A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study
Abstract
:1. Introduction
The Intervention OFTT
2. Materials and Methods
2.1. Framework Development
2.1.1. Phase 1: OFTT Set Up
2.1.2. Phase 2: Quantitative Data Collection
2.1.3. Phase 3: Qualitative Data Collection
2.1.4. Phase 4: Brainstorming, Triangulation and Discussion
2.2. Stakeholders
- Patients: the direct users of OFTTs
- Health care providers, doctors and GPs: they know the questions that are being asked by patients and help define the essential contents of an OFTT
- Health care authorities: They are responsible for health care provision and legal frameworks and criteria to be considered. See Figure 1.
2.3. Ethics
3. Results
How to Apply the Framework
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- SMASS. Available online: https://covidguide.smass.ch/#/pathfinder/chatbot (accessed on 30 September 2020).
- CoviCare24. Available online: https://www.covicare24.com (accessed on 20 January 2021).
- Mellish, T.I.; Luzmore, N.J.; Shahbaz, A.A. Why were the UK and USA unprepared for the COVID-19 pandemic? The systemic weaknesses of neoliberalism: A comparison between the UK, USA, Germany, and South Korea. J. Glob. Faultlines 2020, 7, 9–45. [Google Scholar] [CrossRef]
- CoronaCheck for Healthcare Professionals|CoronaCheck Unisanté. Available online: https://coronavirus.unisante.ch/en/professionnels (accessed on 1 December 2020).
- Zhang, Z.; Brazil, J.; Ozkaynak, M.; Desanto, K. Evaluative Research of Technologies for Prehospital Communication and Coordination: A Systematic Review. J. Med. Syst. 2020, 44, 100. [Google Scholar] [CrossRef] [PubMed]
- Effects and Utility of an Online forward Triage Tool during the SARS-CoV-2 Pandemic: Patient Perspectives. JMIR Prepr n.d. Available online: https://preprints.jmir.org/preprint/26553 (accessed on 4 January 2021).
- Langford, M. A Poverty of Rights: Six Ways to Fix the MDGs; Institute of Development Studies: Brighton, UK, 2010; Available online: https://www.ids.ac.uk/publications/a-poverty-of-rights-six-ways-to-fix-the-mdgs/ (accessed on 1 January 2021).
- Omboni, S.; Caserini, M.; Coronetti, C. Telemedicine and M-Health in Hypertension Management: Technologies, Applications and Clinical Evidence. High Blood Press. Cardiovasc. Prev. Off. J. Ital. Soc. Hypertens. 2016, 23, 187–196. [Google Scholar] [CrossRef] [PubMed]
- Rhoads, S.J.; Serrano, C.I.; Lynch, C.E.; Ounpraseuth, S.T.; Gauss, C.H.; Payakachat, N.; Lowery, C.L.; Eswaran, H. Exploring Implementation of m-Health Monitoring in Postpartum Women with Hypertension. Telemed. J. E-Health Off. J. Am. Telemed. Assoc. 2017, 23, 833–841. [Google Scholar] [CrossRef] [PubMed]
- Hsu, W.C.; Lau, K.H.K.; Huang, R.; Ghiloni, S.; Le, H.; Gilroy, S.; Abrahamson, M.; Moore, J. Utilization of a Cloud-Based Diabetes Management Program for Insulin Initiation and Titration Enables Collaborative Decision Making Between Healthcare Providers and Patients. Diabetes Technol. Ther. 2016, 18, 59–67. [Google Scholar] [CrossRef] [PubMed]
- Chambers, D.; Cantrell, A.J.; Johnson, M.; Preston, L.; Baxter, S.K.; Booth, A.; Turner, J. Digital and online symptom checkers and health assessment/triage services for urgent health problems: Systematic review. BMJ Open 2019, 9, e027743. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stratil, J.M.; Voss, M.; Arnold, L. WICID framework version 1.0: Criteria and considerations to guide evidence-informed decision-making on non-pharmacological interventions targeting COVID-19. BMJ Global Health 2020, 5, e003699. [Google Scholar] [CrossRef] [PubMed]
- Michel, J.; Hautz, W.; Sauter, T. Telemedicine and Online Platforms as an Opportunity to Optimise Qualitative Data Collection, Explore and Understand Disease Pathways in a Novel Pandemic Like COVID-19. J. Int. Soc. Telemed. E-Health 2020, 8, e9.1–e9.4. [Google Scholar] [CrossRef]
- Michel, J.; Chimbindi, N.; Mohlakoana, N.; Orgill, M.; Bärnighausen, T.; Obrist, B.; Tediosi, F.; Evans, D.; McIntryre, D.; Bressers, H.T.; et al. How and why policy-practice gaps come about: A South African Universal Health Coverage context. J. Glob. Health Rep. 2019, 3, e2019069. [Google Scholar] [CrossRef]
- Michel, J.; Mettler, A.; Stuber, R.; Müller, M.; Ricklin, M.; Jent, P.; Hautz, W.E.; Sauter, T.C. Effects and utility of an online forward triage tool during the SARS-CoV-2 pandemic: A mixed method study and patient perspectives, Switzerland. BMJ Open, 2022; in press. [Google Scholar]
- ResearchGate. Figure 1 Social Ecological Framework for Nutrition and Physical Activity. Available online: https://www.researchgate.net/figure/Social-ecological-framework-for-nutrition-and-physical-activity-decisions-Source_fig1_276060761 (accessed on 15 March 2021).
- World Health Organization. The Ecological Framework. Available online: https://www.who.int/violenceprevention/approach/ecology/en/ (accessed on 15 March 2021).
- Bauman, D.H. Five Questions to Help Navigate Evaluating Symptom Checker/Triage Tools. EBSCO Health Notes. 2020. Available online: https://health.ebsco.com/blog/article/five-questions-to-help-navigate-evaluating-symptom-checker-triage-tools (accessed on 15 July 2020).
- bsco Health. Enabling Patient Engagement with a Symptom Checker. 2020. Available online: https://www.ebsco.com/sites/g/files/nabnos191/files/acquiadam-assets/Enabling-Patient-Engagement-with-a-Symptom-Checker-White-Paper.pdf (accessed on 1 February 2022).
- Michel, J.; Stuber, R.; Müller, M.; Mettler, A.; Furrer, H.; Ferrand, R.A.; Exadaktylos, A.K.; Hautz, W.E.; Sauter, T.C. COVID-19 and HIV testing: Different viruses but similar prejudices and psychosocial impacts. J. Glob. Health Rep. 2021, 5, e2021022. [Google Scholar] [CrossRef]
- Michel, J.; Mettler, A.; Hautz, W.E.; Sauter, T.C. What is the optimal length of an Online Forward Triage Tool? The need for a framework. J. Glob. Health 2020, 10, 0203103. [Google Scholar] [CrossRef] [PubMed]
- Battineni, G.; Nittari, G.; Sirignano, A.; Amenta, F. Are telemedicine systems effective healthcare solutions during the COVID-19 pandemic? J. Taibah Univ. Med. Sci. 2021, 16, 305–306. [Google Scholar] [CrossRef] [PubMed]
- Michel, J.; Mettler, A.; Starvaggi, C.; Aebi, C.; Keitel, K.; Sauter, T.C. The utility of a pediatric COVID-19 online forward triage tool in. Front Public Health, 2022; under review. [Google Scholar]
- Battineni, G.; Pallotta, G.; Nittari, G.; Amenta, F. Telemedicine framework to mitigate the impact of the COVID-19 pandemic. J. Taibah Univ. Med. Sci. 2021, 16, 300–302. [Google Scholar] [CrossRef] [PubMed]
| Stage 1: Building Up and Setting Up OFTT, Vetting the Engine, Algorithms etc. | Stage 2: Ensuring Content Validity, Reliability and Comprehensiveness and Timeliness-Evidence Constantly Changing in Novel Conditions Science vs. Social Media News | Stage 3. Effects on Individual, Societal and Health System and Broader Structural Levels |
|---|---|---|
 | ||
| Stage and Type of Data | Results | Implications |
|---|---|---|
| Online OFTT set up | Number of completed requests between 2 March and 12 May 2020 (n = 6272) [6] | The tool was not advertised, despite that, many people visited the tool-demonstrating that the Swiss society has embraced OFTTs |
| Survey | The mean age of the participants of the email survey was 50.1 years (SD 15.4, range 18–82), with 57.4% being female | All age groups accessed the OFTT |
| 87.5% of the survey participants found the website helpful [6] | Participants trusted and followed the tool recommendations | |
| 85.2% of the participants followed the recommendations given to test or not test [6]. | 85% (Effects and Utility of an Online Forward Triage Tool during the SARS-CoV-2 Pandemic.) | |
| 65% of the participants called their GP ahead of their visit [6] | Participants followed the recommendation to call the health care provider ahead of time in case they suspected COVID-19 (Effects and Utility of an Online Forward Triage Tool during the SARS-CoV-2 Pandemic.) | |
| 41.1% of all users would have contacted the GP or visited a hospital had the tool not existed; furthermore, 16.8% would have contacted a hotline (Effects and Utility of an Online Forward Triage Tool during the SARS-CoV-2 Pandemic.) | Many participants would have called the GP or hotline, so the tool potentially reduced the burden on the health system (Effects and Utility of an Online Forward Triage Tool during the SARS-CoV-2 Pandemic.) | |
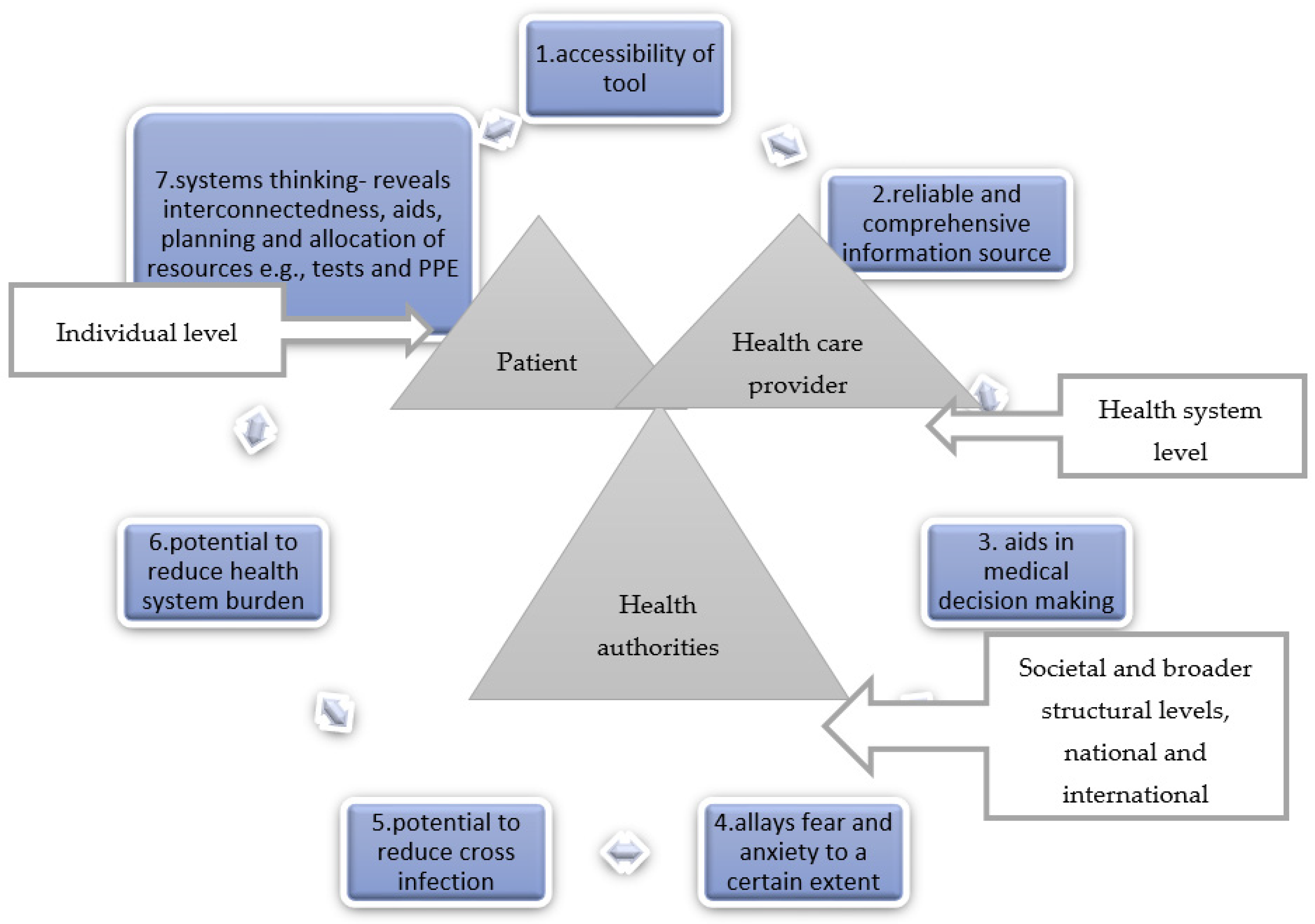
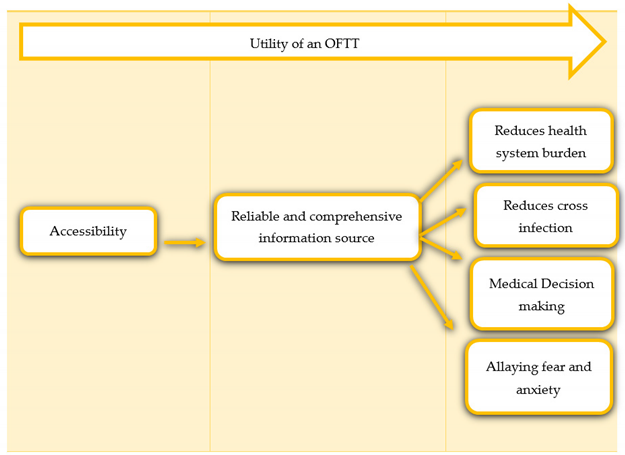
| Face-to-face interviews | Themes that emerged accessibility, utility of tool in preventing cross-infection, utility of tool in reducing health system burden, utility of tool as a comprehensive and reliable information source, utility of tool in allaying fear and anxiety and utility of tool in medical decision-making | Our main qualitative findings demonstrated that a COVID-19 OFTT can go beyond reducing the health system burden. Our primary hypothesis to having the potential to prevent cross-infection, allaying fear and anxiety to a certain extent, facilitating decision-making and providing reliable information, once accessibility issues are overcome These themes and concepts guided our framework |
| Criteria | Stakeholder | Description of the Criteria | Points |
|---|---|---|---|
| Accessibility of tool | Patient Health care provider Health Authorities | This covers the implication that tool accessibility can be assessed by how high up the tool appears on top search engines, such as Google. This also covers the implication that the language is clear, the length of the tool, i.e., how long it takes a sick patient to respond to the questions, including how long it takes for the patient to get the recommendation to call 911, completion rates, number of questions, etc., all affect tool accessibility [21] | 1 |
| A reliable source of information | Patient Health care provider Health Authorities | This covers the implication that how comprehensive a tool is depends upon the users finding the information that led them to the search engine, for example, with regards to symptoms, when to test, where to test, including contact numbers, when to call a doctor and how-to self-care | 1 |
| Medical decision-making | Patient Health care provider Health Authorities | This covers the implication that the utility of a tool can be measured by the proportion of users who follow the recommendations given by the tool. This covers the implication that trust in the tool is very important. Transparency with regards to tool validation and algorithm behind recommendations increases trust, e.g., you have a 95% probability of having COVID-19, test, or you have a 5% probability of having COVID-19, do not test | 1 |
| Allaying fear and anxiety | Patient Health care provider Health Authorities | This covers the implications of feeling better, reassured and/or less anxious after filling the OFTT. Knowledge is power | 1 |
| Reducing health system burden | Patient Health care provider Health Authorities | This covers the implication of being able to access health care services and or knowledge within the comfort of one’s own home without the need to visit a healthcare facility | 1 |
| Reducing cross-infection | Patient Health care provider Health Authorities | This covers the implication of communicating with the health care providers well ahead of visiting and making them aware a suspect is visiting the practice and taking all necessary precautions and arrangements | 1 |
| Systems thinking-showing interconnectedness- | Patient Health care provider Health Authorities | This covers the implications that a health system is a complex, adapted system. Issues affecting one area, e.g., supply chain, will affect other areas. This covers the implication that the utility of the tool is dependent upon other health systems and societal components, e.g., participants were told by the tool to test only to be told that there are no tests (shortages). This covers the implication that economic factors, such as the cost of the test influenced some not to test This covers the implication that a new life-threatening disease in a population is associated with psycho-social and behavioural issues that need to be taken into account. Fear of a positive test, psychological readiness, can prevent people from testing | 1 |
| Total points | 7 points =OFTT is fit for purpose, i.e., COVID-19. 5–6 points =OFTT is good but can be improved. 4 or less points =OFTT is insufficient. Criterion based utility The usefulness of a tool can also be based on criteria fulfilled. Depending on context and purpose, the more criterion fulfilled, the better the tool For example The tool is useful in reducing the health system burden and as an information source | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Michel, J.; Mettler, A.; Müller, M.; Hautz, W.E.; Sauter, T.C. A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study. Int. J. Environ. Res. Public Health 2022, 19, 5184. https://doi.org/10.3390/ijerph19095184
Michel J, Mettler A, Müller M, Hautz WE, Sauter TC. A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5184. https://doi.org/10.3390/ijerph19095184
Chicago/Turabian StyleMichel, Janet, Annette Mettler, Martin Müller, Wolf E. Hautz, and Thomas C. Sauter. 2022. "A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study" International Journal of Environmental Research and Public Health 19, no. 9: 5184. https://doi.org/10.3390/ijerph19095184
APA StyleMichel, J., Mettler, A., Müller, M., Hautz, W. E., & Sauter, T. C. (2022). A Utility Framework for COVID-19 Online Forward Triage Tools: A Swiss Telehealth Case Study. International Journal of Environmental Research and Public Health, 19(9), 5184. https://doi.org/10.3390/ijerph19095184






