Critical Care Providers’ Moral Distress: Frequency, Burden, and Potential Resources
Abstract
1. Introduction
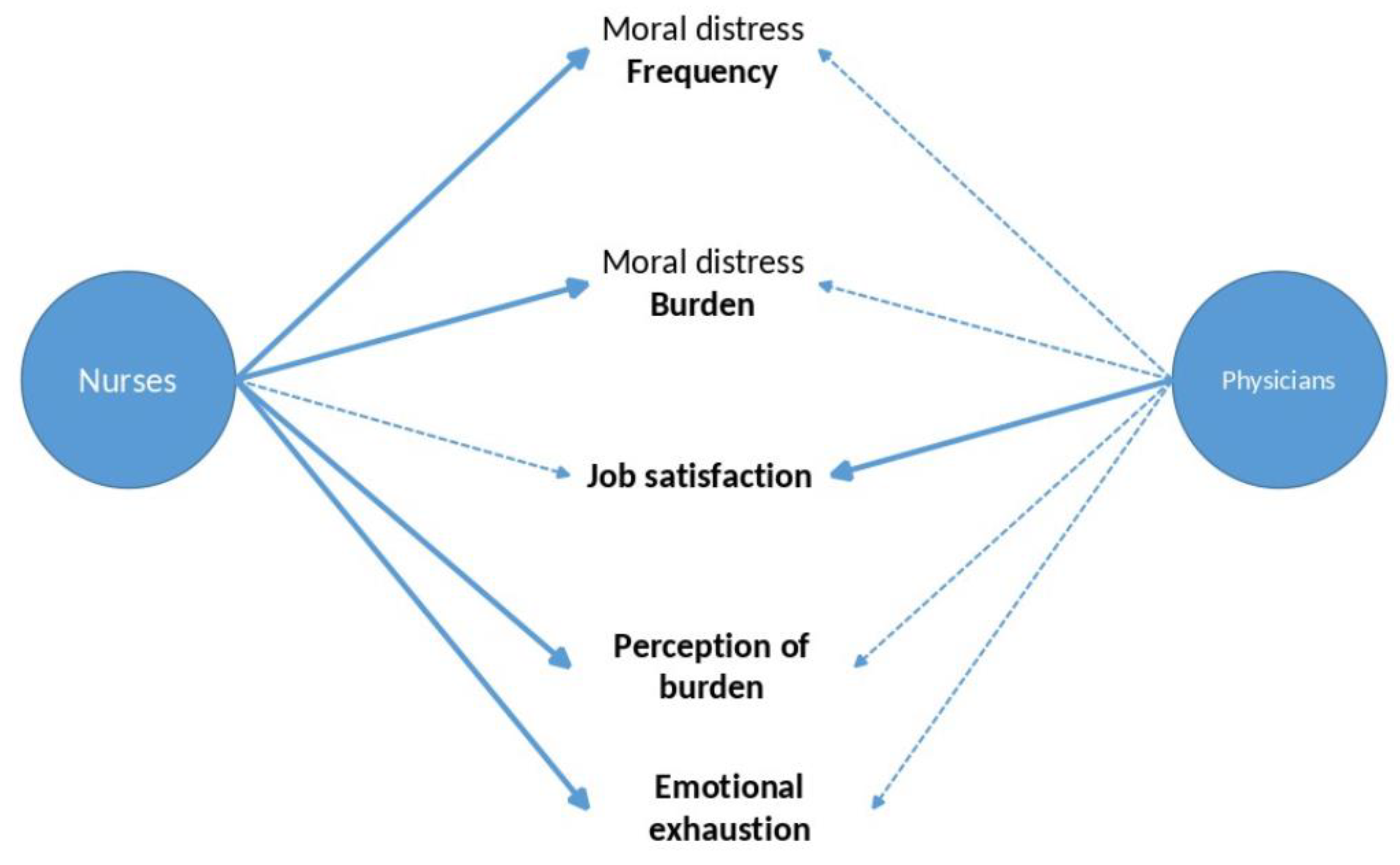
- Which situations were perceived as particularly burdensome?
- Do nurses and physicians differ in their perceptions of MD?
- What are the predictors of MD frequency and burden?
- Does spirituality mitigate or enhance CCPs’ MD?
2. Methods
2.1. Description of Participants
2.2. Measures
2.2.1. Moral Distress
2.2.2. Job Burden
2.2.3. Professional Satisfaction
2.2.4. Spiritual Attitudes and Behaviours
- (1)
- Search (for Support/Access): Cronbach’s alpha = 0.91; 5 items, e.g., F1.5—My situation has led me to deal intensively with spiritual or religious questions again; F1.6—I am convinced that my situation can be positively influenced if I can find access to a spiritual source; F1.9—I am looking for access to spirituality/religiousness.
- (2)
- Trust (in Higher Guidance/Source): Cronbach’s alpha = 0.91; 5 items, e.g., F37—Due to my (stressful) life situation, I get to think about what is really important to me in my life; F38—I have faith in spiritual guidance in my life; F39—I feel connected to a “higher source”.
- (3)
- Reflection (Positive Interpretation of Disease): Cronbach’s alpha = 0.86; 5 items, e.g., F3.3—What happens to me is a clue to change something in my life; F3.4—Due to my (stressful) situation, I am able to deal more with myself again; F3.7—I see my (stressful) life situation as an opportunity for my personal development.
2.2.5. Statistical Analyses
3. Results
3.1. Description of Participants
3.2. Moral Distress Scale
3.3. Perceived Stress in Specific Situations
3.4. MD and Perceived Stress in the Study Group
3.5. Correlations between MD, Stress, and Work-Associated Indicators
3.6. Predictors of MD Perceptions
4. Discussion
- Both physicians and nurses perceived similar situations as burdensome, e.g., insufficient shift staffing, insufficient competence of employees, lack of continuity, and organizational or financial pressures.
- The frequency of conflicting clinical situations provoking MD was similar for physicians and nurses, although more burdensome for nurses.
- The best predictor of both the frequency and burden of MD was emotional exhaustion, with further influences of work satisfaction and being a nurse for the frequency of MD perception. Being a nurse, experience in ICU/ED, and being of male gender were further predictors of the burden caused by MD.
- Being a non-believer predicted the frequency of MD perception. Participants’ underlying spirituality (in terms of the search for spirituality, religious trust, frequency of meditation or praying, and self-assessment of being a believer) was only marginally associated with MD.
4.1. MD in Different Professional Groups: Frequency, Burden, and Components [52]
4.2. MD Predictors and Practical Consequences
5. Limitations
6. Conclusions
7. Key Messages
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CCP | Critical care provider |
| ED | Emergency Department |
| ICU | Intensive Care Unit |
| MD | Moral Distress |
| MDI | Moral Distress Intensity |
| MDS | Moral Distress Scale |
| R | Religion |
| Sp | Spirituality |
References
- Anantham, D.; Chai-Lim, C.; Zhou, J.X.; Phua, G.C. Operationalization of critical care triage during a pandemic surge using protocolized communication and integrated supportive care. J. Intensive Care 2020, 8, 59. [Google Scholar] [CrossRef] [PubMed]
- Sugrue, E. Understanding the effect of moral transgressions in the helping professions: In search of conceptual clarity. Soc. Serv. Rev. 2019, 93, 4–25. [Google Scholar] [CrossRef]
- Jameton, A. Nursing Practice: The Ethical Issues; Prentice-Hall: Englewood Cliffs, NJ, USA, 1984. [Google Scholar]
- Shay, J. Moral injury. Psychoanal. Psychol. 2014, 31, 182. [Google Scholar] [CrossRef]
- Kissane, D.W.; Clarke, D.M.; Street, A.F. Demoralization syndrome—A relevant psychiatric diagnosis for palliative care. J. Pall. Care 2001, 17, 12–21. [Google Scholar] [CrossRef]
- Ada, H.M.; Dehom, S.; D’Errico, E.; Boyd, K.; Taylor, E.J. Sanctification of work and hospital nurse employment outcomes: An observational study. J. Nurs. Manag. 2021, 29, 442–450. [Google Scholar] [CrossRef]
- Jones, K.A.; Freijah, I.; Carey, L.; Carleton, R.N.; Devenish-Meares, P.; Dell, L.; Rodrigues, S.; Madden, K.; Johnson, L.; Hosseiny, F.; et al. Moral injury, chaplaincy and mental health provider approaches to treatment: A scoping review. J. Relig. Health 2022, 61, 1051–1094. [Google Scholar] [CrossRef]
- Carletto, S.; Ariotti, M.C.; Garelli, G.; Di Noto, L.; Berchialla, P.; Malandrone, F.; Guardione, R.; Boarino, F.; Campagnoli, M.F.; Savant Levet, P.; et al. Moral distress and burnout in neonatal intensive care unit healthcare providers: A cross-sectional study in Italy. Int. J. Environ. Res. Public Health 2022, 19, 8526. [Google Scholar] [CrossRef]
- Kubitza, J.; Große, G.; Schütte-Nütgen, K.; Frick, E. Influence of spirituality on moral distress and resilience among critical care staff in the era of the Covid 19 pandemic: A scoping review. Intensive Crit. Care Nurs. 2023, in press. [CrossRef]
- Vranas, K.C.; Golden, S.E.; Nugent, S.; Valley, T.S.; Schutz, A.; Duggal, A.; Seitz, K.P.; Chang, S.Y.; Slatore, C.G.; Sullivan, D.R.; et al. The influence of the COVID-19 pandemic on intensivists’ well-being: A qualitative study. Chest 2022, 162, 331–345. [Google Scholar] [CrossRef]
- Siddiqui, S. Building organizational and individual resilience in times of moral distress. J. Crit. Care 2022, 67, 184–185. [Google Scholar] [CrossRef]
- Riedel, P.-L.; Kreh, A.; Kulcar, V.; Lieber, A.; Juen, B. A scoping review of moral stressors, moral distress and moral injury in healthcare workers during COVID-19. Int. J. Environ. Res. Public Health 2022, 19, 1666. [Google Scholar] [CrossRef] [PubMed]
- Niven, A.S.; Sessler, C.N. Supporting Professionals in Critical Care Medicine: Burnout, Resiliency, and System-Level Change. Clin. Chest Med. 2022, 43, 563–577. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.C.; Rankin, L. COVID-19: Update on health care workers’ mental health and coping during the pandemic. Crit. Care Nurs. Q. 2022, 45, 22–24. [Google Scholar] [CrossRef] [PubMed]
- Guttormson, J.L.; Calkins, K.; McAndrew, N.; Fitzgerald, J.; Losurdo, H.; Loonsfoot, D. Critical care nurses’ experiences during the COVID-19 pandemic: A US national survey. Am. J. Crit. Care 2022, 31, 96–103. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Marvaldi, M.; Thomas, I.; Lachal, J.; Carretier, E.; Moro, M.R.; Benoit, L. The experience of anaesthesiology care providers in temporary intensive care units during the COVID-19 pandemic in France: A qualitative study. Anaesth. Crit. Care Pain Med. 2022, 41, 101061. [Google Scholar] [CrossRef] [PubMed]
- Grasso, C.; Massidda, D.; Maslak, K.Z.; Favara-Scacco, C.; Grasso, F.A.; Bencivenga, C.; Confalone, V.; Lampugnani, E.; Moscatelli, A.; Somaini, M.; et al. Moral distress in healthcare providers who take care of critical pediatric patients throughout Italy-Cultural adaptation and validation of the Italian pediatric instrument. Int. J. Environ. Res. Public Health 2022, 19, 3880. [Google Scholar] [CrossRef]
- Gee, P.M.; Weston, M.J.; Harshman, T.; Kelly, L.A. Beyond Burnout and Resilience: The Disillusionment Phase of COVID-19. AACN Adv. Crit. Care 2022, 33, 134–142. [Google Scholar] [CrossRef]
- Carton, A.M.; Steinhardt, K.; Cordwell, J. Exploring factors which contribute to the resilience of nurses working in the neonatal care unit: A grounded theory study. Intensive Crit. Care Nurs. 2022, 68, 103137. [Google Scholar] [CrossRef]
- Siber-Sanderowitz, S.; Limowski, A.R.; Gallo, L.; Schneider, M.; Pimentel, S.; Mueller, S.; Rego, S.; Alpert, J. Mobilizing a psychiatric crisis response to COVID-19 for NYC hospital workers: Lessons learned from the mental health front lines. Gen. Hosp. Psychiat. 2022, 74, 141–143. [Google Scholar] [CrossRef]
- Maben, J.; Conolly, A.; Abrams, R.; Rowland, E.; Harris, R.; Kelly, D.; Kent, B.; Couper, K. ‘You can’t walk through water without getting wet’ UK nurses’ distress and psychological health needs during the COVID-19 pandemic: A longitudinal interview study. Int. J. Nurs. Stud. 2022, 131, 104242. [Google Scholar] [CrossRef]
- LeClaire, M.; Poplau, S.; Linzer, M.; Brown, R.; Sinsky, C. Compromised integrity, burnout, and intent to leave the job in critical care nurses and physicians. Crit. Care Explor. 2022, 4, e0629. [Google Scholar] [CrossRef] [PubMed]
- Clari, M.; Gonella, S.; Gatti, P.; Garzaro, G.; Paleologo, M.; Cortese, C.G.; Dimonte, V. Multi-level analysis of individual and work environment factors associated with nurses’ perceived emotional exhaustion. Appl. Nurs. Res. 2022, 63, 151514. [Google Scholar] [CrossRef] [PubMed]
- Blumberg, D.M.; Papazoglou, K.; Schlosser, M.D. Moral distress and ethical exhaustion. In The POWER Manual: A Step-by-Step Guide to Improving Police Officer Wellness, Ethics, and Resilience; American Psychological Association: Washington, DC, USA, 2022; pp. 153–165. [Google Scholar]
- Barr, P. Dimensions of the burnout measure: Relationships with shame- and guilt-proneness in neonatal intensive care unit nurses. Aust. Crit. Care 2022, 35, 174–180. [Google Scholar] [CrossRef] [PubMed]
- Moll, V.; Meissen, H.; Pappas, S.; Xu, K.; Rimawi, R.; Buchman, T.G.; Fisher, L.; Bakshi, V.; Zellinger, M.; Coopersmith, C.M. The Coronavirus Disease 2019 pandemic impacts burnout syndrome differently among multiprofessional critical care clinicians-A longitudinal survey study. Crit. Care Med. 2022, 50, 440. [Google Scholar] [CrossRef] [PubMed]
- Kok, N.; Van Gurp, J.; van der Hoeven, J.G.; Fuchs, M.; Hoedemaekers, C.; Zegers, M. Complex interplay between moral distress and other risk factors of burnout in ICU professionals: Findings from a cross-sectional survey study. BMJ Qual. Saf. 2021. [Google Scholar] [CrossRef]
- Ghazanfari, M.J.; Emami Zeydi, A.; Panahi, R.; Ghanbari, R.; Jafaraghaee, F.; Mortazavi, H.; Karkhah, S. Moral distress in nurses: Resources and constraints, consequences, and interventions. Clin. Ethics 2021, 17, 265–271. [Google Scholar] [CrossRef]
- Alzailai, N.; Barriball, L.; Xyrichis, A. Burnout and job satisfaction among critical care nurses in Saudi Arabia and their contributing factors: A scoping review. Nurs. Open 2021, 8, 2331–2344. [Google Scholar] [CrossRef]
- Clark, P.; Hulse, B.; Povlika, B.J. Resilience, moral distress, and job satisfaction driving engagement in emergency department nurses: A qualitative analysis. J. Nurs. Admin. 2022, 52, 112–117. [Google Scholar] [CrossRef]
- Sheppard, K.N.; Runk, B.G.; Maduro, R.S.; Fancher, M.; Mayo, A.N.; Wilmoth, D.D.; Morgan, M.K.; Zimbro, K.S. Nursing moral distress and intent to leave employment during the COVID-19 pandemic. J. Nurs. Care Qual. 2022, 37, 28–34. [Google Scholar] [CrossRef]
- Magnavita, N.; Soave, P.M.; Antonelli, M. A one-year prospective study of work-related mental health in the intensivists of a COVID-19 hub hospital. Int. J. Environ. Res. Public Health 2021, 18, 9888. [Google Scholar] [CrossRef]
- Maximiano Faraco, M.; Lima Gelbcke, F.; Brehmer, L.C.d.F.; Ramos, F.R.S.; Ghizoni Schneider, D. Moral distress-associated sociodemographic and occupational aspects in nursing managers at federal university hospitals. Rev. Da Esc. De Enferm. Da U S P 2022, 56, e20210447. [Google Scholar] [CrossRef] [PubMed]
- Nelson, K.E.; Hanson, G.C.; Boyce, D.; Ley, C.D.; Swavely, D.; Reina, M.; Rushton, C.H. Organizational impact on healthcare workers’ moral injury during COVID-19: A mixed-methods analysis. J. Nurs. Admin. 2022, 52, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Chutiyami, M.C.; Allen, M.Y.; Salihu, D.; Bello, U.M.; Ndwiga, D.; Maharaj, R.; Naidoo, K.; Kolo, M.A.; Jacob, P.; Chhina, N.; et al. COVID-19 pandemic and overall mental health of healthcare professionals globally: A meta-review of systematic reviews. Front. Psychiat. 2022, 12, 804525. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Ruiz, E.; Campelo-Izquierdo, M.; Estany-Gestal, A.; Rodríguez-Calvo, M.S.; Rodríguez-Núñez, A. Impact of the Coronavirus disease 2019 pandemic on moral distress among nurses and physicians in Spanish ICUs. Crit. Care Med. 2021, 50, e487–e497. [Google Scholar] [CrossRef] [PubMed]
- Kok, N.; van Gurp, J.; Teerenstra, S.; van der Hoeven, H.; Fuchs, M.; Hoedemaekers, C.; Zegers, M. Coronavirus disease 2019 immediately increases burnout symptoms in ICU professionals: A longitudinal cohort study. Crit. Care Med. 2021, 49, 419–427. [Google Scholar] [CrossRef]
- Crilly, J.; Greenslade, J.H.; Johnston, A.; Carlström, E.; Thom, O.; Abraham, L.; Mills, D.; Wallis, M. Staff perceptions of the emergency department working environment: An international cross-sectional survey. Emerg. Med. Australas. EMA 2019, 31, 1082–1091. [Google Scholar] [CrossRef]
- Yarad, E.; Bates, S.; Butler, M.; Byrne, K.; Eastwood, G.; Grattan, S.; Miller, J.; Morrison, L.; Murray, L.; Palermo, A.; et al. Job satisfaction and symptoms of depression, anxiety, stress, and burnout: A survey of Australian and New Zealand intensive care research coordinators. Aust. Crit. Care 2022. [Google Scholar] [CrossRef]
- Spilg, E.G.; Rushton, C.H.; Phillips, J.L.; Kendzerska, T.; Saad, M.; Gifford, W.; Gautam, M.; Bhatla, R.; Edwards, J.D.; Quilty, L.; et al. The new frontline: Exploring the links between moral distress, moral resilience and mental health in healthcare workers during the COVID-19 pandemic. BMC Psychiat. 2022, 22, 19. [Google Scholar] [CrossRef]
- Fantus, S.; Cole, R.; Hawkins, L. The hierarchy is your constraint: A qualitative investigation of social workers’ moral distress across a U.S. health system. Soc. Work Health Care 2022, 61, 1–25. [Google Scholar] [CrossRef]
- Silverman, H.; Wilson, T.; Tisherman, S.; Kheirbek, R.; Mukherjee, T.; Tabatabai, A.; McQuillan, K.; Hausladen, R.; Davis-Gilbert, M.; Cho, E.; et al. Ethical decision-making climate, moral distress, and intention to leave among ICU professionals in a tertiary academic hospital center. BMC Med. Ethics 2022, 23, 45. [Google Scholar] [CrossRef]
- Faraco, M.M.; Gelbcke, F.L.; Brehmer, L.C.d.F.; Ramos, F.R.S.; Schneider, D.G.; Silveira, L.R. Moral distress and moral resilience of nurse managers. Nurs. Ethics 2022, 29, 1253–1265. [Google Scholar] [CrossRef] [PubMed]
- Beck, J.; Falco, C.N.; O’Hara, K.L.; Bassett, H.K.; Randall, C.L.; Cruz, S.; Hanson, J.L.; Dean, W.; Senturia, K. The norms and corporatization of medicine influence physician moral distress in the United States. Teach. Learn. Med. 2022. [Google Scholar] [CrossRef] [PubMed]
- Lamiani, G.; Biscardi, D.; Meyer, E.C.; Giannini, A.; Vegni, E. Moral distress trajectories of physicians 1 year after the COVID-19 outbreak: A grounded theory study. Int. J. Environ. Res. Public Health 2021, 18, 13367. [Google Scholar] [CrossRef] [PubMed]
- Ramos, F.R.S.; Brehmer, L.C.d.F.; Dalmolin, G.d.L.; Silveira, L.R.; Schneider, D.G.; Vargas, M.A.d.O. Association between moral distress and supporting elements of moral deliberation in nurses. Rev. Lat. Am. Enferm. 2020, 28, e3332. [Google Scholar] [CrossRef] [PubMed]
- Kleinknecht-Dolf, M.; Spichiger, E.; Müller, M.; Bartholomeyczik, S.; Spirig, R. Advancement of the German version of the moral distress scale for acute care nurses-A mixed methods study. Nurs. Open 2017, 4, 251–266. [Google Scholar] [CrossRef] [PubMed]
- Hamric, A.; Blackhall, L. Nurse-physician perspectives on the care of dying patients in intensive care units: Collaboration, moral distress, and ethical climate. Crit. Care Med. 2007, 35, 422–429. [Google Scholar] [CrossRef]
- Büssing, A.; Scheer, K.; Tewes, M.; Niesert, W.; Büntzel, J.; Rentschler, J. Erfassung existenzieller und spiritueller Bedürfnisse in der palliativen Betreuung—Erste Erkenntnisse zur Implementierung des Spiritual Needs Screeners. Spirit. Care 2022, 11, 278–281. [Google Scholar] [CrossRef]
- Büssing, A.; Balzat, H.J.; Heusser, P. Spiritual needs of patients with chronic pain diseases and cancer—Validation of the spiritual needs questionnaire. Eur. J. Med. Res. 2010, 15, 266. [Google Scholar] [CrossRef]
- Büssing, A.; Matthiessen, P.F.; Ostermann, T. Engagement of patients in religious and spiritual practices: Confirmatory results with the SpREUK-P 1.1 questionnaire as a tool of quality of life research. Health Qual. Life Outcomes 2005, 3, 53. [Google Scholar] [CrossRef]
- Mills, M.; Cortezzo, D.E. Moral distress in the neonatal intensive care unit: What is it, why it happens, and how we can address it. Front. Pediat. 2020, 8, 581. [Google Scholar] [CrossRef]
- Bayanzay, K.; Amoozgar, B.; Kaushal, V.; Holman, A.; Som, V.; Sen, S. Impact of profession and wards on moral distress in a community hospital. Nurs. Ethics 2022, 29, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Thomas, T.A.; Davis, D.; Kumar, S.; Thammasitboon, S.; Rushton, C.H. COVID-19 and moral distress: A pediatric critical care survey. Am. J. Crit. Care 2021, 30, e80–e98. [Google Scholar] [CrossRef] [PubMed]
- Schneider, J.N.; Hiebel, N.; Kriegsmann-Rabe, M.; Schmuck, J.; Erim, Y.; Morawa, E.; Jerg-Bretzke, L.; Beschoner, P.; Albus, C.; Hannemann, J.; et al. Moral distress in hospitals during the first wave of the COVID-19 pandemic: A web-based survey among 3293 healthcare workers within the German Network University Medicine. Front. Psychol. 2021, 12, 775204. [Google Scholar] [CrossRef]
- Rodríguez-Ruiz, E.; Campelo-Izquierdo, M.; Estany-Gestal, A.; Hortas, A.B.; Rodríguez-Calvo, M.S.; Rodríguez-Núñez, A. Validation and psychometric properties of the Spanish version of the Measure of Moral Distress for Health Care Professionals (MMD-HP-SPA). Med. Intensiv. 2021, 46, 169–170. [Google Scholar] [CrossRef] [PubMed]
- Rodríguez-Ruiz, E.; Campelo-Izquierdo, M.; Veiras, P.B.; Rodríguez, M.M.; Estany-Gestal, A.; Hortas, A.B.; Rodríguez-Calvo, M.S.; Rodríguez-Núñez, A. Moral distress among healthcare professionals working in intensive care units in Spain. Med. Intensiv. 2022, 7, 383–391. [Google Scholar] [CrossRef]
- Prokopová, T.; Hudec, J.; Vrbica, K.; Stašek, J.; Pokorná, A.; Štourač, P.; Rusinová, K.; Kerpnerová, P.; Štěpánová, R.; Svobodník, A. Palliative care practice and moral distress during COVID-19 pandemic (PEOpLE-C19 study): A national, cross-sectional study in the Czech Republic. BMC Crit. Care 2022. under review. [Google Scholar] [CrossRef] [PubMed]
- Donkers, M.A.; Gilissen, V.J.H.S.; Candel, M.J.J.M.; van Dijk, N.M.; Kling, H.; Heijnen-Panis, R.; Pragt, E.; van der Horst, I.; Pronk, S.A.; van Mook, W.N.K.A. Moral distress and ethical climate in intensive care medicine during COVID-19: A nationwide study. BMC Med. Ethics 2021, 22, 73. [Google Scholar] [CrossRef]
- Fumis, R.R.L.; Junqueira Amarante, G.A.; de Fátima Nascimento, A.; Vieira Junior, J.M. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann. Intensive Care 2017, 7, 1–8. [Google Scholar] [CrossRef]
- Voultsos, P. Nurses’ emotional reactions and compassion fatigue: A systematic review. Aristotle Biomed. J. 2021, 3, 2653–9748. [Google Scholar]
- Dalton, A. Mitigating burnout and enhancing wellness in anesthesiologists: Individual interventions, wellness programs, and peer support. Int. Anesthesiol. Clin. 2021, 59, 73–80. [Google Scholar] [CrossRef]
- Kühlmeyer, K.; Kuhn, E.; Knochel, K.; Hildesheim, H.; Witt, V.D.; Friedrich, O.; Rogge, A. Moral distress in medical students and young professionals: Research desiderata in the context of the COVID-19 pandemic. Bundesgesundheitsblatt Gesundh. Gesundh. 2020, 63, 1483–1490. [Google Scholar] [CrossRef] [PubMed]
- Epstein, E.G.; Hamric, A.B. Moral distress, moral residue, and the crescendo effect. J. Clin. Ethics 2009, 20, 330. [Google Scholar] [CrossRef] [PubMed]
- Alazmani-Noodeh, F.; Abdi, K.; Ranjbar, H. The moderating effect of spiritual beliefs on job dissatisfaction related to the futile care. BMC Nurs. 2021, 20, 64. [Google Scholar] [CrossRef] [PubMed]
- Callis, A.; Cacciata, M.; Wickman, M.; Choi, J. An effective in-hospital chaplaincy-led care program for nurses: Tea for the soul a qualitative investigation. J. Health Care Chaplain. 2021, 28, 526–539. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.; Batcheller, J. Managing moral distress in the workplace: Creating a resiliency bundle. Nurse Lead. 2020, 18, 604–608. [Google Scholar] [CrossRef]
- LoGiudice, J.A.; Bartos, S. Experiences of nurses during the COVID-19 pandemic: A mixed-methods study. AACN Adv. Crit. Care 2021, 32, 14–26. [Google Scholar] [CrossRef]
- Sala Defilippis, T.M.L.; Curtis, K.; Gallagher, A. Moral resilience through harmonised connectedness in intensive care nursing: A grounded theory study. Intensive Crit. Care Nurs. 2020, 57, 102785. [Google Scholar] [CrossRef]
- Silverman, H.J.; Kheirbek, R.E.; Moscou-Jackson, G.; Day, J. Moral distress in nurses caring for patients with Covid-19. Nurs. Ethics 2021, 28, 1137–1164. [Google Scholar] [CrossRef]
- Smiechowski, J.; Stelfox, H.; Sinclair, S.; Sinuff, T.; Grindrod-Millar, K.; Roze des Ordons, A. Vicarious spiritual distress in intensive care unit healthcare providers: A qualitative study. Intensive Crit. Care Nurs. 2020, 63, 102982. [Google Scholar] [CrossRef]
- Wu, A.W.; Connors, C.A.; Norvell, M. Adapting RISE: Meeting the needs of healthcare workers during the COVID-19 pandemic. Int. Rev. Psychiat. 2022, 33, 711–717. [Google Scholar] [CrossRef]
- Smith-MacDonald, L.; Lusk, J.; Lee-Baggley, D.; Bright, K.; Laidlaw, A.; Voth, M.; Spencer, S.; Cruikshank, E.; Pike, A.; Jones, C.; et al. Companions in the abyss: A feasibility and acceptability study of an online therapy group for healthcare providers working during the COVID-19 pandemic. Front. Psychiat. 2022, 2500, 12. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Zaben, F.A.; Koenig, H.G.; Ding, Y. Spirituality, moral injury and mental health among Chinese health professionals. BJPsych Open 2021, 7, e135, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Alhassan, R.K.; Nutor, J.J.; Abuosi, A.A.; Afaya, A.; Mohammed, S.S.; Dalaba, M.A.; Immurana, M.; Manyeh, A.K.; Klu, D.; Aberese-Ako, M.; et al. Urban health nexus with coronavirus disease 2019 (COVID-19) preparedness and response in Africa: Rapid scoping review of the early evidence. SAGE Open Med. 2021, 9, 2050312121994360. [Google Scholar] [CrossRef] [PubMed]
- Lentz, L.M.; Smith-MacDonald, L.; Malloy, D.; Carleton, R.N.; Brémault-Phillips, S. Compromised conscience: A scoping review of moral injury among firefighters, paramedics, and police officers. Front. Psychol. 2021, 12, 639781. [Google Scholar] [CrossRef] [PubMed]
- Borges, L.M.; Holliday, R.; Barnes, S.M.; Bahraini, N.H.; Kinney, A.; Forster, J.E.; Brenner, L.A. A longitudinal analysis of the role of potentially morally injurious events on COVID-19-related psychosocial functioning among healthcare providers. PLoS ONE 2021, 16, e0260033. [Google Scholar] [CrossRef]
- Borges, L.M.; Barnes, S.M.; Farnsworth, J.K.; Evans, W.R.; Moon, Z.; Drescher, K.D.; Walser, R.D. Cultivating psychological flexibility to address religious and spiritual suffering in moral injury. J. Health Care Chaplain. 2022, 28 (Suppl. S1), S32–S41. [Google Scholar] [CrossRef]
- Schlak, A.E.; Rosa, W.E.; Rushton, C.H.; Poghosyan, L.; Root, M.C.; McHugh, M.D. An expanded institutional- and national-level blueprint to address nurse burnout and moral suffering amid the evolving pandemic. Nurs. Manag. 2022, 53, 16–27. [Google Scholar] [CrossRef]
- Smigelsky, M.A.; Trimm, V.; Meador, K.G.; Jackson, G.L.; Wortmann, J.H.; Nieuwsma, J.A. Core components of moral injury groups co-facilitated by mental health providers and chaplains. Spiritual. Clin. Pract. 2022, 9, 159–174. [Google Scholar] [CrossRef]
- Wocial, L.D. Resilience as an incomplete strategy for coping with moral distress in critical care Nurses. Crit. Care Nurse 2020, 40, 62–66. [Google Scholar] [CrossRef]
- Zhang, Y.; Wu, X.; Wan, X.; Hayter, M.; Wu, J.; Li, S.; Hu, Y.; Yuan, Y.; Liu, Y.; Cao, C.; et al. Relationship between burnout and intention to leave amongst clinical nurses: The role of spiritual climate. J. Nurs. Manage. 2019, 27, 1285–1293. [Google Scholar] [CrossRef]
- Moll, T. Exploring aspects of New Work: Spirituality at Work in agile organizations. Spirit. Care 2022, 11, 203–211. [Google Scholar] [CrossRef]
| MW ± SD [0–4] | Perception of Burden (%) | |||||
|---|---|---|---|---|---|---|
| None | Little | Moderate | Large | Very Large | ||
| I worked in a nursing team with shift staffing that I considered insufficient (item b9). | 2.86 ± 1.14 | 4.4 | 11.3 | 12.5 | 37.5 | 34.4 |
| I have worked with people from my own or another professional group who I found to be insufficiently competent so the quality of care suffered or patient safety was endangered (item b6). | 2.45 ± 1.14 | 4.9 | 16.7 | 27.8 | 29.6 | 21.0 |
| I have not been able to provide care that is consistent with my professional ethics due to operational or financial pressures (item b1). | 2.38 ± 1.14 | 5.6 | 19.1 | 23.5 | 35.2 | 16.7 |
| I observed that the quality of care and treatment suffered due to a lack of continuity in the treatment team (item b8). | 2.37 ± 0.96 | 3.1 | 13.0 | 39.8 | 32.2 | 11.8 |
| I have not been able to avoid or alleviate a patient’s suffering due to inadequate prescriptions (item b11). | 2.25 ± 1.33 | 11.6 | 20.0 | 24.5 | 20.0 | 23.9 |
| MW ± SD [0–4] | Perception of Burden (%) | |||||
|---|---|---|---|---|---|---|
| None | Little | Moderate | Large | Very Large | ||
| I worked in a nursing team with shift staffing that I considered insufficient (item b9). | 2.24 ± 1.18 | 7.1 | 22.5 | 25.3 | 29.1 | 15.8 |
| I observed that the quality of care and treatment suffered due to a lack of continuity in the treatment team (item b8). | 2.07 ± 1.05 | 5.8 | 25.3 | 34.7 | 24.7 | 9.5 |
| I have worked with people from my own or another professional group who I found to be insufficiently competent so the quality of care suffered or patient safety was endangered (item b6). | 2.05 ± 1.05 | 6.9 | 25.4 | 31.7 | 27.5 | 8.5 |
| I have not been able to provide care that is consistent with my professional ethics due to operational or financial pressures (item b1). | 1.76 ± 1.25 | 17.9 | 27.4 | 26.8 | 16.8 | 11.1 |
| I have not been able to provide care that is consistent with my professional ethics due to non-partnership collaboration (item b10). | 1.70 ± 1.21 | 18.0 | 30.3 | 24.2 | 19.1 | 8.4 |
| MDI Frequency | MDI Frequency: External Causes | MDI Frequency: Looking Away/Resignation | MDI Frequency: Inappropriate Acting | MDI Burden | MDI Burden: External Causes | MDI Burden: Looking Away | |
|---|---|---|---|---|---|---|---|
| MDI Frequency | 1.000 | ||||||
| MDI Frequency: External causes | 0.932 ** | 1.000 | |||||
| MDI Frequency: Looking away/resignation | 0.693 ** | 0.517 ** | 1.000 | ||||
| MDI Frequency: Inappropriate acting | 0.656 ** | 0.457 ** | 0.377 ** | 1.000 | |||
| MDI Burden | 0.761 ** | 0.670 ** | 0.749 ** | 0.474 ** | 1.000 | ||
| MDI Burden: External causes | 0.765 ** | 0.701 ** | 0.629 ** | 0.508 ** | 0.967 ** | 1.000 | |
| MDI Burden: Looking away | 0.545 ** | 0.406 ** | 0.762 ** | 0.247 ** | 0.668 ** | 0.499 ** | 1.000 |
| Age (years) | −0.167 ** | −0.126 | −0.205 ** | −0.097 | −0.204 ** | −0.187 ** | −0.180 ** |
| Employment (years) | −0.096 | −0.062 | −0.157 ** | −0.042 | −0.108 | −0.080 | −0.157 ** |
| Experience in emergency/intensive care medicine | −0.081 | −0.038 | −0.207 ** | −0.003 | −0.161 ** | −0.120 | −0.194 ** |
| Working hours per week | −0.156 ** | −0.126 | −0.164 ** | −0.104 | −0.183 ** | −0.196 ** | −0.109 |
| Professional satisfaction | −0.335 ** | −0.328 ** | −0.226 ** | −0.224 ** | −0.285 ** | −0.308 ** | −0.157 ** |
| Perception of burden/stress | 0.264 ** | 0.250 ** | 0.182 ** | 0.199 ** | 0.252 ** | 0.271 ** | 0.110 |
| Emotional exhaustion | 0.315 ** | 0.274 ** | 0.264 ** | 0.255** | 0.342 ** | 0.359 ** | 0.161 ** |
| SpREUK: Search | 0.012 | −0.019 | 0.105 | −0.030 | 0.075 | 0.043 | 0.142 ** |
| SpREUK: Trust | −0.140 ** | −0.153 ** | −0.028 | −0.110 | −0.053 | −0.082 | 0.042 |
| SpREUK: Reflection | 0.061 | 0.040 | 0.095 | 0.053 | 0.118 | 0.092 | 0.115 |
| Self-perception of being a believer | −0.135 ** | −0.137 ** | −0.039 | −0.130 | −0.062 | −0.083 | 0.015 |
| Frequency of prayer/meditation | −0.037 | −0.045 | 0.022 | −0.026 | 0.004 | −0.018 | 0.043 |
|
Dependent Variable: MDI Frequency Model 5: * F = 17.9. p < 0.001; R2 = 0.22 | Unstandardized Regression Coefficient B | Standard Error | Standardized Beta | T | p |
|---|---|---|---|---|---|
| (constant) | 19.997 | 2.694 | 7.424 | <0.0001 | |
| Job satisfaction | −1.456 | 0.502 | −0.167 | −2.898 | 0.004 |
| Emotional Exhaustion | 0.076 | 0.018 | 0.239 | 4.225 | <0.0001 |
| Profession: Nurses | 2.434 | 0.809 | 0.155 | 3.007 | 0.003 |
| Believer | −1.014 | 0.370 | −0.137 | −2.737 | 0.007 |
| Level of care of the hospital | −1.145 | 0.451 | −0.127 | −2.536 | 0.012 |
|
Dependent variable: MDI Burden Model 3: ** F = 19.8. p < 0.001; R2 = 0.20 | Unstandardized Regression Coefficient B | Standard error | Standardized Beta | T | p |
| (constant) | 13.498 | 2.758 | 4.895 | <0.0001 | |
| Emotional Exhaustion | 0.115 | 0.019 | 0.303 | 5.943 | <0.0001 |
| Profession: Nurses | 3.718 | 0.995 | 0.200 | 3.737 | <0.0001 |
| Experience in emergency/intensive care medicine | −0.630 | 0.296 | −0.109 | −2.129 | 0.034 |
| Female gender | −2.022 | 1.012 | −0.108 | −1.998 | 0.047 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hinzmann, D.; Schütte-Nütgen, K.; Büssing, A.; Boenisch, O.; Busch, H.-J.; Dodt, C.; Friederich, P.; Kochanek, M.; Michels, G.; Frick, E. Critical Care Providers’ Moral Distress: Frequency, Burden, and Potential Resources. Int. J. Environ. Res. Public Health 2023, 20, 333. https://doi.org/10.3390/ijerph20010333
Hinzmann D, Schütte-Nütgen K, Büssing A, Boenisch O, Busch H-J, Dodt C, Friederich P, Kochanek M, Michels G, Frick E. Critical Care Providers’ Moral Distress: Frequency, Burden, and Potential Resources. International Journal of Environmental Research and Public Health. 2023; 20(1):333. https://doi.org/10.3390/ijerph20010333
Chicago/Turabian StyleHinzmann, Dominik, Katharina Schütte-Nütgen, Arndt Büssing, Olaf Boenisch, Hans-Jörg Busch, Christoph Dodt, Patrick Friederich, Matthias Kochanek, Guido Michels, and Eckhard Frick. 2023. "Critical Care Providers’ Moral Distress: Frequency, Burden, and Potential Resources" International Journal of Environmental Research and Public Health 20, no. 1: 333. https://doi.org/10.3390/ijerph20010333
APA StyleHinzmann, D., Schütte-Nütgen, K., Büssing, A., Boenisch, O., Busch, H.-J., Dodt, C., Friederich, P., Kochanek, M., Michels, G., & Frick, E. (2023). Critical Care Providers’ Moral Distress: Frequency, Burden, and Potential Resources. International Journal of Environmental Research and Public Health, 20(1), 333. https://doi.org/10.3390/ijerph20010333










