Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review
Abstract
1. Introduction
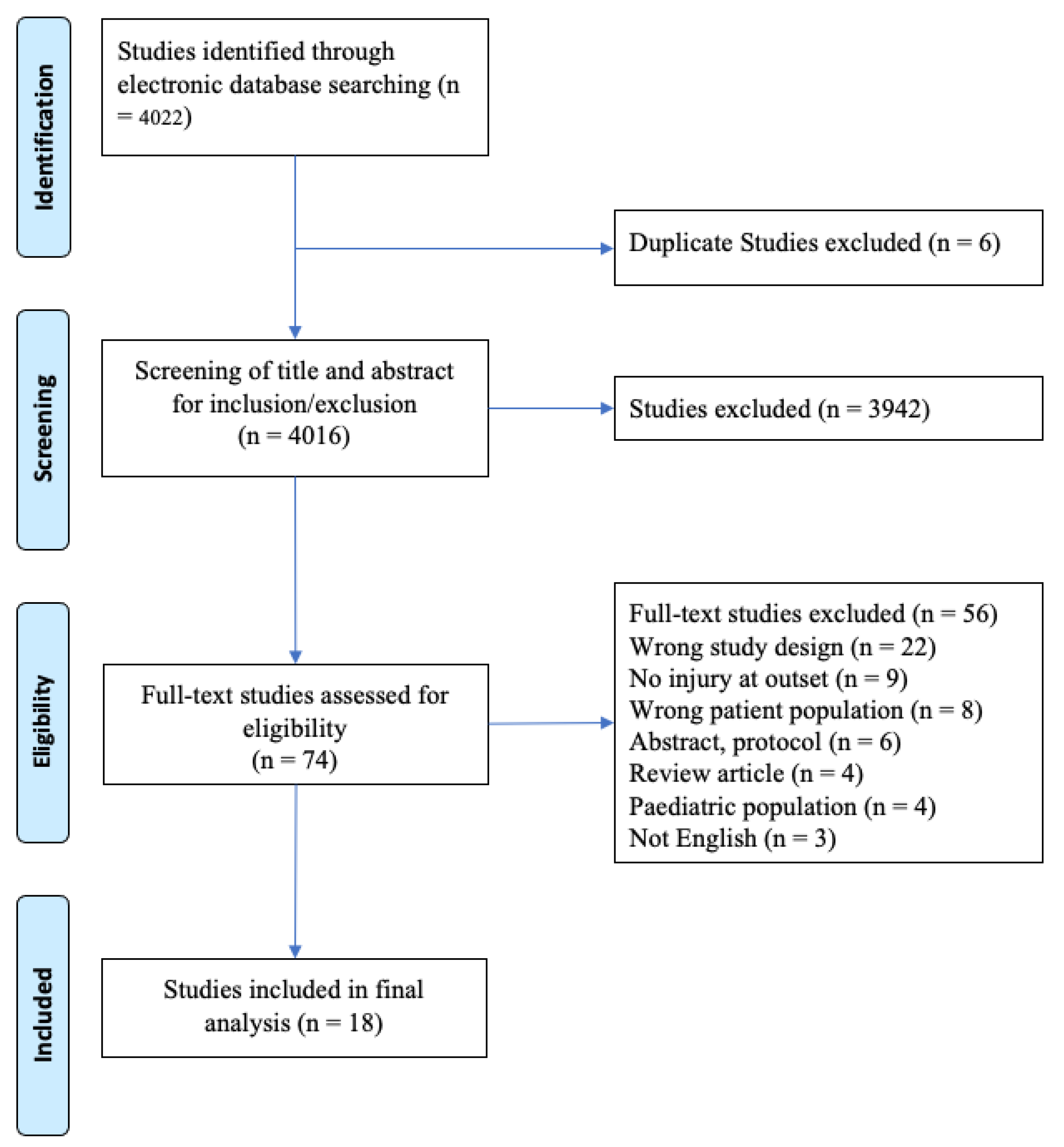
2. Materials and Methods
2.1. Search Strategy
2.2. Selection Criteria
2.3. Data Extraction
2.4. Quality Assessment
3. Results
3.1. Study Selection and Characteristics
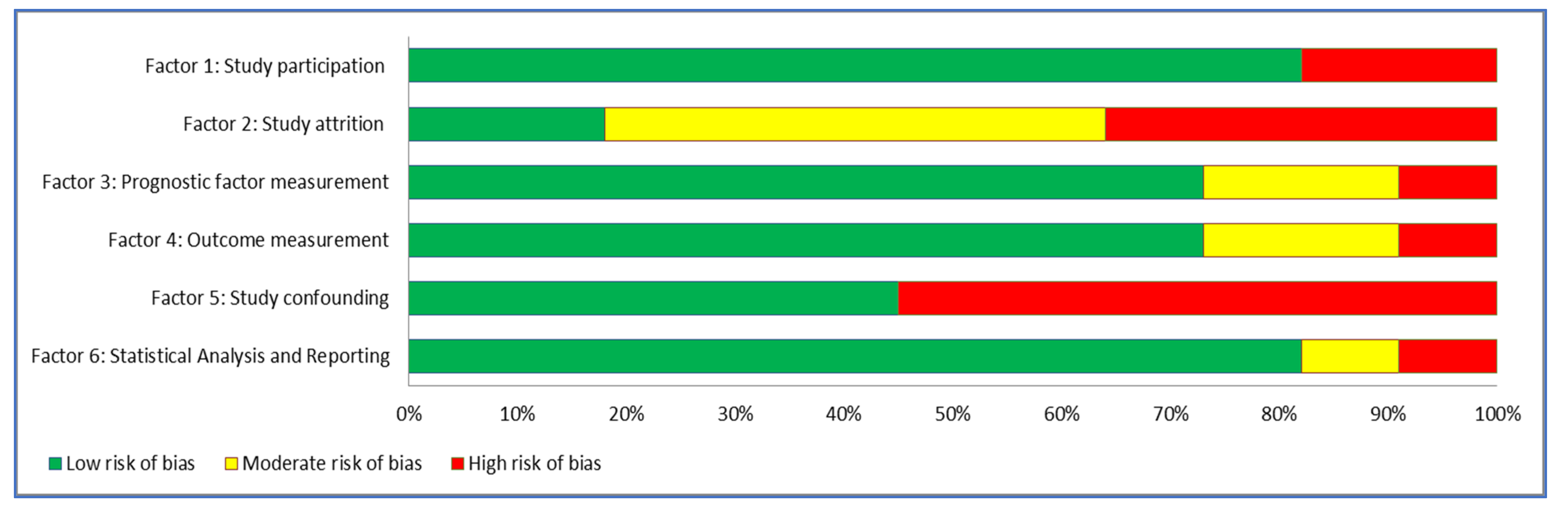
3.2. Study Quality (Risk of Bias)
3.3. Risk Factors for Persistent Pain
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diseases, G.B.D.; Injuries, C. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar]
- Rosenbloom, B.N.; Khan, S.; McCartney, C.; Katz, J. Systematic review of persistent pain and psychological outcomes following traumatic musculoskeletal injury. J. Pain Res. 2013, 6, 39. [Google Scholar] [CrossRef]
- Radresa, O.; Chauny, J.-M.; Lavigne, G.; Piette, E.; Paquet, J.; Daoust, R. Current views on acute to chronic pain transition in post-traumatic patients. J. Trauma Acute Care Surg. 2014, 76, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Young Casey, C.; Greenberg, M.A.; Nicassio, P.M.; Harpin, R.E.; Hubbard, D. Transition from acute to chronic pain and disability: A model including cognitive, affective, and trauma factors. Pain 2008, 134, 69–79. [Google Scholar] [CrossRef] [PubMed]
- Artus, M.; Campbell, P.; Mallen, C.D.; Dunn, K.M.; van der Windt, D.A. Generic prognostic factors for musculoskeletal pain in primary care: A systematic review. BMJ Open 2017, 7, e012901. [Google Scholar] [CrossRef]
- Truong, L.K.; Mosewich, A.D.; Holt, C.J.; Le, C.Y.; Miciak, M.; Whittaker, J.L. Psychological, social and contextual factors across recovery stages following a sport-related knee injury: A scoping review. Br. J. Sports Med. 2020, 54, 1149–1156. [Google Scholar] [CrossRef]
- Puentedura, E.J.; Louw, A. A neuroscience approach to managing athletes with low back pain. Phys. Ther. Sport 2012, 13, 123–133. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef]
- Hayden, J.A.; Côté, P.; Bombardier, C. Evaluation of the quality of prognosis studies in systematic reviews. Ann. Intern. Med. 2006, 144, 427–437. [Google Scholar] [CrossRef] [PubMed]
- Hayden, J.A.; van der Windt, D.A.; Cartwright, J.L.; Côté, P.; Bombardier, C. Assessing bias in studies of prognostic factors. Ann. Intern. Med. 2013, 158, 280–286. [Google Scholar] [CrossRef]
- Hemingway, H.; Philipson, P.; Chen, R.; Fitzpatrick, N.K.; Damant, J.; Shipley, M.; Abrams, K.R.; Moreno, S.; McAllister, K.S.; Palmer, S. Evaluating the quality of research into a single prognostic biomarker: A systematic review and meta-analysis of 83 studies of C-reactive protein in stable coronary artery disease. PLoS Med. 2010, 7, e1000286. [Google Scholar] [CrossRef] [PubMed]
- Kamper, S.J.; Hancock, M.J.; Maher, C.G. Optimal designs for prediction studies of whiplash. Spine 2011, 36, S268–S274. [Google Scholar] [CrossRef]
- Tate, R.L.; Douglas, J. Use of reporting guidelines in scientific writing: PRISMA, CONSORT, STROBE, STARD and other resources. Brain Impair. 2011, 12, 1–21. [Google Scholar] [CrossRef]
- Slavin, R.E. Best evidence synthesis: An intelligent alternative to meta-analysis. J. Clin. Epidemiol. 1995, 48, 9–18. [Google Scholar] [CrossRef]
- Harris, I.A.; Young, J.M.; Rae, H.; Jalaludin, B.B.; Solomon, M.J. Factors associated with back pain after physical injury: A survey of consecutive major trauma patients. Spine 2007, 32, 1561–1565. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.; Williamson, O.; Hogg, M.; Arnold, C.; O’Donnell, M.L. Determinants of chronic pain 3 years after moderate or serious injury. Pain Med. 2013, 14, 336–344. [Google Scholar] [CrossRef]
- Holmes, A.; Williamson, O.; Hogg, M.; Arnold, C.; Prosser, A.; Clements, J.; Konstantatos, A.; O’Donnell, M. Predictors of pain 12 months after serious injury. Pain Med. 2010, 11, 1599–1611. [Google Scholar] [CrossRef]
- Williamson, O.D.; Epi, G.D.C.; Gabbe, B.J.; Physio, B.; Cameron, P.A.; Edwards, E.R.; Richardson, M.D.; Group, V.O.T.O.R.P. Predictors of moderate or severe pain 6 months after orthopaedic injury: A prospective cohort study. J. Orthop. Trauma 2009, 23, 139–144. [Google Scholar] [CrossRef]
- Friedman, B.W.; Conway, J.; Campbell, C.; Bijur, P.E.; John Gallagher, E. Pain one week after an emergency department visit for acute low back pain is associated with poor three-month outcomes. Acad. Emerg. Med. 2018, 25, 1138–1145. [Google Scholar] [CrossRef] [PubMed]
- Silva, F.M.; Brismée, J.-M.; Sizer, P.S.; Hooper, T.L.; Robinson, G.E.; Diamond, A.B. Musicians injuries: Upper quarter motor control deficits in musicians with prolonged symptoms-A case-control study. Musculoskelet. Sci. Pract. 2018, 36, 54–60. [Google Scholar] [CrossRef]
- Wellsandt, E.; Axe, M.J.; Snyder-Mackler, L. Poor performance on Single-Legged hop tests associated with development of posttraumatic knee osteoarthritis after anterior cruciate ligament injury. Orthop. J. Sports Med. 2018, 6, 2325967118810775. [Google Scholar] [CrossRef] [PubMed]
- Rosenbloom, B.N.; Katz, J.; Chin, K.Y.; Haslam, L.; Canzian, S.; Kreder, H.J.; McCartney, C.J. Predicting pain outcomes after traumatic musculoskeletal injury. Pain 2016, 157, 1733–1743. [Google Scholar] [CrossRef] [PubMed]
- Modarresi, S.; Suh, N.; Walton, D.M.; MacDermid, J.C. Depression affects the recovery trajectories of patients with distal radius fractures: A latent growth curve analysis. Musculoskelet. Sci. Pract. 2019, 43, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Andersen, T.E.; Karstoft, K.I.; Brink, O.; Elklit, A. Pain-catastrophizing and fear-avoidance beliefs as mediators between post-traumatic stress symptoms and pain following whiplash injury–A prospective cohort study. Eur. J. Pain 2016, 20, 1241–1252. [Google Scholar] [CrossRef]
- Heidari, J.; Mierswa, T.; Kleinert, J.; Ott, I.; Levenig, C.; Hasenbring, M.; Kellmann, M. Parameters of low back pain chronicity among athletes: Associations with physical and mental stress. Phys. Ther. Sport 2016, 21, 31–37. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Pierik, J.; IJzerman, M.J.; Gaakeer, M.; Vollenbroek-Hutten, M.M.R.; Van Vugt, A.; Doggen, C.J.M. Incidence and prognostic factors of chronic pain after isolated musculoskeletal extremity injury. Eur. J. Pain 2016, 20, 711–722. [Google Scholar] [CrossRef]
- Hallegraeff, J.M.; Kan, R.; van Trijffel, E.; Reneman, M.F. State anxiety improves prediction of pain and pain-related disability after 12 weeks in patients with acute low back pain: A cohort study. J. Physiother. 2020, 66, 39–44. [Google Scholar] [CrossRef]
- Åkerblom, S.; Larsson, J.; Malmström, E.-M.; Persson, E.; Westergren, H. Acceptance: A factor to consider in persistent pain after neck trauma. Scand. J. Pain 2019, 19, 733–741. [Google Scholar] [CrossRef]
- Söderlund, A.; Löfgren, M.; Stålnacke, B.-M. Predictors before and after multimodal rehabilitation for pain acceptance and engagement in activities at a 1-year follow-up for patients with whiplash-associated disorders (WAD)—A study based on the Swedish Quality Registry for Pain Rehabilitation (SQRP). Spine J. 2018, 18, 1475–1482. [Google Scholar] [CrossRef]
- Kovacs, F.M.; Abraira, V.; Zamora, J.; Fernández, C.; Network, S.B.P.R. The transition from acute to subacute and chronic low back pain: A study based on determinants of quality of life and prediction of chronic disability. Spine 2005, 30, 1786–1792. [Google Scholar] [CrossRef]
- Potter, R.G.; Jones, J.M.; Boardman, A.P. A prospective study of primary care patients with musculoskeletal pain: The identification of predictive factors for chronicity. Br. J. Gen. Pract. 2000, 50, 225–227. [Google Scholar] [PubMed]
- O’Connor, S.R.; Bleakley, C.M.; Tully, M.A.; McDonough, S.M. Predicting Functional Recovery after Acute Ankle Sprain. PLoS ONE 2013, 8, e72124. [Google Scholar] [CrossRef] [PubMed]
- Friedman, B.W.; Gensler, S.; Yoon, A.; Nerenberg, R.; Holden, L.; Bijur, P.E.; Gallagher, E.J. Predicting three-month functional outcomes after an ED visit for acute low back pain. Am. J. Emerg. Med. 2017, 35, 299–305. [Google Scholar] [CrossRef]
- Daoust, R.; Paquet, J.; Moore, L.; Emond, M.; Gosselin, S.; Lavigne, G.; Choiniere, M.; Boulanger, A.; Mac-Thiong, J.-M.; Chauny, J.-M. Early factors associated with the development of chronic pain in trauma patients. Pain Res. Manag. 2018, 2018, 7203218. [Google Scholar] [CrossRef] [PubMed]
- Jenewein, J.; Moergeli, H.; Wittmann, L.; Büchi, S.; Kraemer, B.; Schnyder, U. Development of chronic pain following severe accidental injury. Results of a 3-year follow-up study. J. Psychosom. Res. 2009, 66, 119–126. [Google Scholar] [CrossRef] [PubMed]
- López-Martínez, A.; Ramírez-Maestre, C.; Esteve, R. An examination of the structural link between post-traumatic stress symptoms and chronic pain in the framework of fear-avoidance models. Eur. J. Pain 2014, 18, 1129–1138. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Párraga, G.T.; López-Martínez, A.E. The contribution of posttraumatic stress symptoms to chronic pain adjustment. Health Psychol. 2014, 33, 958. [Google Scholar] [CrossRef]
- Stratton, K.J.; Clark, S.L.; Hawn, S.E.; Amstadter, A.B.; Cifu, D.X.; Walker, W.C. Longitudinal interactions of pain and posttraumatic stress disorder symptoms in US Military service members following blast exposure. J. Pain 2014, 15, 1023–1032. [Google Scholar] [CrossRef]
- Bérubé, M.; Choinière, M.; Laflamme, Y.G.; Gélinas, C. Acute to chronic pain transition in extremity trauma: A narrative review for future preventive interventions (part 1). Int. J. Orthop. Trauma Nurs. 2016, 23, 47–59. [Google Scholar] [CrossRef]
- Bérubé, M.; Choinière, M.; Laflamme, Y.G.; Gélinas, C. Acute to chronic pain transition in extremity trauma: A narrative review for future preventive interventions (part 2). Int. J. Orthop. Trauma Nurs. 2017, 24, 59–67. [Google Scholar] [CrossRef]
- Rivara, F.P.; MacKenzie, E.J.; Jurkovich, G.J.; Nathens, A.B.; Wang, J.; Scharfstein, D.O. Prevalence of pain in patients 1 year after major trauma. Arch. Surg. 2008, 143, 282–287. [Google Scholar] [CrossRef] [PubMed]
| Studies | Year of Publication | Country of Study | Study Design | Participants | Follow-upPeriods | Outcome | Risk Factors | Sample Size |
|---|---|---|---|---|---|---|---|---|
| Hallegraeff et al. [27] | 2020 | The Netherlands | Longitudinal prospective cohort | Acute low back pain (LBP with <6 weeks duration with or without radiating pain and had been pain free for at least 3 months before the onset of their current back pain) Age 18–60 years | Baseline and 12 weeks | Pain: NRS and PDI Anxiety: STAI-Y (STAI-S and STAI_T) | Pain intensity at outset Duration of pain Physical workload State and Trait Anxiety | 225 |
| Akerblom et al. [28] | 2019 | Sweden | Retrospective cohort | Persistent pain following neck trauma | NR | Anxiety and depression: HADS Acceptance: CPAQ-8 Pain: distribution and severity: MPI | Participant demographics, anxiety, depression, acceptance, persistent pain | 565 |
| Modarresi et al. [23] | 2019 | Canada | Retrospective Exploratory cohort | Adults > 18 years who were recovering from distal radius fracture | Baseline, 3, 6, and 12 months | Pain and disability: PRWE Comorbidities: SCQ | Depression, participant demographics, education and employment status, pain and disability | 318 |
| Friedman et al. [19] | 2018 | USA | Retrospective cohort | Acute LBP | Baseline, 1 week following ED visit and 3 month follow-up | LBP-related functional impairment (RMDQ) Presence of moderate or severe LBP | Pain and functional impairment | 354 |
| Soderlund et al. [29] | 2018 | Sweden | Prospective cohort | General population with whiplash history 2–4 months prior to recruitment. WAD grade 1–2 Age 18–65 years | Baseline, prior to discharge and 1 year follow-up | CPAQ MPQ TSK | Pain acceptance, fear of movement and fear of (re)injury | 177 |
| Wellsandt et al. [21] | 2018 | USA | Prospective cohort | Athletes with acute, unilateral ACL injury Athletes were level 1 or 2 athletes | 5 years post initial injury: Baseline), immediately following 10 additional physical therapy sessions and 6 months following completion | Quadriceps strength: MVIC Impairment and functional limitation KOS-ADLS General function GRS IKDC | Knee function | 66 |
| Silva et al. [20] | 2018 | USA | Case-control study | Student or professional musicians with upper limb injuries Age 18–65 years | NR | Cervical flexor endurance test Scapular dyskinesis test Craniocervical test | Motor control | 72 |
| Andersen et al. [24] | 2016 | Denmark | Longitudinal cohort | General population admitted to hospital emergency department with traumatic whiplash QTFC-WAD grade 1–3 Age > 18 years | Baseline, 3 months and 6 months | Pain: NRS Fear-avoidance beliefs: Orebro musculoskeletal pain screening questionnaire PTSS: Harvard trauma questionnaire Depressive symptoms: HADS Catastrophizing: PCS | Pain at outset Pain catastrophizing PTSS Depression Fear avoidance | 198 |
| Heidari et al. [25] | 2016 | Germany | Longitudinal cohort | Presence of non-specific back pain Participation in some form of active exercise therapy Age > 18 years | 6 months | Back pain: Chronic pain grade Stress: Recovery stress questionnaire and trier inventory for assessment of chronic stress | Pain and chronification stress | 139 |
| Rosenbloom et al. [22] | 2016 | Canada | prospective, observational, longitudinal design | Traumatic musculoskeletal injury Admitted to hospital for >2 days Age > 18 years | 14 days and 4 months | Neuropathic pain: self-report Leeds assessment of neuropathic symptoms and signs and NRS BPI Mental health: HADS Pain anxiety: pain anxiety symptom scale Post-traumatic stress disorder checklist pain self-efficacy checklist Pain catastrophizing scale Anxiety sensitivity index | Chronicity | 128 |
| Pierik et al. [26] | 2016 | The Netherlands | Prospective 1 year follow-up study | Isolated musculoskeletal injury caused by blunt trauma Age 18–69 years | 1 week, 6 weeks, 3 months, and 6 months | Pain: NRS HRQoL: SF-36 Anxiety and depression: HADS Pain Catastrophizing: PCS Kinesiophobia: TSK Pain experience during follow-up: BPI | Chronic pain 6 months post-injury | 435 |
| Holmes et al. [16] | 2013 | Australia | 3 year follow-up cohort | Scored >2 on abbreviated injury score Admitted for more than 24 h Age 18–70 years | 3 months, 12 months, and 3 years | Pain: NRS Disability: SF-36 Social Support: Multidimensional scale of perceived social support Mental health: NRS Psychological symptoms: HADS | Presence of chronic pain Pain-related disability | 220 |
| O’Connor et al. [32] | 2013 | United Kingdom | Secondary analysis | Acute ankle injury Age > 16 years | 4 weeks and 4 months | Pain: Y/N Injury grade | Ankle function | 85 |
| Holmes et al. [17] | 2010 | Australia | prospective cohort with 12 months follow-up | Scored > 2 on abbreviated injury score Admitted for more than 24 h Age 18–70 years | 3 months and 12 months | Pain: NRS Disability: SF-36 Social Support: Multidimensional scale of perceived social support Mental health: NRS Psychological symptoms: HADS | Presence of chronic pain Pain-related disability | 238 |
| Williamson et al. [18] | 2009 | Australia | Prospective cohort study | Admitted to hospital with orthopedic injury | In hospital and 6 months | SF12 Pain: VAS | Chronic pain 6 months post-injury | 1290 |
| Harris et al. [15] | 2007 | Australia | Cross- sectional study | Major trauma after accidental injury Age > 18 years | 1–6 years post-injury | PTSD: PTSD checklist Back pain in the preceding week General health: SF-36 Disability: ODI | NR | 355 |
| Kovacs et al. [30] | 2005 | Spain | Longitudinal study | Acute LBP with or without radiation to leg | 14 days, 59 days | Pain: VAS Disability: RMQ and EQ-5D | Pain and disability | 366 |
| Potter et al. [31] | 2000 | United Kingdom | Prospective longitudinal study | Uncomplicated musculoskeletal pain Age 18–65 years | Baseline and 12 weeks | Health: general health questionnaire Pain: VAS, pain measurement inventory Coping: active coping score and passive coping score | chronicity | 141 |
| Factor | Hallegraeff et al. (2020) [27] | Akerblom et al. (2019) [28] | Modarresi et al. (2019) [23] | Friedman et al. (2018) [33] | Soderlund et al. (2018) [29] | Wellsandt et al. (2018) [21] | Silva et al. (2018) [20] | Andersen et al. (2016) [24] | Heidari et al. (2016) [25] | Rosenbloom et al. (2016) [22] | Pierik et al. (2015) [26] | Holmes et al. (2013) [16] | O’Connor et al. (2013) [32] | Holmes et al. (2010) [17] | Williamson et al. (2009) [18] | Harris et al. (2007) [15] | Kovacs et al. (2005) [30] | Potter et al. (2000) [31] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study participation summary | L | L | L | L | L | L | L | L | H | L | H | L | L | L | L | L | L | L |
| Study attrition summary | L | M | M | M | L | L | L | H | H | L | M | M | M | M | L | H | H | H |
| Prognostic factor measurement summary | L | L | M | M | L | M | H | L | L | L | L | L | M | L | M | L | L | H |
| Outcome measurement summary | L | L | L | L | L | L | L | L | L | L | L | L | L | L | M | L | L | H |
| Study confounding summary | L | L | M | M | L | M | H | L | H | L | L | L | H | L | H | H | H | H |
| Statistical analysis and presentation summary | L | L | L | L | L | L | L | L | L | L | L | L | L | L | L | M | L | H |
| Overall | +++ | +++ | ++ | ++ | +++ | ++ | + | ++ | + | +++ | ++ | +++ | ++ | +++ | ++ | + | + | + |
| Citations | Age, Y Mean (SD) | Gender, n (%) | Activity | Injury Type | Region | Risk Factors | Results |
|---|---|---|---|---|---|---|---|
| Hallegraeff et al. [27] | 41 (12) | Female 103 (51%) | Physically active 141 (69%) | Non-specific acute LBP | Lumbar | State and trait anxiety Pain intensity at outset Pain related disability Duration of LBP Widespread pain | State anxiety levels (OR 1.1 (95% CI 1.0–1.1, p = 0.00)) and pain intensity (OR 1.3 (95% CI 1.1–1.7 p = 0.01)) at baseline were independent predictors of still having pain at 12 weeks. Trait anxiety was not found to be predictive of pain at 12 weeks. |
| Akerblom et al. [28] | Median age 39 | Traumatic neck injury | Neck | Participant demographics, anxiety, depression, acceptance, persistent pain | Widespread Pain: females and lower acceptance Pain Interference: females, depression, and lower acceptance Pain Severity: lower acceptance, increased levels of anxiety or depression, and lower education level. | ||
| Modarresi et al. [23] | 59.6 ± 11.9 | Female 80.5% | NR | Distal radius fracture | Wrist | Depression, participant demographics, education and employment status, pain and disability | Majority recovered within normal limits, depression was associated with non-recovery 24% v 8%, X2 = 6.36, p = 0.01 (rapid recovery) and 16%, X2 = 4.07, p = 0.04 (slow recovery) No other factors associated with slow/non recovery. |
| Friedman et al. [33] | 38 (12) | Female 160 (45) | NR | Acute low back pain | Lumbar | Pain one week following injury Functional impairment | At the 3 month follow-up 39% of patients reported LBP related functional impairment and 16% reported moderate to severe LBP. The baseline STaRT score was not associated with long-term pain. The length of pain duration anticipated by the patient (>7 days) was associated with both the pain at 3 months (OR 2.31 (95% CI 1.17–4.54)) and functional disability (OR 1.93 (95% CI 1.09–3.43)) |
| Soderlund et al. [29] | 39.5 | Female 225 | NR | Whiplash | Neck | Fear of movement and fear of (re)injury Pain acceptance | Patients with support from significant others and lower levels of fear of movement and better outcome predictions were associated with better outcomes at the 1 year follow-up than those without. |
| Wellsandt et al. [21] | Non-OA 28.8 (11.3) OA 28.3 (11.5) | Non-OA Male/ Female: 43/24 OA Male/ Female: 6/3 | Level 1 52 Level 2 24 | ACL | Knee | Knee function | The risk of developing knee OA 5 years after experiencing an ACL injury is increased when individuals had poor performance in the single-legged hop test. This result was not the same as patients who underwent ACL reconstruction. |
| Silva et al. [20] | Symptomatic 23.3 ± 8.21 CG 25.03 ± 10.5 | EG: M/F 12/24 CG: M/F 12/24 | Exercise Days 3.1 Minutes 164.9 | Upper limb and neck pain | Upper limb and neck | Motor control | Musicians who present with upper quadrant playing-related pain had reduced performance in clinical tests and demonstrated poor scapular motor function. |
| Andersen et al. [24] | 36.79 (12.61) | Female, 61.6% | NR | Whiplash injury | Neck | Demographics Fear avoidance (FA) beliefs Catastrophizing Depression | 35.4% as non-recovered. The non-recovered (the medium stable, high stable and very high stable trajectories) displayed significantly higher levels of post-traumatic stress symptoms (PTSS), pain-catastrophizing (PCS), FA, and depression compared to the recovered trajectories. Importantly, PCS and FA beliefs mediated the effect of PTSS on pain intensity |
| Heidari et al. [25] | 32.24 (11.32) | Female, 41% | Athletes | Musculoskeletal pain | Back | Pain factors Stress | No significant differences noted between the chronic group and non-chronic group, insignificantly elevated stress levels. |
| Rosenbloom et al. [22] | 43.0 (19.9) | Female, 32.2% | NR | Motor- vehicle accidents | Multiple locations | Demographics, Pain factors, Mental health | The deleterious effects of neuropathic pain were seen in the 32% of young trauma patients who had symptoms of neuropathic pain 4 months after injury. The pain interfered significantly with their daily living, employment, mood, sleep, and enjoyment of life. |
| Pierik et al. [26] | Median: 50.0 (IQR 36.0–60.0) | Female, 60.5% | NR | Fracture: 328 (75.4%) Dislocation: 25 (5.7%) Sprains and Strains: 47 (10.8%) Contusion: 24 (5.5%) Muscle rupture: 10 (2.3%) | Lower extremity | Demographics Pain factors Psychological factors Injury and treatment factors Clinical Factors | Age: 40–49: OR 1.03 (95% CI 0.28–1.07); 50–59: OR 3.43 (95% CI 1.29–9.09); 60–69: OR 3.85 (95% CI 1.47–10.08) Pain level at discharge, severe pain: OR 3.41 (95% CI 1.73–6.71); Preexisting chronic pain: OR 6.09 (95% CI 3.18–11.69); Pre-injury physical, Poor: OR 3.18 (95% CI 1.68–6.02); Comorbidities, yes: OR 2.87 (95% CI 1.53–5.40) |
| Holmes et al. [16] | Chronic Pain: 41.4 (13.0) No Chronic pain: 38.5 (13.1) | Chronic Pain, female: 31% No Chronic pain, female: 27% | NR | Multiple trauma | Multiple locations | Demographics Pain factors Psychological factors Social support | Initial pain: OR 1.26 (95% CI 1.09–1.46); Injury severity: OR 1.12 (95% CI 1.01–1.24) |
| O’Connor et al. [32] | 27 (9.8) | Female, 30% | NR | Inversion sprain | Ankle | Demographics Injury variables | Increased risk of poor function pain med joint line: 4.92 (95% CI 1.39–8.44); pain weight-bearing ankle dorsiflexion: 6.8 (95% CI 4.8–8.7) |
| Holmes et al. [17] | Chronic Pain: 42 (14) No Chronic pain: 39 (14) | Chronic Pain, female: 71% No Chronic pain, female: 75% | NR | Multiple trauma | Multiple locations | Demographics Pain factors Psychological factors Social support | Number of injuries: OR 1.14 (95% CI 1.02–1.27); Initial pain: OR 1.34 (95% CI 1.13–1.61); Pain control attitudes: OR 0.79 (95% CI 0.69–0.99) |
| Williamson et al. [18] | Range: 14–95 | Female: 39% | NR | Multiple trauma | Multiple locations | Demographics, Pain factors Function | Self-reported pre-injury, pain-related disability, and moderate or severe pain at discharge from the acute hospital were found to be independent predictors of moderate or severe pain at 6 months post-injury. |
| Harris et al. [15] | 47.8 (19–91) | Female, 28% | NR | Musculoskeletal pain | Back | Demographic, Clinical factors Injury severity Psychosocial factors | PTSD: OR 4.92 (95% CI 2.83–8.56); >3 chronic illness: OR 5.83 (95% CI 2.41–14.09). The presence of back pain was significantly associated with increasing chronic illnesses at follow-up. |
| Kovacs et al. [30] | 47.7 (15.5) | Female, 54% | NR | Musculoskeletal pain | Low back | Demographics, Pain factors Function | The more pain an individual had at baseline the increased risk of disability at 60 days follow-up. |
| Potter et al. [31] | Chronic Pain: <40 = 28 (41.2%) 40–50 = 23 (33.8%) >55 = 17 (25.0%) Acute Pain: <40 = 36 (49.3%) 40–50 = 15 (20.5%) >55 = 22(30.1%) | Chronic Pain, female: 64.5% Acute Pain, female: 53.4% | NR | Musculoskeletal pain | Multiple locations | Demographics, Health status Pain factors | Pain intensity, active coping score, and previous episode of continuous pain were significantly and independently related to the development of chronic pain. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkassabi, O.; Voogt, L.; Andrews, P.; Alhowimel, A.; Nijs, J.; Alsobayel, H. Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review. Int. J. Environ. Res. Public Health 2022, 19, 9318. https://doi.org/10.3390/ijerph19159318
Alkassabi O, Voogt L, Andrews P, Alhowimel A, Nijs J, Alsobayel H. Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review. International Journal of Environmental Research and Public Health. 2022; 19(15):9318. https://doi.org/10.3390/ijerph19159318
Chicago/Turabian StyleAlkassabi, Othman, Lennard Voogt, Pamela Andrews, Ahmad Alhowimel, Jo Nijs, and Hana Alsobayel. 2022. "Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review" International Journal of Environmental Research and Public Health 19, no. 15: 9318. https://doi.org/10.3390/ijerph19159318
APA StyleAlkassabi, O., Voogt, L., Andrews, P., Alhowimel, A., Nijs, J., & Alsobayel, H. (2022). Risk Factors to Persistent Pain Following Musculoskeletal Injuries: A Systematic Literature Review. International Journal of Environmental Research and Public Health, 19(15), 9318. https://doi.org/10.3390/ijerph19159318








