Predictors of Healthcare Professionals’ Work Difficulty Perception during the COVID-19 Pandemic: Study of Work Environment in a Pandemic Hospital
Abstract
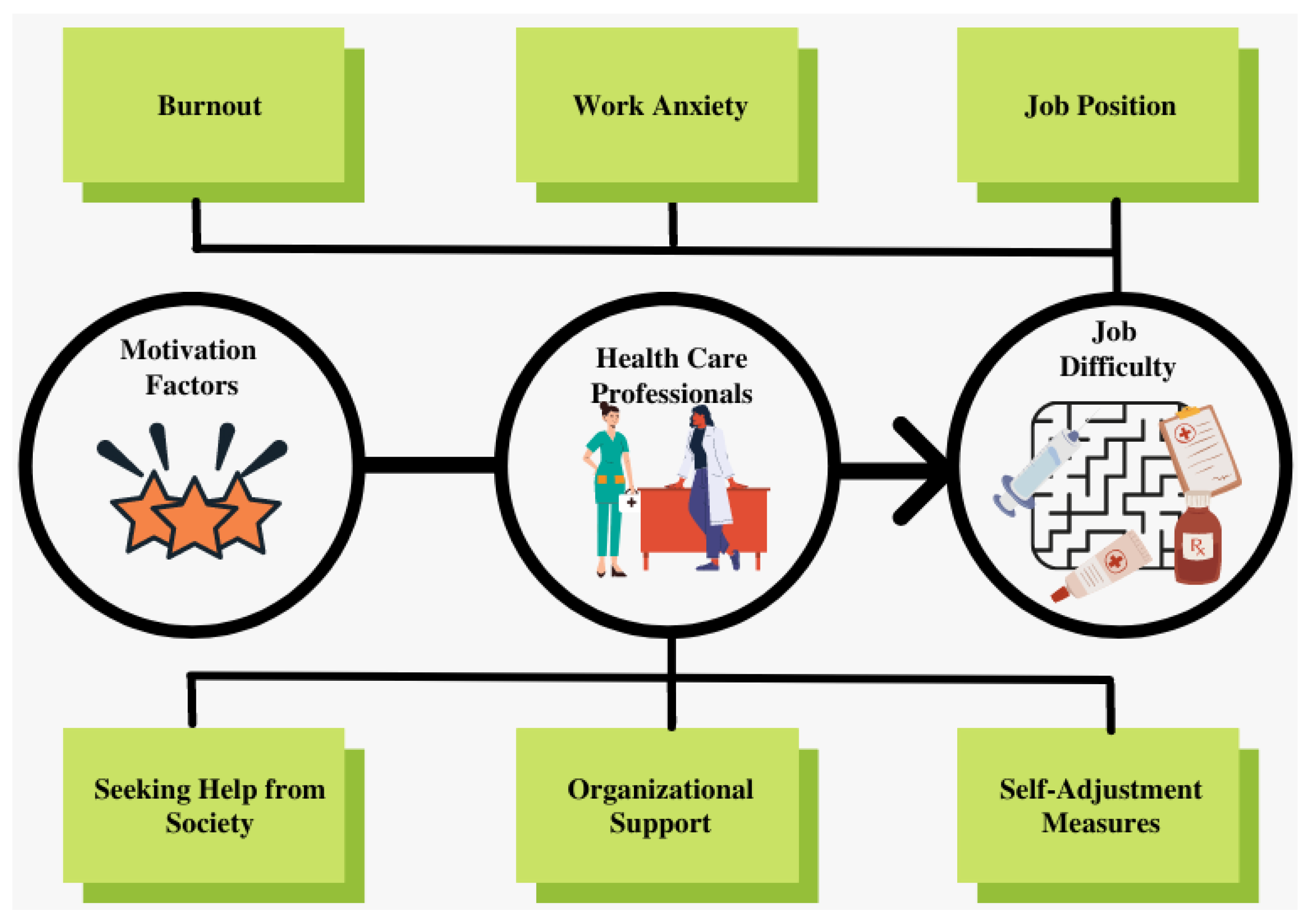
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Instrumentation
2.3. Statistical Data Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Van Knippenberg, D. Work motivation and performance: A social identity perspective. Appl. Psychol. 2000, 49, 357–371. [Google Scholar] [CrossRef]
- Shortell, S.M.; Kaluzny, A.D. Podstawy zarządzania opieką zdrowotną. In Uniwersyteckie Wydawawnictwo Medyczne “Vesalius”; VÉSALIUS: Kraków, Poland, 2001; ISBN 83-85688-67-6. [Google Scholar]
- Arnetz, B.B. Psychosocial challenges facing physicians of today. Soc. Sci. Med. 2001, 52, 203–213. [Google Scholar] [CrossRef]
- World Health Organization. The World Health Report 2006: Working Together for Health; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Lambrou, P.; Kontodimopoulos, N.; Niakas, D. Motivation and job satisfaction among medical and nursing staff in a Cyprus public general hospital. Hum. Resour. Health 2010, 8, 1–9. [Google Scholar] [CrossRef] [Green Version]
- Grujičić, M.; Jovičić-Bata, J.; Novaković, B. Work motivation and job satisfaction of doctors and nurses in Vojvodina, Serbia. Srp. Arh. Za Celok. Lek. 2018, 146, 48–54. [Google Scholar] [CrossRef] [Green Version]
- Aiken, L.H.; Sermeus, W.; van den Heede, K.; Sloane, D.M.; Busse, R.; McKee, M.; Bruyneel, L.; Rafferty, A.M.; Griffiths, P.; Moreno-Casbas, M.T.; et al. Patient safety, satisfaction, and quality of hospital care: Cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ 2012, 344, e1717. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kutney-Lee, A.; Wu, E.S.; Sloane, D.M.; Aiken, L.H. Changes in hospital nurse work environments and nurse job outcomes: An analysis of panel data. Int. J. Nurs. Stud. 2013, 50, 195–201. [Google Scholar] [CrossRef] [Green Version]
- Yin, K.; Jung, J.; Coiera, E.; Laranjo, L.; Blandford, A.; Khoja, A.; Tai, W.; Phillips, D.P.; Lau, A.Y.S. Patient Work and Their Contexts: Scoping Review. J. Med. Internet Res. 2020, 22, e16656. [Google Scholar] [CrossRef]
- Cullen, W.; Gulati, G.; Kelly, B.D. Mental health in the COVID-19 pandemic. QJM Int. J. Med. 2020, 113, 311–312. [Google Scholar] [CrossRef]
- Baskin, R.G.; Bartlett, R. Healthcare worker resilience during the COVID-19 pandemic: An integrative review. J. Nurs. Manag. 2021, 29, 2329–2342. [Google Scholar]
- Shah, K.; Chaudhari, G.; Kamrai, D.; Lail, A.; Patel, R.S. How essential is to focus on physician’s health and burnout in coronavirus (COVID-19) pandemic? Cureus 2020, 12, e7538. [Google Scholar] [CrossRef] [Green Version]
- Suleiman, A.; IBsisu, s.; Guzu, H.; Santarisi, A.; Alsatari, M.; Abbad, A.; Jaber, A.; Harb, T.; Abuhejleh, A.; Nadi, N.; et al. Preparedness of Frontline Doctors in Jordan Healthcare Facilities to COVID-19 Outbreak. Int. J. Environ. Res. Public Health 2020, 17, 3181. [Google Scholar] [CrossRef] [PubMed]
- Shreffler, J.; Petrey, J.; Huecker, M. The Impact of COVID-19 on Healthcare Worker Wellness: A Scoping Review. West J. Emerg. Med. 2020, 21, 1059–1066. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Director-General’s Opening Remarks at the Media Briefing on COVID-19-17 July 2020; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Spoorthy, M.S.; Pratapa, S.K.; Mahant, S. Mental health problems faced by healthcare workers due to the COVID-19 pandemic—A review. Asian J. Psychiatry 2020, 51, 102119. [Google Scholar] [CrossRef] [PubMed]
- Denning, M.; Goh, E.T.; Tan, B.; Kanneganti, A.; Almonte, M.; Scott, A.; Martin, G.; Clarke, J.; Sounderajah, V.; Markar, S.; et al. Determinants of burnout and other aspects of psychological well-being in healthcare workers during the Covid-19 pandemic: A multinational cross-sectional study. PLoS ONE 2021, 16, e0238666. [Google Scholar] [CrossRef] [PubMed]
- Brand, K.J.; Hapfelmeier, A.; Haller, B. A systematic review of subgroup analyses in randomised clinical trials in cardiovascular disease. Clin. Trials 2021, 18, 351–360. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. 2001, 16, 606–613. [Google Scholar] [CrossRef]
- The State-Trait Anxiety Inventory. Available online: https://journal.sipsych.org/index.php/IJP/article/view/620 (accessed on 21 April 2022).
- Kristensen, T.S.; Borritz, M.; Villadsen, E.; Christensen, K.B. The Copenhagen Burnout Inventory: A new tool for the assessment of burnout. Work. Stress 2005, 19, 192–207. [Google Scholar] [CrossRef]
- Walsh, J.P.; Ashford, S.J.; Hill, T.E. Feedback obstruction: The influence of the information environment on employee turnover intentions. Hum. Relat. 1985, 38, 23–46. [Google Scholar] [CrossRef]
- Kayikcioglu, O.; Bilgin, S.; Seymenoglu, G.; Deveci, A. State and trait anxiety scores of patients receiving intravitreal injections. Biomed. Hub 2017, 2, 1–5. [Google Scholar] [CrossRef] [Green Version]
- Tabur, A.; Tabur, A.; Elkefi, S.; Emhan, A.; Mengenci, C.; Bez, Y.; Asan, O. Anxiety, Burnout and Depression, Psychological Well-Being as Predictor of Healthcare Professionals’ Turnover during the COVID-19 Pandemic: Study in a Pandemic Hospital. Healthcare 2022, 10, 525. [Google Scholar] [CrossRef] [PubMed]
- Kocalevent, R.-D.; Hinz, A.; Brähler, E. Standardization of the depression screener Patient Health Questionnaire (PHQ-9) in the general population. Gen. Hosp. Psychiatry 2013, 35, 551–555. [Google Scholar] [CrossRef] [PubMed]
- Özdin, S.; Bayrak Özdin, Ş. Levels and predictors of anxiety, depression and health anxiety during COVID-19 pandemic in Turkish society: The importance of gender. Int. J. Soc. Psychiatry 2020, 66, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Russ-Jara, A.L.; Luckhurst, C.L.; Dismore, R.A.; Arthur, K.J.; Ifeachor, A.P.; Militello, L.G.; Glassman, P.A.; Zillich, A.J.; Weiner, M. Care Coordination Strategies and Barriers during Medication Safety Incidents: A Qualitative, Cognitive Task Analysis. J. Gen. Intern. Med. 2021, 36, 2212–2220. [Google Scholar] [CrossRef]
- Luk, A.L.; Yau, A.F.T. Experiences of Public Doctors on Managing Work Difficulties and Maintaining Professional Enthusiasm in Acute General Hospitals: A Qualitative Study. Front. Public Health 2018, 6, 19. [Google Scholar] [CrossRef] [Green Version]
- Karaboga, T.; Erdal, N.; Karaboga, H.A.; Tatoglu, E. Current Psychology (2022)Cite this article Creativity as a mediator between personal accomplishment and task performance: A multigroup analysis based on gender during the COVID-19 pandemic. Curr. Psychol. 2022, 1–13. [Google Scholar] [CrossRef]
- Zhiqiang, M.; Khan, H.S.u.d.; Chughtai, M.S.; Li, M. Re-Engineering the Human Resource Strategies Amid and Post-Pandemic Crisis: Probing into the Moderated Mediation Model of the High-Performance Work Practices and Employee’s Outcomes. Front. Psychol. 2021, 12, 710266. [Google Scholar] [CrossRef]
- Hines, S.E.; Chin, K.H.; Levine, A.R.; Wickwire, E.M. Initiation of a survey of healthcare worker distress and moral injury at the onset of the COVID-19 surge. Am. J. Ind. Med. 2020, 63, 830–833. [Google Scholar] [CrossRef]
- Fumis, R.R.L.; Amarante, G.A.J.; Nascimento, A.d.; Junior, J.M.V. Moral distress and its contribution to the development of burnout syndrome among critical care providers. Ann. Intensive Care 2017, 7, 1–8. [Google Scholar] [CrossRef] [Green Version]
- Barua, L.; Zaman, M.S.; Omi, F.R.; Faruque, M. Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: A cross-sectional study. F1000 Res. 2020, 9, 1304. [Google Scholar] [CrossRef]
- Labrague, L.J.; De Los Santos, J.A.A. COVID-19 anxiety among front-line nurses: Predictive role of organisational support, personal resilience and social support. J. Nurs. Manag. 2020, 28, 1653–1661. [Google Scholar] [CrossRef] [PubMed]
- Chen, Q.; Chen, M.; Zheng, X.; Liu, J. Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 2020, 7, e15–e16. [Google Scholar] [CrossRef]
- Lavoie-Tremblay, M.; Bonin, J.; Lesage, A.D.; Bonneville-Roussy, A.; Lavigne, G.L.; Laroche, D. Contribution of the psychosocial work environment to psychological distress among health care professionals before and during a major organizational change. Health Care Manag. (Frederick) 2010, 29, 293–304. [Google Scholar] [CrossRef]
- Albrecht, T.; Goldsmith, D. Social Support, Social Networks and Health. Teoksessa TL Thompson, AM Dorsey, KI Miller & R. Parrott (toim.) Handbook of Health Communication; Lawrence Erlbaum Associates, Inc.: Mahwah, NJ, USA, 2003. [Google Scholar]
- Lindfors, P.M.; Heponiemi, T.; Meretoja, O.A.; Leino, T.J.; Elovainio, M.J. Mitigating on-call symptoms through organizational justice and job control: A cross-sectional study among Finnish anesthesiologists. Acta Anaesthesiol. Scand. 2009, 53, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Franz, S.; Zeh, A.; Schablon, A.; Kuhnert, S.; Nienhaus, A. Aggression and violence against health care workers in Germany-a cross sectional retrospective survey. BMC Health Serv. Res. 2010, 10, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de Figueiredo, C.S.; Sandre, P.C.; Portugal, L.C.L.; Mázala-de-Oliveira, T.; Chagas, L.d.; Raony, Í.; Ferreira, E.S.; Giestal-de-Araujobg, E.; Santose, A.A.; Bomfimabgh, P.O.-S. COVID-19 pandemic impact on children and adolescents’ mental health: Biological, environmental, and social factors. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110171. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020, 1540. [Google Scholar] [CrossRef]
| Variables | % (n) | |
|---|---|---|
| Sex | Male | 14.78% (n = 51) |
| Female | 85.22% (n = 294) | |
| Education | Middle school | 66.38% (n = 229) |
| High school | 16.23% (n = 56) | |
| University | 7.25% (n = 25) | |
| Doctorate | 10.14% (n = 35) | |
| Job Position | Health staff | 20.00% (n = 69) |
| Nurse | 28.99% (n = 100) | |
| Doctor | 20.58% (n = 71) | |
| Other | 30.43% (n = 105) | |
| Department | ER | 44.93% (n = 155) |
| Inpatient Unit | 24.64% (n = 85) | |
| ICU | 6.38% (n = 22) | |
| Other | 24.06% (n = 83) | |
| Age | HCWs less than <34 years old | 60.29% (n = 208) |
| HCWs more than ≥35 years old | 39.71% (n = 137) | |
| PHQ-9 | Low | 51.88% (n = 179) |
| Moderate | 28.70% (n = 99) | |
| High | 19.42% (n = 67) | |
| Anxiety1 | Low | 8.70% (n = 30) |
| Moderate | 15.65% (n = 54) | |
| High | 75.65% (n = 261) | |
| Anxiety2 | Low | 18.55% (n = 64) |
| Moderate | 26.96% (n = 93) | |
| High | 54.49% (n = 188) | |
| Burnout | Low | 15.07% (n = 52) |
| Moderate | 33.91% (n = 117) | |
| High | 51.01% (n = 176) | |
| Sufficient Information | No | 17.39% (n = 285) |
| Yes | 82.61% (n = 60) | |
| Department Change | No | 59.71% (n = 206) |
| Yes | 40.29% (n = 139) | |
| Applause | No | 41.45% (n = 143) |
| Yes | 58.55% (n = 202) | |
| Motivation | Oath | 10.72% (n = 37) |
| Religious beliefs | 37.39% (n = 129) | |
| Peer support | 21.74% (n = 75) | |
| Family support | 17.97% (n = 62) | |
| Monetary compensation | 12.17% (n = 42) | |
| Variables | Job Is Difficult | Total All | p-Value | ||
|---|---|---|---|---|---|
| No | Yes | ||||
| Sex | Male | 64.71% | 35.29% | 14.78% | 0.507 |
| Female | 69.39% | 30.61% | 85.22% | ||
| Education | Middle school | 65.94% | 34.06% | 66.38% | 0.293 |
| High school | 76.79% | 23.21% | 16.23% | ||
| University | 72.00% | 28.00% | 7.25% | ||
| Doctorate | 71.43% | 28.57% | 10.14% | ||
| Job Position | Health staff | 67.82% | 32.18% | 50.43% | 0.151 |
| Nurse | 62.00% | 38.00% | 28.99% | ||
| Doctor | 80.28% | 19.72% | 20.58% | ||
| Other | 68.67% | 31.33% | 24.06% | ||
| Department | ER | 68.39% | 31.61% | 44.93% | 0.744 |
| Inpatient Unit | 67.06% | 32.94% | 24.64% | ||
| ICU | 77.27% | 22.73% | 6.38% | ||
| Age | Younger population (≤34) | 66.83% | 33.17% | 60.29% | 0.358 |
| Older population (≥35) | 71.53% | 28.47% | 39.71% | ||
| PHQ-9 | Low | 79.89% | 20.11% | 51.88% | 0.00 *** |
| Moderate | 76.77% | 23.23% | 28.70% | ||
| High | 26.87% | 73.13% | 19.42% | ||
| Anxiety1 | Low | 83.33% | 16.67% | 8.70% | 0.01 * |
| Moderate | 75.93% | 24.07% | 15.65% | ||
| High | 65.52% | 34.48% | 75.65% | ||
| Anxiety2 | Low | 85.94% | 14.06% | 18.55% | 0.00 *** |
| Moderate | 80.65% | 19.35% | 26.96% | ||
| High | 56.91% | 43.09% | 54.49% | ||
| Burnout | Low | 90.38% | 9.62% | 15.07% | 0.00 *** |
| Moderate | 80.34% | 19.66% | 33.91% | ||
| High | 54.55% | 45.45% | 51.01% | ||
| Total | 68.70% | 31.30% | NA | ||
| Odds Ratios (OR) | p-Value | ||
|---|---|---|---|
| PHQ-9 | Low | NA | |
| Moderate | 10.8 (5.73–21.22) | 0.00 ** | |
| Severe | 1.04 (0.40–2.69) | 0.93 | |
| Burnout | Low | NA | |
| Moderate | 2.30 (0.88–7.18) | 0.112 | |
| Severe | 7.83 (3.24–23.39) | 0.00 *** | |
| Applause | No | NA | |
| Yes | 0.56 (0.35–0.90) | 0.016 * | |
| Department change | No | NA | |
| Yes | 1.60 (1.00–2.54) | 0.045 * | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Emhan, A.; Elkefi, S.; Asan, O. Predictors of Healthcare Professionals’ Work Difficulty Perception during the COVID-19 Pandemic: Study of Work Environment in a Pandemic Hospital. Int. J. Environ. Res. Public Health 2022, 19, 5174. https://doi.org/10.3390/ijerph19095174
Emhan A, Elkefi S, Asan O. Predictors of Healthcare Professionals’ Work Difficulty Perception during the COVID-19 Pandemic: Study of Work Environment in a Pandemic Hospital. International Journal of Environmental Research and Public Health. 2022; 19(9):5174. https://doi.org/10.3390/ijerph19095174
Chicago/Turabian StyleEmhan, Abdurrahim, Safa Elkefi, and Onur Asan. 2022. "Predictors of Healthcare Professionals’ Work Difficulty Perception during the COVID-19 Pandemic: Study of Work Environment in a Pandemic Hospital" International Journal of Environmental Research and Public Health 19, no. 9: 5174. https://doi.org/10.3390/ijerph19095174
APA StyleEmhan, A., Elkefi, S., & Asan, O. (2022). Predictors of Healthcare Professionals’ Work Difficulty Perception during the COVID-19 Pandemic: Study of Work Environment in a Pandemic Hospital. International Journal of Environmental Research and Public Health, 19(9), 5174. https://doi.org/10.3390/ijerph19095174






