Chronic Effects of Different Types of Neuromuscular Training on Hemodynamic Responses Estimated VO2max, and Walking Performance in Older People
Abstract
1. Introduction
2. Materials and Methods
2.1. Experimental Design
2.2. Training Protocols
2.3. Anthropometric Analyses
2.4. Hemodynamic Analyses
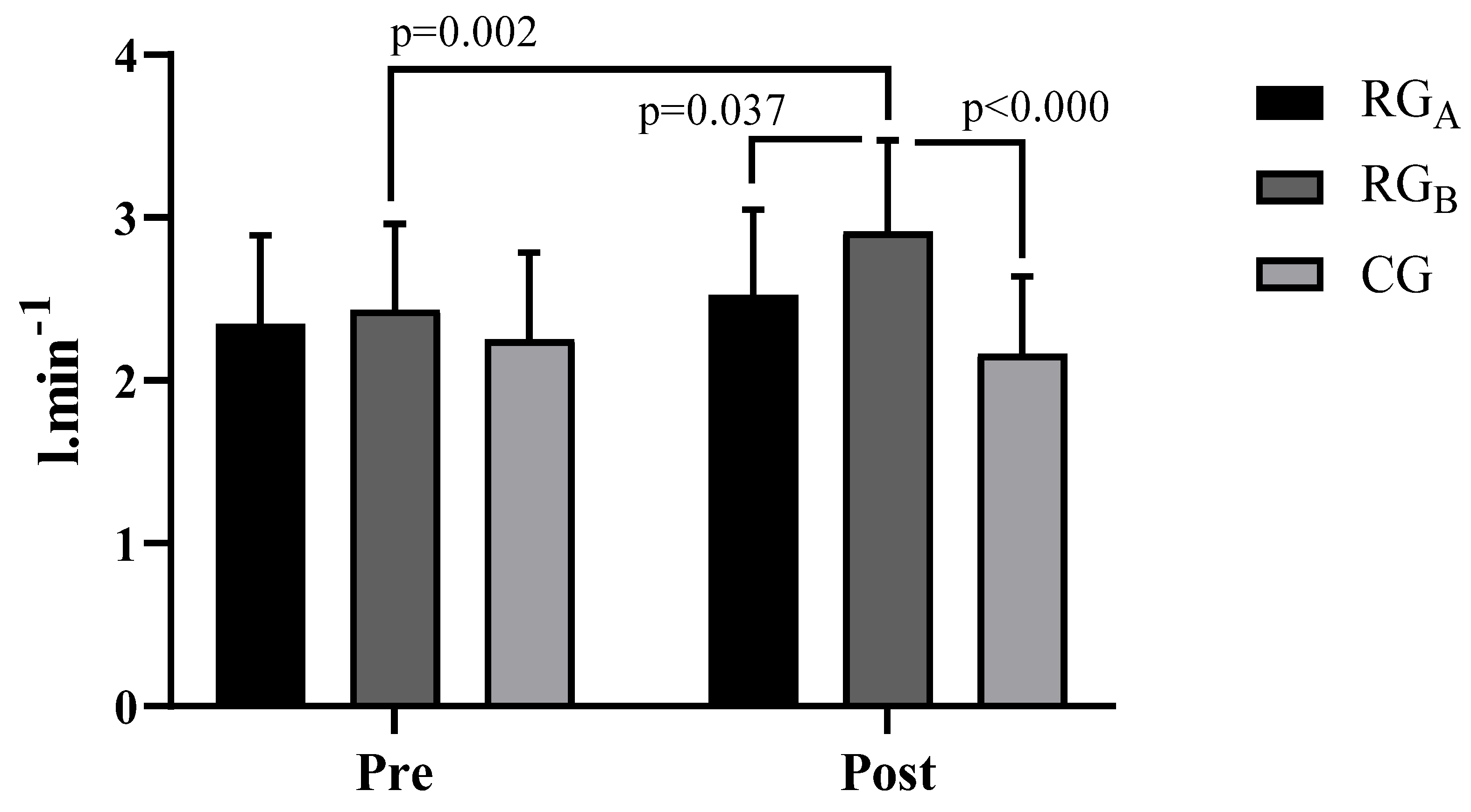
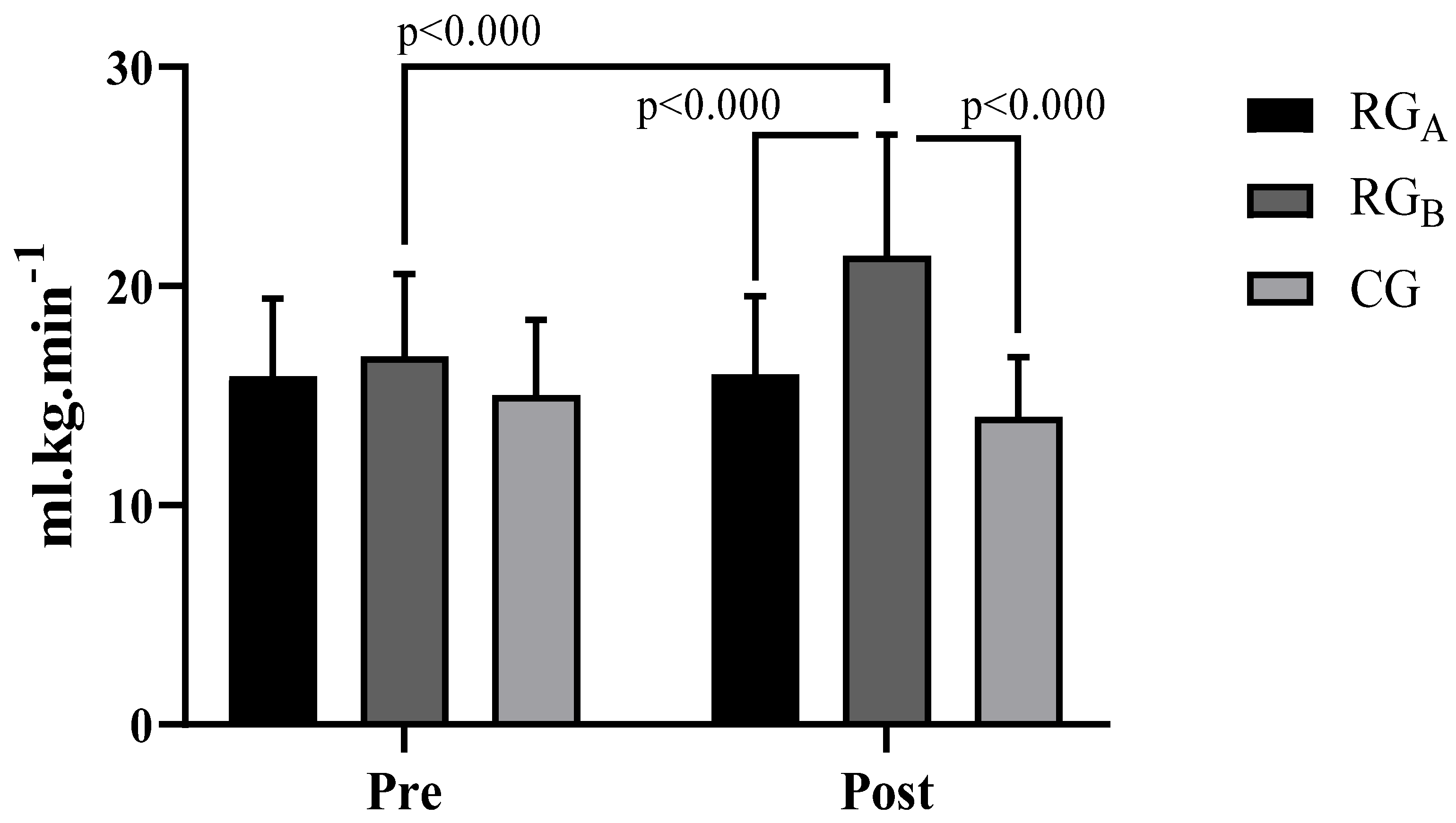
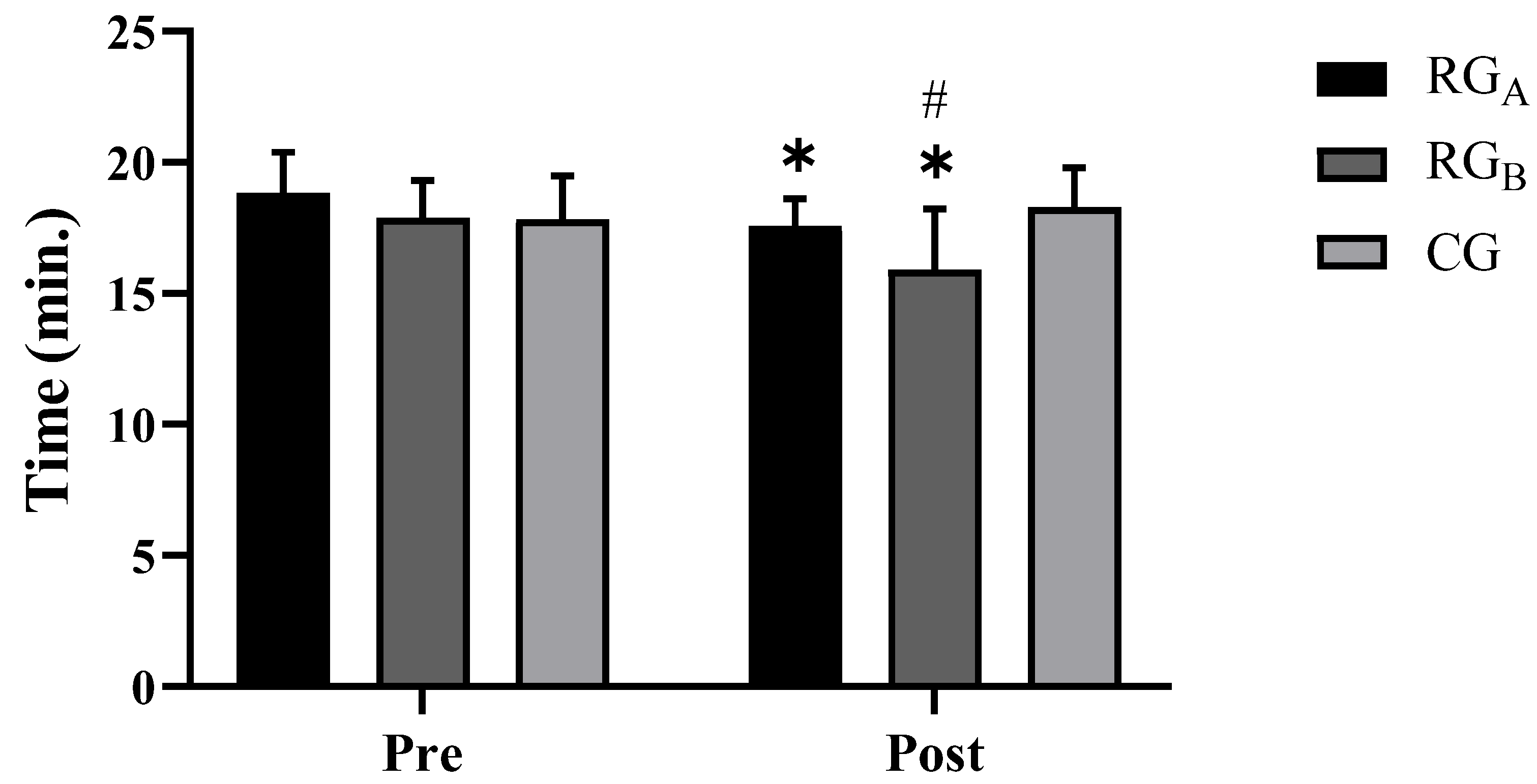
2.5. Maximum Oxygen Uptake Analyses (VO2max) and Walking Performance
2.6. Statistical Analyses
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
References
- Sant’ Ana, L.O.; Machado, S.; Ribeiro, A.A.S.; Reis, N.R.; Campos, Y.A.C.; Silva, J.G.V.; Scartoni, F.R.; Brown, A.F.; Monteiro, E.R.; Novaes, J.S.; et al. Effects of Cardiovascular Interval Training in Healthy Elderly Subjects: A Systematic Review. Front. Physiol. 2020, 11, 739. [Google Scholar] [CrossRef] [PubMed]
- Fraga, M.J.; Cader, S.A.; Ferreira, M.A.; Giani, T.S.; Dantas, E.H.M. Aerobic Resistance, Functional Autonomy and Quality of Life (QoL) of Elderly Women Impacted by a Recreation and Walking Program. Arch. Gerontol. Geriatr. 2011, 52, e40–e43. [Google Scholar] [CrossRef] [PubMed]
- Hoefelmann, C.P.; Benedetti, T.R.B.; Antes, D.L.; Lopes, M.A.; Mazo, G.Z.; Korn, S. Aptidão Funcional de Mulheres Idosas Ativas Com 80 Anos Ou Mais Functional Fitness of Elderly Active Women Aged 80 or More. Mot. Rev. Educ. Fis. 2011, 17, 19–25. [Google Scholar]
- Bondi, D.; Jandova, T.; Ve rratti, V.; D’Amico, M.; Kinel, E.; D’Attilio, M.; Di Filippo, E.S.; Fulle, S.; Pietrangelo, T. Static Balance Adaptations after Neuromuscular Electrical Stimulation on Quadriceps and Lumbar Paraspinal Muscles in Healthy Elderly. Sports Sci. Health 2021, 18, 85–96. [Google Scholar] [CrossRef]
- Ferreira, O.G.L.; Maciel, S.C.; Costa, S.M.G.; Silva, A.O.; Moreira, M. Envelhecimento Ativo e Sua Relação Com a Independência Funcional. Texto Context. enferm 2012, 21, 513–518. [Google Scholar] [CrossRef]
- Cipriani, N.C.S.; Meurer, S.T.; Benedetti, T.R.B.; Lopes, M. Aptidão Funcional de Idosas Praticantes de Atividades Físicas. Rev. Bras. Cineantropometria E Desempenho Hum. 2010, 12, 106–111. [Google Scholar]
- Fletcher, G.F.; Landolfo, C.; Niebauer, J.; Ozemek, C.; Arena, R.; Lavie, C.J. Promoting Physical Activity and Exercise: JACC Health Promotion Series. J. Am. Coll. Cardiol. 2018, 72, 1622–1639. [Google Scholar] [CrossRef]
- Scartoni, F.R.; Rabelo, M.F.P.; Silva, S.N.R.; Sant’Ana, L.O.; Scudese, E.; Ramos, A.M.; Senna, G.W.; Garcia, A.A.; Dantas, E.H.M. Physical Conditioning Index on Active Elderly Population. Biomed. J. Sci. Technol. Res. 2018, 11, 8–11. [Google Scholar] [CrossRef][Green Version]
- Dos Reis, N.R.; Vianna, J.M.; Colugnati, F.B.; da Silva Novaes, J.; Mansur, H.N. Sensitivity and Specificity of SARC-F in the Classification of Sarcopenia in the Elderly: Preliminary Results. Rev. Bras. Fisiol. do Exerc. 2020, 19, 258–266. [Google Scholar] [CrossRef]
- Chodzko Zajko, W.J.; Proctor, D.N.; Fiatarone Singh, M.A.; Minson, C.T.; Nigg, C.R.; Salen, G.J.; Skinner, J.S. American College of Sports Medicine Position Stand. Exercise and Physical Activity for Older Adults. Med. Sci. Sport. Exerc. 2009, 41, 1510–1530. [Google Scholar] [CrossRef]
- Bavaresco Gambassi, B.; dos Santos, C.P.C.; Queiroz, C.; Mesquita, F.; Santos, P.R.; Furtado Almeida, A.E.A.; Schwingel, P.A.; Furtado Almeida, F. de J. Effects of a Four-Exercise Resistance Training Protocol on Functional Parameters in Sedentary Elderly Women. Sport Sci. Health 2020, 16, 99–104. [Google Scholar] [CrossRef]
- Nelson, M.E.; Rejeski, W.J.; Blair, S.N.; Duncan, P.W.; Judge, J.O.; King, A.C.; Al, E. Physical Activity and Public Health in Older Adults: Recommendation From the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1094–1105. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Liu, S.; Wang, K.; Zhang, T.; Yin, L.; Liang, J.; Yang, Y.; Luo, J. Time-Dependent Effects of Physical Activity on Cardiovascular Risk Factors in Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 14194. [Google Scholar] [CrossRef] [PubMed]
- Pescatello, L.S.; Franklin, B.A.; Fagard, R.; Farquhar, W.B.; Kelley, G.A.; Ray, C.A. Exercise and Hypertension-ACSM Position Stand. Med. Sci. Sports Exerc. 2004, 36, 533–553. [Google Scholar] [CrossRef]
- Fragala, M.S.; Cadore, E.L.; Dorgo, S.; Izquierdo, M.; Kraemer, W.J.; Peterson, M.D.; Ryan, E.D. Resistance Training for Older Adults: Position Statement from the National Strength and Conditioning Association. J. Strength Cond. Res. 2019, 33, 8. [Google Scholar] [CrossRef]
- Lee, D.; Artero, E.G.; Sui, X.; Blair, S.N. Mortality Trends in the General Population: The Importance of Cardiorespiratory Fitness. J. Psychopharmacol. 2010, 24, 27–35. [Google Scholar] [CrossRef]
- Jackson, A.S.; Sui, X.; Hebert, J.R.; Church, T.S.; Blair, S.N. Role of Lifestyle and Aging on the Longitudinal Change in Cardiorespiratory Fitness. Arch. Intern. Med. 2009, 169, 1781–1787. [Google Scholar] [CrossRef]
- Saif, M. World Medical Association Declaration of Helsinki: Ethical Principles for Medical Research Involving Human Subjects. Jama 2000, 284, 3043–3045. [Google Scholar]
- WMA World Medical Association. Declaration of Helsinki; WMA World Medical Association: Edinburgh, UK, 2006. [Google Scholar]
- World Health Organization. WHO|Global Nutrition Policy Review 2016–2017; World Health Organization: Geneva, Switzerland, 2018; ISBN 9789241514873. [Google Scholar]
- Dantas, E. Flexibilidade, Alongamento e Flexionamento, 6th ed.; Editora Manole: São Paulo, Brazil, 2017; ISBN 852045447X. [Google Scholar]
- Who, J.; Consultation, F.A.O.E. Diet, Nutrition and the Prevention of Chronic Diseases. World Health Organ Technol. Rep. Ser. 2003, 916, 1–149. [Google Scholar]
- Marfell-Jones, M.; Olds, T.; Stewart, A.; Carter, J.E.L. ISAK: Potchefstroom: International Standards for Anthropometric Assessment; International Society for the Advancement of Kinanthropometry: Potchefstroom, South Africa, 2006. [Google Scholar]
- Ansari, M.; Javadi, H.; Pourbehi, M.; Mogharrabi, M.; Rayzan, M.; Semnani, S.; Jallalat, S.; Amini, A.; Abbaszadeh, M.; Barekat, M. The Association of Rate Pressure Product (RPP) and Myocardial Perfusion Imaging (MPI) Findings: A Preliminary Study. Perfusion 2012, 27, 207–213. [Google Scholar] [CrossRef]
- Topouchian, J.A.; El Assaad, M.A.; Orobinskaia, L.V.; El Feghali, R.N.; Asmar, R.G. Validation of Two Automatic Devices for Self-Measurement of Blood Pressure According to the International Protocol of the European Society of Hypertension: The Omron M6 (HEM-7001-E) and the Omron R7 (HEM 637-IT). Blood Press. Monit. 2006, 11, 165–171. [Google Scholar] [CrossRef] [PubMed]
- Chobanian, A.V. National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee: The Seventh Report of the Joint National. JAMA 2003, 289, 2560–2572. [Google Scholar] [CrossRef] [PubMed]
- Kline, G.M.; Porcari, J.P.; Hintermeister, R.; Freedson, P.S.; Ward, A.; McCarron, R.F.; Ross, J.; Rippe, J.M. Estimation of VO2maxfrom a One-Mile Track Walk, Gender, Age, and Body Weight. Med. Sci. Sports Exerc. 1987, 19, 253–259. [Google Scholar] [CrossRef]
- Marins, J.; Giannichi, R. Avaliação e Prescrição de Atividade Física, 3rd ed.; Shape: Rio de Janeiro, Brazil, 2003. [Google Scholar]
- Quintana, D.S.; Heathers, J.A.J.; Kemp, A.H. On the Validity of Using the Polar RS800 Heart Rate Monitor for Heart Rate Variability Research. Eur. J. Appl. Physiol. 2012, 112, 4179–4180. [Google Scholar] [CrossRef]
- Mota, M.R.; Oliveira, R.J.; Dutra, M.T.; Pardono, E.; Terra, D.T.; Lima, R.M.; Simões, H.G.; Silva, F.M. Acute and Chronic Effects of Resistive Exercise on Blood Pressure in Hypertensive Elderly Women. J. Strength Cond. Res. 2013, 27, 3475–3480. [Google Scholar] [CrossRef]
- Da Cunha Nascimento, D.; Tibana, R.A.; Benik, F.M.; Fontana, K.E.; Neto, F.R.; de Santana, F.S.; Santos-Neto, L.; Silva, R.A.S.; Silva, A.O.; Farias, D.L. Sustained Effect of Resistance Training on Blood Pressure and Hand Grip Strength Following a Detraining Period in Elderly Hypertensive Women: A Pilot Study. Clin. Interv. Aging 2014, 9, 219. [Google Scholar] [CrossRef] [PubMed]
- Da Cunha Nascimento, D.; da Silva, C.R.; Valduga, R.; Saraiva, B.; de Sousa Neto, I.V.; Vieira, A.; Funghetto, S.S.; Silva, A.O.; da Cunha Oliveira, S.; Pereira, G.B. Blood Pressure Response to Resistance Training in Hypertensive and Normotensive Older Women. Clin. Interv. Aging 2018, 13, 541. [Google Scholar] [CrossRef]
- Grgic, J. Use It or Lose It? A Meta-Analysis on the Effects of Resistance Training Cessation (Detraining) on Muscle Size in Older Adults. Int. J. Environ. Res. Public Health 2022, 19. [Google Scholar] [CrossRef]
- Vianna, J.M.; Werneck, F.Z.; Coelho, E.F.; Damasceno, V.O.; Reis, V.M. Oxygen Uptake and Heart Rate Kinetics after Different Types of Resistance Exercise. J. Hum. Kinet. 2014, 42, 235–244. [Google Scholar] [CrossRef]
- Adamson, S.; Kavaliauskas, M.; Yamagishi, T.; Phillips, S.; Lorimer, R.; Babraj, J. Extremely Short Duration Sprint Interval Training Improves Vascular Health in Older Adults. Sports Sci. Health 2019, 15, 123–131. [Google Scholar] [CrossRef]
- Nemoto, K.; Gen-no, H.; Masuki, S.; Okazaki, K.; Nose, H. Effects of High-Intensity Interval Walking Training on Physical Fitness and Blood Pressure in Middle-Aged and Older People. In Proceedings of the Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2007; Volume 82, pp. 803–811. [Google Scholar]
- MacInnis, M.J.; Gibala, M.J. Physiological Adaptations to Interval Training and the Role of Exercise Intensity. J. Physiol. 2017, 595, 2915–2930. [Google Scholar] [CrossRef] [PubMed]


| Resistance Group A (RGA) | Resistance Group B (RGB) | Control Group (CG) | ||||
|---|---|---|---|---|---|---|
| N = 35 (69.08 ± 5.9 Age) | N = 35 (68.6 ± 5.9 Age) | N = 35 (69.4 ± 8.1 Age) | ||||
| Variables | Moment | Moment | Moment | |||
| Pre | Post | Pre | Post | Pre | Post | |
| Weight(kg) | 67.7 ± 11.1 | 67.7 ± 11.1 | 66.9 ± 11.9 | 66.5 ± 11.7 | 68.6 ± 11.1 | 70.3 ± 10.6 |
| Height (cm) | 158.6 ± 8.9 | 159.0 ± 9.1 | 158.2 ± 0.08 | 158.2 ± 0.08 | 163.6 ± 0.07 | 163.6 ± 0.07 |
| BMI (kg/m2) | 27.03 ± 4.04 | 26.8 ± 4.1 | 26.6 ± 3.7 | 26.6 ± 3.7 | 26.08 ± 4.5 | 26.4 ± 4.3 |
| Variables | Groups | |||||
|---|---|---|---|---|---|---|
| Resistance Group A | Resistance Group B | Control Group | ||||
| Moment | Moment | Moment | ||||
| Pre | Post | Pre | Post | Pre | Post | |
| SBP (mm/Hg) | 136.57 ± 17.14 | 122.25 ± 12.83 *† | 142.28 ± 18.32 | 132.85 ± 14.46 | 141.14 ± 17.95 | 142.57 ± 18.04 |
| DBP (mm/Hg) | 85.42 ± 10.93 | 76.12 ± 8.43 *† | 81.42 ± 6.01† | 79.42 ± 6.39 | 82.28 ± 7.70 | 87.42 ± 9.50 |
| HR (bpm) | 86.97 ± 17.07 | 92.64 ± 9.69 † | 97.48 ± 10.67 | 93.60 ± 9.36 † | 105.82 ± 10 | 107.88 ± 9.48 |
| DP (bpm × mm/Hg) | 11,862.28 ± 2658.19 | 11,312.25 ± 1604.50 † | 13,886.85 ± 2459.58 | 12,429.71 ± 1808.27 † | 14,923.42 ± 2291.63 | 14,357.71 ± 2164.50 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dantas, E.H.M.; de Oliveira Sant’Ana, L.; Vianna, J.M.; Machado, S.; Bezerra, J.C.P.; Corey, M.T.; Scartoni, F.R. Chronic Effects of Different Types of Neuromuscular Training on Hemodynamic Responses Estimated VO2max, and Walking Performance in Older People. Int. J. Environ. Res. Public Health 2023, 20, 640. https://doi.org/10.3390/ijerph20010640
Dantas EHM, de Oliveira Sant’Ana L, Vianna JM, Machado S, Bezerra JCP, Corey MT, Scartoni FR. Chronic Effects of Different Types of Neuromuscular Training on Hemodynamic Responses Estimated VO2max, and Walking Performance in Older People. International Journal of Environmental Research and Public Health. 2023; 20(1):640. https://doi.org/10.3390/ijerph20010640
Chicago/Turabian StyleDantas, Estélio Henrique Martin, Leandro de Oliveira Sant’Ana, Jeferson Macedo Vianna, Sergio Machado, Jani Cleria Pereira Bezerra, Matthew T. Corey, and Fabiana Rodrigues Scartoni. 2023. "Chronic Effects of Different Types of Neuromuscular Training on Hemodynamic Responses Estimated VO2max, and Walking Performance in Older People" International Journal of Environmental Research and Public Health 20, no. 1: 640. https://doi.org/10.3390/ijerph20010640
APA StyleDantas, E. H. M., de Oliveira Sant’Ana, L., Vianna, J. M., Machado, S., Bezerra, J. C. P., Corey, M. T., & Scartoni, F. R. (2023). Chronic Effects of Different Types of Neuromuscular Training on Hemodynamic Responses Estimated VO2max, and Walking Performance in Older People. International Journal of Environmental Research and Public Health, 20(1), 640. https://doi.org/10.3390/ijerph20010640








