Sci. Technol. 2013, 47, 5939–5946. [Google Scholar] [CrossRef]
- Gingrich, J.; Ticiani, E.; Veiga-Lopez, A. Placenta disrupted: Endocrine disrupting chemicals and pregnancy. Trends Endocrinol. Metab. 2020, 31, 508–524. [Google Scholar] [CrossRef]
- Li, K.; Fu, S. Polybrominated diphenyl ethers (PBDEs) in house dust in Beijing, China. Bull. Environ. Contam. Toxicol. 2013, 91, 382–385. [Google Scholar] [CrossRef]
- Knoth, W.; Mann, W.; Meyer, R.; Nebhuth, J. Polybrominated diphenyl ether in sewage sludge in Germany. Chemosphere 2007, 67, 1831–1837. [Google Scholar] [CrossRef]
- Lin, C.; Zeng, Z.; Xu, R.; Liang, W.; Guo, Y.; Huo, X. Risk assessment of PBDEs and PCBs in dust from an e-waste recycling area of China. Sci. Total Environ. 2022, 803, 150016. [Google Scholar] [CrossRef]
- Zhao, S.; Breivik, K.; Jones, K.C.; Sweetman, A.J. Modeling the time-variant dietary exposure of PCBs in China over the period 1930 to 2100. Environ. Sci. Technol. 2018, 52, 7371–7379. [Google Scholar] [CrossRef]
- Mallol, J.; Crane, J.; von Mutius, E.; Odhiambo, J.; Keil, U.; Stewart, A. The International Study of Asthma and Allergies in Childhood (ISAAC) Phase Three: A global synthesis. Allergol. Immunopathol. 2013, 41, 73–85. [Google Scholar] [CrossRef]
- Braman, S.S. The global burden of asthma. Chest 2006, 130, 4S–12S. [Google Scholar] [CrossRef]
- Redd, S.C. Asthma in the United States: Burden and current theories. Environ. Health Perspect. 2002, 110, 557–560. [Google Scholar] [CrossRef]
- Zhu, C.; Sun, Y.; Zhao, Y.; Hou, J.; Zhang, Q.; Wang, P. Associations between Children’s asthma and allergic symptoms and phthalates in dust in metropolitan Tianjin, China. Chemosphere 2022, 302, 134786. [Google Scholar] [CrossRef]
- Wang, L.; Zhao, B.; Liu, C.; Lin, H.; Yang, X.; Zhang, Y. Indoor SVOC pollution in China: A review. Chin. Sci. Bull. 2010, 55, 1469–1478. [Google Scholar] [CrossRef]
- Wang, X.; Tao, W.; Xu, Y.; Feng, J.; Wang, F. Indoor phthalate concentration and exposure in residential and office buildings in Xi’an, China. Atmos. Environ. 2014, 87, 146–152. [Google Scholar] [CrossRef]
- Nie, Z.; Meng, G.; Xiaomeng, W.; Yan, F.; Yong, Y.; Yan, W. Association between POPs in indoor PM2.5 and pediatric asthma. Acta Sci. Circumstantiae 2016, 36, 1849–1858. (In Chinese) [Google Scholar]
- Wang, F.L.; Dai, X.D. Risk factor analysis of female lung cancer in Harbin—Indoor air pollution. Chin. J. Prev. Med. 1989, 23, 270–273. (In Chinese) [Google Scholar]
- China Preventive Medical Center. Determination of air pollutants in areas with high and low incidence of lung cancer in Xuanwei County. Health Res. 1984, 2, 22–27. (In Chinese) [Google Scholar]
- Lan, Q.; He, X.; Shen, M.; Tian, L.; Liu, L.Z.; Lai, H.; Chen, W.; Berndt, S.I.; Hosgood, H.D.; Lee, K.M. Variation in lung cancer risk by smoky coal subtype in Xuanwei, China. Int. J. Cancer 2008, 123, 2164–2169. [Google Scholar] [CrossRef]
- Hoshuyama, T.; Pan, G.; Tanaka, C.; Feng, Y.; Liu, T.; Liu, L.; Hanaoka, T.; Takahashi, K. Mortality of iron-steel workers in Anshanl China: A retrospective cohort study. Int. J. Occup. Environ. Health 2006, 12, 193–202. [Google Scholar] [CrossRef]
- He, L. The Effect and Mechanism of Polycyclic Aromatic Hydrocarbons Exposure on the Capability of Learning and Memory in Crowd. Master’s Thesis, Chongqing Medical University, Chongqing, China, 2010. (In Chinese). [Google Scholar]
- Moorthy, B.; Chu, C.; Carlin, D.J. Polycyclic aromatic hydrocarbons: From metabolism to lung cancer. Toxicol. Sci. 2015, 145, 5–15. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for Europe. WHO Guidelines for Indoor Air Quality: Selected Pollutants; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2010; pp. 1–454. [Google Scholar]
- Tian, L.; Lan, Q.; Yang, D.; He, X.; Ignatius, T.; Hammond, S.K. Effect of chimneys on indoor air concentrations of PM10 and benzo [a] pyrene in Xuan Wei, China. Atmos. Environ. 2009, 43, 3352–3355. [Google Scholar] [CrossRef]
- Bai, Z.; Wang, Z.; Zhu, T.; Zhang, J.J. Developing indoor air quality related standards in China. J. Asian Archit. Build. Eng. 2003, 2, 55–60. [Google Scholar] [CrossRef][Green Version]
- Verma, R.; Patel, K.S.; Verma, S.K. Indoor polycyclic aromatic hydrocarbon concentration in central India. Polycycl. Aromat. Compd. 2016, 36, 152–168. [Google Scholar] [CrossRef]
- World Health Organization, Regional Office for Europe. Air Quality Guidelines for Europe; WHO Regional Office for Europe: Copenhagen, Denmark, 1987; pp. 1–426. [Google Scholar]
- Hosgood, H.; Chapman, R.; Shen, M.; Blair, A.; Chen, E.; Zheng, T.; Lee, K.; He, X.; Lan, Q. Portable stove use is associated with lower lung cancer mortality risk in lifetime smoky coal users. Br. J. Cancer 2008, 99, 1934–1939. [Google Scholar] [CrossRef]
- Lee, K.; Chapman, R.; Shen, M.; Lubin, J.; Silverman, D.; He, X.; Hosgood, H.; Chen, B.; Rajaraman, P.; Caporaso, N. Differential effects of smoking on lung cancer mortality before and after household stove improvement in Xuanwei, China. Br. J. Cancer 2010, 103, 727–729. [Google Scholar] [CrossRef]
- Shen, G.; Lin, W.; Chen, Y.; Yue, D.; Liu, Z.; Yang, C. Factors influencing the adoption and sustainable use of clean fuels and cookstoves in China-a Chinese literature review. Renew. Sustain. Energy Rev. 2015, 51, 741–750. [Google Scholar] [CrossRef]
- Wu, A.H.; Henderson, B.E.; Pike, M.C.; Yu, M.C. Smoking and other risk factors for lung cancer in women. J. Natl. Cancer Inst. 1985, 74, 747–751. [Google Scholar]
- Lissowska, J.; Bardin-Mikolajczak, A.; Fletcher, T.; Zaridze, D.; Szeszenia-Dabrowska, N.; Rudnai, P.; Fabianova, E.; Cassidy, A.; Mates, D.; Holcatova, I. Lung cancer and indoor pollution from heating and cooking with solid fuels: The IARC international multicentre case-control study in Eastern/Central Europe and the United Kingdom. Am. J. Epidemiol. 2005, 162, 326–333. [Google Scholar] [CrossRef] [PubMed]
- Sram, R.J.; Binkova, B.; Dostal, M.; Merkerova-Dostalova, M.; Libalova, H.; Milcova, A.; Rossner Jr, P.; Rossnerova, A.; Schmuczerova, J.; Svecova, V. Health impact of air pollution to children. Int. J. Hyg. Environ. Health 2013, 216, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Cho, J.; Sohn, J.; Noh, J.; Jang, H.; Kim, W.; Cho, S.-K.; Seo, H.; Seo, G.; Lee, S.-K.; Noh, Y. Association between exposure to polycyclic aromatic hydrocarbons and brain cortical thinning: The Environmental Pollution-Induced Neurological EFfects (EPINEF) study. Sci. Total Environ. 2020, 737, 140097. [Google Scholar] [CrossRef]
- Wu, M.-T.; Lee, L.-H.; Ho, C.-K.; Wu, S.-C.; Lin, L.-Y.; Cheng, B.-H.; Liu, C.-L.; Yang, C.-Y.; Tsai, H.-T.; Wu, T.-N. Environmental exposure to cooking oil fumes and cervical intraepithelial neoplasm. Environ. Res. 2004, 94, 25–32. [Google Scholar] [CrossRef]
- Sun, Y. Research on the Association between Dorm Environmental Factors and Allergies among College Students. Ph.D. Thesis, Tianjin University, Tianjin, China, 2008. (In Chinese). [Google Scholar]
- Zhang, Q. Study on Phthalates Exposure in Residential Buildings and its Health Effects. Master’s Thesis, Tianjin University, Tianjin, China, 2016. (In Chinese). [Google Scholar]
- Hu, J. Research on the Influence of Indoor Environment on Children’s Health Risk in Urban Buildings. Ph.D. Thesis, Hunan University, Hunan, China, 2017. (In Chinese). [Google Scholar]
- Zhang, W. Study on Exposure of Phthalates in Typical Indoor Environment of Campus. Master’s Thesis, Beijing University of Civil Engineering and Architecture, Beijing, China, 2017. (In Chinese). [Google Scholar]
- ISAAC Steering Committee. Worldwide variations in the prevalence of asthma symptoms: The international study of asthma and allergies in childhood (ISSAC). Eur. Respir. J. 1998, 12, 315–335. [Google Scholar] [CrossRef]
- Sun, Y.; Hou, J.; Sheng, Y.; Kong, X.; Weschler, L.B.; Sundell, J. Modern life makes children allergic. A cross-sectional study: Associations of home environment and lifestyles with asthma and allergy among children in Tianjin region, China. Int. Arch. Occup. Environ. Health 2019, 92, 587–598. [Google Scholar] [CrossRef]
- Zhang, Y.; Mo, J.; Weschler, C.J. Reducing health risks from indoor exposures in rapidly developing urban China. Environ. Health Perspect. 2013, 121, 751–755. [Google Scholar] [CrossRef]
- Bornehag, C.-G.; Sundell, J.; Weschler, C.J.; Sigsgaard, T.; Lundgren, B.; Hasselgren, M.; Hägerhed-Engman, L. The association between asthma and allergic symptoms in children and phthalates in house dust: A nested case–control study. Environ. Health Perspect. 2004, 112, 1393–1397. [Google Scholar] [CrossRef]
- Kolarik, B.; Naydenov, K.; Larsson, M.; Bornehag, C.-G.; Sundell, J. The association between phthalates in dust and allergic diseases among Bulgarian children. Environ. Health Perspect. 2008, 116, 98–103. [Google Scholar] [CrossRef]
- Bamai, Y.A.; Shibata, E.; Saito, I.; Araki, A.; Kanazawa, A.; Morimoto, K.; Nakayama, K.; Tanaka, M.; Takigawa, T.; Yoshimura, T. Exposure to house dust phthalates in relation to asthma and allergies in both children and adults. Sci. Total Environ. 2014, 485, 153–163. [Google Scholar] [CrossRef] [PubMed]
- Bølling, A.K.; Sripada, K.; Becher, R.; Bekö, G. Phthalate exposure and allergic diseases: Review of epidemiological and experimental evidence. Environ. Int. 2020, 139, 105706. [Google Scholar] [CrossRef] [PubMed]
- Zhu, Q.; Jia, J.; Zhang, K.; Zhang, H.; Liao, C.; Jiang, G. Phthalate esters in indoor dust from several regions, China and their implications for human exposure. Sci. Total Environ. 2019, 652, 1187–1194. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.; Chapman, R.S.; Hu, W.; He, X.; Hosgood, H.D.; Liu, L.Z.; Lai, H.; Chen, W.; Silverman, D.T.; Vermeulen, R. Smoky coal, tobacco smoking, and lung cancer risk in Xuanwei, China. Lung Cancer 2014, 84, 31–35. [Google Scholar] [CrossRef] [PubMed]
- Chuang, J.; Cao, S.; Xian, Y.; Harris, D.; Mumford, J. Chemical characterization of indoor air of homes from communes in Xuan Wei, China, with high lung cancer mortality rate. Atmospheric Environment. Part A. Gen. Top. 1992, 26, 2193–2201. [Google Scholar] [CrossRef]
- Lan, Q.; Chen, W.; Chen, H.; He, X. Risk factors for lung cancer in non-smokers in Xuanwei County of China. Biomed. Environ. Sci. BES 1993, 6, 112. [Google Scholar]
- Wei, C.-F.; Chen, M.-H.; Lin, C.-C.; Guo, Y.L.; Lin, S.-J.; Hsieh, W.-S.; Chen, P.-C. Household incense burning and infant gross motor development: Results from the Taiwan Birth Cohort Study. Environ. Int. 2018, 115, 110–116. [Google Scholar] [CrossRef]

| References | Health Outcomes | Types of Study | Settings/Locations | Investigated Population | Indoor Pollutants | Findings |
|---|---|---|---|---|---|---|
| Wang and Dai (1989) [53] | Lung cancer | Case–control | Homes in Harbin, Heilongjiang Province | 55 females with lung adenocarcinoma and 55 healthy females aged 30–69 (±5) years old | B[a]P | The highest risk variables for lung cancer were a high coal consumption index (odds ratio (OR): 10.59) and indoor smog pollution (OR: 15.19). The daily amounts of total suspended particulate (TSP) and B[a]P in residents’ bedrooms were 4.4 and 26.7 times higher indoors than outdoors in the winter. The indoor daily average concentration of B[a]P was 0.0106–0.0598 μg/m3. |
| China Preventive Medical Center (1984) [54] | Lung cancer | Case–control | Homes in Xuanwei County, Yunnan Province | People in areas with high/low incidence of lung cancer | B[a]P | The indoor concentrations of B[a]P in lung cancer high-incidence areas (6.29 µg/m3) were significantly higher (more than ten times) than in low-incidence areas (0.45 µg/m3). |
| Lan et al. (2008) [55] | Lung cancer | Case–control | Homes in Xuanwei, Yunnan Province | 498 farmers with lung cancer as a case group and 498 farmers as a control group | Smoky coal subtype as an indicator of BaP exposure | When compared to the use of smokeless coal or wood (OR = 7.7, 95% confidence interval (CI) = 4.5–13.3), the influence of smokey coal (with subtypes of Laibin and Longtan) on lung cancer was significantly stronger (24.8 (95% CI: 12.4–49.6)). |
| Hoshuyama et al. (2006) [56] | Lung cancer | Cohort | Iron and steel manufactories in Anshan, Liaoning Province | 121,846 workers in iron and steel factories | PAHs | PAH exposure was a main risk factor for lung cancer in exposed workers with standardized rate ratios (SRR) of 159 (95% Confidence Interval: 115–219). |
| Nie et al. (2016) [52] | Asthma | Case–control | Homes in Shanghai | 29 children (3-6 years old) with diagnosed asthma as case group and 31 healthy children as control group | PAHs | In comparison to the control group (0.0442 µg/m3), the case group with asthma had considerably higher concentrations of PAHs in their indoor PM2.5 (0.0572 µg/m3). |
| He (2010) [57] | Ability of population learning and memory | Cohort study | Factories in Chongqing | 100 male workers in cock plant of a steel company and 100 male workers of oxygen installation | B[a]P | The occupational exposure of B[a]P for coke oven workers was 0.27–2.47 ug/m3, and it was significantly higher than that for oxygen installation workers (0.025 ug/m3). Tension–Anxiety(T) and Fatigue–Inertia(F) of the Profile of Mood States (POM S) in coke oven employees were substantially greater than in controls (p < 0.05). Compared to the coke oven workers, the scores of the oxygen installation workers were higher in the total digital span, average simple reaction time, the forward digital span, first right dotting, digit symbol, mean right dotting, and mean total dotting, and the differences were statistically significant (p < 0.05). |
| References | Health Outcomes | Types of Study | Settings/Locations | Investigated Population | Indoor Pollutants | Findings |
|---|---|---|---|---|---|---|
| Hu (2017) [74] | Allergic diseases | Case–control | 10 homes in Changsha, Hunan Province | 10 children aged 10–12 years old | DEHP and DBP | The concentrations of DEHP (891 ug/g dust) and DBP (263 ug/g) in allergic children’s homes were higher than those in homes with healthy children (DEHP: 755 ug/g, DBP 200 ug/g). However, the difference was not significant (p > 0.05). |
| Zhang (2016) [73] | Asthma and allergy | A nested case–control | Home in Tianjin municipal and Cangzhou city | 410 children aged 0–8 years old | DEP, DiBP, DnBP, DEHP, BBzP, DiNP | The median concentrations of DEP, DiBP, BBzP, DnBP, DiNP, and DEHP were 0.31 μg/g, 16.38 μg/g, 0.11 μg/g, 42.6 μg/g, 0.28 μg/g, and 127.11 μg/g, respectively, in investigated homes. The adjusted odds ratios (AOR) for children with diagnosed asthma were 2.08 and 2.48, respectively, when the concentrations of DEP and DiBP in dust in urban residential buildings were above 0.33 µg/g and 16.38 µg/g. Children’s dry cough was linked to increased DEP and/or DEHP concentrations in rural areas. |
| Fan et al., (2017) [4] | Respiratory and allergic symptoms | Case–control | Homes in Beijing | Six children (8–12 years old) diagnosed with allergic and respiratory symptoms as case group (group A) and four healthy children as control group (group B) | DEHP, DBP, DBA, DOA, and DEP | The mean concentrations of SVOCs in living rooms and bedrooms of thecontrol group (1590 µg/g and 2347.8 µg/g) were higher than the case group (1347.5 µg/g and 1754 µg/g) in winter. In summer, the mean concentrations of SVOCs in living rooms and bedrooms of the case group were higher than the control group (except one home, and two homes were detected with no SVOCs). |
| Zhang et al. (2016) [6] | Allergy | Case–control | Home in Shanghai | Seven children (9–10 years old) diagnosed with allergic symptoms as case group and five healthy children as control group | DEP, DBP, DEHP, BHT, DBA, DOA, TBP, TCEP, TPP | The concentrations of DEHP and DBP were not substantially different between healthy and allergic children. |
| Sun (2008) [72] | Allergies | A nested case–control | Dormitories at Tianjin University | 209 students diagnosed with allergic symptoms as case group and 227 healthy students as control group | DEP, DiBP, DBP, BBzP, DEHP, and DiNP | The average indoor concentrations of DEP, DiBP, DBP, BBzP, DEHP, and DiNP were 21.38, 23.09, 24.90, 21.75, 48.54, and 31.95 μg/g. The adjusted odds ratio (AOR) for diagnosed rhinitis was 5.03 (1.32–19.14) in the dust of rooms with a concentration above 24.9 μg/g. |
| Zhang (2017) [75] | Eczema, allergic rhinitis | Case–control | 146 Dormitories at Beijing University of Civil Enginering and Architecture. 74 were case rooms and 72 were control rooms | College students lived in these dorm rooms | DBP, DCHP, DiBP, and DEHP | The concentrations of DBP (43–60 μg/g), DCHP (119–155 μg/g), and DEHP (149–181 μg/g) in the dust of allergic students’ dormitories were similar to those in healthy students’ dormitories (DBP 20 μg/g, DCHP 126 μg/g, and DEHP 152 μg/g, respectively). The difference was not significant (p > 0.05). |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ataei, Y.; Sun, Y.; Liu, W.; S. Ellie, A.; Dong, H.; Ahmad, U.M. Health Effects of Exposure to Indoor Semi-Volatile Organic Compounds in Chinese Building Environment: A Systematic Review. Int. J. Environ. Res. Public Health 2023, 20, 678. https://doi.org/10.3390/ijerph20010678
Ataei Y, Sun Y, Liu W, S. Ellie A, Dong H, Ahmad UM. Health Effects of Exposure to Indoor Semi-Volatile Organic Compounds in Chinese Building Environment: A Systematic Review. International Journal of Environmental Research and Public Health. 2023; 20(1):678. https://doi.org/10.3390/ijerph20010678
Chicago/Turabian StyleAtaei, Yeganeh, Yuexia Sun, Wei Liu, Agnes S. Ellie, Hui Dong, and Umme Marium Ahmad. 2023. "Health Effects of Exposure to Indoor Semi-Volatile Organic Compounds in Chinese Building Environment: A Systematic Review" International Journal of Environmental Research and Public Health 20, no. 1: 678. https://doi.org/10.3390/ijerph20010678
APA StyleAtaei, Y., Sun, Y., Liu, W., S. Ellie, A., Dong, H., & Ahmad, U. M. (2023). Health Effects of Exposure to Indoor Semi-Volatile Organic Compounds in Chinese Building Environment: A Systematic Review. International Journal of Environmental Research and Public Health, 20(1), 678. https://doi.org/10.3390/ijerph20010678







