The Acute Impact of the Early Stages of COVID-19 Pandemic in People with Pre-Existing Psychiatric Disorders: A Systematic Review
Abstract
:1. Introduction
2. Methods
2.1. Protocol Search Strategy
2.2. Search Strategy
2.3. Eligibility Criteria
3. Results
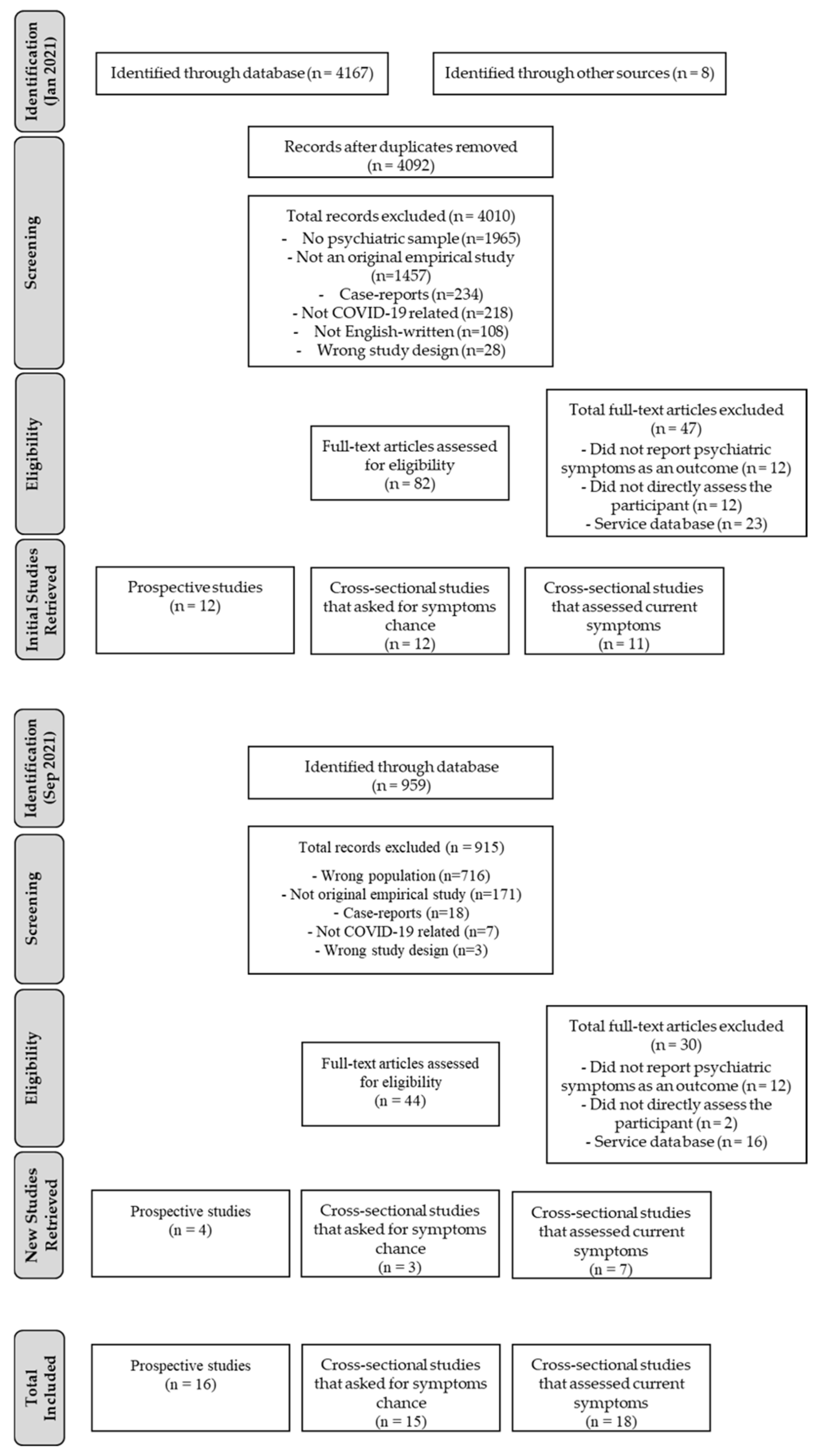
3.1. Study Selection
3.2. General Studies Characteristics
3.2.1. Mood Disorders
3.2.2. Anxiety Disorders
3.2.3. Obsessive Compulsive Disorders
3.2.4. Eating Disorders
3.2.5. Substance Use and Addictive Disorders
3.2.6. Attention-Deficit Hyperactivity Disorder
3.2.7. Schizophrenia Disorder
3.2.8. Tourette Syndrome or Chronic Tic Disorder
3.2.9. Insomnia Disorder
3.2.10. Somatic Symptom Disorder
3.2.11. Global Impact on Multiple Psychiatric Disorders
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ozili, P. COVID-19 in Africa: Socio-economic impact, policy response and opportunities. Int. J. Sociol. Soc. Policy 2022, 42, 177–200. [Google Scholar] [CrossRef]
- Karunathilake, K. Positive and negative impacts of COVID-19, an analysis with special reference to challenges on the supply chain in South Asian countries. J. Soc. Econ. Dev. 2021, 23, 568–581. [Google Scholar] [CrossRef] [PubMed]
- Alifano, M.; Attanasi, G.; Iannelli, F.; Cherikh, F.; Iannelli, A. COVID-19 pandemic: A European perspective on health economic policies. J. Behav. Econ. Policy 2020, 4, 35–43. [Google Scholar]
- Martin, A.; Markhvida, M.; Hallegatte, S.; Walsh, B. Socio-Economic Impacts of COVID-19 on Household Consumption and Poverty. Econ. Disasters Clim. Chang. 2020, 4, 453–479. [Google Scholar] [CrossRef]
- Agyapong, V.I.O.; Hrabok, M.; Vuong, W.; Shalaby, R.; Noble, J.M.; Gusnowski, A.; Mrklas, K.J.; Li, D.; Urichuk, L.; Snaterse, M.; et al. Changes in stress, anxiety, and depression levels of subscribers to a daily supportive text message program (Text4Hope) during the COVID-19 pandemic: Cross-sectional survey study. JMIR Ment. Health 2020, 7, e22423. [Google Scholar] [CrossRef]
- Cousijn, J.; Kuhns, L.; Larsen, H.; Kroon, E. For better or for worse? A pre–post exploration of the impact of the COVID-19 lockdown on cannabis users. Addiction 2020, 116, 2104–2115. [Google Scholar] [CrossRef]
- Ogrodniczuk, J.S.; Rice, S.M.; Kealy, D.; Seidler, Z.E.; Delara, M.; Oliffe, J.L. Psychosocial impact of the COVID-19 pandemic: A cross-sectional study of online help-seeking Canadian men. Postgrad. Med. 2021, 133, 750–759. [Google Scholar] [CrossRef]
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [Green Version]
- Xiong, J.; Lipsitz, O.; Nasri, F.; Lui, L.M.W.; Gill, H.; Phan, L.; Chen-Li, D.; Iacobucci, M.; Ho, R.; Majeed, A.; et al. Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J. Affect. Disord. 2020, 277, 55–64. [Google Scholar] [CrossRef]
- Paulino, M.; Dumas-Diniz, R.; Brissos, S.; Brites, R.; Alho, L.; Simões, M.R.; Silva, C.F. COVID-19 in Portugal: Exploring the immediate psychological impact on the general population. Psychol. Health Med. 2021, 26, 44–55. [Google Scholar] [CrossRef]
- Santabárbara, J.; Lasheras, I.; Lipnicki, D.M.; Bueno-Notivol, J.; Pérez-Moreno, M.; López-Antón, R.; De la Cámara, C.; Lobo, A.; Gracia-García, P. Prevalence of anxiety in the COVID-19 pandemic: An updated meta-analysis of community-based studies. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 109, 110207. [Google Scholar] [CrossRef] [PubMed]
- Davide, P.; Andrea, P.; Martina, O.; Andrea, E.; Davide, D.; Mario, A. The impact of the COVID-19 pandemic on patients with OCD: Effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res. 2020, 291, 113213. [Google Scholar] [CrossRef] [PubMed]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef] [PubMed]
- Kozloff, N.; Mulsant, B.H.; Stergiopoulos, V.; Voineskos, A.N. The COVID-19 global pandemic: Implications for people with schizophrenia and related disorders. Schizophr. Bull. 2020, 46, 752–757. [Google Scholar] [CrossRef]
- Sher, L. The impact of the COVID-19 pandemic on suicide rates. QJM Mon. J. Assoc. Physicians 2020, 113, 707–712. [Google Scholar] [CrossRef] [PubMed]
- Tanir, Y.; Karayagmurlu, A.; Kaya, İ.; Kaynar, T.B.; Türkmen, G.; Dambasan, B.N.; Meral, Y.; Coşkun, M. Exacerbation of obsessive compulsive disorder symptoms in children and adolescents during COVID-19 pandemic. Psychiatry Res. 2020, 293, 113363. [Google Scholar] [CrossRef] [PubMed]
- Smith, M.L.; Gradus, J.L. Psychiatric disorders and risk of infections: Early lessons from COVID-19. Lancet Healthy Longev. 2020, 1, 51–52. [Google Scholar] [CrossRef]
- Attanasi, G.; Maffioletti, A.; Shalukhina, T.; Bel, C.; Cherikh, F. Gender Differences in the Impact of COVID-19 Lockdown on Potentially Addictive Behaviors: An Emotion-Mediated Analysis. Front. Psychol. 2021, 12, 703897. [Google Scholar] [CrossRef]
- Cherikh, F.; Frey, S.; Bel, C.; Attanasi, G.; Alifano, M.; Iannelli, A. Behavioral Food Addiction During Lockdown: Time for Awareness, Time to Prepare the Aftermath. Obes. Surg. 2020, 30, 3585–3587. [Google Scholar] [CrossRef]
- Jacques-Aviñó, C.; López-Jiménez, T.; Medina-Perucha, L.; De Bont, J.; Gonçalves, A.Q.; Duarte-Salles, T.; Berenguera, A. Gender-based approach on the social impact and mental health in Spain during COVID-19 lockdown: A cross-sectional study. BMJ Open 2020, 10, e044617. [Google Scholar] [CrossRef]
- Cummings, J.R.; Ackerman, J.M.; Wolfson, J.A.; Gearhardt, A.N. COVID-19 stress and eating and drinking behaviors in the United States during the early stages of the pandemic. Appetite 2021, 162, 105163. [Google Scholar] [CrossRef] [PubMed]
- Hilty, D.M.; Ferrer, D.C.; Parish, M.B.; Johnston, B.; Callahan, E.J.; Yellowlees, P.M. The effectiveness of telemental health: A 2013 review. Telemed. E-Health 2013, 19, 444–454. [Google Scholar] [CrossRef] [PubMed]
- Langarizadeh, M.; Tabatabaei, M.S.; Tavakol, K.; Naghipour, M.; Rostami, A.; Moghbeli, F. Telemental health care, an effective alternative to conventional mental care: A systematic review. Acta Inform. Med. 2017, 25, 240–246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Byrne, A.; Barber, R.; Lim, C.H. Impact of the COVID-19 pandemic—A mental health service perspective. Prog. Neurol. Psychiatry 2021, 25, 27–33. [Google Scholar] [CrossRef]
- Moher, D.; Hopewell, S.; Schulz, K.F.; Montori, V.; Gøtzsche, P.C.; Devereaux, P.J.; Elbourne, D.; Egger, M.; Altman, D.G.; Group, C.S.o.R.T. CONSORT 2010 Explanation and Elaboration: Updated guidelines for reporting parallel group randomised trials. J. Clin. Epidemiol. 2010, 63, e1–e37. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yocum, A.K.; Zhai, Y.; McInnis, M.G.; Han, P. COVID-19 pandemic and lockdown impacts: A description in a longitudinal study of bipolar disorder. J. Affect. Disord. 2021, 282, 1226–1233. [Google Scholar] [CrossRef]
- Zhang, H.; Xu, H.; Huang, L.; Wang, Y.; Deng, F.; Wang, X.; Tang, X.; Wang, W.; Fu, X.; Tao, Y.; et al. Increased occurrence of PTSD symptoms in adolescents with major depressive disorder soon after the start of the COVID-19 outbreak in China: A cross-sectional survey. BMC Psychiatry 2021, 21, 395. [Google Scholar] [CrossRef]
- Carmassi, C.; Bertelloni, C.A.; Dell’Oste, V.; Barberi, F.M.; Maglio, A.; Buccianelli, B.; Cordone, A.; Dell’Osso, L. Tele-Psychiatry Assessment of Post-traumatic Stress Symptoms in 100 Patients With Bipolar Disorder During the COVID-19 Pandemic Social-Distancing Measures in Italy. Front. Psychiatry 2020, 11, 580736. [Google Scholar] [CrossRef]
- Di Nicola, M.; Dattoli, L.; Moccia, L.; Pepe, M.; Janiri, D.; Fiorillo, A.; Janiri, L.; Sani, G. Serum 25-hydroxyvitamin D levels and psychological distress symptoms in patients with affective disorders during the COVID-19 pandemic. Psychoneuroendocrinology 2020, 122, 104869. [Google Scholar] [CrossRef]
- Franchini, L.; Ragone, N.; Seghi, F.; Barbini, B.; Colombo, C. Mental health services for mood disorder outpatients in Milan during COVID-19 outbreak: The experience of the health care providers at San Raffaele hospital. Psychiatry Res. 2020, 292, 19–22. [Google Scholar] [CrossRef]
- Pinkham, A.E.; Ackerman, R.A.; Depp, C.A.; Harvey, P.D.; Moore, R.C. A Longitudinal Investigation of the Effects of the COVID-19 Pandemic on the Mental Health of Individuals with Pre-existing Severe Mental Illnesses. Psychiatry Res. 2020, 294, 113493. [Google Scholar] [CrossRef] [PubMed]
- Rogers, A.H.; Bogiaizian, D.; Salazar, P.L.; Solari, A.; Garey, L.; Fogle, B.M.; Schmidt, N.B.; Zvolensky, M.J. COVID-19 and Anxiety Sensitivity Across Two Studies in Argentina: Associations with COVID-19 Worry, Symptom Severity, Anxiety, and Functional Impairment. Cogn. Ther. Res. 2021, 45, 697–707. [Google Scholar] [CrossRef] [PubMed]
- Plunkett, R.; Costello, S.; McGovern, M.; McDonald, C.; Hallahan, B. Impact of the COVID-19 pandemic on patients with pre-existing anxiety disorders attending secondary care. Ir. J. Psychol. Med. 2021, 38, 123–131. [Google Scholar] [CrossRef]
- Alonso, P.; Bertolín, S.; Segalàs, J.; Tubío, M.; Real, E.; Mar-Barrutia, L.; Fernández, M.; Carvalho, S.R.; Carracedo, A.; Menchón, J.M. How is COVID-19 Affecting Patients with Obsessive-Compulsive Disorder? A longitudinal study on the initial phase of the pandemic in a Spanish cohort. Eur. Psychiatry 2021, 64, 1–27. [Google Scholar] [CrossRef]
- Hassoulas, A.; Umla-Runge, K.; Zahid, A.; Adams, O.; Green, M.; Hassoulas, A.; Panayiotou, E. Investigating the Association Between Obsessive-Compulsive Disorder Symptom Subtypes and Health Anxiety as Impacted by the COVID-19 Pandemic: A Cross-Sectional Study. Psychol. Rep. 2021. [Google Scholar] [CrossRef]
- Khosravani, V.; Asmundson, G.J.G.; Taylor, S.; Sharifi Bastan, F.; Samimi Ardestani, S.M. The Persian COVID stress scales (Persian-CSS) and COVID-19-related stress reactions in patients with obsessive-compulsive and anxiety disorders. J. Obs.-Compuls. Relat. Disord. 2021, 28, 100615. [Google Scholar] [CrossRef] [PubMed]
- Benatti, B.; Albert, U.; Maina, G.; Fiorillo, A.; Celebre, L.; Girone, N.; Fineberg, N.; Bramante, S.; Rigardetto, S.; Dell’Osso, B. What Happened to Patients With Obsessive Compulsive Disorder During the COVID-19 Pandemic? A Multicentre Report from Tertiary Clinics in Northern Italy. Front. Psychiatry 2020, 11, 720. [Google Scholar] [CrossRef]
- Chakraborty, A.; Karmakar, S. Impact of COVID-19 on obsessive compulsive disorder (OCD). Iran. J. Psychiatry 2020, 15, 256–259. [Google Scholar] [CrossRef]
- Matsunaga, H.; Mukai, K.; Yamanishi, K. The acute impact of COVID-19 pandemic on phenomenological features in fully or partially remitted patients with obsessive–compulsive disorder. Psychiatry Clin. Neurosci. 2020, 74, 74. [Google Scholar] [CrossRef]
- Nissen, J.B.; Højgaard, D.R.M.A.; Thomsen, P.H. The immediate effect of COVID-19 pandemic on children and adolescents with obsessive compulsive disorder. BMC Psychiatry 2020, 20, 511. [Google Scholar] [CrossRef]
- Giel, K.E.; Schurr, M.; Zipfel, S.; Junne, F.; Schag, K. Eating behaviour and symptom trajectories in patients with a history of binge eating disorder during COVID-19 pandemic. Eur. Eat. Disord. Rev. 2021, 29, 657–662. [Google Scholar] [CrossRef] [PubMed]
- Baenas, I.; Caravaca-Sanz, E.; Granero, R.; Sánchez, I.; Riesco, N.; Testa, G.; Vintró-Alcaraz, C.; Treasure, J.; Jiménez-Murcia, S.; Fernández-Aranda, F. COVID-19 and eating disorders during confinement: Analysis of factors associated with resilience and aggravation of symptoms. Eur. Eat. Disord. Rev. 2020, 28, 855–863. [Google Scholar] [CrossRef] [PubMed]
- Castellini, G.; Cassioli, E.; Rossi, E.; Innocenti, M.; Gironi, V.; Sanfilippo, G.; Felciai, F.; Monteleone, A.M.; Ricca, V. The impact of COVID-19 epidemic on eating disorders: A longitudinal observation of pre versus post psychopathological features in a sample of patients with eating disorders and a group of healthy controls. Int. J. Eat. Disord. 2020, 53, 1855–1862. [Google Scholar] [CrossRef] [PubMed]
- Fernández-Aranda, F.; Munguía, L.; Mestre-Bach, G.; Steward, T.; Etxandi, M.; Baenas, I.; Granero, R.; Sánchez, I.; Ortega, E.; Andreu, A.; et al. COVID Isolation Eating Scale (CIES): Analysis of the impact of confinement in eating disorders and obesity—A collaborative international study. Eur. Eat. Disord. Rev. 2020, 28, 871–883. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, S.; Maier, J.; Meule, A.; Voderholzer, U. Eating disorders in times of the COVID-19 pandemic—Results from an online survey of patients with anorexia nervosa. Int. J. Eat. Disord. 2020, 53, 1791–1800. [Google Scholar] [CrossRef] [PubMed]
- Schlegl, S.; Meule, A.; Favreau, M.; Voderholzer, U. Bulimia nervosa in times of the COVID-19 pandemic—Results from an online survey of former inpatients. Eur. Eat. Disord. Rev. 2020, 28, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Blithikioti, C.; Nuño, L.; Paniello, B.; Gual, A.; Miquel, L. Impact of COVID-19 lockdown on individuals under treatment for substance use disorders: Risk factors for adverse mental health outcomes. J. Psychiatr. Res. 2021, 139, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Chappuy, M.; Peyrat, M.; Lejeune, O.; Duvernay, N.; David, B.; Joubert, P.; Lack, P. Drug consumption during prolonged lockdown due to COVID-19 as observed in French addiction center. Therapies 2021, 76, 361–382. [Google Scholar] [CrossRef]
- Bar-Or, R.L.; Shalit, N.; Shpitzer, R.; Kor, A.; Lev-Ran, S. Self-reported changes in use of addictive substances and behaviors among patients. Isr. Med. Assoc. J. 2021, 23, 11. [Google Scholar]
- Martinotti, G.; Alessi, M.C.; Di Natale, C.; Sociali, A.; Ceci, F.; Lucidi, L.; Picutti, E.; Di Carlo, F.; Corbo, M.; Vellante, F.; et al. Psychopathological Burden and Quality of Life in Substance Users During the COVID-19 Lockdown Period in Italy. Front. Psychiatry 2020, 11, 896. [Google Scholar] [CrossRef]
- Yazdi, K.; Fuchs-Leitner, I.; Rosenleitner, J.; Gerstgrasser, N.W. Impact of the COVID-19 Pandemic on Patients With Alcohol Use Disorder and Associated Risk Factors for Relapse. Front. Psychiatry 2020, 11, 1470. [Google Scholar] [CrossRef] [PubMed]
- Becker, S.P.; Breaux, R.; Cusick, C.N.; Dvorsky, M.R.; Marsh, N.P.; Sciberras, E.; Langberg, J.M. Remote Learning During COVID-19: Examining School Practices, Service Continuation, and Difficulties for Adolescents With and Without Attention-Deficit/Hyperactivity Disorder. J. Adolesc. Health 2020, 67, 769–777. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.; Hua, T.; Zeng, K.; Zhong, B.; Wang, G.; Liu, X. Influence of social isolation caused by coronavirus disease 2019 (COVID-19) on the psychological characteristics of hospitalized schizophrenia patients: A case-control study. Transl. Psychiatry 2020, 10, 411. [Google Scholar] [CrossRef] [PubMed]
- Mataix-Cols, D.; Ringberg, H.; Fernández de la Cruz, L. Perceived Worsening of Tics in Adult Patients with Tourette Syndrome after the COVID-19 Outbreak. Mov. Disord. Clin. Pract. 2020, 7, 725–726. [Google Scholar] [CrossRef] [PubMed]
- Cheng, P.; Casement, M.D.; Kalmbach, D.A.; Castelan, A.C.; Drake, C.L. Digital cognitive behavioral therapy for insomnia promotes later health resilience during the coronavirus disease 19 (COVID-19) pandemic. Sleep 2021, 44, zsaa258. [Google Scholar] [CrossRef]
- De Nardi, L.; Abbracciavento, G.; Cozzi, G.; Ronfani, L.; Viola, I.; Bigolin, L.; Barbi, E.; Trombetta, A. Adolescents with somatic symptom disorder experienced less anxiety and depression than healthy peers during the first COVID-19 lockdown. Acta Paediatr. Int. J. Paediatr. 2021, 110, 2385–2386. [Google Scholar] [CrossRef]
- Favreau, M.; Hillert, A.; Osen, B.; Gärtner, T.; Hunatschek, S.; Riese, M.; Hewera, K.; Voderholzer, U. Psychological consequences and differential impact of the COVID-19 pandemic in patients with mental disorders. Psychiatry Res. 2021, 302, 114045. [Google Scholar] [CrossRef]
- Imai, H.; Furukawa, T.A. Psychological Impact of Masks and Infection-Prevention Plastic Partitions on Anxiety for Infection and Patient-Doctor Relationships During the COVID-19 Pandemic. Prim. Care Companion CNS Disord. 2021, 23, 35186. [Google Scholar] [CrossRef]
- Mergel, E.; Schützwohl, M. A longitudinal study on the COVID-19 pandemic and its divergent effects on social participation and mental health across different study groups with and without mental disorders. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1459–1468. [Google Scholar] [CrossRef]
- Ting, T.C.M.; Wong, A.W.S.; Liu, W.S.; Leung, F.L.T.; Ng, M.T. Impact of COVID-19 outbreak on posttraumatic stress in patients with psychiatric illness. Psychiatry Res. 2021, 303, 114065. [Google Scholar] [CrossRef]
- Tundo, A.; Betro’, S.; Necci, R. What is the impact of COVID-19 pandemic on patients with pre-existing mood or anxiety disorder? An observational prospective study. Medicine 2021, 57, 304. [Google Scholar] [CrossRef]
- Vissink, C.E.; van Hell, H.H.; Galenkamp, N.; van Rossum, I.W. The effects of the COVID-19 outbreak and measures in patients with a pre-existing psychiatric diagnosis: A cross-sectional study. J. Affect. Disord. Rep. 2021, 4, 100102. [Google Scholar] [CrossRef] [PubMed]
- Burrai, J.; Roma, P.; Barchielli, B.; Biondi, S.; Cordellieri, P.; Fraschetti, A.; Pizzimenti, A.; Mazza, C.; Ferracuti, S.; Giannini, A.M. Psychological and Emotional Impact of Patients Living in Psychiatric Treatment Communities during COVID-19 Lockdown in Italy. J. Clin. Med. 2020, 9, 3787. [Google Scholar] [CrossRef] [PubMed]
- Chang, K.-C.; Strong, C.; Pakpour, A.H.; Griffiths, M.D.; Lin, C.-Y. Factors related to preventive COVID-19 infection behaviors among people with mental illness. J. Formos. Med. Assoc. 2020, 119, 1772–1780. [Google Scholar] [CrossRef] [PubMed]
- Hao, F.; Tan, W.; Jiang, L.; Zhang, L.; Zhao, X.; Zou, Y.; Hu, Y.; Luo, X.; Jiang, X.; McIntyre, R.S.; et al. Do psychiatric patients experience more psychiatric symptoms during COVID-19 pandemic and lockdown? A case-control study with service and research implications for immunopsychiatry. Brain Behav. Immun. 2020, 87, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Iasevoli, F.; Fornaro, M.; D’Urso, G.; Galletta, D.; Casella, C.; Paternoster, M.; Buccelli, C.; Bartolomeis, A.d. Psychological distress in patients with serious mental illness during the COVID-19 outbreak and one-month mass quarantine in Italy. Psychol. Med. 2020, 51, 1054–1056. [Google Scholar] [CrossRef]
- Marchitelli, S.; Mazza, C.; Lenzi, A.; Ricci, E.; Gnessi, L.; Roma, P. Weight gain in a sample of patients affected by overweight/obesity with and without a psychiatric diagnosis during the COVID-19 lockdown. Nutrients 2020, 12, 3525. [Google Scholar] [CrossRef]
- Muruganandam, P.; Neelamegam, S.; Menon, V.; Alexander, J. COVID-19 and Severe Mental Illness: Impact on patients and its relation with their awareness about COVID-19 Partheeban. Psychiatry Res. 2020, 291, 113265. [Google Scholar] [CrossRef]
- Pan, K.Y.; Kok, A.A.L.; Eikelenboom, M.; Horsfall, M.; Jörg, F.; Luteijn, R.A.; Rhebergen, D.; Oppen, P.v.; Giltay, E.J.; Penninx, B.W.J.H. The mental health impact of the COVID-19 pandemic on people with and without depressive, anxiety, or obsessive-compulsive disorders: A longitudinal study of three Dutch case-control cohorts. Lancet Psychiatry 2021, 8, 121–129. [Google Scholar] [CrossRef]
- Porcellana, M.; Morganti, C.; Boccalari, L.; Limosani, I.; Manzo, V.; Zerbinati, L.; Corradin, M.; Moreno, M.; Percudani, M. The impact of the COVID-19 emergency in a community mental health setting of a metropolitan hospital. J. Psychopathol. 2020, 26, 134–140. [Google Scholar] [CrossRef]
- Zou, S.; Liu, Z.H.; Yan, X.; Wang, H.; Li, Y.; Xu, X.; Du, X.; Zhang, L.; Zhang, Q.; Jackson, T.; et al. Prevalence and correlates of fatigue and its association with quality of life among clinically stable older psychiatric patients during the COVID-19 outbreak: A cross-sectional study. Glob. Health 2020, 16, 119. [Google Scholar] [CrossRef] [PubMed]
- Bridgland, V.M.E.; Moeck, E.K.; Green, D.M.; Swain, T.L.; Nayda, D.M.; Matson, L.A.; Hutchison, N.P.; Takarangi, M.K.T. Why the COVID-19 pandemic is a traumatic stressor. PLoS ONE 2021, 16, e0240146. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Paluszek, M.M.; Landry, C.A.; Rachor, G.S.; McKay, D.; Taylor, S. Do pre-existing anxiety-related and mood disorders differentially impact COVID-19 stress responses and coping? J. Anxiety Disord. J. 2020, 74, 102271. [Google Scholar] [CrossRef] [PubMed]
- Neelam, K.; Duddu, V.; Anyim, N.; Neelam, J.; Lewis, S. Pandemics and pre-existing mental illness: A systematic review and meta-analysis. Brain Behav. Immun. Health 2020, 10, 100177. [Google Scholar] [CrossRef]
- Rheenen, T.E.V.; Meyer, D.; Neill, E.; Phillipou, A.; Tan, E.J.; Toh, W.L.A.; Rossell, S.L. Mental health status of individuals with a mood-disorder during the COVID-19 pandemic in Australia: Initial results from the COLLATE project. J. Affect. Disord. 2020, 275, 69–77. [Google Scholar] [CrossRef]
- Mclaughlin, K.A.; Hatzenbuehler, M.L. Mechanisms Linking Stressful Life Events and Mental Health Problems in a Prospective, Community-Based Sample of Adolescents. J. Adolesc. Health 2009, 44, 153–160. [Google Scholar] [CrossRef] [Green Version]
- Łosiak, W.; Blaut, A.; Kłosowska, J.; Łosiak-Pilch, J. Stressful Life Events, Cognitive Biases, and Symptoms of Depression in Young Adults. Front. Psychol. 2019, 10, 2165. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. COVID stress syndrome: Concept, structure, and correlates. Depress. Anxiety 2020, 37, 706–714. [Google Scholar] [CrossRef]
- Taylor, S.; Landry, C.A.; Paluszek, M.M.; Fergus, T.A.; McKay, D.; Asmundson, G.J.G. Development and initial validation of the COVID Stress Scales. J. Anxiety Disord. 2020, 72, 102232. [Google Scholar] [CrossRef]
- Zaccari, V.; D’Arienzo, M.C.; Caiazzo, T.; Magno, A.; Amico, G.; Mancini, F. Narrative Review of COVID-19 Impact on Obsessive-Compulsive Disorder in Child, Adolescent and Adult Clinical Populations. Front. Psychiatry 2021, 12, 673161. [Google Scholar] [CrossRef]
- Cunning, C.; Hodes, M. The COVID-19 pandemic and obsessive–compulsive disorder in young people: Systematic review. Clin. Child Psychol. Psychiatry 2021, 27, 18–34. [Google Scholar] [CrossRef] [PubMed]
- Sideli, L.; Lo Coco, G.; Bonfanti, R.C.; Borsarini, B.; Fortunato, L.; Sechi, C.; Micali, N. Effects of COVID-19 lockdown on eating disorders and obesity: A systematic review and meta-analysis. Eur. Eat. Disord. Rev. 2021, 29, 826–841. [Google Scholar] [CrossRef] [PubMed]
- Jemberie, W.B.; Stewart Williams, J.; Eriksson, M.; Grönlund, A.S.; Ng, N.; Blom Nilsson, M.; Padyab, M.; Priest, K.C.; Sandlund, M.; Snellman, F.; et al. Substance Use Disorders and COVID-19: Multi-Faceted Problems Which Require Multi-Pronged Solutions. Front. Psychiatry 2020, 11, 714. [Google Scholar] [CrossRef]
- Mallet, J.; Dubertret, C.; Strat, Y.L. Addictions in the COVID-19 era: Current evidence, future perspectives a comprehensive review. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2021, 106, 110070. [Google Scholar] [CrossRef] [PubMed]
- Munro, A.; Booth, H.; Gray, N.M.; Love, J.; Mohan, A.R.M.; Tang, J.; Macgillivray, S. Understanding the impacts of novel coronavirus outbreaks on people who use drugs: A systematic review to inform practice and drug policy responses to COVID-19. Int. J. Environ. Res. Public Health 2021, 18, 8470. [Google Scholar] [CrossRef]
- Tsamakis, K.; Tsiptsios, D.; Ouranidis, A.; Mueller, C.; Schizas, D.; Terniotis, C.; Nikolakakis, N.; Tyros, G.; Kympouropoulos, S.; Lazaris, A.; et al. COVID-19 and its consequences on mental health (Review). Exp. Ther. Med. 2021, 21, 1. [Google Scholar] [CrossRef] [PubMed]
- Murphy, L.; Markey, K.; O’ Donnell, C.; Moloney, M.; Doody, O. The impact of the COVID-19 pandemic and its related restrictions on people with pre-existent mental health conditions: A scoping review. Arch. Psychiatr. Nurs. 2021, 35, 375–394. [Google Scholar] [CrossRef]
- Barber, S.; Reed, L.; Syam, N.; Jones, N. Severe Mental Illness and Risks from COVID-19. Available online: https://www.cebm.net/covid-19/severe-mental-illness-and-risks-from-covid-19/ (accessed on 2 September 2021).
- Pignon, B.; Gourevitch, R.; Tebeka, S.; Dubertret, C.; Cardot, H.; Dauriac-Le Masson, V.; Trebalag, A.K.; Barruel, D.; Yon, L.; Hemery, F.; et al. Dramatic reduction of psychiatric emergency consultations during lockdown linked to COVID-19 in Paris and suburbs. Psychiatry Clin. Neurosci. 2020, 74, 557–559. [Google Scholar] [CrossRef]
- Capuzzi, E.; Brita, C.D.; Caldiroli, A.; Colmegna, F.; Nava, R.; Buoli, M.; Clerici, M. Psychiatric emergency care during Coronavirus 2019 (COVID 19) pandemic lockdown: Results from a Department of Mental Health and Addiction of northern Italy. Psychiatry Res. J. 2020, 293, 113463. [Google Scholar] [CrossRef]
- Rodriguez-Jimenez, R.; Rentero, D.; Romero-Ferreiro, V.; García-Fernández, L. Impact of outbreak COVID-19 pandemic on psychiatry emergencies in Spain. Psychiatry Res. 2020, 295, 113581. [Google Scholar] [CrossRef]
- Murphy, S.M.; Yoder, J.; Pathak, J.; Avery, J. Healthcare utilization patterns among persons who use drugs during the COVID-19 pandemic Sean. J. Subst. Abus. Treat. 2021, 121, 108177. [Google Scholar] [CrossRef] [PubMed]
- Yang, J.; Beth, M.; Zhou, L.; Busch, A.B. Disparities in outpatient visits for mental health and/or substance use disorders during the COVID surge and partial reopening in Massachusetts. Gen. Hosp. Psychiatry 2020, 67, 100–106. [Google Scholar] [CrossRef] [PubMed]
- Türkoğlu, S.; Uçar, H.N.; Çetin, F.H.; Güler, H.A.; Tezcan, M.E. The relationship between chronotype, sleep, and autism symptom severity in children with ASD in COVID-19 home confinement period. Chronobiol. Int. 2020, 37, 1207–1213. [Google Scholar] [CrossRef] [PubMed]
| First Author (Year) | Study Categorization | Sample n (Mean Age (% Women)) | Healthcare Information |
|---|---|---|---|
| Mood Disorders | |||
| Yocum et al. (2021) [26] | Prospective | - BD: 345 (nr (nr)) - WDC: 68 ( nr (nr)) - Healthy controls: 147 (nr (nr)) | - Participants admitted as outpatient or inpatient in clinical services |
| Zhang et al. (2021) [27] | Cross-sectional (current symptoms) | - MDD group: 90 (15 (80)) - Control group: 107 (15 (77)) | - Outpatients - Psychopharmacological treatment |
| Carmassi et al. (2020) [28] | Cross-sectional (current symptoms) | - BD, PTSS: 17 (nr (88)) - BD, No-PTSS: 83 (nr (59)) | - Online/telephone intervention - Psychopharmacological treatment |
| Di Nicola et al. (2020) [29] | Prospective | - No psychological distress: 29 (43 (48)); - Mild psychological distress: 35 (45 (51)); - Moderate to severe psychological distress: 48 (51 (58)) | - Psychopharmacological treatment. |
| Franchini et al. (2020) [30] | Cross-sectional (current symptoms) | - Euthymic MD: 101 (62 (65)) | - Online/telephone intervention |
| Pinkham et al. (2020) [31] | Prospective | - SPD: 92 (43 (54)) - MD: 56 (41 (71)) | - Outpatients |
| Anxiety Disorders | |||
| Rogers et al. (2021) [32] | Cross-sectional (current symptoms) | - AD: 99 (35 (67)) | - Treatment-seeking patients |
| Plunkett et al. (2020) [33] | Prospective | - AD: 30 (39 (60)) | - Outpatients |
| Obsessive-Compulsive Disorders | |||
| Alonso et al. (2021) [34] | Prospective | - OCD:127 (42 (54)) - Healthy controls: 237 (41 (58)) | - Outpatients |
| Hassoulas et al. (2021) [35] | Cross-sectional (changes) | - OCD: 254 (nr (nr)) | NA |
| Khosravani et al. (2021) [36] | Cross-sectional (changes) | - OCD: 300 (36 (59)) - AD: 310 (36 (60)) | - Treatment-seeking patients |
| Benatti et al. (2020) [37] | Cross-sectional (changes) | - OCD, worsening: 44 (40 (46)) - OCD, not worsening: 79 (40 (44)) | - Outpatients |
| Chakraborty et al. (2020) [38] | Cross-sectional (changes) | - OCD: 84 (nr (76)) | - Outpatients - Pharmacological treatment |
| Davide et al. (2020) [12] | Prospective | - OCD: 30 (43 (53)) | - Psychopharmacological treatment |
| Matsunaga et al. (2020) [39] | Prospective | - OCD: 60 (42 (58)) | - Outpatients |
| Nissen et al. (2020) [40] | Cross-sectional (changes) | - OCD clinical group: 65 (15 (63)) - Survey group: 37 (14 (67)) | - Outpatients - Psychotherapy treatment - Pharmacological treatment |
| Tanir et al. (2020) [16] | Cross-sectional (changes) | - OCD: 61 (14 (44)) | - Outpatients - Psychotherapy treatment (CBT) - Pharmacological treatment |
| Eating Disorders | |||
| Giel et al. (2021) [41] | Prospective | - ED: 23 (nr (nr)) - Healthy controls: 19 (nr (nr)) | - Outpatients - Psychotherapy treatment (CBT) |
| Baenas et al. (2020) [42] | Prospective | - ED, worse: 19 (33 (nr)) - ED, non-worse: 55 (32 (nr)) | - Outpatients |
| Castellini et al. (2020) [43] | Prospective | - ED: 74 (32 (100)) - Healthy controls: 97 (31 (100)) | - Outpatients - Psychotherapy treatment (CBT) |
| Fernández-Aranda et al. (2020) [44] | Cross-sectional (changes) | - AN: 55 (24 (89)) - BN: 18 (31 (94)) - OSFED: 14 (37 (86)) - Obesity: 34 (49 (77)) | - Pre-pandemic: outpatients - During pandemic: Online/telephone intervention |
| Schlegl et al. (2020) [45] | Cross-sectional (changes) | - Adults with AN: 112 (25 (100)) - Adolescents with AN: 47 (16 (100)) | - Outpatient, inpatient and online/telephone intervention |
| Schlegl et al. (2020) [46] | Cross-sectional (changes) | - Inpatients with BN: 55 (24 (nr)) | - Pharmacological treatment - Online/telephone intervention |
| Substance-related disorders | |||
| Blithikioti et al. (2021) [47] | Prospective | - SUD: 303 (49 (37)) | - Outpatients |
| Chappuy et al. (2021) [48] | Cross-sectional(changes) | - SUD: 219(43 (22)) | - Outpatients |
| Lev Bar-Or et al. (2021) [49] | Cross-sectional (changes) | - SUD: 92 (40 (38)) | - Outpatients |
| Cousijn et al. (2020) [6] | Prospective | - Daily cannabis users: 120 (18–46 (nr)) - non-using controls: 63 (18–31 (nr)) | NA |
| Martinotti et al. (2020) [50] | Cross-sectional (current symptoms) | - SUD inpatients: 56 (nr (nr)) - SUD outpatients: 97 (nr (nr)) | - Outpatients. - Inpatients - Pharmacological treatment |
| Yazdi et al. (2020) [51] | Cross-sectional (current symptoms) | - Abstinent: 37 (51 (35)) - Consuming: 49 (48 (37)) - Relapsed: 41 (49 (27) | - Outpatient |
| Attention Deficit Hyperactivity Disorder | |||
| Becker et al. (2020) [52] | Cross-sectional (current symptoms) | - ADHD: 118 (17 (35)) - Healthy controls: 120 (17 (46)) | - Pharmacological treatment |
| Schizophrenia or Other Psychotic Disorder | |||
| Ma et al. (2020) [53] | Prospective | - Isolated patients: 30 (43 (60)); - Non-isolated patients: 30 (45 (50)) | - Inpatients |
| Tourette Syndrome/Chronic Tic Disorder | |||
| Mataix-Cols et al. (2020) [54] | Cross-sectional (changes) | - TS/CTD: 178 (31 (57)) | NA |
| Insomnia Disorder | |||
| Cheng et al. (2021) [55] | Cross-sectional (current symptoms) | - dCBT-I group: 102 (45 (73)) - Control group: 106 (45 (84)) | - Online psychotherapy treatment (CBT) |
| Somatic Symptom Disorder | |||
| De Nardi et al. (2021) [56] | Cross-sectional (current symptoms) | - SSD group: 58 (15 (52)) - Control group: 57 (16 (46)) | - Outpatients |
| Multiple Psychiatric Disorders | |||
| Favreau et al. (2021) [57] | Cross-sectional (changes) | - GPP: 538 (70 (36)) | - Inpatients |
| Imai et al. (2021) [58] | Cross-sectional (changes) | - GPP: 425 (53 (53)) | - Outpatients |
| Mergel et al. (2021) [59] | Prospective | - CMD: 25–27 (50 (48)) - AMD: 29–30 (44 (60)) - WMD: 46–49 (41 (76)) | - Outpatients - Psychiatric treatment - Psychotherapeutic treatment |
| Ting et al. (2021) [60] | Cross-sectional (changes) | - GPP: 193 (16–20 (7.3); 21–30 (14.5) 31–40 (21.2); 41–50 (21.2); 51–60 (23.8); 61–70 (10.4); >70 (1.6) (72)) | - Outpatients |
| Tundo et al. (2021) [61] | Prospective (observational) | - No relapse/worsening: 365 (52 (59)) - Relapse/worsening: 21 (48 (67)) | - Outpatients - Pharmacological treatment |
| Vissink et al. (2021) [62] | Cross-sectional (changes) | - GPP: 189 (40 (46)) | - Outpatients |
| Burrai et al. (2020) [63] | Cross-sectional (current symptoms) | - GPP: 77 (47 (34)) - Healthy controls: 100 (46 (50)) | - Inpatients |
| Chang et al. (2020) [64] | Cross-sectional (current symptoms) | - GPP: 414 (46 (44)) | - Inpatients - Outpatients |
| Hao et al. (2020) [65] | Cross-sectional (current symptoms) | - Psychiatric patients: 76 (33 (37)) - Healthy controls: 109 (33 (62)) | - Outpatients |
| Iasevoli et al. (2020) [66] | Cross-sectional (current symptoms) | - GPP: 205 (nr (nr)) - Caregivers: 51 (nr (nr)) - Controls: 205 (nr (nr)) | - Outpatients |
| Marchitelli et al. (2020) [67] | Prospective | - Patients with psychiatric diagnosis: 47 (46 (77)) - Patients without psychiatric diagnosis: 63 (47 (67)) | - Psychotherapy treatment - Pharmacological treatment |
| Muruganandam et al. (2020) [68] | Cross-sectional (changes) | - SMI outpatients: 132 (34 (52)) | - Outpatients |
| Pan et al. (2020) [69] | Prospective | - With psychiatric disorder: 1181 (56 (67)) - Without psychiatric disorder: 336 (58 (55)) | - Outpatients |
| Porcellana et al. (2020) [70] | Cross-sectional (current symptoms) | - GPP: 140 (50 (55)) | - Treatment-seeking patients |
| Zou et al. (2020) [71] | Cross-sectional (current symptoms) | - Fatigue: 501 (62 (69)) - No fatigue: 562 (63 (66)) | - Outpatients |
| Study ID | Country | Previous Assessments | Data Collection Method | 2020 | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | ||||
| Mood Disorders | |||||||||||||||
| Yocum et al. (2021) [26] | United States | None | - Online | o | o | ||||||||||
| Zhang et al. (2021) [27] | China | 2019 | - Telephone/Online | o | |||||||||||
| Carmassi et al. (2020) [28] | Italy | None | - Online | o | |||||||||||
| Di Nicola et al. (2020) [29] | Italy | Dec 2019 | - Online | o | o | o | |||||||||
| Franchini et al. (2020) [30] | Italy | None | - Telephone | o | o | ||||||||||
| Pinkham et al. (2020) [31] | United States | 2018 | - T0: Face-to-face/T1: Telephone | o | o | o | |||||||||
| Anxiety Disorders | |||||||||||||||
| Rogers et al. (2021) [32] | Spain | None | - Online | o | |||||||||||
| Plunkett et al. (2020) [33] | Ireland | None | - Telephone/Face-to-face | o | o | ||||||||||
| Obsessive Compulsive Disorders | |||||||||||||||
| Alonso et al. (2021) [34] | Spain | None | - Telephone/Online | o | o | ||||||||||
| Hassoulas et al. (2021) [35] | United Kingdom | None | - Online | o | o | o | o | ||||||||
| Khosravani et al. (2021) [36] | Iran | None | - Face-to-face/Telephone/Online | o | o | o | |||||||||
| Benatti et al. (2020) [37] | Italy | None | - Telephone/Face-to-face | ||||||||||||
| Chakraborty et al. (2020) [38] | India | None | - Telephone | o | o | ||||||||||
| Davide et al. (2020) [12] | Italy | None | - Face-to-face | o | o | o | |||||||||
| Matsunaga et al. (2020) [39] | Japan | None | - Face-to-face | o | o | ||||||||||
| Nissen et al. (2020) [40] | Denmark | None | - Online | o | o | ||||||||||
| Tanir et al. (2020) [16] | Turkey | None | - Telephone/Online | o | o | ||||||||||
| Eating Disorders | |||||||||||||||
| Giel et al. (2021) [41] | Germany | 2017 | - Telephone/Online | o | o | o | |||||||||
| Baenas et al. (2020) [42] | Spain | None | - T0: Face-to-face/T1: Telephone | o | |||||||||||
| Castellini et al. (2020) [43] | Italy | Dec 2019 | - T0: Face-to-face/T1, T2: Online | o | o | o | o | o | |||||||
| Fernández-Aranda et al. (2020) [44] | Spain | None | - Online | o | o | ||||||||||
| Schlegl et al. (2020) [45] | Germany | None | - Online | o | |||||||||||
| Schlegl et al. (2020) [46] | Germany | None | - Online | o | |||||||||||
| Substance-related disorders | |||||||||||||||
| Blithikioti et al. (2021) [47] | Spain | 2019 | - Online | o | o | ||||||||||
| Chappuy et al. (2021) [48] | French | None | - Face-to-face | o | o | ||||||||||
| Lev Bar-Or et al. (2021) [49] | Israel | None | - Face-to-face | o | |||||||||||
| Cousijn et al. (2020) [6] | Netherlands | 2019 | - Online | o | o | o | o | o | |||||||
| Martinotti et al. (2020) [50] | Italy | None | - Face-to-face/Online | o | o | o | |||||||||
| Yazdi et al. (2020) [51] | Austria | None | - Face-to-face | o | o | o | |||||||||
| Attention-Deficit Hyperactivity Disorder | |||||||||||||||
| Becker et al. (2020) [52] | United States | None | - Online | o | o | ||||||||||
| Schizophrenia or Other Psychotic Disorder | |||||||||||||||
| Ma et al. (2020) [53] | China | None | - Face-to-face | o | o | ||||||||||
| Tourette Syndrome or Chronic Tic Disorder | |||||||||||||||
| Mataix-Cols et al. (2020) [54] | Europe/North America | None | - Online | o | o | ||||||||||
| Insomnia Disorder | |||||||||||||||
| Cheng et al. (2021) [55] | United States | 2016, 1017 | - Online | o | |||||||||||
| Somatic Symptom Disorder | |||||||||||||||
| De Nardi et al. (2021) [56] | Italy | None | - Online | o | o | ||||||||||
| Global impact on multiple psychiatric disorders | |||||||||||||||
| Favreau et al. (2021) [57] | Germany | None | - Online | o | o | o | o | o | o | o | o | o | |||
| Imai et al. (2021) [58] | Japan | None | - Face-to-face | o | o | o | o | o | |||||||
| Mergel et al. (2021) [59] | Germany | 2019 | - Face-to-face | o | o | o | |||||||||
| Ting et al. (2021) [60] | China | None | - Online | o | o | ||||||||||
| Tundo et al. (2021) [61] | Italy | None | - Face-to-face/Online | o | o | o | o | ||||||||
| Vissink et al. (2021) [62] | Netherlands | None | - Online/face-to-face | o | o | o | o | o | |||||||
| Burrai et al. (2020) [63] | Italy | None | - Online | o | o | ||||||||||
| Chang et al. (2020) [64] | Taiwan | None | - Face-to-face | o | o | o | o | ||||||||
| Hao et al. (2020) [65] | China | None | - Online | o | |||||||||||
| Iasevoli et al. (2020) [66] | Italy | None | - Telephone | o | |||||||||||
| Marchitelli et al. (2020) [67] | Italy | None | - Online | o | o | ||||||||||
| Muruganandam et al. (2020) [68] | India | 2019 | - Telephone | o | o | o | |||||||||
| Pan et al. (2020) [69] | Netherlands | 2006, 2008, 2010, 2012, 2014 | - Online | o | o | ||||||||||
| Porcellana et al. (2020) [70] | Italy | None | - Face-to-face | o | |||||||||||
| Zou et al. (2020) [71] | China | None | - Face-to-face | o | o | o | |||||||||
| First Author (Year) | Aim | Assessment Instruments during Pandemic and/or Lockdown | Main Results |
|---|---|---|---|
| Mood Disorders | |||
| Yocum et al. (2021) [26] | To evaluate the impact of the COVID-19 pandemic and lockdown on individuals with BD, as compared to healthy controls. | Pandemic and lockdown: CIS; GAD-7; PHQ-9; PSQI. | - Both BD patients and heathy controls reported a negative impact of lockdown measures. - Over time, healthy controls recover more rapidly and with greater magnitude than people with BD. - Greater negative impact on mood symptoms on healthy controls. |
| Zhang et al. (2021) [27] | To evaluate the impact of the COVID-19 outbreak at 1 month after the start on the mental health of adolescents with or without MDD. | Pandemic: BDI-II; CRIES-13. | - Adolescents with MDD were more likely than those without MDD to experience severe psychological stress and symptoms of PTSD. |
| Carmassi et al. (2020) [28] | To investigate acute PTSS symptoms in patients with BD in a telepsychiatry service. | Lockdown: GAD-7; HAM-D; IES-R; YMRS. | - PTSS and moderate to severe depressive symptoms were reported by 17% of the patients, while severe anxiety was reported by 26%. - Acute manic symptoms may exert a protective function. |
| Di Nicola et al. (2020) [29] | To investigate the effects of lockdown on psychological distress perceived in people with MDD and BD. To assess the usefulness of serum 25(OH)D levels as a predictor of distress severity. | Lockdown: clinical interview; K10; biological data: serum 25(OH)D levels. | - A total of 74% perceived a form of psychological distress at the time of the study; 26% reported no likelihood of psychological distress; 31% displayed mild psychological distress; and 43% displayed moderate to severe psychological distress. |
| Franchini et al. (2020) [30] | To describe the telephone-based mental illness surveillance on euthymic MD patients to evaluate reactions to lockdown measures. | Lockdown: physical conditions; psychiatric conditions: emotional stressors and unpleasant experiences during the lockdown. | - The main concerns were frustration due to restrictions (76%); fears about infection (54%); financial concerns (46%); anxiety (45%); and low mood (41%). Moreover, about 30% of the participants reported somatization, increased alertness, and insomnia. - A total of 21% of the patients were self-medicated with sedatives, and 3% of the patients reported inadequate supplies. |
| Anxiety disorders | |||
| Rogers et al. (2021) [32] | To examine the association between anxiety sensitivity with COVID-19 worry, functional impairment, and symptom severity in a community sample as compared to people with anxiety disorders. | Pandemic: ASI-3; COVID-19 screening. and symptoms; COVID-19 worry index; COVID-19 functional impairment; COVID-19 anxiety; severity of COVID-19 symptoms. | - Increased anxiety sensitivity was significantly associated with increased COVID-19-related worry, anxiety, functional impairment, and symptom severity. |
| Plunkett et al. (2020) [33] | To examine the impact of social restrictions on people with AD. | Lockdown: BAI; HAMA; CGI-I; CGI-S; GAF; Y-BOCS. | - A total of 50% of the participants described a deleterious effect of the COVID-19 pandemic on their mental health; 40% described a deleterious effect pertaining to their levels of anxiety. - Clinician-rated data revealed that 27% of the participants had worsened mental health prior to COVID-19 restrictions; 47% of the participants demonstrated an improvement in their mental health prior to COVID-19 restrictions. |
| Obsessive compulsive disorders | |||
| Alonso et al. (2021) [34] | To investigate the impact of the COVID-19 pandemic on individuals with OCD, as compared to a community sample at an early stage of the pandemic. | Pandemic: clinical interview, Y-BOCS, VAS (depression/ anxiety levels); HDRS. | - Worsening of symptoms in 65% of the patients; 31% of OCD patients showed an increase of more than 25% in their pre-pandemic Y-BOCS scores; 45% developed an obsession related to the risk of getting infected by SARS-CoV2; however, only 10% reported it as being their main obsessive concern. - Increased suicidal ideation among the OCD cohort. |
| Hassoulas et al. (2021) [35] | - To investigate the impact of the COVID-19 pandemic on individuals with OCD. | Lockdown: OCI-R; SHAI; brief COVID-19 impact measure. | - Pandemic-related restrictions impacted mental well-being in 57% of the participants. Moreover, 22% reported impacts in terms of physical health, 10% reported impacts due to their social isolation, and 5% mentioned financial and occupational impacts. |
| Khosravani et al. (2021) [36] | - To compare COVID-19-related stress reactions among patients with AD and OCD. | Pandemic: CSS; PHQ-4; FCV-19S; C19P-S; SHAI; VOCI; XS; HCQ-54; OCI-R; OCS. | - Patients with OCD, generalized AD, and panic disorder might have a higher risk for COVID-19 stress syndrome and COVID-19 stress disorder when compared to other ADs. |
| Benatti et al. (2020) [37] | - To describe the impact of COVID-19 pandemics in a sample of patients with OCD. | Pandemic: clinical interview. | - More than 1/3 of the sample reported OCD worsening; 30% of the worsening group developed new obsessions and compulsions and 41% re-experienced past obsessions and compulsions; 66% of these patients experienced an increase in avoidance behaviors; 71% had significantly higher rates of pharmacological therapy adjustment; 9% reported suicidal ideation; and 52% reported sleep disturbances. |
| Chakraborty et al. (2020) [38] | - To assess the impact of COVID-19 on OCD patients. | Pandemic: interview: changes in symptoms; Y-BOCS. | - Most of the participants did not report any deterioration of symptoms due to the pandemic; 3 of the participants were in complete remission, and 2 were in partial remission. Only 2% of the participants had a >25% increase in the Y-BOCS total score. |
| Davide et al. (2020) [12] | - To evaluate changes due to the pandemic in a group of OCD patients that underwent psychiatric treatment before the pandemic period. | Lockdown: Y-BOCS; questionnaire on COVID-19 pandemic and life during the quarantine. | - Out of the 40% of patients that were remitted before the quarantine, 13% relapsed with clinically significant OCD. |
| Matsunaga et al. (2020) [39] | - To investigate the acute impact of the COVID-19 pandemic in fully or partially remitted OCD patients. | Pandemic: Y-BOCS. | - A total of 10% experienced increased symptom severity, while 7% had additional or renewed OCD symptoms associated with COVID-19. - Higher traits of anxiety, depressive status, higher prevalence of generalized AD, fear of contamination and washing compulsions were found in patients whose pre-COVID-19 obsessions/compulsions were associated with respiratory virus infection. |
| Nissen et al. (2020) [40] | - To examine how children and adolescents with OCD react to the COVID-19 crisis. | Pandemic: self-developed questionnaire on well-being (i.e., perceived changes in quality of life, psychiatric symptoms’ severity, avoidance behaviors). | - Clinical group: 45% reported a worsening of their symptoms, namely, 32% concerning anxiety; 34% concerning depressive symptoms; and 19% concerning avoidance behavior. - Survey group: 73% reported a worsening of their symptoms, namely, 54% concerning anxiety; and 43% concerning depressive symptoms. - In both groups there was a positive correlation between aggravation of anxiety and depressive symptoms and experienced worsening of OCD. |
| Tanir et al. (2020) [16] | - To investigate the effects of COVID-19-related home confinement on the profile, severity, and exacerbation of symptoms in OCD individuals. | Lockdown: CGI-S; CY-BOCS. | - A total of 54% reported an increase in symptom severity; there was a significant increase in the frequency of contamination obsessions and cleaning/washing compulsions during the pandemic; 34% of the patients reported no change in symptom severity; 11% reported a decrease in CY-BOCS scores; 56% relapsed with obsessive compulsive symptoms; and 31% returned to clinically significant levels of OCD during the pandemic. |
| Eating Disorders | |||
| Giel et al. (2021) [41] | - To investigate ED symptoms, as well as general psychopathology, after the first COVID-19 lockdown in patients with a history of BED. | Lockdown: BDI-II; EDE-Q. | - Comparing the results obtained before and during COVID-19, there was a reduction of 50% in BED and a reduction of 14% in comorbid mental disorder. - No relations were found between binge eating frequency and self-reported distress, emotion regulation capacities, and sense of coherence. |
| Baenas et al. (2020) [42] | - To assess the level of deterioration in functioning and the factors that impact the adjustment of people with ED to the COVID-19 confinement. | Lockdown: EDI-2; SCL-90-R; TCI-R; YFAS-2. | - A total of 70% of the patients reported concerns related with the confinement; 26% reported non-adaptive reactions; 42% reported anxiety symptoms; and 30% reported depression symptoms. - A total of 26% of the patients had a worse symptom evolution during the confinement, while for 51% of the patients, the ED symptoms became less dominant. |
| Castellini et al. (2020) [43] | - To evaluate the impact of COVID-19 on ED patients, considering the role of pre-existing vulnerabilities. | Lockdown: BSI; CTQ-SF; ECR-R; EDE-Q; IES-R. | - 13% of the patients experienced full remission from baseline to pre-lockdown, and 25% of the patients achieved partial remission. - At post-lockdown assessment, 14% of the participants reported full remission, and 18% reported partial remission, whereas 62% still reported an ED diagnosis. |
| Fernández-Aranda et al. (2020) [44] | - The impact of confinement on eating symptomatology; and to explore the general acceptance of the use of telemedicine among people with ED. | Lockdown: CIES. | - AN patients reported less impact on eating symptoms, changes in eating habits and in emotion regulation. Obese patients reported decreased weight, BMI, and changes in eating habits; - Apart from AN and obese patients, other specified ED patients showed deterioration in eating symptomatology. |
| Schlegl et al. (2020) [45] | - To explore effects of the COVID-19 pandemic on ED symptoms and other psychological aspects in former inpatients with AN. | Pandemic: self-developed questionnaire on the overall impact of the COVID-19 pandemic on eating disorders symptoms and general well-being. | - Around 50% of the patients reported a deterioration of their quality of life; 17% indicated no worsening of it; 70% of the sample reported an increase in loneliness, inner restlessness, and sadness; 50% of the patients indicated fears of not being able to stop or control worries and worried that feelings get out of control; 50% of the patients reported that worries were related to infectng others and relapse; and 47% reported increases in family conflicts. No changes were reported in terms of friendships, romantic relationships, or workplace conflicts for 80% of the individuals. |
| Schlegl et al. (2020) [46] | - To investigate the impact of the current pandemic on patients with BN. | Pandemic: self-developed questionnaire on the overall impact of the COVID-19 pandemic on ED symptoms and general well-being. | - A total of 49% of the patients experienced worsening of ED symptomatology, while 62% had decreased quality-of-life scores. Moreover, binge eating increased in 47% of the patients, whereas self-induced vomiting increased in 36%. |
| Substance-Related Disorders | |||
| Blithikioti et al. (2021) [47] | - To assess risk factors of adverse mental health outcomes during lockdown in a SUD population. | Lockdown: questions of the ASSIST Screening Test; CTQ-SF; LEC; DTS; BDI; STAI; perception about symptom change due to quarantine measures. | - Increased consumption of: alcohol (13%), cannabis (1%), cocaine (3%), methamphetamine (1%), and sedatives (9%). One participant reported an increase in opioid consumption. - More than 50% of the participants reported a deterioration in depression and anxiety symptoms, associated with trauma exposure, female gender, perceived stress and isolation, income reduction, and alcohol use. |
| Chappuy et al. (2021) [48] | - To measure the impact of the COVID-19 lockdown on the addictions of SUD; to examine how anxiety, mood, and sleep are related to consumption; to investigate changes in their condition due to COVID-19. | Lockdown: online questionnaire (all questions were related to the lockdown period in France). | - Increased consumption of: alcohol (29%), cannabis (28%), psychostimulants (36%), heroin (40%), anxiolytics (26%), methadone (14%), and buprenorphine (23%). There was a 49% increase in addictive behaviors. - A total of 61% of the patients remained stable regarding general psychiatric symptoms, while they worsened for 30% and improved for 9%. |
| Lev Bar-Or et al. (2021) [49] | - To investigate changes in addictive behaviors among individuals treated in a specialized outpatient addiction treatment clinic. | Lockdown: interview: initiated, increased, decreased, or ceased use of various specific addictive substances and behaviors. | - A total of 36% increased their addictive behavior or the use of at least one substance: 25% alcohol, 29% cannabis, 29% stimulants, 15% sedatives, 15% pornography, and 11% gambling; 11% initiated an addictive behavior or the use of an addictive substance. |
| Cousijn et al. (2020) [6] | - To investigate the influence of the lockdown on SUD. | Lockdown: MINI (SUD section); AUDIT; motives for cannabis use; DSM-5-CCSM; COVID-19-related worries; social contact. | - There was a significant increase in cannabis use during the first months of lockdown. However, there was no evidence of a change in substance disorder symptoms’ severity. The lockdown period was weakly associated with reductions in substance disorders symptoms. |
| Martinotti et al. (2020) [50] | - To evaluate the impact of the COVID-19 pandemic and the containment measures on patients with SUD and/or behavioral addictions. | Lockdown: BDI-II; DTS; IDAS; SAS; VAS (level of craving for the substance). | - A total of 23% of our sample reported moderate/severe depressive symptoms; 30% reported moderate/severe anxiety symptoms. - A positive correlation was also verified between craving and depressive symptoms, anxiety, and traumatic stress. |
| Yazdi et al. (2020) [51] | - To investigate addictive behavior, craving, and PTSD symptoms, as well as various COVID-19 factors in a clinical sample of patients with SUD. | Pandemic: AUDIT; PC-PTSD5; interview: physiological, economic, and substance use factors related to COVID-19. | - A total of 29% of patients were abstinent; 38% were consuming; 32% relapsed. In the total sample, psychosocial COVID-19 distress was reported by 53.5% of the patients. - A total of 8% of the participants were found to be at risk of PTSD. |
| Attention-Deficit Hyperactivity Disorder | |||
| Becker et al. (2020) [52] | - To examine remote learning practices and difficulties during initial stay-at-home orders in adolescents with and without ADHD. | Lockdown: Home Adjustment to COVID-19 Scale; Adolescent Routines Questionnaire; COVID-19 Adolescent Symptom and Psychological Experience Questionnaire. | - The lack of routines during stay-at-home mandates, negative effects, and trouble concentrating were associated with remote learning difficulties in adolescents with ADHD. |
| Schizophrenia or Other Psychotic Disorder | |||
| Ma et al. (2020) [53] | - To explore the influence of social isolation on the psychological characteristics of hospitalized SPD patients. | Lockdown (in patients): CPSS; HAMA; HAMD; PANSS; PSQI. | - Inpatients with schizophrenia who went through social isolation showed higher and more severe levels of stress, anxiety, and depression, and worse sleep quality afterwards than those who were not isolated. |
| Pinkham et al. (2020) [31] | To examine the effects of the pandemic on people with pre-existing SMI’s (including people with schizophrenia spectrum disorder or severe affective disorders). | Pandemic: EMA; MADRS; PANSS; SUMD; YMRS. | - There were no significant changes in mood or psychotic symptoms and sleep duration over time; there was a small but significant increase in the number of substances used. - Participants also referred to a significant increase in well-being post-pandemic onset. |
| Tourette Syndrome or Chronic Tic Disorder | |||
| Mataix-Cols et al. (2020) [54] | - To investigate the impact of the COVID-19 outbreak on tic severity in people with TS or CTD. | Lockdown: self-developed Likert scale (Do you feel that your tics have worsened since the start of the coronavirus pandemic? | - Around 50% of the participants experienced a worsening in their tic symptomatology. - Increased stress and anxiety, worries about family, future, finances, changes in routines, etc., were associated with perceived tic worsening. |
| Insomnia Disorder | |||
| Cheng et al. (2021) [55] | - To examine resilience in the sleep and stress systems during the COVID-19 pandemic in participants with ID. | Life Events Checklist; CIS; ISI; IES COVID-19; QIDS-SR; PROMIS; GMH; GPH. | - More than two-thirds of the sample (67%) reported a direct impact from the pandemic; - COVID-19-related disruptions were associated with insomnia symptoms. |
| Somatic Symptom Disorder | |||
| De Nardi et al. (2021) [56] | - To evaluate how the COVID-19 lockdown affected adolescents with and without SSD. | Lockdown: MASC-2-SR; CDI-2-SF. | - Adolescents with SSD presented slightly lower significant anxiety raw scores and lower mean anxiety levels when compared to the controls. The physical symptoms, social anxiety, tension and restlessness scores, and levels of depression were also significantly lower in the SSD group than the controls. |
| Global impact on Multiple Psychiatric Disorders | |||
| Favreau et al. (2021) [57] | - To evaluate the impact of the pandemic on patients with GPP who were admitted to inpatient treatment. | Pandemic: Questionnaire: changes in symptom severity, quality of life and treatment; restrictions and pandemic-related worries. | - More than 50% reported worsening of symptoms; a 40% increased need of therapeutic support; nearly 1/4 reported a setback in treatment. |
| Imai et al. (2021) [58] | - To investigate the impact of masks and plastic partitions on patient-doctor communication and subjective anxiety for infection in patients with psychiatric disorders. | Pandemic: questionnaire: differences in the variable’s barrier to communication and anxiety for infection for use of masks and partitions. | - A total of 91% of the patients answered that there was no change with regard to communication when the doctor was wearing a mask or using a plastic partition (83%). - Results suggest that masks and plastic partitions do not prevent patient–doctor communication, and both bring beneficial effects in reducing anxiety for infection among patients with psychiatric disorders. |
| Mergel et al. (2021) [59] | - To investigate social participation, inclusion and psychological well-being in adults with and without pre-pandemic mental disorders. | Pandemic and lockdown: F-INK; IMET; BSI-18; specific questions regarding their subjective concerns; subjective possibilities of events in relation to the COVID-19 pandemic. | - The group with CMD did not report an impact in terms of their social participation. The group with pre-pandemic AMD exhibited fewer impairments during the lockdown period, whereas the group without mental disorders exhibited some impairments, which were transient and decreased over time, as the limitations were lifted. |
| Ting et al. (2021) [60] | - To examine the prevalence of posttraumatic stress response towards COVID-19, among patients with pre-existing psychiatric illness. | Pandemic: questionnaire: impact of Effect of COVID-19 on patients’ psychological response; IES-R; PHQ-2. | - PTSD-like symptoms were reported by more than 45% of the participants. - Rumination about COVID-19 and social isolation were predictors of higher levels of PTSD-like symptoms. |
| Tundo et al. (2021) [61] | - To examine the psychological and psychopathological impact of the pandemic stress on patients with pre-existing MD, AD and OCD. | Pandemic and lockdown: HAMD; Y-MANIA; Y-BOCS; PAAS; BSPS. | - A total of 11% of the patients reported higher distress levels than their family and friends regarding the fear of being infected; 5% reported changes in lifestyle; and 1% also reported changes in terms of financial burden. However, 37% of the patients reported that they were better-adapted than family and friends; - Only 5% of the patients relapsed/worsened due to COVID-19 distress. |
| Vissink et al. (2021) [62] | - To investigate the effects of COVID-19 and the restrictive measures on stress, anxiety and loneliness in patients with psychiatric disorders. | Pandemic: BAI; BDI; PSWQ; PQL-5; PSS; WHO-ASSIST questionnaire. | - Patients reported a deterioration in general health and mental health, as well as the presence of depressive symptoms and loneliness. - A total of 26% of the affective disorder patients reported severe loneliness, versus 9% of the psychotic disorder participants. |
| Burrai et al. (2020) [63] | - To assess the psychological and emotional impact of isolation on patients compared to healthy controls. | Lockdown: DASS-21; BRCS; risk perception; worry about the present emergency situation; knowledge about COVID-19. | - GPP patients demonstrated lower stress compared to healthy controls; however, they presented a higher perceived risk of getting infected with COVID-19, higher levels of worry, and higher levels of anxiety relative to healthy controls. |
| Chang et al. (2020) [64] | - To investigate the potential factors explaining preventive COVID-19 infection behaviors among individuals with mental illness. | Pandemic: BCIS; DASS-21; FCV-19S; PCIBS; SSS-S. | - Most of the patients reported experiencing self-stigma, fear of COVID-19, trust in COVID-19 information, engagement in preventive behaviors, and psychological distress. - Less trust in the information, higher levels of self-stigma, and fear of COVID explained more psychological distress. |
| Hao et al. (2020) [65] | - To compare the immediate stress and psychological impact experienced by people with and without psychiatric disorder during the pandemic. | Pandemic and lockdown: IES-R; DASS-21; ISI. | - Psychiatric patients when compared to healthy controls reported a significant increase in: worries about their physical health (29% vs. 5%); moderate to severe anger and impulsivity (21% vs. 0.9%); and moderate to severe suicidal ideation (12% vs. 0.9%). |
| Iasevoli et al. (2020) [66] | - To examine the severity of COVID-19-related perceived stress, anxiety, depressive, and psychotic symptoms in patients with serious mental disorders, caregivers, and control group. | Pandemic and lockdown: PSS; GAD-7; PHQ-9; SPEQ. | - Patients with mental illness had higher rates of perceived stress severity, moderate to severe anxiety, and significantly higher severe depressive symptoms compared to healthy controls. - Caregivers had lower results in all evaluated components compared to healthy and mentally ill patients. |
| Marchitelli et al. (2020) [67] | - To identify psychological and psychosocial variables that predict weight gain in overweight patients with and without a psychiatric diagnosis. | Lockdown: BES; DASS-21; DERS; GHQ-12; PAPF-SC; risk perception. | - Among the surveyed patients affected by overweight/obesity, 50% of those without a psychiatric diagnosis and 66% of those with a psychiatric diagnosis reported weight gain during the COVID-19 lockdown. - Weight gain predictors were binge eating behaviors for patients with a psychiatric diagnosis and stress and low depression for patients without a psychiatric diagnosis. |
| Muruganandam et al. (2020) [68] | - To determine the impact of COVID-19 in patients with SMI and identify its relationship with their COVID-19 knowledge. | Pandemic: questionnaire: self-developed questionnaire on awareness about symptoms of COVID-19. | - A total of 73% of the SMI patients did not report any anxiety/fear of contracting COVID-19. - Impairment was noted in sleep (38%), food intake (23%), and personal care (20%). A total of 30% of the patients showed re-emergence of previous psychiatric symptoms; 14% expressed suicidal ideas during this period; and 5% reported an increase in suicidal ideas; 28% expressed feelings of physical aggression toward their caregivers; 64% reported that they were experiencing verbal and physical aggression from others; 7% reported an increase in substance use during this lockdown period. |
| Pan et al. (2020) [69] | - To compare the perceived mental health impact on depressive symptoms, anxiety, worry, and loneliness before and during the COVID-19 pandemic among people with/without mental disorders. | Pandemic: NESDA: QIDS; BAI; PSWQ; DJGLS; - NESDO: QIDS; BAI; DJGLS; - NOCDA: BAI; DJGLS. | - Only 3% of the participants without a history of mental health disorders scored above the threshold for moderate to severe depressive symptoms during the pandemic. By contrast, in individuals with the largest mental health disorder burden, no overall increase in symptom severity was seen. |
| Porcellana et al. (2020) [70] | - To evaluate the relationship between traumatic aspects of COVID-19 and clinical correlates of consecutive outpatients in a community mental health setting. | Lockdown: CGI-S; BPRS-18; IES-R; SRQ-20. | - A total of 34% of the participants reported mild symptoms of distress; 32% reported moderate symptoms of distress; and 26% reported severe symptoms of distress. SRQ-20 total score was positive in 59% of the patients, particularly in the female population aged 45–65. Actively working and SRQ-20 significantly predicted IES-R total score. |
| Zou et al. (2020) [71] | - To investigate the prevalence of psychiatric symptoms and pain in older, clinically stable patients with and without psychiatric disorders during the COVID-19 pandemic. | Lockdown: questionnaire: self-developed questionnaire for current fatigue; - Instruments and scales: PHQ-9; ISI; NPRS; WHOQOL-BREF. | - A total of 47% of older, clinically stable patients with psychiatric disorders reported fatigue during the COVID-19 outbreak. - A total of 69% of the fatigue group reported illness worsening during COVID-19, while 39% of the non-fatigue group reported illness worsening during COVID-19. |
| Psychiatric Disorders | Main Results | Major Concerns or Potential Risk Factors |
|---|---|---|
| Mood |
|
|
| Anxiety |
|
|
| Obsessive compulsive |
|
|
| Eating |
|
|
| Substance use and addiction |
|
|
| Attention-deficit hyperactivity |
|
|
| Schizophrenia Spectrum |
|
|
| Tourette Syndrome or Chronic Tic Disorder |
|
|
| Insomnia |
| |
| Somatic Symptom Disorders |
|
|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carvalho, S.; Coelho, C.G.; Kluwe-Schiavon, B.; Magalhães, J.; Leite, J. The Acute Impact of the Early Stages of COVID-19 Pandemic in People with Pre-Existing Psychiatric Disorders: A Systematic Review. Int. J. Environ. Res. Public Health 2022, 19, 5140. https://doi.org/10.3390/ijerph19095140
Carvalho S, Coelho CG, Kluwe-Schiavon B, Magalhães J, Leite J. The Acute Impact of the Early Stages of COVID-19 Pandemic in People with Pre-Existing Psychiatric Disorders: A Systematic Review. International Journal of Environmental Research and Public Health. 2022; 19(9):5140. https://doi.org/10.3390/ijerph19095140
Chicago/Turabian StyleCarvalho, Sandra, Catarina G. Coelho, Bruno Kluwe-Schiavon, Juliana Magalhães, and Jorge Leite. 2022. "The Acute Impact of the Early Stages of COVID-19 Pandemic in People with Pre-Existing Psychiatric Disorders: A Systematic Review" International Journal of Environmental Research and Public Health 19, no. 9: 5140. https://doi.org/10.3390/ijerph19095140
APA StyleCarvalho, S., Coelho, C. G., Kluwe-Schiavon, B., Magalhães, J., & Leite, J. (2022). The Acute Impact of the Early Stages of COVID-19 Pandemic in People with Pre-Existing Psychiatric Disorders: A Systematic Review. International Journal of Environmental Research and Public Health, 19(9), 5140. https://doi.org/10.3390/ijerph19095140








