Can Homecare Chronic Respiratory Disease Patients with Home Oxygen Treatment (HOT) in Southern Okinawa, Japan Be Evacuated Ahead of the Next Anticipated Tsunami?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants and Data Collection
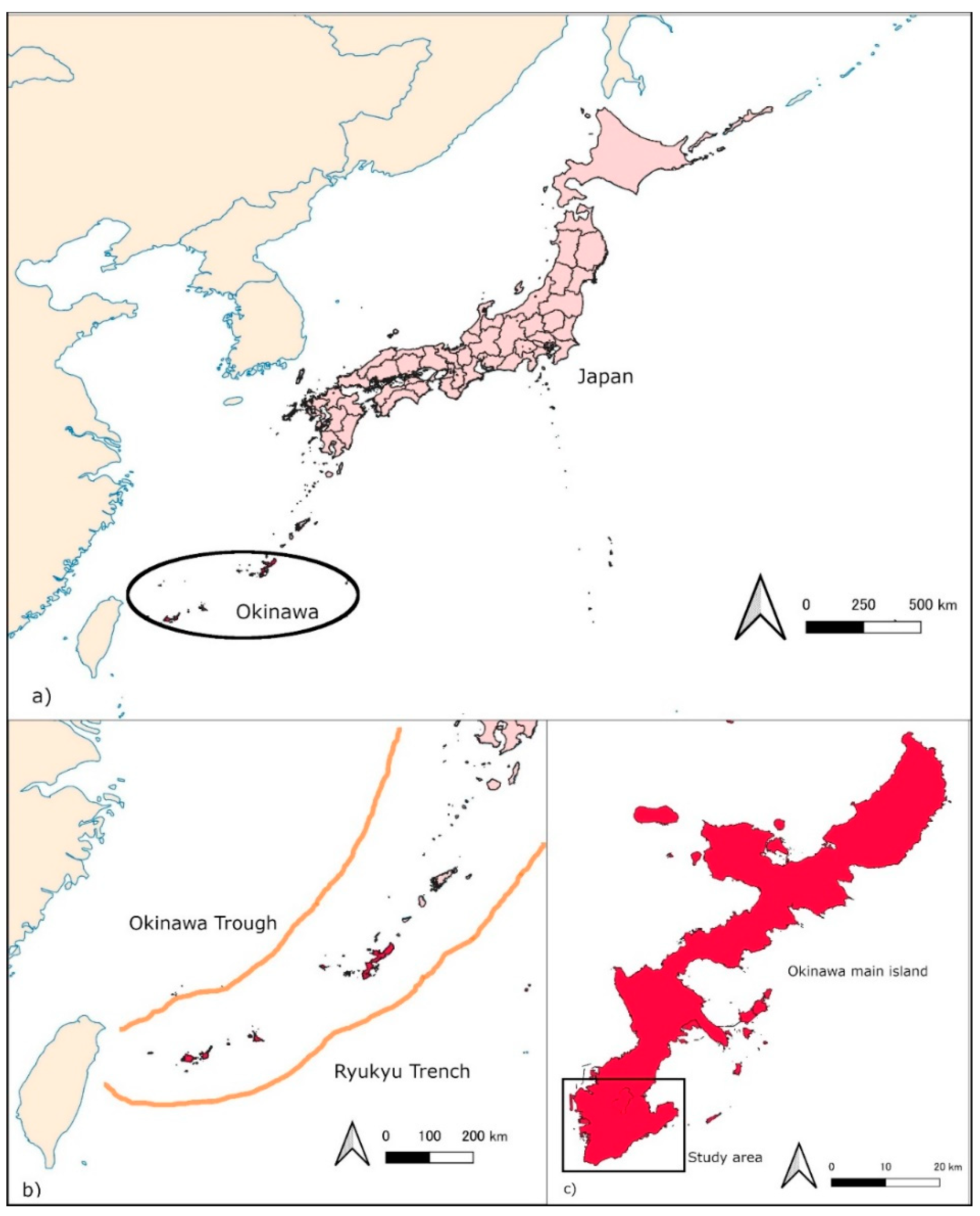
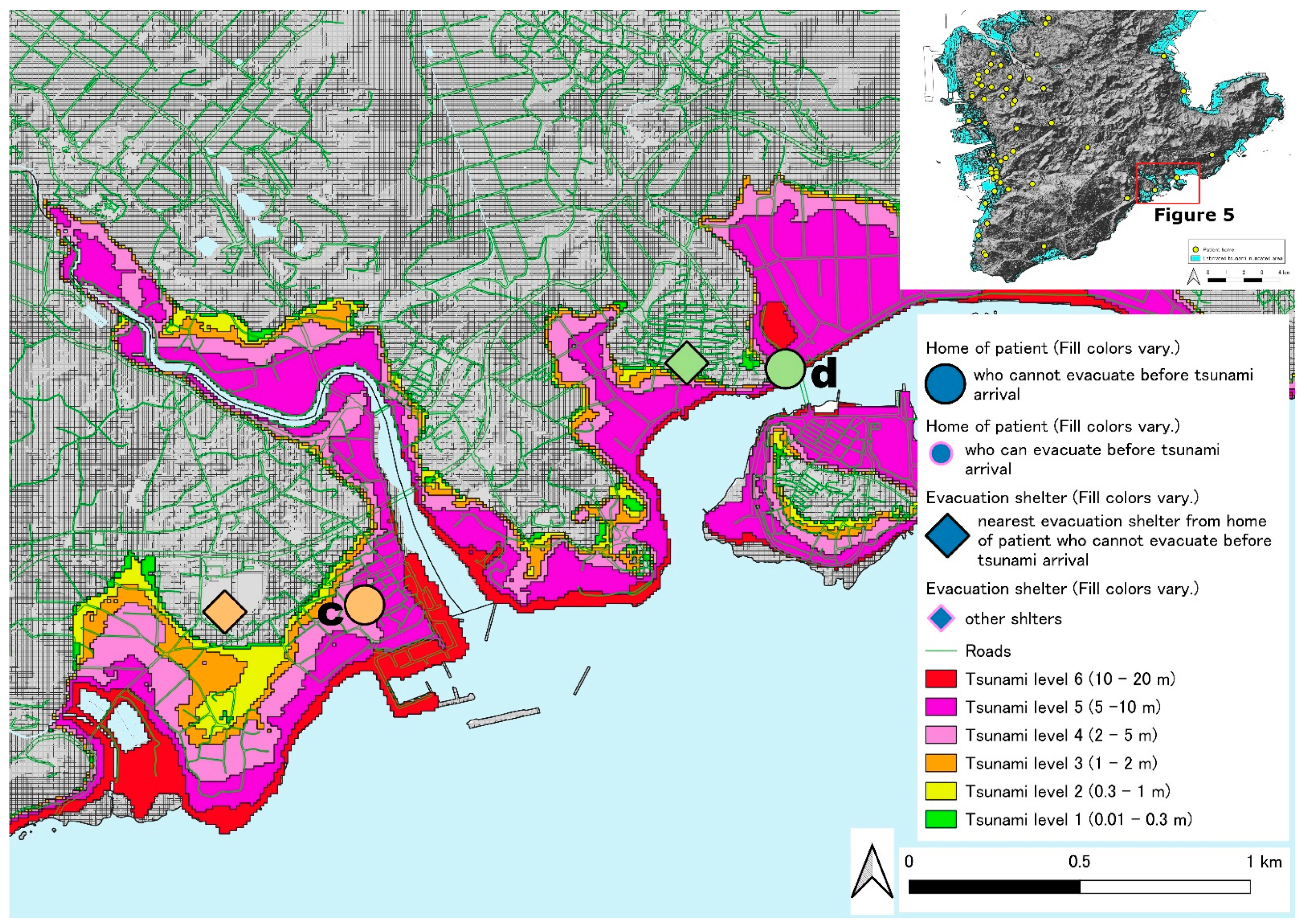
2.2. Target Area
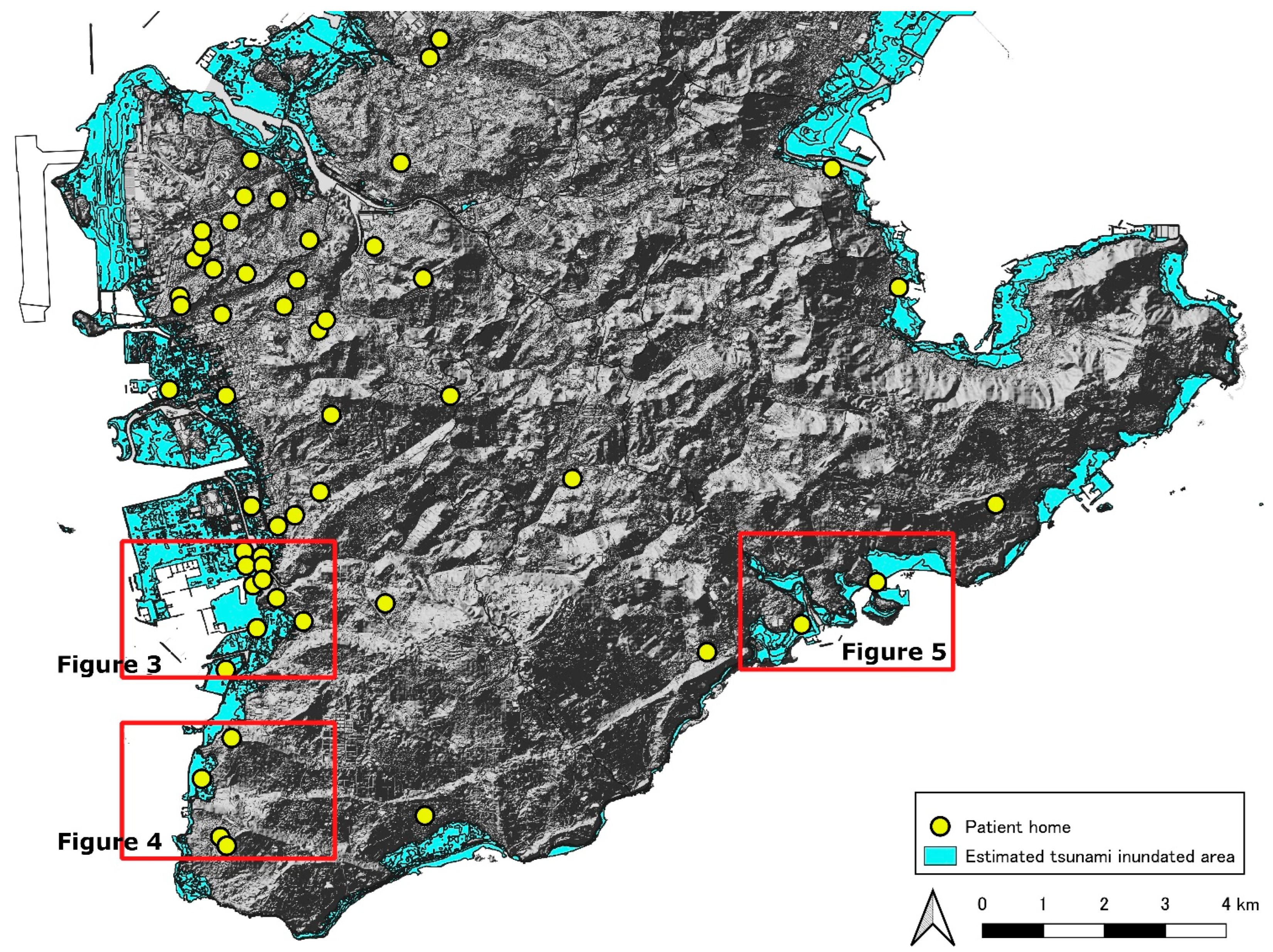
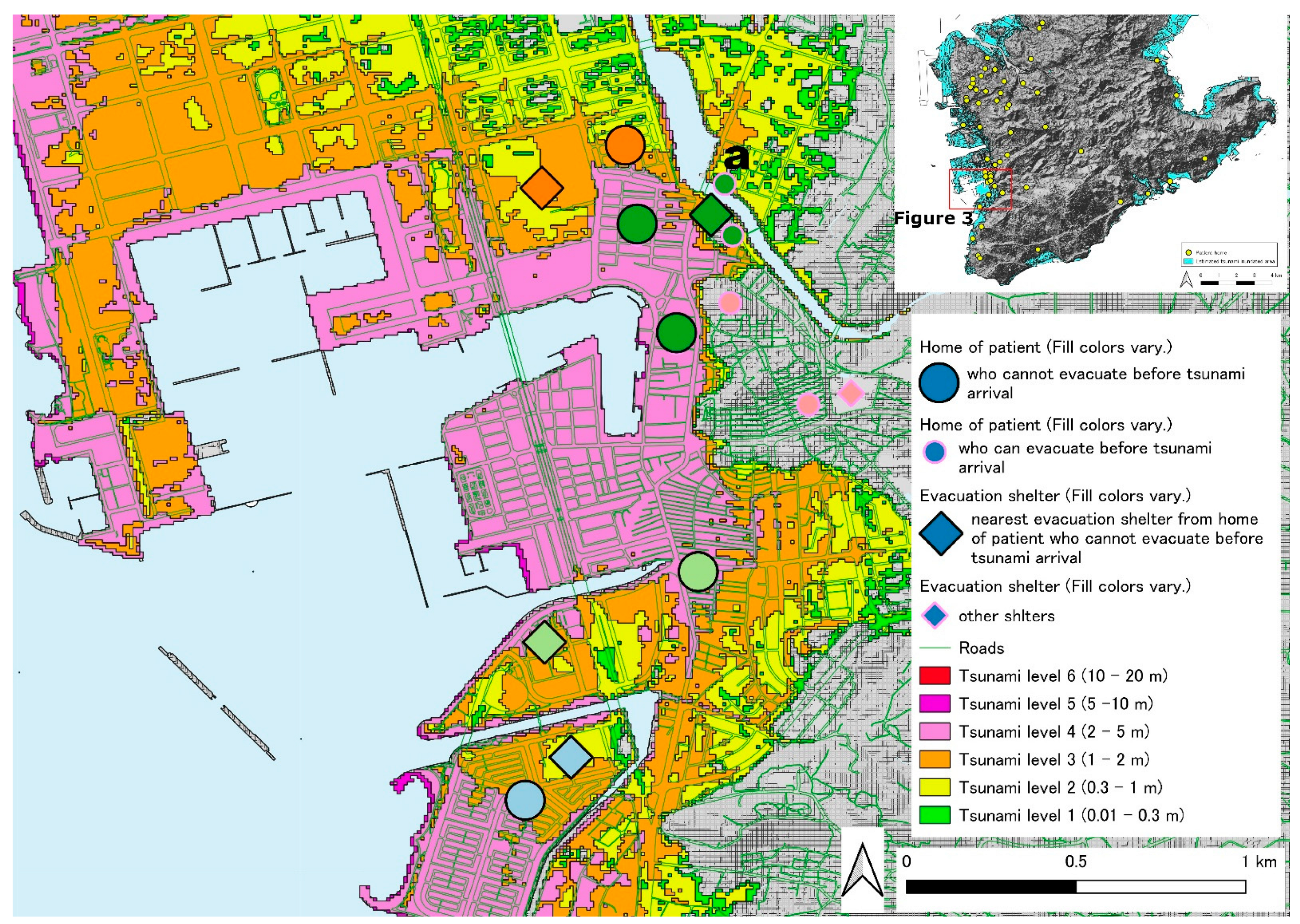
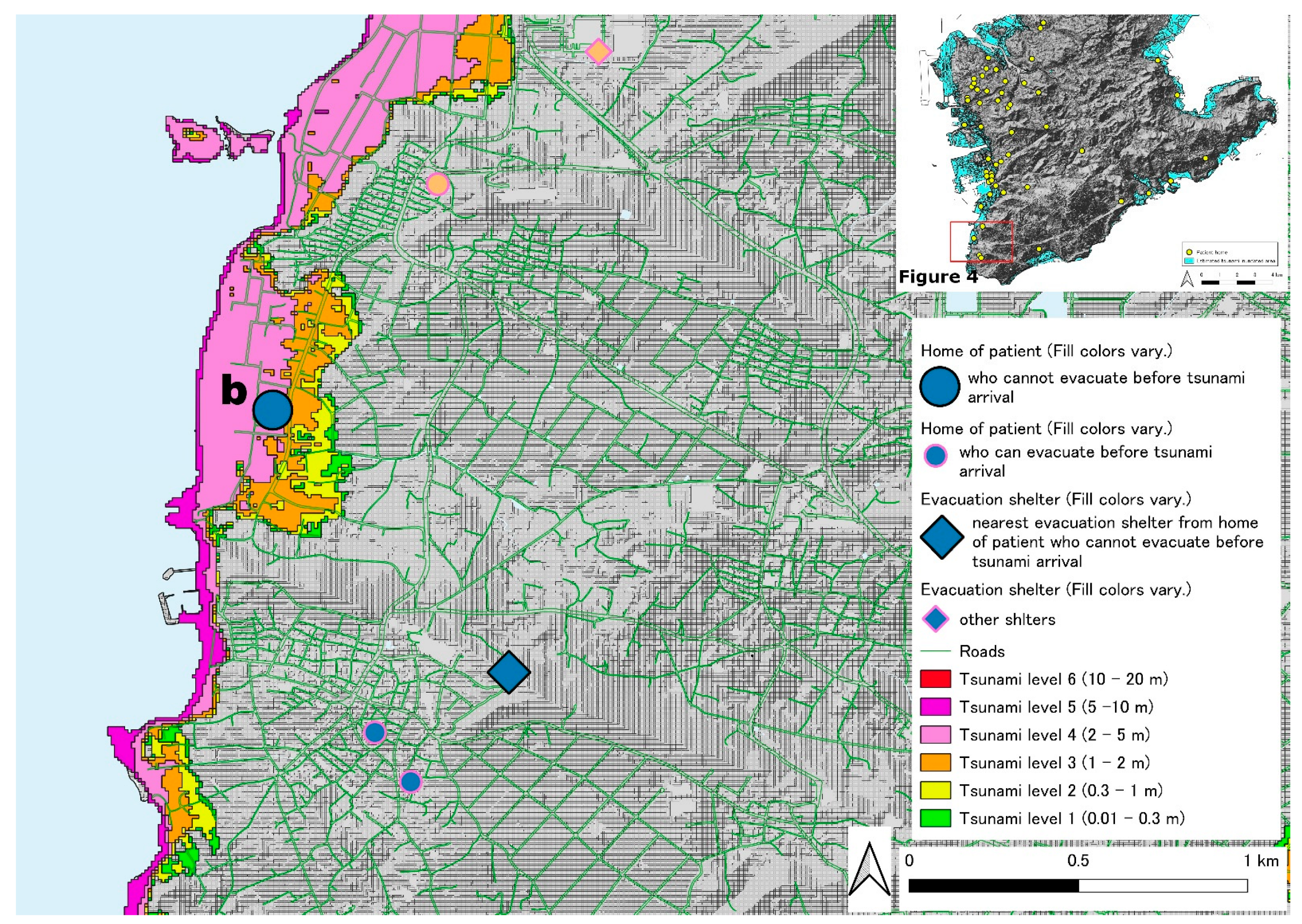
2.3. Mapping Locations of Chronic Respiratory Disease Patient and Tsunami Evacuation Area/Shelters
- Green area (0.01 m or more and less than 0.3 m): Although the tsunami has reached the area, no human or building damage is expected.
- Yellow area (0.3 m or more and less than 1.0 m): Evacuation behavior is not possible.
- Orange area (1.0 m or more and less than 2.0 m): Most people die when caught in a tsunami.
- Pink area (2.0 m or more and less than 5.0 m): 50% of wooden houses will be destroyed.
- Purple area (5.0 m or more and less than 10 m): A two-story building is submerged.
- Red area (10 m or more and less than 20 m): A three-story building is completely submerged.
2.4. Analysis of Data on Patients with Chronic Respiratory Disease
3. Results
3.1. Participant Characteristics
3.2. Data on Patients with Chronic Respiratory Diseases in Tsunami Inundation Areas
3.3. Locations of Patients with Chronic Respiratory Diseases
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Morrow, R.C.; Llewellyn, D.M. Tsunami overview. Mil. Med. 2006, 171 (Suppl. 1), 5–7. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nagata, S.; Teramoto, C.; Okamoto, R.; Koide, K.; Nishida, M.; Suzuki, R.; Nomura, M.; Tada, T.; Kishi, E.; Sakai, Y.; et al. The tsunami’s impact on mortality in a town severely damaged by the 2011 Great East Japan Earthquake. Disasters 2014, 38, S111–S122. [Google Scholar] [CrossRef] [PubMed]
- Mostafizi, A.; Wang, H.Z.; Cox, D.; Dong, S.J. An agent-based vertical evacuation model for a near-field tsunami: Choice behavior, logical shelter locations, and life safety. Int. J. Disaster Risk Reduct. 2019, 34, 467–479. [Google Scholar] [CrossRef]
- Shuto, N.; Fujima, K. A short history of tsunami research and countermeasures in Japan. Proc. Jpn. Acad. Ser. B Phys. Biol. Sci. 2009, 85, 267–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aydan, O.; Tokashiki, N. Tsunami boulders and their implications on the potential for a mega-earthquake along the Ryukyu Archipelago, Japan. Bull. Eng. Geol. Environ. 2019, 78, 3917–3925. [Google Scholar] [CrossRef]
- Okinawa Tsunami Inundation Assumption, Executive Office of the Governor, Disaster Prevention and Crisis Management Division, Okinawa. Available online: https://www.pref.okinawa.lg.jp/kaigannbousai/tsunami/oh_A_1.pdf (accessed on 6 April 2022).
- Suppasri, A.; Shuto, N.; Imamura, F.; Koshimura, S.; Mas, E.; Yalciner, A.C. Lessons learned from the 2011 great East Japan tsunami: Performance of tsunami countermeasures, coastal buildings, and tsunami evacuation in Japan. Pure Appl. Geophys. 2013, 170, 993–1018. [Google Scholar] [CrossRef] [Green Version]
- Fujiu, M.; Morisaki, Y.; Takayama, J.; Yanagihara, K.; Nishino, T.; Sagae, M.; Hirako, K. Evaluation of regional vulnerability to disasters by people of Ishikawa, Japan: A cross sectional study using national health insurance data. Int. J. Environ. Res. Public Health 2018, 15, 507. [Google Scholar] [CrossRef] [Green Version]
- Okinawa Prefecture Tsunami Evacuation Plan Formulation Guidelines, Executive Office of the Governor, Disaster Prevention and Crisis Management Division, Okinawa. Available online: https://www.pref.okinawa.jp/site/chijiko/bosai/kikikanri/documents/h25tsunamihinankeikaku-sakuteishishin.pdf (accessed on 6 April 2022).
- Crapo, R.O.; Casaburi, R.; Coates, A.L.; Enright, P.L.; MacIntyre, N.R.; McKay, R.T.; Johnson, D.; Wanger, J.S.; Zeballos, R.J.; Bittner, V.; et al. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar]
- Horiike, R.; Nakai, H.; Itatani, T.; Shirai, F.; Konishi, K. Using GIS to simulate tsunami evacuation guidance signs for the hearing impaired. PLoS ONE 2019, 14, e0217512. [Google Scholar] [CrossRef] [Green Version]
- Hinan_Okinawa, Executive Office of the Governor, Disaster Prevention and Crisis Management Division, Okinawa. Available online: https://www.kokuminhogo.go.jp/pdf/hinan_okinawa.pdf (accessed on 6 April 2022).
- Wood, N.; Jones, J.; Schelling, J.; Schmidtlein, M. Tsunami vertical-evacuation planning in the U.S. Pacific Northwest as a geospatial, multi-criteria decision problem. Int. J. Disaster Risk Reduc. 2014, 9, 68–83. [Google Scholar] [CrossRef] [Green Version]
- Takabatake, T.; Fujisawa, K.; Esteban, M.; Shibayama, T. Simulated effectiveness of a car evacuation from a tsunami. Int. J. Disaster Risk Reduct. 2020, 47, 101532. [Google Scholar] [CrossRef]
- Bernard, E.N. Tsunami preparedness: Is zero casualties possible? Pure Appl. Geophys. 2022, 1–14. [Google Scholar] [CrossRef]
- Ritz, R.H.; Previtera, J.E. Oxygen supplies during a mass casualty situation. Respir. Care 2008, 53, 215–224. [Google Scholar]
- Kobayashi, S.; Hanagama, M.; Yamanda, S.; Satoh, H.; Tokuda, S.; Kobayashi, M.; Ueda, S.; Suzuki, S.; Yanai, M. Impact of a large-scale natural disaster on patients with chronic obstructive pulmonary disease: The aftermath of the 2011 Great East Japan earthquake. Respir. Investig. 2013, 51, 17–23. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sato, K.; Morita, R.; Tsukamoto, K.; Sato, N.; Sasaki, Y.; Asano, M.; Okuda, Y.; Miura, H.; Sano, M.; Kosaka, T.; et al. Questionnaire survey on the continuity of home oxygen therapy after a disaster with power outages. Respir. Investig. 2013, 51, 9–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, S.; Hanagama, M.; Yamanda, S.; Yanai, M. Home oxygen therapy during natural disasters: Lessons from the great East Japan earthquake. Eur. Respir. J. 2012, 39, 1047–1048. [Google Scholar] [CrossRef] [PubMed]
- Kida, K.; Motegi, T.; Ishii, T.; Hattori, K. Long-term oxygen therapy in Japan: History, present status, and current problems. Pneumonol. Alergol. Pol. 2013, 81, 468–478. [Google Scholar]
- Di Mauro, M.; Megawati, K.; Cedillos, V.; Tucker, B. Tsunami risk reduction for densely populated Southeast Asian cities: Analysis of vehicular and pedestrian evacuation for the city of Padang, Indonesia, and assessment of interventions. Nat. Hazards 2013, 68, 373–404. [Google Scholar] [CrossRef] [Green Version]
- Hall, S.; Pettersson, J.; Meservy, W.; Harris, R.; Agustinawati, D.; Olson, J.; McFarlane, A. Awareness of tsunami natural warning signs and intended evacuation behaviors in Java, Indonesia. Nat. Hazards 2017, 89, 473–496. [Google Scholar] [CrossRef]
- Harnantyari, A.S.; Takabatake, T.; Esteban, M.; Valenzuela, P.; Nishida, Y.; Shibayama, T.; Achiari, H.; Rusli; Marzuki, A.G.; Marzuki, M.F.H.; et al. Tsunami awareness and evacuation behaviour during the 2018 Sulawesi Earthquake tsunami. Int. J. Disaster Risk Reduc. 2020, 43, 101389. [Google Scholar] [CrossRef]
- Foster, M.; Brice, J.H.; Shofer, F.; Principe, S.; Dewalt, D.; Falk, R.; Ferris, M. Personal disaster preparedness of dialysis patients in North Carolina. Clin. J. Am. Soc. Nephrol. 2011, 6, 2478–2484. [Google Scholar] [CrossRef] [PubMed]
- Hogaboom, N.S.; Oyster, M.L.; Riggins, M.S.; Boninger, M.L. Evacuation preparedness in full-time wheelchair users with spinal cord injury. J. Spinal Cord Med. 2013, 36, 290–295. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mace, S.E.; Doyle, C.J. Patients with access and functional needs in a disaster. South. Med. J. 2017, 110, 509–515. [Google Scholar]
- Nakai, H.; Itatani, T.; Kaganoi, S.; Okamura, A.; Horiike, R.; Yamasaki, M. Needs of children with neurodevelopmental disorders and geographic location of emergency shelters suitable for vulnerable people during a tsunami. Int. J. Environ. Res. Public Health 2021, 18, 1845. [Google Scholar] [CrossRef]
- Khorram-Manesh, A.; Yttermyr, J.; Sorensson, J.; Carlstrom, E. The impact of disasters and major incidents on vulnerable groups: Risk and medical assessment of Swedish patients with advanced care at home. Home Health Care Manag. Pract. 2017, 29, 183–190. [Google Scholar] [CrossRef]
- Uscher-Pines, L.; Hausman, A.J.; Powell, S.; Demara, P.; Heake, G.; Hagen, M.G. Disaster preparedness of households with special needs in Southeastern Pennsylvania. Am. J. Prev. Med. 2009, 37, 227–230. [Google Scholar] [CrossRef]
- Dall’Osso, F.; Dominey-Howes, D. Public assessment of the usefulness of “draft” tsunami evacuation maps from Sydney, Australia—Implications for the establishment of formal evacuation plans. Nat. Hazards Earth Syst. Sci. 2010, 10, 1739–1750. [Google Scholar] [CrossRef] [Green Version]
- Nakai, H.; Itatani, T.; Horiike, R.; Kyota, K.; Tsukasaki, K. Tsunami evacuation simulation using geographic information systems for homecare recipients depending on electric devices. PLoS ONE 2018, 13, e0199252. [Google Scholar] [CrossRef] [Green Version]
- Laberge, M.; Heykoop, C.; Camp, P.G. Personal disaster preparedness of people with chronic obstructive pulmonary disease: Development and validation of a self-report questionnaire. Can. J. Respir. Crit. Care Sleep Med. 2021, 5, 316–322. [Google Scholar] [CrossRef]
- Tanaka, Y.; Hotta, M.; Inuzuka, T. The preparations of patients with amyotrophic lateral sclerosis for disaster after the Great East Japan earthquake. J. Neurol. Sci. 2017, 379, 304–305. [Google Scholar] [CrossRef]
- Lind, J.D.; Fickel, J.; Cotner, B.A.; Katzburg, J.R.; Cowper-Ripley, D.; Fleming, M.; Ong, M.K.; Bergman, A.A.; Bradley, S.E.; Tubbesing, S.A. Implementing Geographic Information Systems (GIS) into VHA home based primary care. Geriatr. Nurs. 2020, 41, 282–289. [Google Scholar] [CrossRef] [PubMed]
- Tomio, J.; Sato, H. Emergency and disaster preparedness for chronically ill patients: A review of recommendations. Open Access Emerg. Med. 2014, 6, 69–79. [Google Scholar] [PubMed] [Green Version]
- Gregg, C.E.; Houghton, B.F.; Paton, D.; Johnston, D.M.; Swanson, D.A.; Yanagi, B.S. Tsunami warnings: Understanding in Hawai’i. Nat. Hazards 2007, 40, 71–87. [Google Scholar] [CrossRef]
- Makinoshima, F.; Oishi, Y.; Nakagawa, M.; Sato, S.; Imamura, F. Revealing complex tsunami evacuation process patterns induced by social interactions: A case study in Ishinomaki. Int. J. Disaster Risk Reduc. 2021, 58, 102182. [Google Scholar] [CrossRef]
- Wei, H.L.; Wu, H.C.; Lindell, M.K.; Prater, C.S.; Shiroshita, H.; Johnston, D.M.; Becker, J.S. Assessment of households’ responses to the tsunami threat: A comparative study of Japan and New Zealand. Int. J. Disaster Risk Reduc. 2017, 25, 274–282. [Google Scholar] [CrossRef]
| Item | Category | Number |
|---|---|---|
| Age | Average ± standard deviation | 71.4 ± 15.7 (year) |
| Gender | Male | 40 |
| Female | 15 | |
| Nearest shelter | Average ± standard deviation | 428 ± 269 |
| Median | 400 | |
| 6 min walk test | Average ± standard deviation | 97 ± 131 |
| Median | 50 | |
| Types of HOT | Liquid Oxygen | 24 |
| Oxygen concentrator | 31 | |
| Oxygen flow on rest | Average ± standard deviation | 1.38 ± 0.9 |
| Median | 1 | |
| Oxygen flow on exercise | Average ± standard deviation | 2.42 ± 1.36 |
| Median | 2 |
| Number | Age | Gender | Diagnosis | Tsunami ID (m) | Ws (m/min) | Tsunami First Wave Rt (min) | Ed (m) | Distance to Shelter (m) | Survival (1-0) |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 57 | M | IP | 0.3–1.0 | 40 | 23 | 920 | 450 | 1 |
| 2 | 83 | M | BE | 2.0–5.0 | 43 | 19 | 817 | 350 | 1 |
| 3 | 67 | F | IP | 1.0–2.0 | 92 | 15 | 1380 | 400 | 1 |
| 4 | 27 | M | PAH | 2.0–5.0 | 8 | 15 | 120 | 450 | 0 |
| 5 | 75 | F | BE | 2.0–5.0 | 7 | 22 | 154 | 7 | 1 |
| 6 | 65 | M | IP | 0.01–0.3 | 13 | 19 | 247 | 1000 | 1 |
| 7 | 88 | F | COPD | 0.01–0.3 | 17 | 22 | 374 | 500 | 1 |
| 8 | 73 | F | IP | 0.3–1.0 | 0 | 21 | 0 | 400 | 1 |
| 9 | 85 | M | COPD | 2.0–5.0 | 2 | 15 | 30 | 550 | 0 |
| 10 | 83 | M | COPD | 0.3–1.0 | 17 | 10 | 170 | 1100 | 1 |
| 11 | 63 | M | COPD | 5.0–10.0 | 0 | 6 | 0 | 400 | 0 |
| 12 | 85 | F | BE | 2.0–5.0 | 2 | 10 | 20 | 1200 | 0 |
| 13 | 74 | M | IP | 2.0–5.0 | 2.5 | 15 | 38 | 270 | 0 |
| 14 | 68 | M | COPD | 10.0–20.0 | 7 | 7 | 49 | 400 | 0 |
| 15 | 91 | M | CPFE | 1.0–2.0 | 5 | 15 | 75 | 66 | 1 |
| 16 | 27 | F | SGS | 0.01–0.3 | 5 | 15 | 75 | 230 | 1 |
| 17 | 32 | M | SGS | 0.01–0.3 | 7 | 15 | 75 | 230 | 1 |
| 18 | 71 | M | PTS | 0.01–0.3 | 2 | 22 | 44 | 300 | 1 |
| 19 | 51 | M | CPFE | 2.0–5.0 | 17 | 15 | 255 | 550 | 0 |
| 20 | 85 | M | COPD | 2.0–5.0 | 8 | 15 | 120 | 300 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sekiguchi, H.; Takeuchi, R.; Sato, Y.; Matsumoto, T.; Kobayashi, J.; Umemura, T. Can Homecare Chronic Respiratory Disease Patients with Home Oxygen Treatment (HOT) in Southern Okinawa, Japan Be Evacuated Ahead of the Next Anticipated Tsunami? Int. J. Environ. Res. Public Health 2022, 19, 5647. https://doi.org/10.3390/ijerph19095647
Sekiguchi H, Takeuchi R, Sato Y, Matsumoto T, Kobayashi J, Umemura T. Can Homecare Chronic Respiratory Disease Patients with Home Oxygen Treatment (HOT) in Southern Okinawa, Japan Be Evacuated Ahead of the Next Anticipated Tsunami? International Journal of Environmental Research and Public Health. 2022; 19(9):5647. https://doi.org/10.3390/ijerph19095647
Chicago/Turabian StyleSekiguchi, Hiroshi, Rie Takeuchi, Yoko Sato, Tsuyoshi Matsumoto, Jun Kobayashi, and Takehiro Umemura. 2022. "Can Homecare Chronic Respiratory Disease Patients with Home Oxygen Treatment (HOT) in Southern Okinawa, Japan Be Evacuated Ahead of the Next Anticipated Tsunami?" International Journal of Environmental Research and Public Health 19, no. 9: 5647. https://doi.org/10.3390/ijerph19095647
APA StyleSekiguchi, H., Takeuchi, R., Sato, Y., Matsumoto, T., Kobayashi, J., & Umemura, T. (2022). Can Homecare Chronic Respiratory Disease Patients with Home Oxygen Treatment (HOT) in Southern Okinawa, Japan Be Evacuated Ahead of the Next Anticipated Tsunami? International Journal of Environmental Research and Public Health, 19(9), 5647. https://doi.org/10.3390/ijerph19095647






