Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest
Abstract
1. Introduction
2. Materials and Methods
Statistical Methods
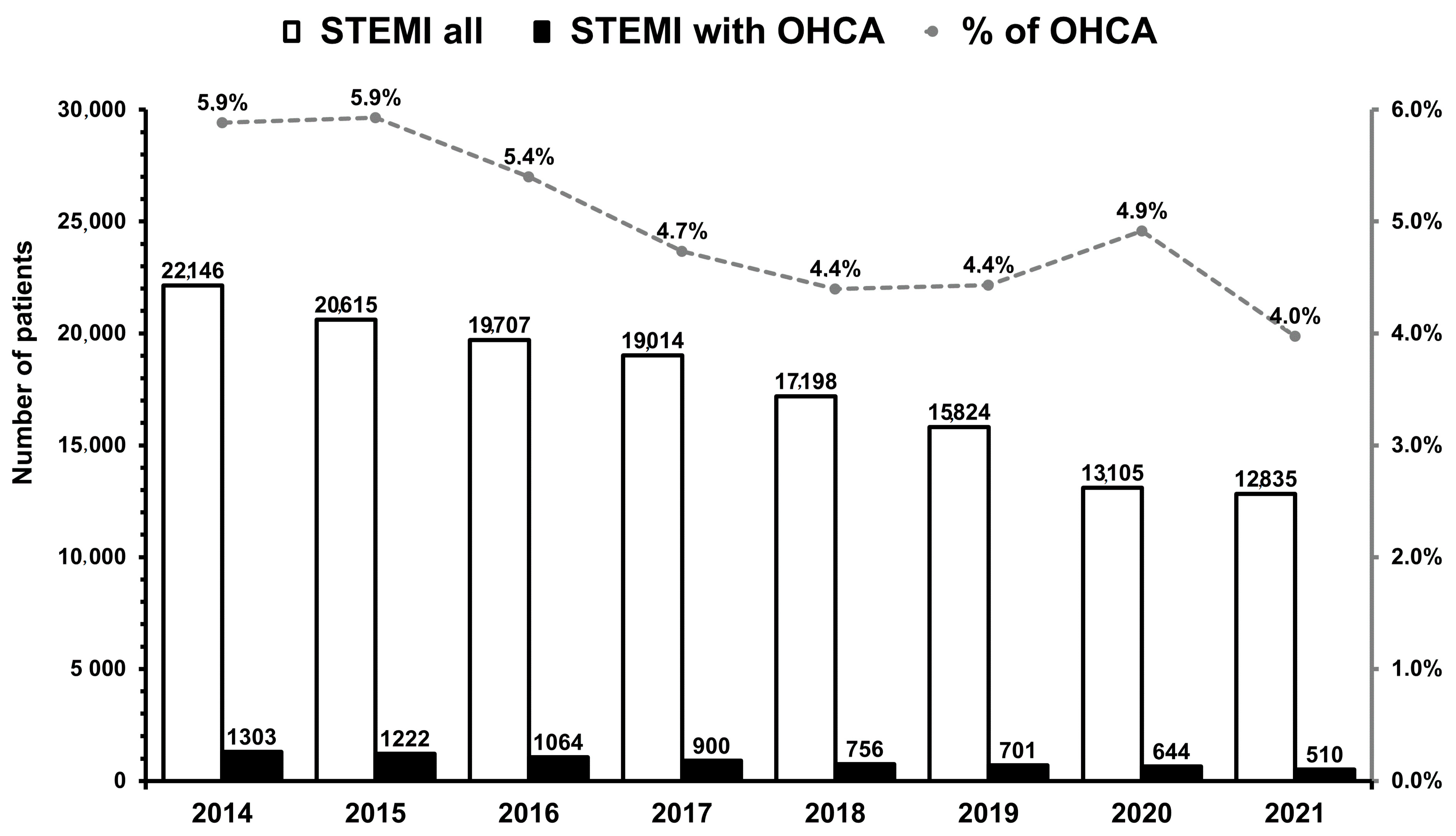
3. Results
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Baldi, E.; Cortegiani, A.; Savastano, S. Cardiac arrest and coronavirus disease 2019. Curr. Opin. Crit. Care 2022, 1, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Cammann, V.L.; Templin, C. The STEMI phenomenon during the COVID-19 pandemic: What is beneath the tip of the iceberg? Heart 2022, 108, 412–413. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Dziewierz, A.; Malinowski, K.P.; Rakowski, T.; Bartuś, S.; Dudek, D.; Siudak, Z. Treatment Delay and Clinical Outcomes in Patients with ST-Segment Elevation Myocardial Infarction during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 3920. [Google Scholar] [CrossRef] [PubMed]
- Kanecki, K.; Nitsch-Osuch, A.; Goryński, P.; Wojtyniak, B.; Juszczyk, G.; Magdalena, B.; Kosińska, I.; Tyszko, P. Coronavirus disease 2019 (COVID-19) among hospitalized patients in Poland: A study based on a national hospital registry. Pol. Arch. Intern. Med. 2021, 131, 535–540. [Google Scholar] [CrossRef] [PubMed]
- Siudak, Z.; Dudek, D.; Grygier, M.; Araszkiewicz, A.; Dąbrowski, M.; Kusa, J.; Hawranek, M.; Huczek, Z.; Kralisz, P.; Roleder, T.; et al. Interventional cardiology in Poland in 2020—Impact of the COVID-19 pandemic. Annual summary report of the Association of Cardiovascular Interventions of the Polish Cardiac Society and Jagiellonian University Medical College. Adv. Interv. Cardiol. 2021, 17, 131–134. [Google Scholar] [CrossRef] [PubMed]
- Kaziród-Wolski, K.; Sielski, J.; Sidło, J.; Januszek, R.; Siudak, Z. The Most Relevant Factors Affecting the Perioperative Death Rate in Patients with Acute Coronary Syndrome and COVID-19, Based on Annual Follow-Up in the ORPKI Registry. Biomedicines 2021, 9, 1813. [Google Scholar] [CrossRef]
- Scquizzato, T.; D’Amico, F.; Rocchi, M.; Saracino, M.; Stella, F.; Landoni, G.; Zangrillo, A. Impact of COVID-19 Pandemic on Out-of-Hospital Cardiac Arrest System-of-Care: A Systematic Review and Meta-Analysis. Prehosp. Emerg. Care 2021, 1, 12. [Google Scholar] [CrossRef]
- Ciszewski, A. Will the COVID-19 pandemic accelerate the implementation of single-day coronary angioplasty in Poland? Adv. Interv. Cardiol. 2020, 16, 184–186. [Google Scholar] [CrossRef]
- Bhatt, A.S.; Varshney, A.S.; Goodrich, E.L.; Gong, J.; Ginder, C.; Senman, B.C.; Johnson, M.; Butler, K.; Woolley, A.E.; de Lemos, J.A.; et al. Epidemiology and Management of ST-Segment-Elevation Myocardial Infarction in Patients With COVID-19: A Report from the American Heart Association COVID-19 Cardiovascular Disease Registry. J. Am. Heart Assoc. 2022, 11, e024451. [Google Scholar] [CrossRef]
- Gitto, M.; Novelli, L.; Reimers, B.; Condorelli, G.; Stefanini, G.G. Specific characteristics of STEMI in COVID-19 patients and their practical implications. Kardiol. Pol. 2022, 80, 266–277. [Google Scholar] [CrossRef]
- Bujak, K.; Nadolny, K.; Ładny, J.R.; Hudzik, B.; Zyśko, D.; Trzeciak, P.; Gąsior, M. Epidemiology, management, and survival rate of out-of-hospital cardiac arrest in Upper Silesia, Poland: An Utstein-style report. Adv. Interv. Cardiol. 2021, 7, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Siudak, Z.; Tokarek, T.; Dziewierz, A.; Wysocki, T.; Wiktorowicz, A.; Legutko, J.; Żmudka, K.; Dudek, D.; Zbigniew, S.; Tomasz, T.; et al. Reduced periprocedural mortality and bleeding rates of radial approach in ST-segment elevation myocardial infarction. Propensity score analysis of data from the ORPKI Polish National Registry. EuroIntervention 2017, 13, 843–850. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Jaroszyńska, A.; Bartuś, S.; Siudak, Z. Percutaneous coronary intervention during on- and off-hours in patients with ST-segment elevation myocardial infarction. Hellenic J. Cardiol. 2021, 62, 212–218. [Google Scholar] [CrossRef] [PubMed]
- Dziewierz, A.; Siudak, Z.; Tokarek, T.; Rakowski, T.; Dudek, D. Determinants of stroke following percutaneous coronary intervention in acute myocardial infarction (from ORPKI Polish National Registry). Int. J. Cardiol. 2016, 223, 236–238. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Januszek, R.; Zabojszcz, M.; Janion-Sadowska, A.; Dudek, D.; Siudak, Z. Comparison of safety and effectiveness between the right and left radial artery approach in percutaneous coronary intervention (English edition). Rev. Esp. Cardiol. 2022, 75, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Tokarek, T.; Dziewierz, A.; Plens, K.; Rakowski, T.; Dudek, D.; Siudak, Z. Radial approach reduces mortality in patients with ST-segment elevation myocardial infarction and cardiogenic shock. Pol. Arch. Intern. Med. 2021, 131, 421–428. [Google Scholar]
- Dudek, D.; Siudak, Z.; Grygier, M.; Araszkiewicz, A.; Dąbrowski, M.; Kusa, J.; Hawranek, M.; Huczek, Z.; Kralisz, P.; Roleder, T.; et al. Interventional cardiology in Poland in 2019. Summary report of the Association of Cardiovascular Interventions of the Polish Cardiac Society (AISN PTK) and Jagiellonian University Medical College. Adv. Interv. Cardiol. 2020, 16, 123–126. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Scientific Document Group; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar]
- Tokarek, T.; Siudak, Z.; Dziewierz, A.; Rakowski, T.; Krycińska, R.; Siwiec, A.; Dudek, D. Clinical outcomes in nonagenarians undergoing a percutaneous coronary intervention: Data from the ORPKI Polish National Registry 2014-2016. Coron. Artery Dis. 2018, 29, 573–578. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized bleeding definitions for cardiovascular clinical trials: A consensus report from the Bleeding Academic Research Consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]
- Garcia, S.; Dehghani, P.; Stanberry, L.; Grines, C.; Patel, R.; Nayak, K.R.; Singh, A.; Htun, W.W.; Kabour, A.; Ghasemzadeh, N.; et al. Initial Findings from the North American COVID-19 Myocardial Infarction Registry. J. Am. Coll. Cardiol. 2021, 77, 1994–2003. [Google Scholar] [CrossRef] [PubMed]
- Kovach, C.P.; Perman, S.M. Impact of the COVID-19 pandemic on cardiac arrest systems of care. Curr. Opin. Crit. Care 2021, 27, 239–245. [Google Scholar] [CrossRef] [PubMed]
- Teoh, S.E.; Masuda, Y.; Tan, D.; Liu, N.; Morrison, L.J.; Ong, M.; Blewer, A.L.; Ho, A. Impact of the COVID-19 pandemic on the epidemiology of out-of-hospital cardiac arrest: A systematic review and meta-analysis. Ann. Intensive Care 2021, 11, 169. [Google Scholar] [CrossRef] [PubMed]
- Bielski, K.; Szarpak, A.; Jaguszewski, M.J.; Kopiec, T.; Smereka, J.; Gasecka, A.; Wolak, P.; Nowak-Starz, G.; Chmielewski, J.; Rafique, Z.; et al. The Influence of COVID-19 on Out-Hospital Cardiac Arrest Survival Outcomes: An Updated Systematic Review and Meta-Analysis. J. Clin. Med. 2021, 10, 5573. [Google Scholar] [CrossRef]
- Baert, V.; Jaeger, D.; Hubert, H.; Lascarrou, J.B.; Debaty, G.; Chouihed, T.; Javaudin, F.; GR RéAC. Assessment of changesin cardiopulmonary resuscitation practices and outcomes on 1005 victims of out-of-hospital cardiac arrest during the COVID-19 outbreak: Registry-based study. Scand. J. Trauma Resusc. Emerg. Med. 2020, 28, 119. [Google Scholar] [CrossRef]
- Lim, Z.J.; Ponnapa Reddy, M.; Afroz, A.; Billah, B.; Shekar, K.; Subramaniam, A. Incidence and outcome of out-of hospital cardiac arrests in the COVID-19 era: A systematic review and metaanalysis. Resuscitation 2020, 157, 248–258. [Google Scholar] [CrossRef]
- Dehghani, P.; Schmidt, C.W.; Garcia, S.; Okeson, B.; Grines, C.L.; Singh, A.; Patel, R.A.G.; Wiley, J.; Htun, W.W.; Nayak, K.R.; et al. North American COVID-19 Myocardial Infarction (NACMI) Risk Score for Prediction of In-Hospital Mortality. J. Soc. Cardiovasc. Angiogr. Interv. 2022, 1, 100404. [Google Scholar] [CrossRef]
- Rodríguez-Leor, O.; Cid-Álvarez, B.; Pérez de Prado, A.; Rossello, X.; Ojeda, S.; Serrador, A.; López-Palop, R.; Martín-Moreiras, J.; Rumoroso, J.R.; Cequier, Á.; et al. Impact of COVID-19 on ST-segment elevation myocardial infarction care. The Spanish experience. Rev. Esp. Cardiol. (Engl. Ed.) 2020, 73, 994–1002. [Google Scholar] [CrossRef]
- Rangé, G.; Hakim, R.; Beygui, F.; Angoulvant, D.; Marcollet, P.; Godin, M.; Deballon, R.; Bonnet, P.; Fichaux, O.; Barbey, C.; et al. Incidence, delays, and outcomes of STEMI during COVID-19 outbreak: Analysis from the France PCI registry. J. Am. Coll. Emerg. Physicians Open 2020, 1, 1168–1176. [Google Scholar] [CrossRef]
- Riyapan, S.; Chantanakomes, J.; Roongsaenthong, P.; Tianwibool, P.; Wittayachamnankul, B.; Supasaovapak, J.; Pansiritanachot, W. Impact of the COVID-19 outbreak on out-of-hospital cardiac arrest management and outcomes in a low-resource emergency medical service system: A perspective from Thailand. Int. J. Emerg. Med. 2022, 15, 26. [Google Scholar] [CrossRef]
- Rollman, J.E.; Kloner, R.A.; Bosson, N.; Niemann, J.T.; Gausche-Hill, M.; Williams, M.; Clare, C.; Tan, W.; Wang, X.; Shavelle, D.M.; et al. Emergency Medical Services Responses to Out-of-Hospital Cardiac Arrest and Suspected ST-Segment-Elevation Myocardial Infarction during the COVID-19 Pandemic in Los Angeles County. J. Am. Heart Assoc. 2021, 10, e019635. [Google Scholar] [CrossRef] [PubMed]
- Chew, N.; Ow, Z.; Teo, V.; Heng, R.; Ng, C.H.; Lee, C.H.; Low, A.F.; Chan, M.Y.; Yeo, T.C.; Tan, H.C.; et al. The Global Effect of the COVID-19 Pandemic on STEMI Care: A Systematic Review and Meta-analysis. Can. J. Cardiol. 2021, 37, 1450–1459. [Google Scholar] [CrossRef] [PubMed]
- Partyński, B.; Tokarek, T.; Dziewierz, A.; Dykla., D.; Januszek, R.; Dudek, D. Impact of basic life support training on knowledge of cardiac patients about first aid for out-of-hospital cardiac arrest. J. Public Health 2021, 173, 1–6. [Google Scholar] [CrossRef]

| Variable | Before COVID-19 (n = 740) | During COVID-19 (n = 740) | p-Value |
|---|---|---|---|
| Male gender | 512 (69.2%) | 525 (70.9%) | 0.5 |
| Age [years] | 63.8 (±12.4) | 64.3 (±12.2) | 0.6 |
| Diabetes mellitus | 111 (15%) | 132 (17.8%) | 0.2 |
| Previous stroke | 36 (4.9%) | 29 (3.9%) | 0.5 |
| Previous MI | 93 (12.6%) | 96 (13%) | 0.3 |
| Previous CABG | 12 (1.6%) | 14 (1.9%) | 0.8 |
| Previous PCI | 83 (11.2%) | 87 (11.8%) | 0.8 |
| Smoking | 238 (32.2%) | 220 (29.7%) | 0.4 |
| Arterial hypertension | 377 (50.9%) | 385 (52%) | 0.8 |
| Chronic kidney disease | 27 (3.6%) | 32 (4.3%) | 0.6 |
| Chronic obstructive Pulmonary disease | 21 (2.8%) | 19 (2.6%) | 0.9 |
| Killip-Kimball class | |||
| I | 323 (43.6%) | 304 (41.1%) | 0.7 |
| II | 133 (18%) | 134 (18.1%) | 0.7 |
| III | 54 (7.3%) | 63 (8.5%) | 0.7 |
| IV | 230 (31.1%) | 239 (32.3%) | 0.7 |
| Direct transport | 316 (42.7%) | 297 (40.1%) | 0.3 |
| Variable | Before COVID-19 (n = 740) | During COVID-19 (n = 740) | p-Value |
|---|---|---|---|
| Single-vessel disease | 325 (43.9%) | 317 (42.8%) | 0.8 |
| LMCA only | 5 (0.7%) | 5 (0.7%) | 0.8 |
| Multivessel disease without LMCA | 328 (44.3%) | 345 (46.6%) | 0.8 |
| Multivessel disease with LMCA | 82 (11.1%) | 73 (9.9%) | 0.8 |
| TIMI 0 or 1 flow before PCI | 599 (80.9%) | 590 (79.7%) | 0.8 |
| TIMI 3 flow after PCI | 623 (84.2%) | 626 (84.6%) | 0.9 |
| Variable | Before COVID-19 (n = 740) | During COVID-19 (n = 740) | p-Value |
|---|---|---|---|
| Site volume ≥400 PCI in the current year | 701 (94.7%) | 692 (93.5%) | 0.4 |
| Radial approach during angiography | 420 (56.8%) | 436 (58.9%) | 0.6 |
| Radial approach during PCI | 412 (55.7%) | 428 (57.8%) | 0.7 |
| PCI operator annual volume (PCI during 2014–2021) | 172.9 (±94.3) | 170.7 (±103.6) | 0.8 |
| PCI operator radial experience (2014–2021) [% of all performed PCI] | 82 (±14.6) | 82.6 (±13.7) | 0.4 |
| Total amount of contrast, [ml] | 158 (±62) | 158 (±66) | 0.9 |
| Total radiation dose, [mGy] | 750 (±590) | 740 (±740) | 0.8 |
| Aspiration thrombectomy during PCI | 113 (15.3%) | 107 (14.5%) | 0.7 |
| Rotablation during PCI | 3 (0.4%) | 5 (0.4%) | 0.9 |
| P2Y12 inhibitors before and during PCI | |||
| Clopidogrel | 455 (61.5%) | 459 (62%) | 0.9 |
| Ticagrelor | 273 (36.9%) | 270 (36.5%) | 0.9 |
| Prasugrel | 12 (1.6%) | 11 (1.5%) | 0.9 |
| GPI IIb/IIIa during PCI | 225 (30.4%) | 237 (32%) | 0.5 |
| Unfractionated heparin during PCI | 636 (85.9%) | 630 (85.1%) | 0.7 |
| Low-molecular-weight heparins during PCI | 6 (0.8%) | 8 (1.1%) | 0.8 |
| Bivalirudin during PCI | 8 (1.1%) | 7 (0.9%) | 0.9 |
| Variable | Before COVID-19 (n = 740) | During COVID-19 (n = 740) | p-Value |
|---|---|---|---|
| Time from pain to first medical contact, minutes | 118.5 (±173.6) | 126.5 (±197.5) | 0.4 |
| Time from pain to angiography, minutes | 207.3 (±192.8) | 227.9 (±231.4) | 0.06 |
| Time from first medical contact to angiography, minutes | 88.8 (±61.5) | 101.4 (±109.8) | 0.006 |
| Time from first medical contact to angiography <90 minutes, % | 286 (38.6%) | 283 (38.2%) | 0.9 |
| Time from first medical contact to angiography <120 minutes, % | 161 (21.8%) | 168 (22.7%) | 0.7 |
| Variable | Before COVID-19 (n = 740) | During COVID-19 (n = 740) | p-Value |
|---|---|---|---|
| Dissection of coronary artery | 0 (0.0%) | 1 (0.1%) | 0.9 |
| Coronary artery perforation | 3 (0.4%) | 1 (0.1%) | 0.6 |
| No-reflow | 20 (2.7%) | 19 (2.6%) | 0.9 |
| Periprocedural stroke | 0 | 0 | - |
| Bleeding at the puncture site | 2 (0.3%) | 2 (0.3%) | 0.9 |
| Allergic reaction | 0 | 0 | - |
| Cardiac arrest | 64 (8.6%) | 47 (6.4%) | 0.1 |
| Periprocedural death | 45 (6.1%) | 32 (4.3%) | 0.2 |
| Periprocedural myocardial infarction | 0 | 0 | - |
| Any complication | 103 (13.9%) | 82 (11.1%) | 0.1 |
| Any complication or death | 91 (12.3%) | 73 (9.9%) | 0.2 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tokarek, T.; Dziewierz, A.; Zeliaś, A.; Malinowski, K.P.; Rakowski, T.; Dudek, D.; Siudak, Z. Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest. Int. J. Environ. Res. Public Health 2023, 20, 337. https://doi.org/10.3390/ijerph20010337
Tokarek T, Dziewierz A, Zeliaś A, Malinowski KP, Rakowski T, Dudek D, Siudak Z. Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest. International Journal of Environmental Research and Public Health. 2023; 20(1):337. https://doi.org/10.3390/ijerph20010337
Chicago/Turabian StyleTokarek, Tomasz, Artur Dziewierz, Aleksander Zeliaś, Krzysztof Piotr Malinowski, Tomasz Rakowski, Dariusz Dudek, and Zbigniew Siudak. 2023. "Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest" International Journal of Environmental Research and Public Health 20, no. 1: 337. https://doi.org/10.3390/ijerph20010337
APA StyleTokarek, T., Dziewierz, A., Zeliaś, A., Malinowski, K. P., Rakowski, T., Dudek, D., & Siudak, Z. (2023). Impact of COVID-19 Pandemic on Patients with ST-Segment-Elevation Myocardial Infarction Complicated by Out-of-Hospital Cardiac Arrest. International Journal of Environmental Research and Public Health, 20(1), 337. https://doi.org/10.3390/ijerph20010337








