Telemedicine and Haemodialysis Care during the COVID-19 Pandemic: An Integrative Review of Patient Safety, Healthcare Quality, Ethics and the Legal Considerations in Singapore Practice
Abstract
:1. Introduction
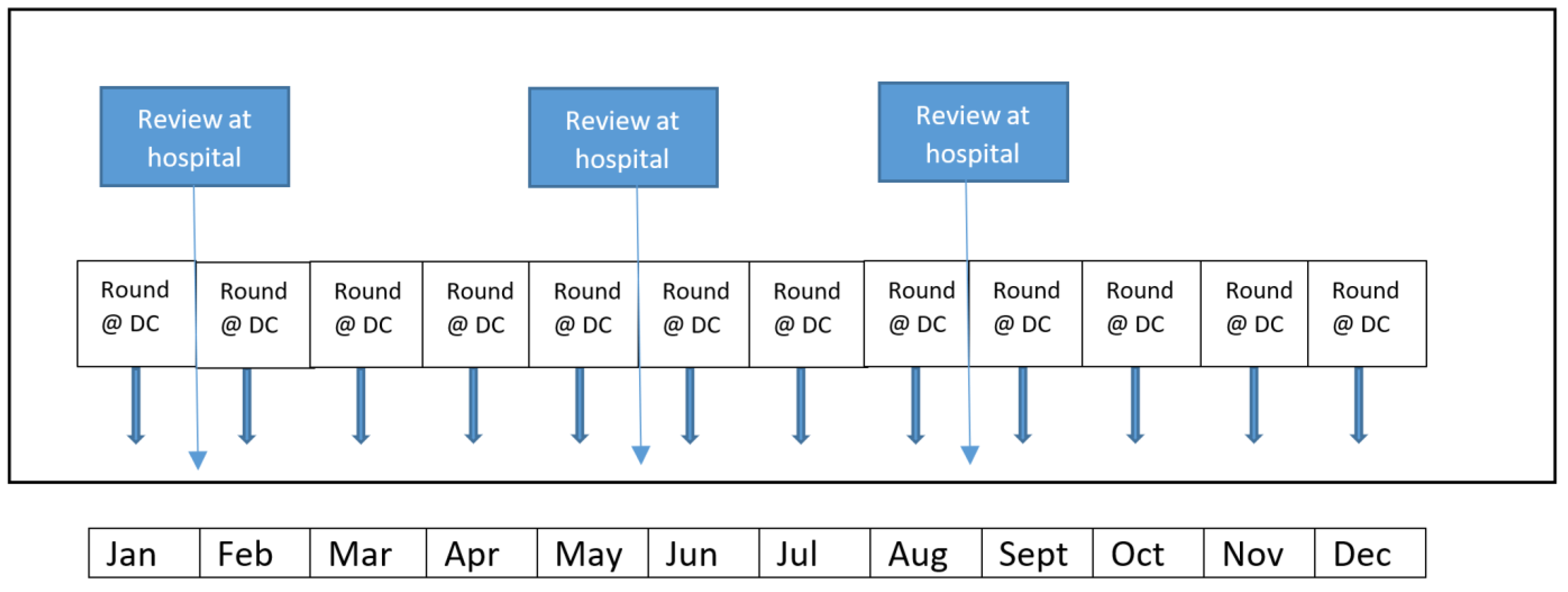
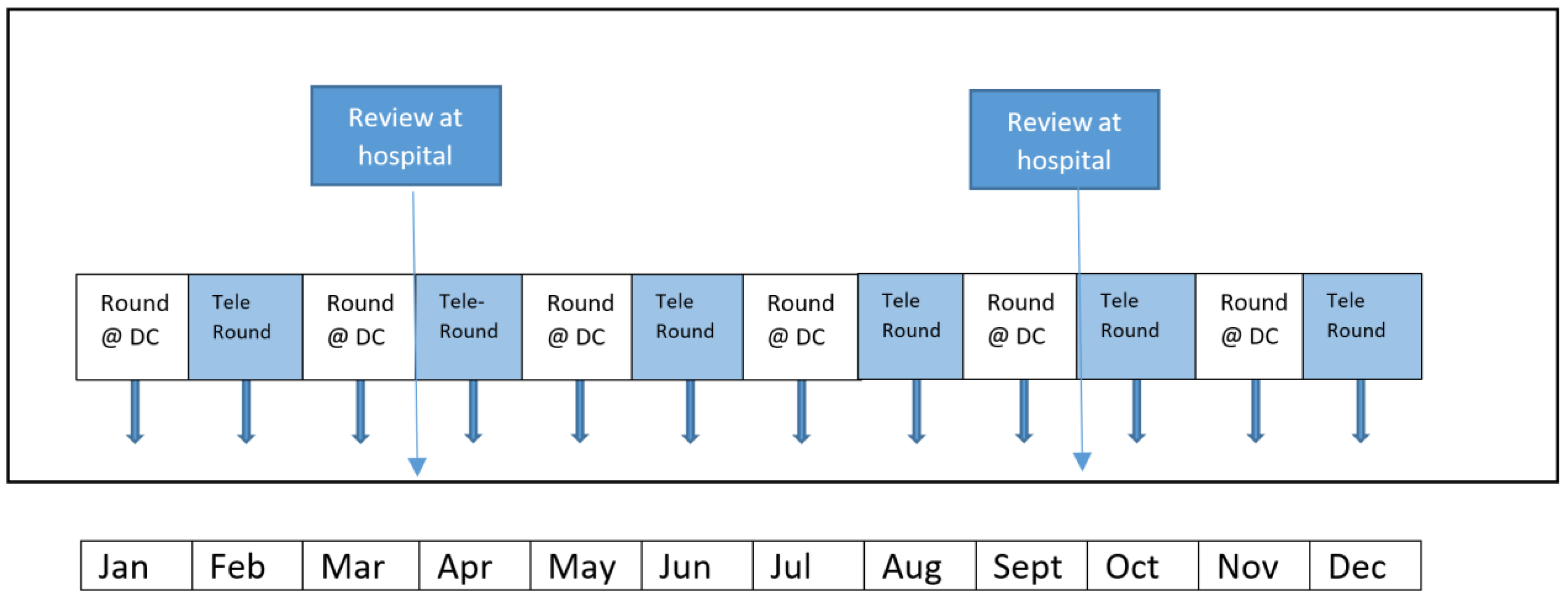
2. Management of ICHD Patients
3. Conduct of Dialysis Review via Telemedicine
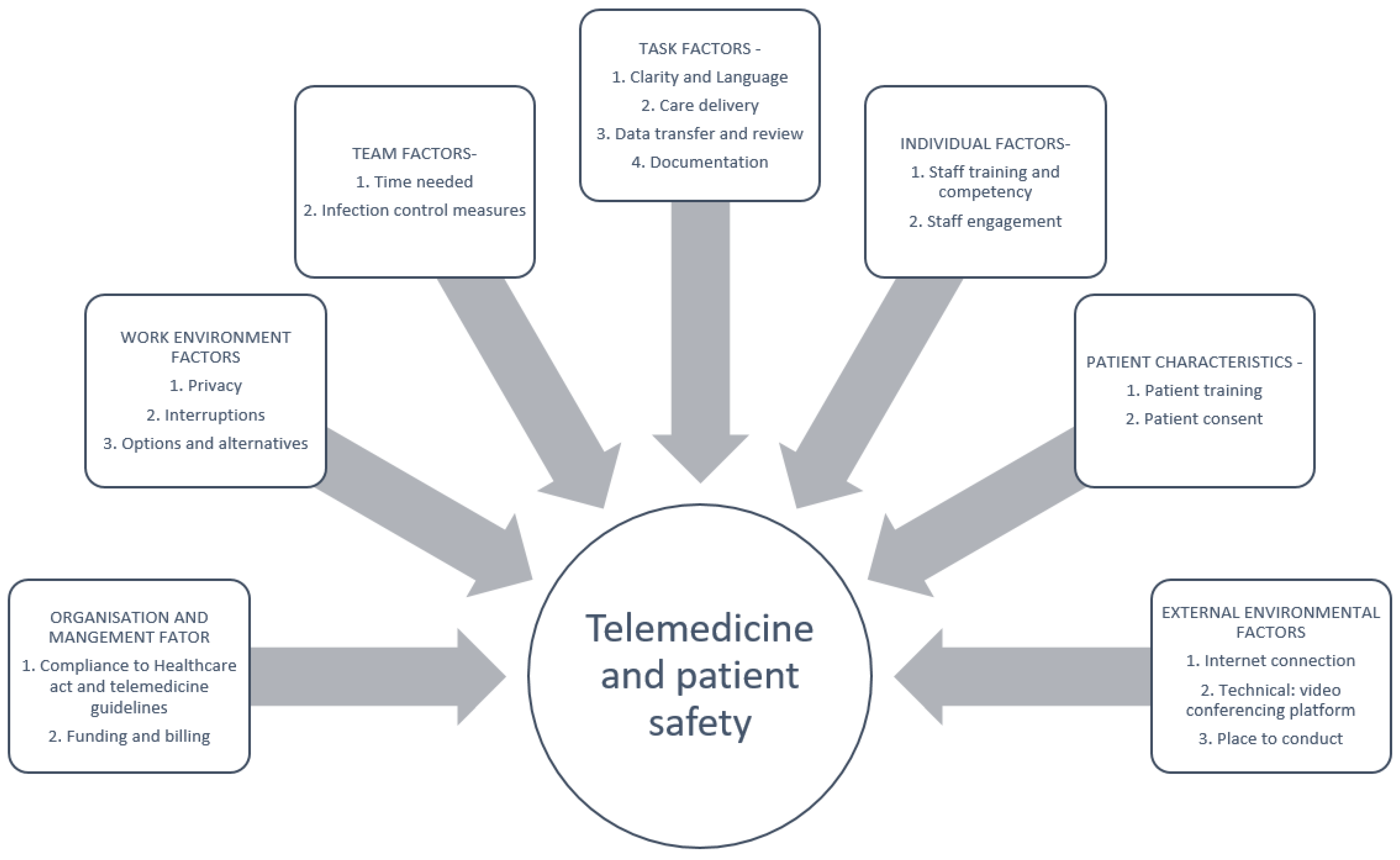
4. Ensuring Patient Safety and Maintaining Care Quality
5. Ethical Considerations and Justifications
6. Regulatory and Legal Requirements
7. Cybersecurity and Data Privacy
8. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Tuckson, R.V.; Edmunds, M.; Hodgkins, M.L. Telehealth. N. Engl. J. Med. 2017, 377, 1585–1592. [Google Scholar] [CrossRef] [PubMed]
- Institute of Medicine (US) Committee on Evaluating Clinical Applications of Telemedicine; Field, M.J. (Eds.) Telemedicine: A Guide to Assessing Telecommunications in Health Care; National Academies Press: Washington, DC, USA, 1996. [Google Scholar]
- Dunn, E.V.; Conrath, D.W.; Bloor, W.G.; Tranquada, B. An evaluation of four telemedicine systems for primary care. Health Serv. Res. 1977, 12, 19–29. [Google Scholar] [PubMed]
- Bradford, N.K.; Caffery, L.J.; Smith, A.C. Telehealth services in rural and remote Australia: A systematic review of models of care and factors influencing success and sustainability. Rural Remote Health 2016, 16, 3808. [Google Scholar] [PubMed]
- Johnston, R.; Staveley, R.; Olfert, L.A.; Jennett, P. An industry, clinical, and academic telehealth partnership venture: Progress, goals achieved, and lessons learned. Telemed. J. e-Health 2000, 6, 341–348. [Google Scholar] [CrossRef]
- Flodgren, G.; Rachas, A.; Farmer, A.J.; Inzitari, M.; Shepperd, S. Interactive telemedicine: Effects on professional practice and health care outcomes. Cochrane Database Syst. Rev. 2015, 9, CD002098. [Google Scholar] [CrossRef]
- Boxer, R.J.; Ellimoottil, C. Advantages and utilization of telemedicine. mHealth 2019, 5, 12. [Google Scholar] [CrossRef]
- Taylor, K. How Digital Technology Is Transforming Health and Social Care; Deloitte Centre for Health Solutions: London, UK, 2015. [Google Scholar]
- Nittari, G.; Savva, D.; Tomassoni, D.; Tayebati, S.K.; Amenta, F. Telemedicine in the COVID-19 Era: A Narrative Review Based on Current Evidence. Int. J. Environ. Res. Public Health 2022, 19, 5101. [Google Scholar] [CrossRef]
- Lurie, N.; Carr, B.G. The Role of Telehealth in the Medical Response to Disasters. JAMA Intern. Med. 2018, 178, 745–746. [Google Scholar] [CrossRef]
- Simmons, S.; Alverson, D.; Poropatich, R.; D’Iorio, J.; DeVany, M.; Doarn, C.R. Applying telehealth in natural and anthropogenic disasters. Telemed. J. e-Health 2008, 14, 968–971. [Google Scholar] [CrossRef]
- Smith, A.C.; Thomas, E.; Snoswell, C.L.; Haydon, H.; Mehrotra, A.; Clemensen, J.; Caffery, L.J. Telehealth for global emergencies: Implications for coronavirus disease 2019 (COVID-19). J. Telemed. Telecare 2020, 26, 309–313. [Google Scholar] [CrossRef] [Green Version]
- Hincapié, M.A.; Gallego, J.C.; Gempeler, A.; Piñeros, J.A.; Nasner, D.; Escobar, M.F. Implementation and Usefulness of Telemedicine During the COVID-19 Pandemic: A Scoping Review. J. Prim. Care Community Health 2020, 11, 2150132720980612. [Google Scholar] [CrossRef] [PubMed]
- Colbert, G.B.; Venegas-Vera, A.V.; Lerma, E.V. Utility of telemedicine in the COVID-19 era. Rev. Cardiovasc. Med. 2020, 21, 583–587. [Google Scholar] [PubMed]
- Michel, J.; Mettler, A.; Müller, M.; Hautz, W.E.; Sauter, T.C. A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study. Int. J. Environ. Res. Public Health 2022, 19, 5184. [Google Scholar] [CrossRef]
- Lai, S.H.S.; Tang, C.Q.Y. Telemedicine and COVID-19: Beyond just virtual consultations—The Singapore experience. Bone Jt. Open 2020, 1, 203–204. [Google Scholar] [CrossRef]
- Zhang, J.; Chua, Q.H.A.; Shen, X.M.; Viseikumaran, J.A.; Teoh, T.; Tan, N.G. A Systematic Implementation of Telemedicine in Singapore’s COVID-19 Community Recovery Facilities. Telemed. J. e-Health, 2022; in press. [Google Scholar] [CrossRef] [PubMed]
- Chia, M.L.; Him Chau, D.H.; Lim, K.S.; Yang Liu, C.W.; Tan, H.K.; Tan, Y.R. Managing COVID-19 in a Novel, Rapidly Deployable Community Isolation Quarantine Facility. Ann. Intern. Med. 2021, 174, 247–251. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health Singapore. Vaccination Statistics. Available online: https://www.moh.gov.sg/covid-19/vaccination/statistics (accessed on 21 April 2022).
- Ministry of Health Continuation of Essential Healthcare Services during Period of Heightened Safe Distancing Measures. Available online: https://www.moh.gov.sg/news-highlights/details/continuation-of-essential-healthcare-services-during-period-of-heightened-safe-distancing-measures (accessed on 8 March 2022).
- Ministry of Health Annex A: Examples of Essential and Non-Essential Services. Available online: https://www.moh.gov.sg/docs/librariesprovider5/pressroom/press-releases/annex-a3685da33172d4ed08bb310ec24a440f8.pdf (accessed on 8 March 2022).
- Singapore Renal Registry Annual Report. National Registry of Disease Office. Available online: https://www.nrdo.gov.sg/docs/librariesprovider3/default-document-library/srr-annual-report-2020.pdf?sfvrsn=658dd717_0 (accessed on 21 April 2022).
- Singapore, M.O.H. Guidelines for Private Healthcare Institutions Providing Renal Dialysis: Regulation 4 of the Private Hospitals or Medical Clinics Regulations [CAP 248, Rg 1]. 2001. Available online: https://www.moh.gov.sg/docs/librariesprovider5/licensing-terms-and-conditions/guidelines-for-private-healthcare-institutions-providing-renal-dialysis.pdf (accessed on 3 March 2022).
- Lew, S.Q.; Sikka, N. Operationalizing Telehealth for Home Dialysis Patients in the United States. Am. J. Kidney Dis. 2019, 74, 95–100. [Google Scholar] [CrossRef]
- Lew, S.Q. Telehealth in Peritoneal Dialysis: Review of Patient Management. Adv. Perit. Dial. 2018, 34, 32–37. [Google Scholar]
- Singapore, M.O.H. National Telemedicine Guidelines. 2015. Available online: https://www.moh.gov.sg/docs/librariesprovider5/licensing-terms-and-conditions/national-telemedicine-guidelines-for-singapore-(dated-30-jan-2015).pdf (accessed on 3 March 2022).
- Staines, A.; Amalberti, R.; Berwick, D.M.; Braithwaite, J.; Lachman, P.; Vincent, C.A. COVID-19: Patient safety and quality improvement skills to deploy during the surge. Int. J. Qual. Health Care 2021, 33, mzaa050. [Google Scholar] [CrossRef]
- Patient Safety Network. Telehealth and Patient Safety during the COVID-19 Response. 2020. Available online: https://www.psnet.ahrq.gov/perspective/telehealth-and-patient-safety-during-covid-19-response (accessed on 21 April 2022).
- Emanuel, L.; Berwick, D.; Conway, J.; Combes, J.; Hatlie, M.; Leape, L.; Reason, J.; Schyve, P.; Vincent, C.; Walton, M. What Exactly Is Patient Safety? In Advances in Patient Safety: New Directions and Alternative Approaches; Henriksen, K., Battles, J.B., Keyes, M.A., Grady, M.L., Eds.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. Available online: https://www.ncbi.nlm.nih.gov/books/NBK43629/ (accessed on 21 April 2022).
- Vincent, C. Patient Safety; Elsevier: London, UK, 2006. [Google Scholar]
- Agarwal, A.K.; Sequeira, A.; Oza-Gajera, B.P.; Ramani, K.; Packer, J.; Litchfield, T.; Nations, M.L.; Lerma, E.V. Lessons learnt and future directions in managing dialysis access during the COVID 19 pandemic: Patient and provider experience in the United States. J. Vasc. Access, 2021; in press. [Google Scholar] [CrossRef]
- Lok, C.E.; Huber, T.S.; Lee, T.; Shenoy, S.; Yevzlin, A.S.; Abreo, K.; Allon, M.; Asif, A.; Astor, B.C.; Glickman, M.H.; et al. National Kidney Foundation. KDOQI Clinical Practice Guideline for Vascular Access: 2019 Update. Am. J. Kidney Dis. 2020, 75 (Suppl. S2), S1–S164. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haroon, S.; Lau, T.; Tan, G.L.; Davenport, A. Telemedicine in the Satellite Dialysis Unit: Is It Feasible and Safe? Front. Med. 2021, 8, 634203. [Google Scholar] [CrossRef] [PubMed]
- Fleming, R.; Gartner, D.; Padman, R.; James, D. An Analytical Approach for Improving Patient-centric Delivery of Dialysis Services. AMIA Annu. Symp. Proc. 2019, 2019, 418–427. [Google Scholar] [PubMed]
- Singh, T.; Ngoh, C.L.; Wong, K.; Khan, B.A. Impact of Telemedicine on Hospitalisation and Mortality Rates in Community-Based Haemodialysis Centres in Singapore during the COVID-19 Pandemic. Ann. Acad. Med. Singap. 2020, 49, 756–763. [Google Scholar] [CrossRef] [PubMed]
- Taylor, M.J.; McNicholas, C.; Nicolay, C.; Darzi, A.; Bell, D.; Reed, J.E. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual. Saf. 2014, 23, 290–298. [Google Scholar] [CrossRef] [PubMed]
- Pham, J.C.; Hoffman, C.; Popescu, I.; Ijagbemi, O.M.; Carson, K.A. A Tool for the Concise Analysis of Patient Safety Incidents. Jt. Comm. J. Qual. Patient Saf. 2016, 42, 26–33. [Google Scholar] [CrossRef]
- Telehealth Consultant Satisfaction Survey. Available online: https://digital.ahrq.gov/sites/default/files/docs/survey/telehealthconsultantsatisfactionsurvey_comp.pdf (accessed on 3 March 2022).
- Utah Telehealth Network. Telehealth Patient Satisfaction Survey. Available online: https://digital.ahrq.gov/sites/default/files/docs/survey/telehealthpatientsatisfactionsurvey_comp.pdf (accessed on 3 March 2022).
- Kawaguchi, T.; Karaboyas, A.; Robinson, B.M.; Li, Y.; Fukuhara, S.; Bieber, B.A.; Rayner, H.C.; Andreucci, V.E.; Pisoni, R.L.; Port, F.K.; et al. Associations of frequency and duration of patient-doctor contact in hemodialysis facilities with mortality. J. Am. Soc. Nephrol. 2013, 24, 1493–1502. [Google Scholar] [CrossRef] [Green Version]
- Singapore Medical Council. Ethical Code and Ethical Guidelines. 2016 Edition. Available online: https://www.healthprofessionals.gov.sg/docs/librariesprovider2/guidelines/2016-smc-ethical-code-and-ethical-guidelines---(13sep16).pdf (accessed on 8 March 2022).
- Goldstein, B.D. The precautionary principle also applies to public health actions. Am. J. Public Health 2001, 91, 1358–1361. [Google Scholar] [CrossRef]
- Fins, J.J.; Miller, F.G. Proportionality, pandemics, and medical ethics. Am. J. Med. 2020, 133, 1243–1244. [Google Scholar] [CrossRef]
- Low, J.; Dujacquier, D.; Kaur, S. Roland Berger Report: Bridging the Digital Divide/Improving Digital Inclusion in Southeast Asia. Available online: https://www.rolandberger.com/en/Insights/Publications/Bridging-the-digital-divide.html (accessed on 14 April 2022).
- International Trade Commission. Singapore—Information and Telecommunications Technology. Available online: https://www.trade.gov/country-commercial-guides/singapore-information-and-telecommunications-technology (accessed on 4 April 2022).
- Ladin, K.; Porteny, T.; Perugini, J.M.; Gonzales, K.M.; Aufort, K.E.; Levine, S.K.; Wong, J.B.; Isakova, T.; Rifkin, D.; Gordon, E.J.; et al. Perceptions of telehealth vs in-person visits among older adults with advanced kidney disease, care partners, and clinicians. JAMA Netw. Open 2021, 4, e2137193. [Google Scholar] [CrossRef]
- Stauss, M.; Floyd, L.; Becker, S.; Ponnusamy, A.; Woywodt, A. Opportunities in the cloud or pie in the sky? Current status and future perspectives of telemedicine in nephrology. Clin. Kidney J. 2021, 14, 492–506. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, S.; Bradley, S.; Chattu, V.K.; Adisesh, A.; Nurtazina, A.; Kyrykbayeva, S.; Sakhamuri, S.; Yaya, S.; Sunil, T.; Thomas, P.; et al. Telemedicine Across the Globe-Position Paper From the COVID-19 Pandemic Health System Resilience PROGRAM (REPROGRAM) International Consortium (Part 1). Front. Public Health 2020, 8, 556720. [Google Scholar] [CrossRef] [PubMed]
- Healthcare Services Act (HCSA). 2020. Available online: https://www.moh.gov.sg/hcsa/home (accessed on 8 March 2022).
- Prabakaran, P. The Medico-Legal Dilemmas of the Regulation of Telemedicine and AI in Singapore’s Healthcare Context. Available online: https://lawtech.asia/the-medico-legal-dilemmas-of-the-regulation-of-telemedicine-and-ai-in-singapores-healthcare-context/ (accessed on 8 March 2022).
- Regulatory Guideline for Telehealth Products. 2019. Available online: https://www.hsa.gov.sg/docs/default-source/hprg-mdb/regulatory-guidelines-for-telehealth-products-rev-2-1.pdf (accessed on 8 March 2022).
- Artificial Intelligence in Healthcare Guidelines (AIHGle). 2021. Available online: https://www.moh.gov.sg/docs/librariesprovider5/eguides/1-0-artificial-in-healthcare-guidelines-(aihgle)_publishedoct21.pdf (accessed on 8 March 2022).
- Guidelines for Telepharmacy 2009. Available online: https://www.pss.org.sg/sites/default/files/Guidelines/guidelines_for_telepharmacy.pdf (accessed on 8 March 2022).
- Health Products (Licensing of Retail Pharmacies) Regulations 2016. Available online: https://sso.agc.gov.sg/SL/HPA2007-S330-2016 (accessed on 8 March 2022).
- World Health Organization. Implementing Telemedicine Services during COVID-19: Guiding Principles and Considerations for a Stepwise Approach. 2021. Available online: https://www.who.int/publications/i/item/WPR-DSE-2020-032 (accessed on 19 April 2022).
- Medical Registration Act 1997, s53(d). Available online: https://sso.agc.gov.sg/Act/MRA1997?ProvIds=P17-#pr53- (accessed on 8 March 2022).
- Koh, E.Y.; Mak, W.M.; Tee, C.; Tham, H.H. COVID-19 and Issues Facing the Healthcare Community: How Can Telemedicine Help? Allen & Gledhill, 23 April 2020. [Google Scholar]
- Leveraging on Telemedicine during an Infectious Disease Outbreak. 2020. Available online: https://www.sma.org.sg/UploadedImg/files/ncov2019/LeveragingTelemedicineInfectiousDiseaseOutbreak20200212.pdf (accessed on 8 March 2022).
- Bolam v Friern Hospital Management Committee [1957] 1 WLR 582.
- Bolitho v City and Hackney Health Authority [1998] AC 232.
- Dr Khoo James & Anor v Gunapathy d/o Muniandy [2002] 2 SLR 414.
- Price, W.N., II. Artificial Intelligence in Health Care: Applications and Legal Implications. SciTech Lawyer 2017, 14, 10–13. [Google Scholar]
- Hii Chii Kok v Ooi Peng Jin London Lucien and Anor [2017] 2 SLR 492.
- Civil Law (Amendment) Bill (No. 33/2020), s37. Available online: https://sso.agc.gov.sg/Bills-Supp/33-2020/Published/20200903?DocDate=20200903 (accessed on 8 March 2022).
- Leite, H.; Hodgkinson, I.R.; Gruber, T. New Development: ‘Healing at a Distance’—Telemedicine and COVID-19. Public Money Manag. 2020, 40, 483–485. [Google Scholar] [CrossRef] [Green Version]
- U.S. Department of Health & Human Services. Notification of Enforcement Discretion for Telehealth Remote Communications during the COVID-19 Nationwide Public Health Emergency. 2021. Available online: https://www.hhs.gov/hipaa/for-professionals/special-topics/emergency-preparedness/notification-enforcement-discretion-telehealth/index.html (accessed on 19 April 2022).
- Personal Data Protection Act 2012, ss2, 13 and 24. Available online: https://sso.agc.gov.sg/Act/PDPA2012? (accessed on 8 March 2022).
- Wong, B. COVID-19 Response Measures and Data Protection Law in Singapore. Available online: https://nus-covaid.com/academics-on-pandemics/covid-19-response-measures-and-data-protection-law-in-singapore-by-benjamin-wong (accessed on 19 April 2022).
- Personal Data Protection Commission, Singapore. Advisories on Collection of Personal Data for COVID-19 Contact Tracing and Use of SafeEntry. 2022. Available online: https://www.pdpc.gov.sg/Help-and-Resources/2021/05/Advisory-on-Collection-of-Personal-Data-for-COVID-19-Contact-Tracing (accessed on 19 April 2022).
- Singapore Health Services Pte. Ltd. & Ors, SGPDPC 3. 2019. Available online: https://www.pdpc.gov.sg/-/media/Files/PDPC/PDF-Files/Commissions-Decisions/Grounds-of-Decision---SingHealth-IHiS---150119.pdf (accessed on 8 March 2022).
- Aw, J.; Cheng, A.W.R. Medicine and the Law: Telemedicine (Part 2). SMA News 2021, 53, 12–13. [Google Scholar]
| Quality Measures | |
|---|---|
| Structure | Number of review per year (physical and telemedicine) |
| Process | Staff satisfaction Patient satisfaction |
| Outcome | Hospitalization rate after adoption of telemedicine Hospitalization numbers from fluid overload |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Haroon, S.; Voo, T.C.; Chua, H.; Tan, G.L.; Lau, T. Telemedicine and Haemodialysis Care during the COVID-19 Pandemic: An Integrative Review of Patient Safety, Healthcare Quality, Ethics and the Legal Considerations in Singapore Practice. Int. J. Environ. Res. Public Health 2022, 19, 5445. https://doi.org/10.3390/ijerph19095445
Haroon S, Voo TC, Chua H, Tan GL, Lau T. Telemedicine and Haemodialysis Care during the COVID-19 Pandemic: An Integrative Review of Patient Safety, Healthcare Quality, Ethics and the Legal Considerations in Singapore Practice. International Journal of Environmental Research and Public Health. 2022; 19(9):5445. https://doi.org/10.3390/ijerph19095445
Chicago/Turabian StyleHaroon, Sabrina, Teck Chuan Voo, Hillary Chua, Gan Liang Tan, and Titus Lau. 2022. "Telemedicine and Haemodialysis Care during the COVID-19 Pandemic: An Integrative Review of Patient Safety, Healthcare Quality, Ethics and the Legal Considerations in Singapore Practice" International Journal of Environmental Research and Public Health 19, no. 9: 5445. https://doi.org/10.3390/ijerph19095445
APA StyleHaroon, S., Voo, T. C., Chua, H., Tan, G. L., & Lau, T. (2022). Telemedicine and Haemodialysis Care during the COVID-19 Pandemic: An Integrative Review of Patient Safety, Healthcare Quality, Ethics and the Legal Considerations in Singapore Practice. International Journal of Environmental Research and Public Health, 19(9), 5445. https://doi.org/10.3390/ijerph19095445






