Could the Improvement of Supraspinatus Muscle Activity Speed up Shoulder Pain Rehabilitation Outcomes in Wheelchair Basketball Players?
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedures
- -
- WUSPI (Wheelchair User’s Shoulder Pain Index): It is a scale which measures shoulder pain associated with the functional activities of wheelchair users. This 15-item index investigates shoulder pain during transfers, self-care, wheelchair mobility, and general activities. The score can range from 0 to 150 [13].
- -
- Supraspinatus muscle activity of both shoulders measured as root mean square (RMS): This evaluation was made using the mDurance sEMG and was expressed in microvolts; after performing a skin disinfection with isopropyl alcohol and placing the patient in a shoulder resting position, two pre-gelled electrodes were applied on two points of the supraspinatus muscle belly and one third on the acromion, for both sides, according to the pre-set device instructions.
- -
- Range of motion (ROM) in abduction and external rotation: It is the evaluation measured in degrees (°) of the shoulder range of movement in the direction most influenced by the activity of the supraspinatus muscle. This evaluation was made using the inertial sensors included in the mDurance device.
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cavalcante, R.N.; Santos, A.C.S.; Rodrigues, R.A.S.; Napoleão, A.C.B.; Balogun, S.O.; de Andrade, B.R.M.; Fett, C.A.; Zavala, A.A.Z.; Arunachalam, K.; de Oliveira, R.G. Wheelchair basketball improves the treatment of urinary tract infection in people with motor disabilities: A clinical trial. Rev. Assoc. Med. Bras. 2022, 68, 559–567. [Google Scholar] [CrossRef]
- Sá, K.; e Silva, A.C.; Gorla, J.; Silva, A.; e Silva, M.M. Injuries in Wheelchair Basketball Players: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5869. [Google Scholar] [CrossRef]
- Tsunoda, K.; Mutsuzaki, H.; Kanae, K.; Tachibana, K.; Shimizu, Y.; Wadano, Y. Associations between wheelchair user’s shoulder pain index and tendinitis in the long head of the biceps tendon among female wheelchair basketball players from the Japanese national team. Asia-Pac. J. Sports Med. Arthrosc. Rehabil. Technol. 2021, 24, 29–34. [Google Scholar] [CrossRef]
- Heyward, O.W.; Vegter, R.J.K.; De Groot, S.; Van Der Woude, L.H.V. Shoulder complaints in wheelchair athletes: A systematic review. PLoS ONE 2017, 12, e0188410. [Google Scholar] [CrossRef] [PubMed]
- Karasuyama, M.; Oike, T.; Okamatsu, S.; Kawakami, J. Shoulder pain in wheelchair basketball athletes: A scoping review. J. Spinal Cord Med. 2022, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Hoo, J.A.S.; Kim, H.; Fram, J.; Lin, Y.; Page, C.; Easthausen, I.; Jayabalan, P. Shoulder pain and ultrasound findings: A comparison study of wheelchair athletes, nonathletic wheelchair users, and nonwheelchair users. PM&R 2021, 14, 551–560. [Google Scholar] [CrossRef]
- Tsunoda, K.; Mutsuzaki, H.; Hotta, K.; Tachibana, K.; Shimizu, Y.; Fukaya, T.; Ikeda, E.; Wadano, Y. Correlates of shoulder pain in wheelchair basketball players from the Japanese national team: A cross-sectional study. J. Back Musculoskelet. Rehabil. 2016, 29, 795–800. [Google Scholar] [CrossRef] [PubMed]
- Aytar, A.; Zeybek, A.; Pekyavas, N.O.; Tigli, A.A.; Ergun, N. Scapular resting position, shoulder pain and function in disabled athletes. Prosthet. Orthot. Int. 2015, 39, 390–396. [Google Scholar] [CrossRef]
- Dutton, R.A. Medical and Musculoskeletal Concerns for the Wheelchair Athlete: A Review of Preventative Strategies. Curr. Sports Med. Rep. 2019, 18, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Neblett, R.; Mayer, T.G.; Gatchel, R.J. Theory and rationale for surface EMG-assisted stretching as an adjunct to chronic musculoskeletal pain rehabilitation. Appl. Psychophysiol. Biofeedback 2003, 28, 139–146. [Google Scholar] [CrossRef] [PubMed]
- Calabrò, R.S.; Filoni, S.; Billeri, L.; Balletta, T.; Cannavò, A.; Militi, A.; Milardi, D.; Pignolo, L.; Naro, A. Robotic Rehabilitation in Spinal Cord Injury: A Pilot Study on End-Effectors and Neurophysiological Outcomes. Ann. Biomed. Eng. 2021, 49, 732–745. [Google Scholar] [CrossRef] [PubMed]
- Van Straaten, M.G.; Cloud-Biebl, B.; Morrow, M.M.; Ludewig, P.; Zhao, K.D. Effectiveness of Home Exercise on Pain, Function, and Strength of Manual Wheelchair Users with Spinal Cord Injury: A High-Dose Shoulder Program with Telerehabilitation. Arch. Phys. Med. Rehabil. 2014, 95, 1810–1817.e2. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.A.; Roach, K.E.; Applegate, E.B.; Amar, T.; Benbow, C.S.; Genecco, T.D.; Gualano, J. Development of the Wheelchair User’s Shoulder Pain Index (WUSPI). Spinal Cord 1995, 33, 290–293. [Google Scholar] [CrossRef] [PubMed]
- Molina-Molina, A.; Ruiz-Malagón, E.J.; Carrillo-Pérez, F.; Roche-Seruendo, L.E.; Damas, M.; Banos, O.; García-Pinillos, F. Validation of mDurance, A Wearable Surface Electromyography System for Muscle Activity Assessment. Front. Physiol. 2020, 11, 606287. [Google Scholar] [CrossRef]
- Farì, G.; Lunetti, P.; Pignatelli, G.; Raele, M.V.; Cera, A.; Mintrone, G.; Ranieri, M.; Megna, M.; Capobianco, L. The Effect of Physical Exercise on Cognitive Impairment in Neurodegenerative Disease: From Pathophysiology to Clinical and Rehabilitative Aspects. Int. J. Mol. Sci. 2021, 22, 11632. [Google Scholar] [CrossRef]
- Vanderstraeten, G.G.; Oomen, A.G. Sports for disabled people: A general outlook. Int. J. Rehabil. Res. 2010, 33, 283–284. [Google Scholar] [CrossRef] [PubMed]
- Farì, G.; Fischetti, F.; Zonno, A.; Marra, F.; Maglie, A.; Bianchi, F.; Messina, G.; Ranieri, M.; Megna, M. Musculoskeletal Pain in Gymnasts: A Retrospective Analysis on a Cohort of Professional Athletes. Int. J. Environ. Res. Public Health 2021, 18, 5460. [Google Scholar] [CrossRef]
- Notarnicola, A.; Farì, G.; Maccagnano, G.; Riondino, A.; Covelli, I.; Bianchi, F.P.; Tafuri, S.; Piazzolla, A.; Moretti, B. Teenagers’ perceptions of their scoliotic curves. an observational study of comparison between sports people and non- sports people. Muscles Ligaments Tendons J. 2019, 9, 225–235. [Google Scholar] [CrossRef]
- Farì, G.; Notarnicola, A.; DI Paolo, S.; Covelli, I.; Moretti, B. Epidemiology of injuries in water board sports: Trauma versus overuse injury. J. Sports Med. Phys. Fit. 2021, 61, 707–711. [Google Scholar] [CrossRef]
- Farì, G.; Santagati, D.; Macchiarola, D.; Ricci, V.; Di Paolo, S.; Caforio, L.; Invernizzi, M.; Notarnicola, A.; Megna, M.; Ranieri, M. Musculoskeletal pain related to surfing practice: Which role for sports rehabilitation strategies? A cross-sectional study. J. Back Musculoskelet. Rehabil. 2022, 35, 911–917. [Google Scholar] [CrossRef]
- De Sire, A.; Demeco, A.; Marotta, N.; Spanò, R.; Curci, C.; Farì, G.; Fortunato, F.; Iona, T.; Lippi, L.; Paolucci, T.; et al. Neuromuscular impairment of knee stabilizer muscles in a COVID-19 cluster of female volleyball players: Which role for rehabilitation in the post-COVID-19 return-to-play? Appl. Sci. 2022, 12, 557. [Google Scholar] [CrossRef]
- Fagher, K.; Lexell, J. Sports-related injuries in athletes with disabilities. Scand. J. Med. Sci. Sports 2014, 24, e320–e331. [Google Scholar] [CrossRef] [PubMed]
- Curtis, K.A.; Black, K. Shoulder Pain in Female Wheelchair Basketball Players. J. Orthop. Sports Phys. Ther. 1999, 29, 225–231. [Google Scholar] [CrossRef] [PubMed]
- Mason, B.; Warner, M.; Briley, S.; Goosey-Tolfrey, V.; Vegter, R. Managing shoulder pain in manual wheelchair users: A scoping review of conservative treatment interventions. Clin. Rehabil. 2020, 34, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Cratsenberg, K.A.; Deitrick, C.E.; Harrington, T.K.; Kopecky, N.R.; Matthews, B.D.; Ott, L.M.; Coeytaux, R.R. Effectiveness of Exercise Programs for Management of Shoulder Pain in Manual Wheelchair Users with Spinal Cord Injury. J. Neurol. Phys. Ther. 2015, 39, 197–203. [Google Scholar] [CrossRef] [PubMed]
- Middaugh, S.; Thomas, K.J.; Smith, A.R.; McFall, T.L.; Klingmueller, J. EMG Biofeedback and Exercise for Treatment of Cervical and Shoulder Pain in Individuals with a Spinal Cord Injury: A Pilot Study. Top. Spinal Cord Inj. Rehabil. 2013, 19, 311–323. [Google Scholar] [CrossRef] [PubMed]
- Boone, B.D.C.; Azen, S.P.; Lin, B.C.-M.; Spence, B.C.; Baron, B.C.; Lee, B.L. Reliability of Goniometric Measurements. Phys. Ther. 1978, 58, 1355–1360. [Google Scholar] [CrossRef]
- Ortega-Santiago, R.; González-Aguado, Á.J.; Fernández-De-Las-Peñas, C.; Cleland, J.A.; De-La-Llave-Rincón, A.I.; Kobylarz, M.D.; Plaza-Manzano, G. Pressure pain hypersensitivity and referred pain from muscle trigger points in elite male wheelchair basketball players. Braz. J. Phys. Ther. 2019, 24, 333–341. [Google Scholar] [CrossRef]
- Wilroy, J.; Hibberd, E. Evaluation of a Shoulder Injury Prevention Program in Wheelchair Basketball. J. Sport Rehabil. 2018, 27, 554–559. [Google Scholar] [CrossRef]
- Dominguez-Romero, J.G.; Jiménez-Rejano, J.J.; Ridao-Fernández, C.; Chamorro-Moriana, G. Exercise-Based Muscle Development Programmes and Their Effectiveness in the Functional Recovery of Rotator Cuff Tendinopathy: A Systematic Review. Diagnostics 2021, 11, 529. [Google Scholar] [CrossRef]
- Cotter, E.J.; Hannon, C.P.; Christian, D.; Frank, R.M.; Bach, B.R., Jr. Comprehensive Examination of the Athlete’s Shoulder. Sports Health A Multidiscip. Approach 2018, 10, 366–375. [Google Scholar] [CrossRef] [PubMed]
- Turgut, E.; Pedersen, Ø.; Duzgun, I.; Baltaci, G. Three-dimensional scapular kinematics during open and closed kinetic chain movements in asymptomatic and symptomatic subjects. J. Biomech. 2016, 49, 2770–2777. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Maccagnano, G.; Maresca, L.; Oliva, M.C.; Fari, G.; Papagni, G.; Pignatelli, G.; Covelli, I.; Gioia, G.; Bianchi, F.P.; et al. Is extracorporeal shockwave therapy effective even in the treatment of partial rotator cuff tear? J. Biol. Regul. Homeost. Agents 2020, 34, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Zaluski, A.J.; Campbell, J.; Hlasny, M.; Nedjelski, M.; Thompson, T.; Vanneste, A.; Kim, S.Y. Activation of neuromuscular sub-regions of supraspinatus and infraspinatus during common rehabilitative exercises. J. Electromyogr. Kinesiol. 2021, 61, 102604. [Google Scholar] [CrossRef] [PubMed]
- Escamilla, R.F.; Yamashiro, K.; Paulos, L.; Andrews, J.R. Shoulder Muscle Activity and Function in Common Shoulder Rehabilitation Exercises. Sports Med. 2009, 39, 663–685. [Google Scholar] [CrossRef] [PubMed]
- Reinold, M.M.; Macrina, L.C.; Wilk, K.E.; Fleisig, G.S.; Dun, S.; Barrentine, S.W.; Ellerbusch, M.T.; Andrews, J.R. Electromyographic analysis of the supraspinatus and deltoid muscles during 3 common rehabilitation exercises. J. Athl. Train. 2007, 42, 464–469. [Google Scholar] [PubMed]
- Picha, K.J.; Jochimsen, K.N.; Heebner, N.R.; Abt, J.P.; Usher, E.; Capilouto, G.; Uhl, T.L. Measurements of self-efficacy in musculoskeletal rehabilitation: A systematic review. Musculoskelet. Care 2018, 16, 471–488. [Google Scholar] [CrossRef]
- Farì, G.; Santagati, D.; Pignatelli, G.; Scacco, V.; Renna, D.; Cascarano, G.; Vendola, F.; Bianchi, F.P.; Fiore, P.; Ranieri, M.; et al. Collagen Peptides, in Association with Vitamin C, Sodium Hyaluronate, Manganese and Copper, as Part of the Rehabilitation Project in the Treatment of Chronic Low Back Pain. Endocr. Metab. Immune Disord. Drug Targets 2022, 22, 108–115. [Google Scholar] [CrossRef]
- Werin, M.; Maenhout, A.; Smet, S.; Van Holder, L.; Cools, A. Muscle recruitment during plyometric exercises in overhead athletes with and without shoulder pain. Phys. Ther. Sport 2020, 43, 19–26. [Google Scholar] [CrossRef]
- Escamilla, R.F.; Fleisig, G.S.; Groeschner, D.; Akizuki, K. Biomechanical Comparisons Among Fastball, Slider, Curveball, and Changeup Pitch Types and Between Balls and Strikes in Professional Baseball Pitchers. Am. J. Sports Med. 2017, 45, 3358–3367. [Google Scholar] [CrossRef]
- Tamburella, F.; Moreno, J.C.; Valenzuela, D.S.H.; Pisotta, I.; Iosa, M.; Cincotti, F.; Mattia, D.; Pons, J.L.; Molinari, M. Influences of the biofeedback content on robotic post-stroke gait rehabilitation: Electromyographic vs joint torque biofeedback. J. Neuroeng. Rehabil. 2019, 16, 95. [Google Scholar] [CrossRef] [PubMed]
- Notarnicola, A.; Covelli, I.; Maccagnano, G.; Marvulli, R.; Mastromauro, L.; Ianieri, G.; Boodhoo, S.; Turitto, A.; Petruzzella, L.; Farì, G.; et al. Extracorporeal shockwave therapy on muscle tissue: The effects on healthy athletes. J. Biol. Regul. Homeost. Agents 2018, 32, 185–193. [Google Scholar] [PubMed]
| Variable | Exercise Group (n = 16) | Exercise Plus sEMG Biofeedback Group (n = 17) | Total (n = 33) | p-Value |
|---|---|---|---|---|
| Age; mean ± SD (range) | 38.7 ± 8.7 (23–55) | 37.2 ± 10.0 (24–57) | 37.9 ± 9.3 (23–57) | 0.648 |
| BMI; mean ± SD (range) | 23.7 ± 3.2 (18.8–31.1) | 24.4 ± 4.9 (17.0–35.9) | 24.0 ± 4.1 (17.0–35.9) | 0.623 |
| Right dominant limb; n (%) | 13 (81.3) | 12 (70.6) | 25 (75.8) | 0.475 |
| Shoulder pain on the right side; n (%) | 14 (87.5) | 13 (76.5) | 27 (81.8) | 0.412 |
| Outcome | Group | T0 | T1 | T2 | Comparison Between Groups | Comparison Between Times | Interaction Between Time and Group |
|---|---|---|---|---|---|---|---|
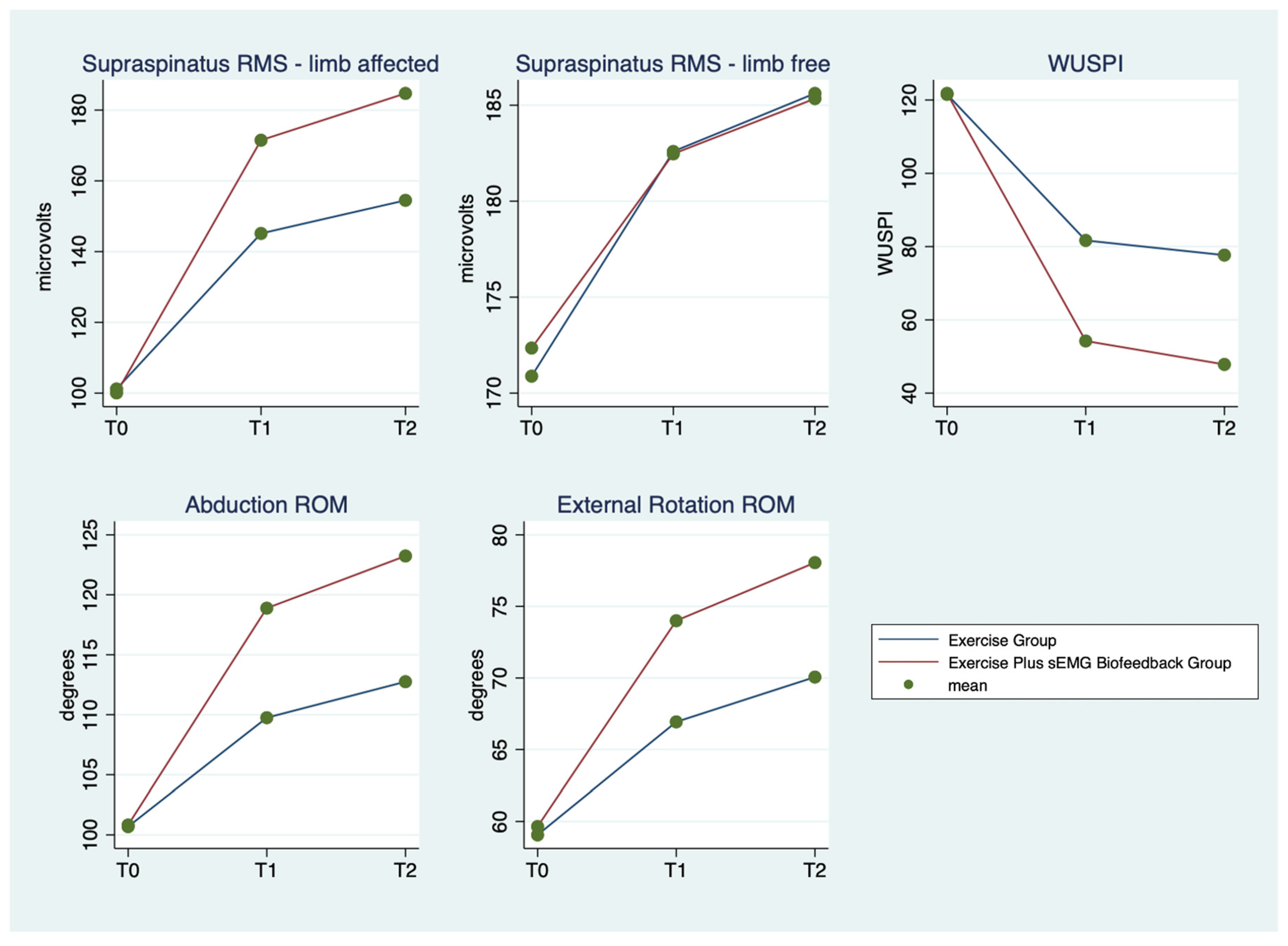
| Supraspinatus RMS (microvolts)—limb affected by SP | Exercise Group | 101.2 ± 11.9 (81.6–118.9) | 145.1 ± 12.9 (123.7–170.0) | 154.5 ± 11.8 (132.1–179.3) | <0.0001 | <0.0001 | <0.0001 |
| Exercise Plus sEMG Biofeedback Group | 100.1 ± 13.1 (78.1–119.1) | 171.5 ± 5.1 (160.2–178.9) | 184.7 ± 6.7 (170.3–195.7) | ||||
| Total | 100.6 ± 12.3 (78.1–119.1) | 158.7 ± 16.4 (123.7–178.9) | 170.1 ± 18.0 (132.1–195.7) | ||||
| Supraspinatus RMS (microvolts)—limb free from SP | Exercise Group | 170.9 ± 4.8 (160.3–180.5) | 182.6 ± 8.7 (167.9–201.7) | 185.6 ± 11.8 (132.1–179.3) | 0.844 | <0.0001 | 0.686 |
| Exercise Plus sEMG Biofeedback Group | 172.3 ± 6.0 (158.5–180.0) | 182.5 ± 5.2 (172.9–189.1) | 185.3 ± 3.8 (178.2–191.0) | ||||
| Total | 171.6 ± 5.4 (158.5–180.5) | 182.5 ± 7.0 (167.9–201.7) | 185.5 ± 6.1 (174.6–200.9) | ||||
| WUSPI | Exercise Group | 121.6 ± 9.6 (107–137) | 81.7 ± 6.3 (71–92) | 77.7 ± 6.6 (66–89) | <0.0001 | <0.0001 | <0.0001 |
| Exercise Plus sEMG Biofeedback Group | 121.8 ± 8.9 (106–135) | 54.2 ± 8.5 (41–70) | 47.8 ± 8.7 (36–67) | ||||
| Total | 121.7 ± 9.1 (106–137) | 67.5 ± 15.8 (41–92) | 62.3 ± 17.0 (36–89) | ||||
| Abduction ROM (degrees) | Exercise Group | 100.7 ± 3.4 (97–107) | 109.8 ± 2.6 (105–115) | 112.8 ± 2.6 (108–118) | <0.0001 | <0.0001 | <0.0001 |
| Exercise Plus sEMG Biofeedback Group | 100.8 ± 3.8 (94–110) | 114.5 ± 5.8 (105–126) | 118.2 ± 6.2 (108–128) | ||||
| Total | 100.8 ± 4.2 (94–110) | 118.9 ± 4.2 (111–126) | 123.2 ± 3.7 (116–128) | ||||
| External Rotation ROM (degrees) | Exercise Group | 59.1 ± 7.9 (47–73) | 66.9 ± 7.2 (58–80) | 70.1 ± 6.8 (62–82) | 0.012 | <0.0001 | <0.0001 |
| Exercise Plus sEMG Biofeedback Group | 59.6 ± 6.9 (48–72) | 74.0 ± 3.2 (70–80) | 78.1 ± 2.9 (74–82) | ||||
| Total | 59.4 ± 7.3 (47–73) | 70.6 ± 6.5 (58–80) | 74.2 ± 6.5 (62–82) |
| Exercise Plus sEMG Biofeedback Group | Exercise Group | ||||
|---|---|---|---|---|---|
| Outcome | Time | Contrast (95%CI) | p-Value | Contrast (95%CI) | p-Value |
| Supraspinatus RMS—limb affected by SP | T1 vs. T0 | 71.4 (65.4–77.5) | <0.0001 | 43.9 (37.7–50.2) | <0.0001 |
| T2 vs. T0 | 84.7 (78.6–90.7) | <0.0001 | 53.3 (47.1–59.2) | <0.0001 | |
| T2 vs. T1 | 13.2 (7.2–19.2) | <0.0001 | 9.4 (3.2–15.6) | 0.004 | |
| Supraspinatus RMS—limb free from SP | T1 vs. T0 | 10.1 (7.0–13.2) | <0.0001 | 11.7 (8.5–14.9) | <0.0001 |
| T2 vs. T0 | 13.0 (9.9–16.1) | <0.0001 | 14.7 (11.6–17.9) | <0.0001 | |
| T2 vs. T1 | 2.9 (−0.2–6.0) | 0.066 | 3.0 (−0.1–6.2) | 0.061 | |
| WUSPI | T1 vs. T0 | −67.6 (−71.2–−63.9) | <0.0001 | −39.9 (−43.6–−36.1) | <0.0001 |
| T2 vs. T0 | −74.0 (−77.6–−70.4) | <0.0001 | −43.9 (−47.6–−40.1) | <0.0001 | |
| T2 vs. T1 | −6.4 (−10.0–−2.8) | 0.001 | −4.0 (−7.7–−0.3) | 0.037 | |
| Abduction ROM | T1 vs. T0 | 18.1 (16.3–19.8) | <0.0001 | 9.1 (7.3–10.9) | <0.0001 |
| T2 vs. T0 | 22.4 (20.7–24.2) | <0.0001 | 12.1 (10.3–13.9) | <0.0001 | |
| T2 vs. T1 | 4.4 (2.6–6.1) | <0.0001 | 3.0 (1.2–4.8) | 0.001 | |
| External Rotation ROM | T1 vs. T0 | 14.3 (12.3–16.4) | <0.0001 | 7.9 (5.7–10.0) | <0.0001 |
| T2 vs. T0 | 18.4 (16.3–20.5) | <0.0001 | 11.0 (8.8–13.2) | <0.0001 | |
| T2 vs. T1 | 4.1 (2.0–6.1) | <0.0001 | 3.1 (1.0–5.3) | 0.005 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farì, G.; Megna, M.; Ranieri, M.; Agostini, F.; Ricci, V.; Bianchi, F.P.; Rizzo, L.; Farì, E.; Tognolo, L.; Bonavolontà, V.; et al. Could the Improvement of Supraspinatus Muscle Activity Speed up Shoulder Pain Rehabilitation Outcomes in Wheelchair Basketball Players? Int. J. Environ. Res. Public Health 2023, 20, 255. https://doi.org/10.3390/ijerph20010255
Farì G, Megna M, Ranieri M, Agostini F, Ricci V, Bianchi FP, Rizzo L, Farì E, Tognolo L, Bonavolontà V, et al. Could the Improvement of Supraspinatus Muscle Activity Speed up Shoulder Pain Rehabilitation Outcomes in Wheelchair Basketball Players? International Journal of Environmental Research and Public Health. 2023; 20(1):255. https://doi.org/10.3390/ijerph20010255
Chicago/Turabian StyleFarì, Giacomo, Marisa Megna, Maurizio Ranieri, Francesco Agostini, Vincenzo Ricci, Francesco Paolo Bianchi, Ludovica Rizzo, Eleonora Farì, Lucrezia Tognolo, Valerio Bonavolontà, and et al. 2023. "Could the Improvement of Supraspinatus Muscle Activity Speed up Shoulder Pain Rehabilitation Outcomes in Wheelchair Basketball Players?" International Journal of Environmental Research and Public Health 20, no. 1: 255. https://doi.org/10.3390/ijerph20010255
APA StyleFarì, G., Megna, M., Ranieri, M., Agostini, F., Ricci, V., Bianchi, F. P., Rizzo, L., Farì, E., Tognolo, L., Bonavolontà, V., Fiore, P., & Reis, V. M. (2023). Could the Improvement of Supraspinatus Muscle Activity Speed up Shoulder Pain Rehabilitation Outcomes in Wheelchair Basketball Players? International Journal of Environmental Research and Public Health, 20(1), 255. https://doi.org/10.3390/ijerph20010255











