Testing the Multiple Disadvantage Model of Health with Ethnic Asian Children: A Secondary Data Analysis
Abstract
1. Introduction
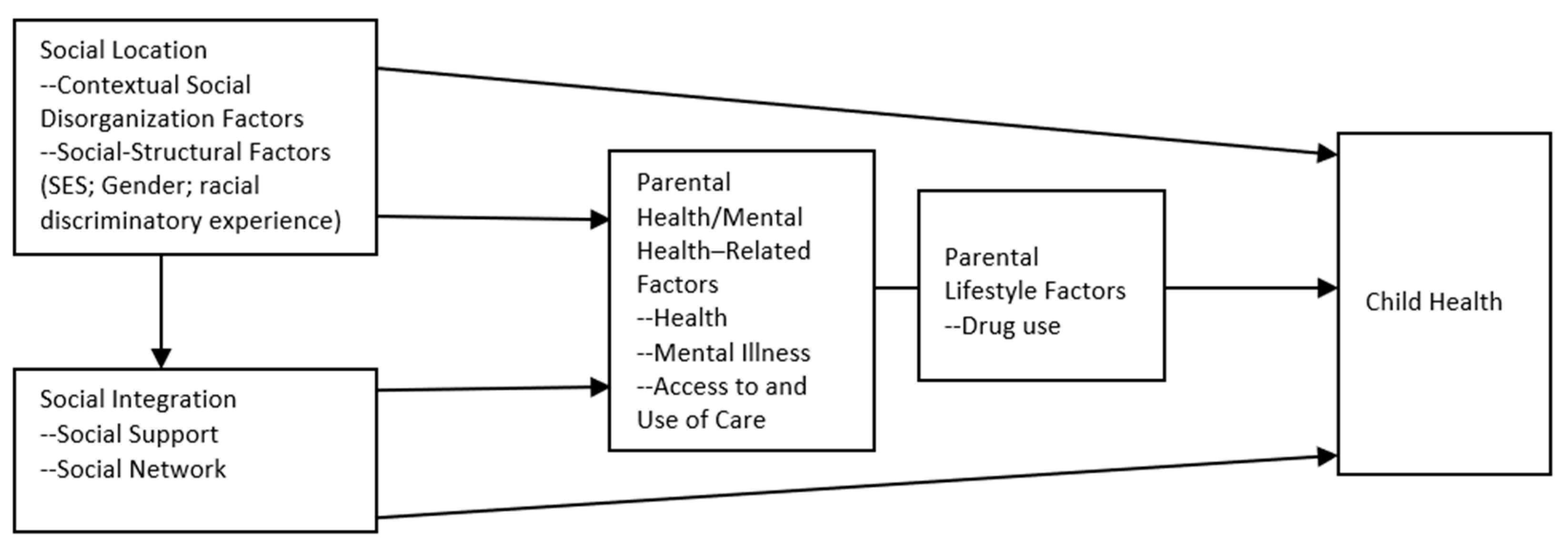
1.1. Multiple Disadvantage Model
1.1.1. Social Disorganization
1.1.2. Social Structural Factors
1.1.3. Social Relationships
1.1.4. Parental Health
1.1.5. Medical Insurance
1.2. Acculturation
1.3. Hypotheses
- Health among ethnic Asian children will be associated positively with safe neighborhood, family income, parents’ educational attainment, parents’ employment, family support, social support, parents’ health, medical coverage, TANF or SNAP enrollment, parents’ birth in U.S., children’s birth in U.S., and families’ English proficiency.
- Health among ethnic Asian children will be associated negatively with rundown neighborhood, discrimination experience, and single-mother household.
2. Methods
2.1. Sample
2.2. Measures
2.3. Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fan, Y.L.; Chen, Q. Family functioning as a mediator between neighborhood conditions and children’s health: Evidence from a national survey in the United States. Soc. Sci. Med. 2012, 74, 1939–1947. [Google Scholar] [CrossRef] [PubMed]
- Stevens, G.D. Gradients in the health status and developmental risks of young children: The combined influences of multiple social risk factors. Matern. Child Health J. 2006, 10, 187–199. [Google Scholar] [CrossRef] [PubMed]
- Larson, K.; Russ, S.A.; Crall, J.J.; Halfon, N. Influence of multiple social risks on children’s health. Pediatrics 2008, 121, 337–344. [Google Scholar] [CrossRef] [PubMed]
- Bauman, L.J.; Silver, E.J.; Stein, R.E.K. Cumulative social disadvantage and child health. Pediatrics 2006, 117, 1321–1328. [Google Scholar] [CrossRef]
- Wen, M. Parental Participation in Religious Services and Parent and Child Well-Being: Findings from the National Survey of America’s Families. J. Relig. Health 2014, 53, 1539–1561. [Google Scholar] [CrossRef]
- Singh, G.K.; Yu, S.M.; Kogan, M.D. Health, Chronic Conditions, and Behavioral Risk Disparities Among US Immigrant Children and Adolescents. Public Health Rep. 2013, 128, 463–479. [Google Scholar] [CrossRef]
- Flores, G.; Lin, H. Trends in racial/ethnic disparities in medical and oral health, access to care, and use of services in US children: Has anything changed over the years? Int. J. Equity Health 2013, 12, 10. [Google Scholar] [CrossRef]
- Flores, G.; Tomany-Korman, S.C. The language spoken at home and disparities in medical and dental health, access to care, and use of services in US children. Pediatrics 2008, 121, E1703–E1714. [Google Scholar] [CrossRef]
- Yu, S.M.; Huang, Z.J.H.; Schwalberg, R.H.; Overpeck, M.D.; Kogan, M.D. Association of language spoken at home with health and school issues among Asian American adolescents. J. Sch. Health 2002, 72, 192–198. [Google Scholar] [CrossRef]
- Rappaport, E.B.; Robbins, J.M. Overweight in southeastern Pennsylvania children: 2002 household health survey data. Public Health Rep. 2005, 120, 525–531. [Google Scholar] [CrossRef]
- Mehta, N.K.; Lee, H.; Ylitalo, K.R. Child health in the United States: Recent trends in racial/ethnic disparities. Soc. Sci. Med. 2013, 95, 6–15. [Google Scholar] [CrossRef] [PubMed]
- Brewer, M.; Kimbro, R.T.; Denney, J.T.; Osiecki, K.M.; Moffett, B.; Lopez, K. Does neighborhood social and environmental context impact race/ethnic disparities in childhood asthma? Health Place 2017, 44, 86–93. [Google Scholar] [CrossRef] [PubMed]
- Melius, J. Overweight and Obesity in Minority Children and Implications for Family and Community Social Work. Soc. Work Public Health 2013, 28, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.K.; Siahpush, M.; Kogan, M.D. Rising Social Inequalities in US Childhood Obesity, 2003-2007. Ann. Epidemiol. 2010, 20, 40–52. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.C.; Lo, C.C. Racial Disparities in Children’s Health: A Longitudinal Analysis of Mothers Based on the Multiple Disadvantage Model. J. Community Health 2016, 41, 753–760. [Google Scholar] [CrossRef] [PubMed]
- Cheng, T.C.; Li, Q. Adolescent delinquency in child welfare system: A multiple disadvantage model. Child. Youth Serv. Rev. 2017, 73, 205–212. [Google Scholar] [CrossRef]
- Cheng, T.C.; Lo, C.C. Social risk and protective factors in adolescents’ reduction and cessation of alcohol use. Subst. Use Misuse 2017, 52, 916–928. [Google Scholar] [CrossRef]
- Li, Q.; Cheng, C.T. New evidence in physical violent behaviors among school-aged children: A multiple disadvantages model. Child. Youth Serv. Rev. 2017, 81, 301–308. [Google Scholar] [CrossRef]
- Kedia, S.K.; Schmidt, M.; Dillon, P.J.; Arshad, H.; Yu, X. Substance use treatment in Appalachian Tennessee amid COVID-19: Challenges and preparing for the future. J. Subst. Abus. Treat. 2021, 124, 108270. [Google Scholar] [CrossRef]
- Lo, C.C.; Howell, R.J.; Cheng, T.C. Explaining Black-White Differences in Homicide Victimization. Aggress. Violent Behav. 2013, 18, 125–134. [Google Scholar] [CrossRef]
- Cheng, T.C.; Lo, C.C. Racial disparities in intimate partner violence and in seeking help with mental health. J. Interpers. Violence 2015, 30, 3283–3307. [Google Scholar] [CrossRef] [PubMed]
- Lo, C.C.; Howell, R.J.; Cheng, T.C. Racial Disparities in Age at Time of Homicide Victimization: A Test of the Multiple Disadvantage Model. J. Interpers. Violence 2015, 30, 152–167. [Google Scholar] [CrossRef] [PubMed]
- Priest, N.; Paradies, Y.; Trenerry, B.; Truong, M.; Karlsen, S.; Kelly, Y. A systematic review of studies examining the relationship between reported racism and health and wellbeing for children and young people. Soc. Sci. Med. 2013, 95, 115–127. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.B.; Posick, C.; Vaughn, M.G. New Evidence of The Nexus Between Neighborhood Violence, Perceptions Of Danger, And Child Health. Health Aff. 2019, 38, 746–754. [Google Scholar] [CrossRef] [PubMed]
- Zuberi, A.; Teixeira, S. Child health in low-income neighborhoods: The unexpected relationship with neighborhood disorder and other aspects of distress. J. Community Psychol. 2017, 45, 459–472. [Google Scholar] [CrossRef]
- Diez Roux, A.V.; Mair, C. Neighborhoods and health. Ann. N. Y. Acad. Sci. 2010, 1186, 125–145. [Google Scholar] [CrossRef] [PubMed]
- Schreier, H.M.C.; Chen, E. Socioeconomic Status and the Health of Youth: A Multilevel, Multidomain Approach to Conceptualizing Pathways. Psychol. Bull. 2013, 139, 606–654. [Google Scholar] [CrossRef]
- Christian, H.; Zubrick, S.R.; Foster, S.; Giles-Corti, B.; Bull, F.; Wood, L.; Knuiman, M.; Brinkman, S.; Houghton, S.; Boruff, B. The influence of the neighborhood physical environment on early child health and development: A review and call for research. Health Place 2015, 33, 25–36. [Google Scholar] [CrossRef]
- Fortson, J.G.; Sanbonmatsu, L. Child Health and Neighborhood Conditions Results from a Randomized Housing Voucher Experiment. J. Hum. Resour. 2010, 45, 840–864. [Google Scholar] [CrossRef]
- Gonzales, F.A.; Jones, R.R.; Deardorff, J.; Windham, G.C.; Hiatt, R.A.; Kushi, L.H. Neighborhood deprivation, race/ethnicity, and urinary metal concentrations among young girls in California. Environ. Int. 2016, 91, 29–39. [Google Scholar] [CrossRef]
- Chen, E.; Martin, A.D.; Matthews, K.A. Understanding health disparities: The role of race and socioeconomic status in children’s health. Am. J. Public Health 2006, 96, 702–708. [Google Scholar] [CrossRef] [PubMed]
- Cook, W.K.; Tseng, W. Associations of Asian Ethnicity and Parental Education with Overweight in Asian American Children and Adolescents: An Analysis of 2011–2016 National Health and Nutrition Examination Surveys. Matern. Child Health J. 2019, 23, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Chatterji, P.; Markowitz, S.; Brooks-Gunn, J. Effects of early maternal employment on maternal health and well-being. J. Popul. Econ. 2013, 26, 285–301. [Google Scholar] [CrossRef] [PubMed]
- Kuhlthau, K.A.; Perrin, J.M. Child health status and parental employment. Arch. Pediatr. Adolesc. Med. 2001, 155, 1346–1350. [Google Scholar] [CrossRef] [PubMed]
- Minkovitz, C.S.; O’Campo, P.J.; Chen, Y.H.; Grason, H.A. Associations between maternal and child health status and patterns of medical care use. Ambul. Pediatr. 2002, 2, 85–92. [Google Scholar] [CrossRef] [PubMed]
- Larson, K.; Halfon, N. Family Income Gradients in the Health and Health Care Access of US Children. Matern. Child Health J. 2010, 14, 332–342. [Google Scholar] [CrossRef]
- Currie, J.; Lin, W.C. Chipping away at health: More on the relationship between income and child health. Health Aff. 2007, 26, 331–344. [Google Scholar] [CrossRef]
- de Cuba, S.A.E.; Bovell-Ammon, A.R.; Cook, J.T.; Coleman, S.M.; Black, M.M.; Chilton, M.M.; Casey, P.H.; Cutts, D.B.; Heeren, T.C.; Sandel, M.T.; et al. SNAP, Young Children’s Health, and Family Food Security and Healthcare Access. Am. J. Prev. Med. 2019, 57, 525–532. [Google Scholar] [CrossRef]
- Reichman, N.E.; Corman, H.; Noonan, K. Effects of child health on sources of public support. South. Econ. J. 2006, 73, 136–156. [Google Scholar] [CrossRef]
- McConnell, D.; Breitkreuz, R.; Savage, A. From financial hardship to child difficulties: Main and moderating effects of perceived social support. Child Care Health Dev. 2011, 37, 679–691. [Google Scholar] [CrossRef]
- Chen, E.; Hayen, R.; Le, V.; Austin, M.K.; Shalowitz, M.U.; Story, R.E.; Miller, G.E. Neighborhood Social Conditions, Family Relationships, and Childhood Asthma. Pediatrics 2019, 144, e20183300. [Google Scholar] [CrossRef] [PubMed]
- Leininger, L.J.; Ryan, R.M.; Kalil, A. Low-income mothers’ social support and children’s injuries. Soc. Sci. Med. 2009, 68, 2113–2121. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.J.; Fuller, T. Neighborhood Disorder and Paternal Involvement of Nonresident and Resident Fathers. Fam. Relat. 2012, 61, 501–513. [Google Scholar] [CrossRef]
- Bass, L.E.; Warehime, M.N. Family Structure and Child Health Outcomes in the United States. Sociol. Inq. 2011, 81, 527–548. [Google Scholar] [CrossRef] [PubMed]
- Wong, M.S.; Showell, N.N.; Bleich, S.N.; Gudzune, K.A.; Chan, K.S. The association between parent-reported provider communication quality and child obesity status: Variation by parent obesity and child race/ethnicity. Patient Educ. Couns. 2017, 100, 1588–1597. [Google Scholar] [CrossRef] [PubMed]
- Lanuza, Y.R. Words and Hugs: Emotional Support for Latino and Asian Children of Immigrants Compared to their White Counterparts with Native-Born Parentage. Race Soc. Probl. 2020, 12, 112–132. [Google Scholar] [CrossRef]
- Ellingsen, R.; Baker, B.L.; Blacher, J.; Crnic, K. Resilient parenting of preschool children at developmental risk. J. Intellect. Disabil. Res. 2014, 58, 664–678. [Google Scholar] [CrossRef]
- Hardie, J.H.; Landale, N.S. Profiles of Risk: Maternal Health, Socioeconomic Status, and Child Health. J. Marriage Fam. 2013, 75, 651–666. [Google Scholar] [CrossRef]
- Akobirshoev, I.; Bowser, D.; Parish, S.L.; Thomas, C.; Bachman, S.S. Does Parental Health Mediate the Relationship between Parental Uninsurance and Insured Children’s Health Outcomes? Evidence from a US National Survey. Health Soc. Work 2017, 42, E68–E76. [Google Scholar] [CrossRef]
- Zea, M.C.; Asner-Self, K.K.; Birman, D.; Buki, L.P. The Abbreviated Multidimensional Acculturation Scale: Empirical Validation with Two Latino/Latina Samples. Cult. Divers. Ethn. Minor. Psychol. 2003, 9, 107–126. [Google Scholar] [CrossRef]
- Guerrero, A.D.; Ponce, N.A.; Chung, P.J. Obesogenic Dietary Practices of Latino and Asian Subgroups of Children in California: An Analysis of the California Health Interview Survey, 2007–2012. Am. J. Public Health 2015, 105, E105–E112. [Google Scholar] [CrossRef] [PubMed]
- Chomitz, V.R.; Lee, V.; Must, A.; Chui, K.K.H.; Brown, A. Healthy Living Behaviors Among Chinese-American Preschool-Aged Children: Results of a Parent Survey. J. Immigr. Minor. Health 2018, 20, 926. [Google Scholar] [CrossRef] [PubMed]
- McGee, S.A.; Luz, C. Nativity as a Determinant of Health Disparities Among Children. J. Immigr. Minor. Health 2018, 20, 517–528. [Google Scholar] [CrossRef] [PubMed]
- Hore, P.; Ahmed, M.S.; Sedlar, S.; Saper, R.B.; Nagin, D.; Clark, N. Blood Lead Levels and Potential Risk Factors for Lead Exposures Among South Asians in New York City. J. Immigr. Minor. Health 2017, 19, 1322–1329. [Google Scholar] [CrossRef]
- Ragavan, M.I.; Li, W.D.; Elwy, A.R.; Cowden, J.D.; Bair-Merritt, M. Chinese, Vietnamese, and Asian Indian Parents’ Perspectives About Well-Child Visits: A Qualitative Analysis. Acad. Pediatr. 2018, 18, 628–635. [Google Scholar] [CrossRef] [PubMed]
- Child and Adolescent Health Measurement Initiative. 2018 National Survey of Children’s Health: SPSS Codebook for Data Users; U.S. Department of Health and Human Services: Washington, DC, USA, 2020. [Google Scholar]
- Tummala-Narra, P.; Sathasivam-Rueckert, N. The Experience of Ethnic and Racial Group Membership Among Immigrant-Origin Adolescents. J. Adolesc. Res. 2016, 31, 299–342. [Google Scholar] [CrossRef]
- Zhang, H. Re-defining stigmatization: Intersectional stigma of single mothers in Thailand. J. Fam. Stud. 2022, 1–27. [Google Scholar] [CrossRef]
- Subramaniam, M.; Prasad, R.O.; Abdin, E.; Vaingankar, J.A.; Chong, S.A. Single Mothers Have a Higher Risk of Mood Disorders. Ann. Acad. Med. Singap. 2014, 43, 145–151. [Google Scholar] [CrossRef]
- Pan, E.L.; Farrell, M.P. Ethnic differences in the effects of intergenerational relations on adolescent problem behavior in US single-mother families. J. Fam. Issues 2006, 27, 1137–1158. [Google Scholar] [CrossRef]
- Dukes, R.L.; Portillos, E.; Miles, M. Models of satisfaction with police service. Polic. Int. J. Police Strateg. Manag. 2009, 32, 297–318. [Google Scholar] [CrossRef]
- De Marco, A.; Vernon-Feagans, L. Rural Neighborhood Context, Child Care Quality, and Relationship to Early Language Development. Early Educ. Dev. 2013, 24, 792–812. [Google Scholar] [CrossRef] [PubMed]
| Frequency | Percent | M | IQR | |
|---|---|---|---|---|
| Outcome variable | ||||
| Child health (excellent/very good/good) | 1331 | 98.6 | N/A | N/A |
| (fair/poor) | 19 | 1.4 | N/A | N/A |
| Explanatory variables | ||||
| Rundown neighborhood (yes) | 350 | 25.9 | N/A | N/A |
| (no) | 1000 | 74.1 | N/A | N/A |
| Racial discrimination (yes) | 84 | 6.2 | N/A | N/A |
| (no) | 1266 | 93.8 | N/A | N/A |
| Safe neighborhood | N/A | N/A | 4 | 1 |
| Parent educational attainment | N/A | N/A | 7 | 8 |
| Employed parent (yes) | 1106 | 81.9 | N/A | N/A |
| (no) | 244 | 18.1 | N/A | N/A |
| Family income-to-poverty ratio (%) | N/A | N/A | 390 | 199 |
| Receipt of TANF (yes) | 16 | 1.2 | N/A | N/A |
| (no) | 1334 | 98.8 | N/A | N/A |
| Receipt of SNAP (yes) | 58 | 4.3 | N/A | N/A |
| (no) | 1292 | 95.7 | N/A | N/A |
| Single mother (yes) | 77 | 43.7 | N/A | N/A |
| (no) | 1273 | 56.3 | N/A | N/A |
| Family cohesiveness | N/A | N/A | 7 | 2 |
| Family support (yes) | 700 | 51.9 | N/A | N/A |
| (no) | 650 | 48.1 | N/A | N/A |
| Professional support (yes) | 221 | 16.4 | N/A | N/A |
| (no) | 1129 | 83.6 | N/A | N/A |
| Peer/religious group support (yes) | 255 | 18.9 | N/A | N/A |
| (no) | 1095 | 81.1 | N/A | N/A |
| Neighbor support | N/A | N/A | 10 | 3 |
| Parent health (excellent/very good/good) | 1303 | 96.5 | N/A | N/A |
| (fair/poor) | 47 | 3.5 | N/A | N/A |
| Insured (yes) | 1282 | 95.0 | N/A | N/A |
| (no) | 68 | 5.0 | N/A | N/A |
| Parent born in U.S. (yes) | 281 | 20.8 | N/A | N/A |
| (no) | 1069 | 79.2 | N/A | N/A |
| Child born in U.S. (yes) | 1059 | 78.4 | N/A | N/A |
| (no) | 291 | 21.6 | N/A | N/A |
| Speaks English at home (yes) | 825 | 61.1 | N/A | N/A |
| (no) | 525 | 38.9 | N/A | N/A |
| Parent age (years) | N/A | N/A | 44 | 10 |
| Child age (years) | N/A | N/A | 10 | 9 |
| Girl | 687 | 50.9 | N/A | N/A |
| Boy | 663 | 49.1 | N/A | N/A |
| Variables | OR | RSE | 90% Confidence-Interval |
|---|---|---|---|
| Rundown neighborhood (no) | 0.73 | 0.57 | 0.20–2.65 |
| Racial discrimination (no) | 2.27 | 2.35 | 0.41–12.43 |
| Safe neighborhood | 2.35 * | 1.17 | 1.03–5.33 |
| Parent educational attainment | 0.76 | 0.13 | 0.57–1.00 |
| Employed parent (no) | 0.76 | 0.84 | 0.12–4.71 |
| Family income-to-poverty ratio | 1.01 ** | 0.00 | 1.00–1.01 |
| Receipt of TANF (no) | 275.79 * | 739.56 | 3.35–22,708.61 |
| Receipt of SNAP (no) | 0.27 | 0.29 | 0.05–1.59 |
| Single mother (no) | 0.09 ** | 0.08 | 0.02–0.40 |
| Family cohesiveness | 2.17 ** | 0.49 | 1.50–3.14 |
| Family support (no) | 15.20 * | 20.20 | 1.71–135.23 |
| Professional support (no) | 0.35 | 0.45 | 0.04–2.90 |
| Peer/religious group support (no) | 0.28 | 0.38 | 0.03–2.58 |
| Neighbor support | 1.01 | 0.16 | 0.78–1.30 |
| Parent health (fair/poor) | 4.35 | 4.77 | 0.72–26.40 |
| Insured (no) | 3.74 | 3.04 | 0.98–14.26 |
| Parent born in U.S. (no) | 0.74 | 0.76 | 0.14–4.01 |
| Child born in U.S. (no) | 1.31 | 1.10 | 0.33–5.21 |
| Speaks English at home (no) | 2.52 | 2.35 | 0.54–11.66 |
| Parent age | 0.97 | 0.07 | 0.86–1.09 |
| Child age | 0.97 | 0.10 | 0.82–1.16 |
| Girl (boy) | 0.39 | 0.24 | 0.14–1.08 |
| Wald’s χ2 = | 71.15 ** |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cheng, T.C.; Lo, C.C. Testing the Multiple Disadvantage Model of Health with Ethnic Asian Children: A Secondary Data Analysis. Int. J. Environ. Res. Public Health 2023, 20, 483. https://doi.org/10.3390/ijerph20010483
Cheng TC, Lo CC. Testing the Multiple Disadvantage Model of Health with Ethnic Asian Children: A Secondary Data Analysis. International Journal of Environmental Research and Public Health. 2023; 20(1):483. https://doi.org/10.3390/ijerph20010483
Chicago/Turabian StyleCheng, Tyrone C., and Celia C. Lo. 2023. "Testing the Multiple Disadvantage Model of Health with Ethnic Asian Children: A Secondary Data Analysis" International Journal of Environmental Research and Public Health 20, no. 1: 483. https://doi.org/10.3390/ijerph20010483
APA StyleCheng, T. C., & Lo, C. C. (2023). Testing the Multiple Disadvantage Model of Health with Ethnic Asian Children: A Secondary Data Analysis. International Journal of Environmental Research and Public Health, 20(1), 483. https://doi.org/10.3390/ijerph20010483






