Validity and Reliability of the Daily Activity Behaviours Questionnaire (DABQ) for Assessment of Time Spent in Sleep, Sedentary Behaviour, and Physical Activity
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Measures
2.2.1. Sleep, Sedentary Behaviour, and Physical Activity
2.2.2. Sociodemographic Data
2.3. Data Processing
2.4. Statistical Analysis
3. Results
3.1. Participant Characteristics
3.2. Reliability of the Daily Activity Behaviours Questionnaire (DABQ)
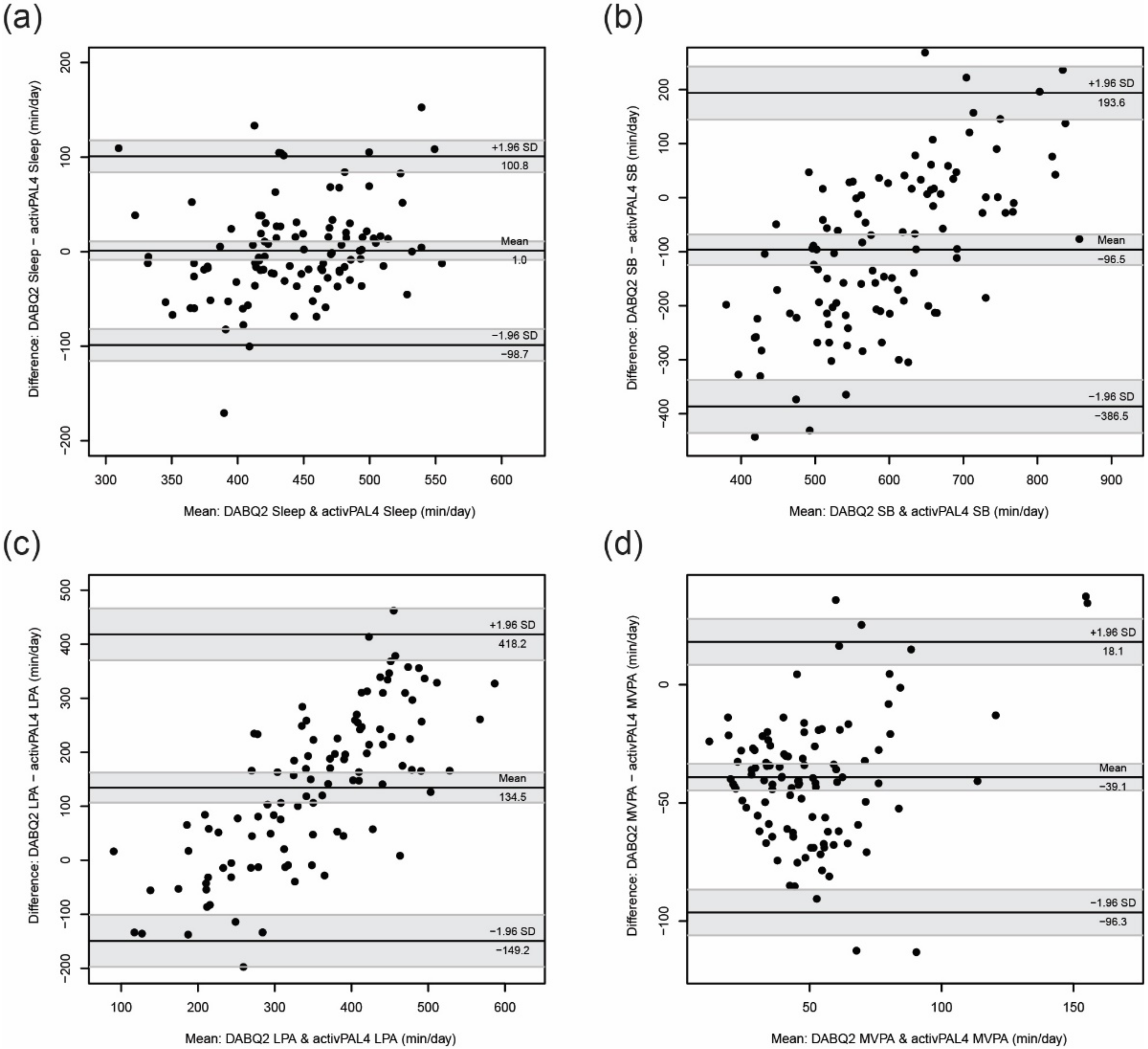
3.3. Validity of the Daily Activity Behaviours Questionnaire (DABQ)
4. Discussion
4.1. Key Findings
4.2. Reliability and Validity of the Estimated Sleep Duration
4.3. Reliability and Validity of the Estimated Time Spent in Sedentary Behaviour
4.4. Reliability and Validity of the Estimated Time Spent in Physical Activity
4.5. Implications for Research and Practice
4.6. Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Physical Activity Guidelines Advisory Committee. 2018 Physical Activity Guidelines Advisory Committee Scientific Report; U.S. Department of Health and Human Services: Washington, DC, USA, 2018. [Google Scholar]
- Chaput, J.-P.; Dutil, C.; Featherstone, R.; Ross, R.; Giangregorio, L.; Saunders, T.J.; Janssen, I.; Poitras, V.J.; Kho, M.E.; Ross-White, A.; et al. Sleep duration and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020, 45, S218–S231. [Google Scholar] [CrossRef] [PubMed]
- Ross, R.; Chaput, J.-P.; Giangregorio, L.M.; Janssen, I.; Saunders, T.J.; Kho, M.E.; Poitras, V.J.; Tomasone, J.R.; El-Kotob, R.; McLaughlin, E.C.; et al. Canadian 24-Hour Movement Guidelines for Adults aged 18–64 years and Adults aged 65 years or older: An integration of physical activity, sedentary behaviour, and sleep. Appl. Physiol. Nutr. Metab. 2020, 45, S57–S102. [Google Scholar] [CrossRef] [PubMed]
- Saunders, T.J.; McIsaac, T.; Douillette, K.; Gaulton, N.; Hunter, S.; Rhodes, R.E.; Prince, S.A.; Carson, V.; Chaput, J.-P.; Chastin, S.; et al. Sedentary behaviour and health in adults: An overview of systematic reviews. Appl. Physiol. Nutr. Metab. 2020, 45, S197–S217. [Google Scholar] [CrossRef] [PubMed]
- Füzéki, E.; Engeroff, T.; Banzer, W. Health Benefits of Light-Intensity Physical Activity: A Systematic Review of Accelerometer Data of the National Health and Nutrition Examination Survey (NHANES). Sports Med. 2017, 47, 1769–1793. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; De Craemer, M.; De Cocker, K.; Powell, L.; Van Cauwenberg, J.; Dall, P.; Hamer, M.; Stamatakis, E. How does light-intensity physical activity associate with adult cardiometabolic health and mortality? Systematic review with meta-analysis of experimental and observational studies. Br. J. Sports Med. 2019, 53, 370–376. [Google Scholar] [CrossRef] [Green Version]
- Pedišić, Ž.; Dumuid, D.; Olds, T.S. Integrating sleep, sedentary behaviour, and physical activity research in the emerging field of time-use epidemiology: Definitions, concepts, statistical methods, theoretical framework, and future directions. Kinesiology 2017, 49, 252–269. [Google Scholar]
- Rollo, S.; Antsygina, O.; Tremblay, M.S. The whole day matters: Understanding 24-hour movement guideline adherence and relationships with health indicators across the lifespan. J. Sport Health Sci. 2020, 9, 493–510. [Google Scholar] [CrossRef]
- Bakker, E.A.; Hartman, Y.A.W.; Hopman, M.T.E.; Hopkins, N.D.; Graves, L.E.F.; Dunstan, D.W.; Healy, G.N.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Validity and reliability of subjective methods to assess sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–31. [Google Scholar] [CrossRef]
- Dowd, K.P.; Szeklicki, R.; Minetto, M.A.; Murphy, M.H.; Polito, A.; Ghigo, E.; Van Der Ploeg, H.; Ekelund, U.; Maciaszek, J.; Stemplewski, R.; et al. A systematic literature review of reviews on techniques for physical activity measurement in adults: A DEDIPAC study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 15. [Google Scholar] [CrossRef]
- Pedišić, Ž.; Bauman, A. Accelerometer-based measures in physical activity surveillance: Current practices and issues. Br. J. Sports Med. 2015, 49, 219–223. [Google Scholar] [CrossRef]
- Pedišić, Ž.; Craig, C.L.; Bauman, A.E. Physical activity surveillance in the context of low- and middle-income countries. In Physical Activity in Low- and Middle-Income Countries; Siefken, K., Ramirez Varela, A., Waqanivalu, T., Schulenkorf, N., Eds.; Routledge: London, UK, 2021; pp. 90–108. [Google Scholar]
- Troiano, R.P.; Stamatakis, E.; Bull, F.C. How can global physical activity surveillance adapt to evolving physical activity guidelines? Needs, challenges and future directions. Br. J. Sports Med. 2020, 54, 1468–1473. [Google Scholar] [CrossRef] [PubMed]
- Lee, P.H. Validation of the National Health and Nutritional Survey (NHANES) single-item self-reported sleep duration against wrist-worn accelerometer. Sleep Breath. 2021, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Craig, C.L.; Marshall, A.L.; Sjöström, M.; Bauman, A.E.; Booth, M.L.; Ainsworth, B.E.; Pratt, M.; Ekelund, U.L.; Yngve, A.; Sallis, J.F.; et al. International Physical Activity Questionnaire: 12-Country Reliability and Validity. Med. Sci. Sports Exerc. 2003, 35, 1381–1395. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bull, F.C.; Maslin, T.S.; Armstrong, T. Global Physical Activity Questionnaire (GPAQ): Nine Country Reliability and Validity Study. J. Phys. Act. Health 2009, 6, 790–804. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grgic, J.; Dumuid, D.; Bengoechea, E.G.; Shrestha, N.; Bauman, A.; Olds, T.; Pedišić, Ž. Health outcomes associated with reallocations of time between sleep, sedentary behaviour, and physical activity: A systematic scoping review of isotemporal substitution studies. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 69. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, I.; Clarke, A.E.; Carson, V.; Chaput, J.-P.; Giangregorio, L.M.; Kho, M.E.; Poitras, V.J.; Ross, R.; Saunders, T.J.; Ross-White, A.; et al. A systematic review of compositional data analysis studies examining associations between sleep, sedentary behaviour, and physical activity with health outcomes in adults. Appl. Physiol. Nutr. Metab. 2020, 45, S248–S257. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, B.; Encantado, J.; Carraça, E.; Sousa-Sá, E.; Lopes, L.; Cliff, D.; Mendes, R.; Silva, M.N.; Godinho, C.; Santos, R. Questionnaires measuring movement behaviours in adults and older adults: Content description and measurement properties. A systematic review. PLoS ONE 2022, 17, e0265100. [Google Scholar] [CrossRef] [PubMed]
- Bonett, D.G. Sample size requirements for estimating intraclass correlations with desired precision. Stat. Med. 2002, 21, 1331–1335. [Google Scholar] [CrossRef]
- Chastin, S.F.M.; Dontje, M.L.; Skelton, D.A.; Čukić, I.; Shaw, R.J.; Gill, J.M.R.; Greig, C.A.; Gale, C.R.; Deary, I.J.; Der, G.; et al. Systematic comparative validation of self-report measures of sedentary time against an objective measure of postural sitting (activPAL). Int. J. Behav. Nutr. Phys. Act. 2018, 15, 21. [Google Scholar] [CrossRef] [Green Version]
- Sellers, C.; Dall, P.; Grant, M.; Stansfield, B. Validity and reliability of the activPAL3 for measuring posture and stepping in adults and young people. Gait Posture 2016, 43, 42–47. [Google Scholar] [CrossRef] [Green Version]
- Lyden, K.; Keadle, S.K.; Staudenmayer, J.; Freedson, P.S. The activPALTM Accurately Classifies Activity Intensity Categories in Healthy Adults. Med. Sci. Sports Exerc. 2017, 49, 1022–1028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carlson, J.A.; Tuz-Zahra, F.; Bellettiere, J.; Ridgers, N.D.; Steel, C.; Bejarano, C.; LaCroix, A.Z.; Rosenberg, D.E.; Greenwood-Hickman, M.A.; Jankowska, M.M.; et al. Validity of Two Awake Wear-Time Classification Algorithms for activPAL in Youth, Adults, and Older Adults. J. Meas. Phys. Behav. 2021, 4, 151–162. [Google Scholar] [CrossRef] [PubMed]
- Aguilar-Farias, N.; Martino-Fuentealba, P.; Salom-Diaz, N.; Brown, W.J. How many days are enough for measuring weekly activity behaviours with the ActivPAL in adults? J. Sci. Med. Sport 2019, 22, 684–688. [Google Scholar] [CrossRef]
- PAL Technologies. Clasification Algorithms: CREA. Available online: https://kb.palt.com/articles/crea/ (accessed on 14 April 2022).
- Chastin, S.F.; Culhane, B.; Dall, P.M. Comparison of self-reported measure of sitting time (IPAQ) with objective measurement (activPAL). Physiol. Meas. 2014, 35, 2319–2328. [Google Scholar] [CrossRef] [Green Version]
- Kastelic, K.; Šarabon, N. Comparison of Self-Reported Sedentary Time on Weekdays with an Objective Measure (activPAL). Meas. Phys. Educ. Exerc. Sci. 2019, 23, 227–236. [Google Scholar] [CrossRef]
- Lyden, K. activpalProcessing: Process activPAL Events Files, R Package Version 1.0.2. 2016. Available online: http://cran.nexr.com/web/packages/activpalProcessing/index.html (accessed on 20 December 2021).
- Haszard, J.J.; Meredith-Jones, K.; Farmer, V.; Williams, S.; Galland, B.; Taylor, R. Non-Wear Time and Presentation of Compositional 24-Hour Time-Use Analyses Influence Conclusions About Sleep and Body Mass Index in Children. J. Meas. Phys. Behav. 2020, 3, 204–210. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020. [Google Scholar]
- R Studio Team. RStudio: Integrated Development Environment for R. Boston MA 2020, 770, 165–171. [Google Scholar]
- Lehnert, B. BlandAltmanLeh: Plots (Slightly Extended) Bland-Altman Plots, R Package Version 0.3.1. 2020. Available online: https://cran.r-project.org/web/packages/BlandAltmanLeh/index.html (accessed on 20 December 2021).
- Signorell, A.; Aho, K.; Alfons, A.; Anderegg, N.; Aragon, T.; Arachchige, C.; Arppe, A.; Baddeley, A.; Barton, K.; Bolker, B.; et al. DescTools: Tools for Descriptive Statistics, R Package Version 0.99.42. 2020. Available online: https://cran.r-project.org/web/packages/DescTools/index.html (accessed on 20 December 2021).
- Wickham, H.; François, R.; Henry, L.; Müller, K. dplyr: A Grammar of Data Manipulation, R Package Version 1.0.5. 2020. Available online: https://cran.r-project.org/package=dplyr (accessed on 20 December 2021).
- Wickham, H.; Chang, W.; Henry, L.; Pedersen, T.L.; Takahashi, K.; Wilke, C.; Woo, K.; Yutani, H. ggplot2: Create Elegant Data Visualisations Using the Grammar of Graphics, R Package Version 3.3.3. 2019. Available online: https://cran.r-project.org/package=ggplot2 (accessed on 20 December 2021).
- Revelle, W. psych: A Package for Personality, Psychometric, and Psychological Research, R Package Version 2.1.6. 2020. Available online: https://cran.r-project.org/web/packages/psych/index.html (accessed on 20 December 2021).
- R Core Team. stats: The R Stats Package, R Package Version 4.0.5. 2020. Available online: https://stat.ethz.ch/R-manual/R-devel/library/stats/html/stats-package.html (accessed on 20 December 2021).
- Prince, S.A.; Cardilli, L.; Reed, J.L.; Saunders, T.J.; Kite, C.; Douillette, K.; Fournier, K.; Buckley, J.P. A comparison of self-reported and device measured sedentary behaviour in adults: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 31. [Google Scholar] [CrossRef]
- Helmerhorst, H.H.J.; Brage, S.; Warren, J.; Besson, H.; Ekelund, U. A systematic review of reliability and objective criterion-related validity of physical activity questionnaires. Int. J. Behav. Nutr. Phys. Act. 2012, 9, 103. [Google Scholar] [CrossRef] [Green Version]
- Lauderdale, D.S.; Knutson, K.L.; Yan, L.L.; Liu, K.; Rathouz, P.J. Self-Reported and Measured Sleep Duration: How Similar Are They? Epidemiology 2008, 19, 838–845. [Google Scholar] [CrossRef] [Green Version]
- Cespedes, E.M.; Hu, F.B.; Redline, S.; Rosner, B.; Alcantara, C.; Cai, J.; Hall, M.H.; Loredo, J.S.; Mossavar-Rahmani, Y.; Ramos, A.R.; et al. Comparison of Self-Reported Sleep Duration with Actigraphy: Results From the Hispanic Community Health Study/Study of Latinos Sueño Ancillary Study. Am. J. Epidemiol. 2016, 183, 561–573. [Google Scholar] [CrossRef] [PubMed]
- Mollayeva, T.; Thurairajah, P.; Burton, K.; Mollayeva, S.; Shapiro, C.M.; Colantonio, A. The Pittsburgh sleep quality index as a screening tool for sleep dysfunction in clinical and non-clinical samples: A systematic review and meta-analysis. Sleep Med. Rev. 2016, 25, 52–73. [Google Scholar] [CrossRef] [PubMed]
- Fabbri, M.; Beracci, A.; Martoni, M.; Meneo, D.; Tonetti, L.; Natale, V. Measuring Subjective Sleep Quality: A Review. Int. J. Environ. Res. Public Health 2021, 18, 1082. [Google Scholar] [CrossRef] [PubMed]
- Sember, V.; Meh, K.; Sorić, M.; Starc, G.; Rocha, P.; Jurak, G. Validity and Reliability of International Physical Activity Questionnaires for Adults across EU Countries: Systematic Review and Meta Analysis. Int. J. Environ. Res. Public Health 2020, 17, 7161. [Google Scholar] [CrossRef]
- Kim, Y.; Park, I.; Kang, M. Convergent validity of the International Physical Activity Questionnaire (IPAQ): Meta-analysis. Public Health Nutr. 2012, 16, 440–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lee, P.H.; Macfarlane, D.J.; Lam, T.H.; Stewart, S.M. Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurtze, N.; Rangul, V.; Hustvedt, B.-E.; Flanders, W.D. Reliability and validity of self-reported physical activity in the Nord-Trøndelag Health Study (HUNT 2). Eur. J. Epidemiol. 2007, 22, 379–387. [Google Scholar] [CrossRef] [PubMed]
- Kastelic, K.; Pedišić, Ž.; Lipovac, D.; Kastelic, N.; Chen, S.-T.; Šarabon, N. Associations of meeting 24-h movement guidelines with stress and self-rated health among adults: Is meeting more guidelines associated with greater benefits? BMC Public Health. 2021, 21, 929. [Google Scholar] [CrossRef]
| Characteristic | Reliability Sample n (%) | Validity Sample n (%) |
|---|---|---|
| Age group | ||
| 24 to 34 years | 42 (36.8) | 38 (35.5) |
| 35 to 45 years | 46 (40.4) | 44 (41.1) |
| 46 to 56 years | 26 (22.8) | 25 (23.4) |
| Sex | ||
| Female | 46 (40.4) | 45 (42.1) |
| Male | 68 (59.6) | 62 (57.9) |
| BMI category | ||
| “Normal” weight (18.0 to 24.9 kg/m2) | 53 (46.5) | 52 (48.6) |
| Overweight (25.0 to 29.9 kg/m2) | 39 (34.2) | 35 (32.7) |
| Obese (≥ 30 kg/m2) | 22 (19.3) | 20 (18.7) |
| Education | ||
| Primary or secondary education | 27 (23.7) | 22 (20.6) |
| Tertiary education (college) | 30 (26.3) | 29 (27.1) |
| Tertiary education (university) | 57 (50.0) | 56 (52.3) |
| Work schedule | ||
| Non-shift work | 58 (50.9) | 55 (51.4) |
| Shift work | 56 (49.1) | 52 (48.6) |
| Movement Behaviour | DABQ1 Mean (SD), min/day | DABQ2 Mean (SD), min/day | ICC[A,1] (95% CI) | ICC[C,1] (95% CI) | Spearman’s ρ (95% CI) |
|---|---|---|---|---|---|
| Sleep | 430 (54) | 443 (63) | 0.59 (0.48, 0.69) | 0.61 (0.50, 0.69) | 0.64 (0.52, 0.74) |
| SB | 547 (163) | 547 (166) | 0.65 (0.55, 0.73) | 0.65 (0.55, 0.73) | 0.62 (0.49, 0.72) |
| LPA | 423 (165) | 416 (167) | 0.69 (0.60, 0.77) | 0.69 (0.60, 0.77) | 0.67 (0.56, 0.76) |
| MVPA | 40 (41) | 34 (35) | 0.65 (0.55, 0.73) | 0.65 (0.56, 0.74) | 0.60 (0.47, 0.71) |
| Movement Behaviour | DABQ2 Mean (SD), min/day | activPAL4 Mean (SD), min/day | ICC[A,1] (95% CI) | ICC[C,1] (95% CI) | Spearman’s ρ (95% CI) |
|---|---|---|---|---|---|
| Sleep | 443 (64) | 442 (52) | 0.63 (0.52, 0.71) | 0.63 (0.52, 0.71) | 0.66 (0.54, 0.76) |
| SB | 547 (165) | 643 (85) | 0.29 (0.09, 0.45) | 0.36 (0.22, 0.49) | 0.42 (0.25, 0.56) |
| LPA | 418 (165) | 284 (70) | 0.22 (−0.00, 0.41) | 0.35 (0.20, 0.48) | 0.45 (0.29, 0.59) |
| MVPA | 31 (32) | 71 (25) | 0.24 (−0.05, 0.48) | 0.47 (0.33, 0.58) | 0.38 (0.21, 0.53) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kastelic, K.; Šarabon, N.; Burnard, M.D.; Pedišić, Ž. Validity and Reliability of the Daily Activity Behaviours Questionnaire (DABQ) for Assessment of Time Spent in Sleep, Sedentary Behaviour, and Physical Activity. Int. J. Environ. Res. Public Health 2022, 19, 5362. https://doi.org/10.3390/ijerph19095362
Kastelic K, Šarabon N, Burnard MD, Pedišić Ž. Validity and Reliability of the Daily Activity Behaviours Questionnaire (DABQ) for Assessment of Time Spent in Sleep, Sedentary Behaviour, and Physical Activity. International Journal of Environmental Research and Public Health. 2022; 19(9):5362. https://doi.org/10.3390/ijerph19095362
Chicago/Turabian StyleKastelic, Kaja, Nejc Šarabon, Michael D. Burnard, and Željko Pedišić. 2022. "Validity and Reliability of the Daily Activity Behaviours Questionnaire (DABQ) for Assessment of Time Spent in Sleep, Sedentary Behaviour, and Physical Activity" International Journal of Environmental Research and Public Health 19, no. 9: 5362. https://doi.org/10.3390/ijerph19095362
APA StyleKastelic, K., Šarabon, N., Burnard, M. D., & Pedišić, Ž. (2022). Validity and Reliability of the Daily Activity Behaviours Questionnaire (DABQ) for Assessment of Time Spent in Sleep, Sedentary Behaviour, and Physical Activity. International Journal of Environmental Research and Public Health, 19(9), 5362. https://doi.org/10.3390/ijerph19095362







