Healthcare Services and Formal Caregiver’s Psychosocial Risk Factors: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Instruments
2.4. Procedures
2.5. Data Analysis
3. Results
3.1. Sample’s Sociodemographic Characteristics
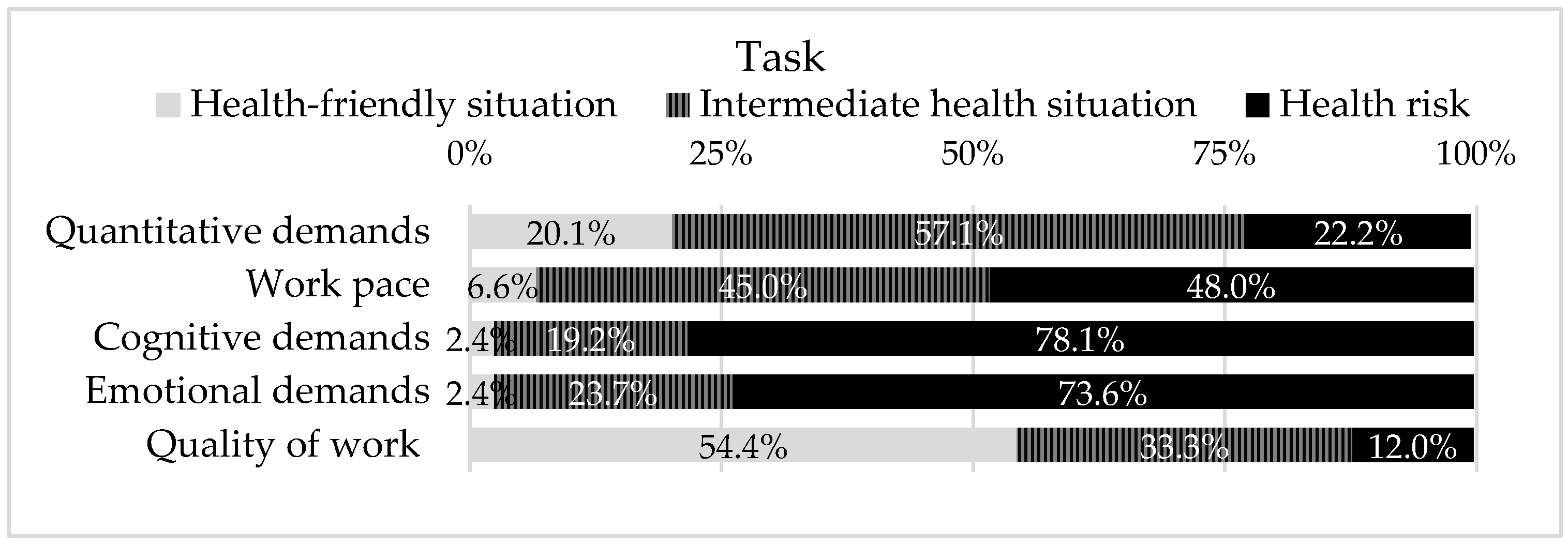
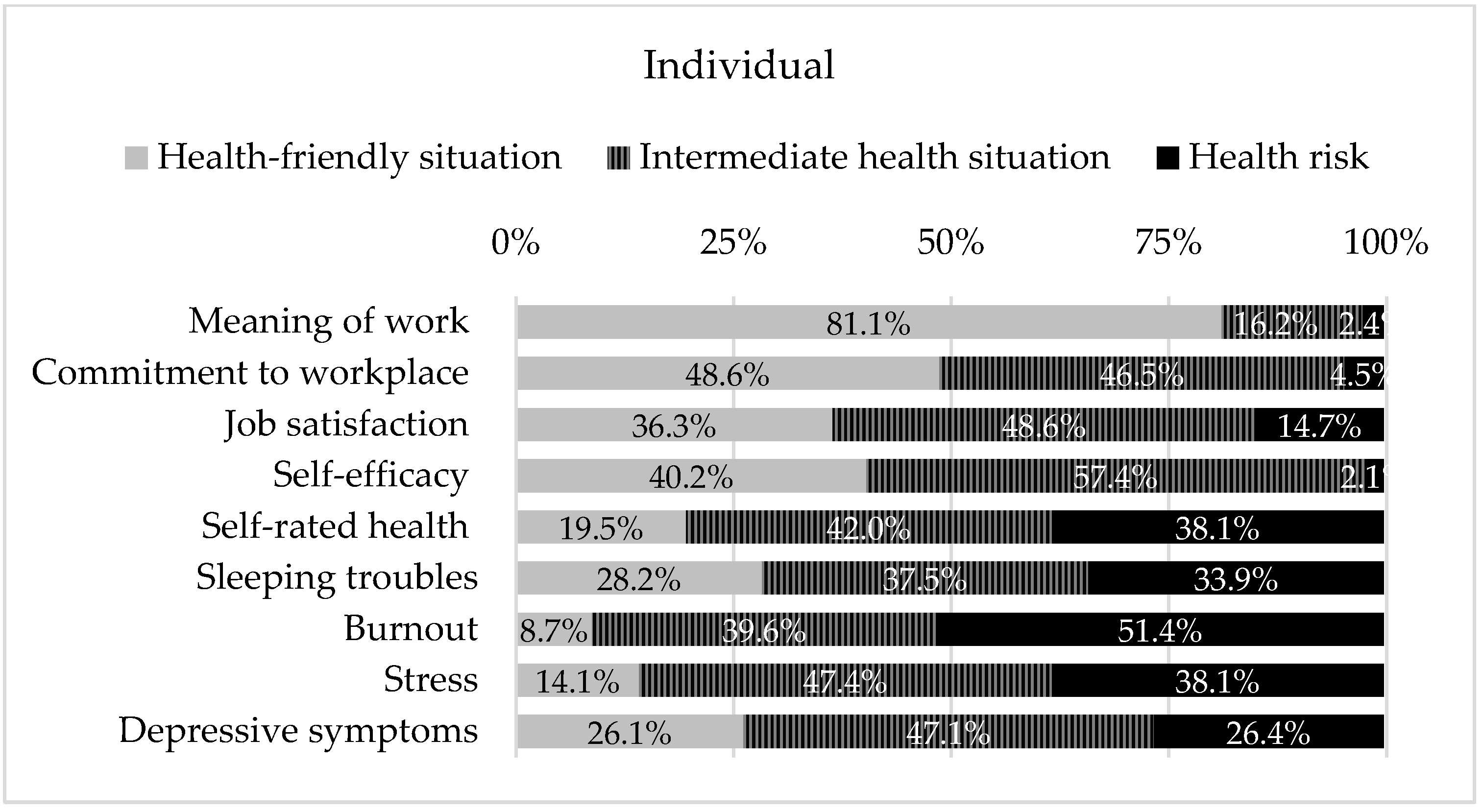
3.2. Psychosocial Risk Factors Exposure
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Noncommunicable Diseases. Available online: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases (accessed on 26 January 2022).
- World Health Organiztion [WHO]. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013.
- Pan American Health Organization [PAHO]. Innovative Care for Chronic Health Conditions. Organizing and Delivering High Quality Care for Chronic Noncommunicable Diseases in the Americas; Pan American Health Organization: Washington, DC, USA, 2013; Volume 12. [Google Scholar]
- Carayon, P.; Wooldridge, A.; Hoonakker, P.; Hundt, A.S.; Kelly, M.M. SEIPS 3.0: Human-Centered Design of the Patient Journey for Patient Safety. Appl. Ergon. 2020, 84, 103033. [Google Scholar] [CrossRef] [PubMed]
- Carayon, P. Human Factors of Complex Sociotechnical Systems. Appl. Ergon. 2006, 37, 525–535. [Google Scholar] [CrossRef] [PubMed]
- Carayon, P.; Smith, M.J. Work Organization and Ergonomics. Appl. Ergon. 2000, 31, 649–662. [Google Scholar] [CrossRef]
- Cox, T. Stress Research and Stress Management: Putting Theory to Work; HSE Contract Research Report No 61/1993; Health and Safety Executive: Norwich, UK, 1993.
- Leka, S.; Jain, A. Health Impact of Psychosocial Hazards at Work: An Overview; World Health Organization: Geneva, Switzerland, 2010.
- Fernandes, C.; Pereira, A. Exposure to Psychosocial Risk Factors in the Context of Work: A Systematic Review. Rev. Saude Publica 2016, 50, 24. [Google Scholar] [CrossRef] [PubMed]
- Instituto Nacional de Estatística [INE]. Estatísticas Da Saúde; Instituto Nacional de Estatística: Lisboa, Portugal, 2019.
- Cotrim, T.P.; Bem-Haja, P.; Pereira, A.; Fernandes, C.; Azevedo, R.; Antunes, S.; Pinto, J.S.; Kanazawa, F.; Souto, I.; Brito, E.; et al. The Portuguese Third Version of the Copenhagen Psychosocial Questionnaire: Preliminary Validation Studies of the Middle Version among Municipal and Healthcare Workers. Int. J. Environ. Res. Public Health 2022, 19, 1167. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, T.S.; Hannerz, H.; Høgh, A.; Borg, V. The Copenhagen Psychosocial Questionnaire—a Tool for the Assessment and Improvement of the Psychosocial Work Environment. Scand. J. Work. Environ. Health 2005, 31, 438–449. [Google Scholar] [CrossRef] [PubMed]
- Silva, C.; Amaral, V.; Pereira, A.; Bem-haja, P.; Pereira, A.; Rodrigues, V.; Cotrim, T.; Silvério, J.; Nossa, P. Copenhagen Psychosocial Questionnaire II: Portugal e Países Africanos de Língua Oficial Portuguesa; Universidade de Aveiro, Departamento de Educação e Psicologia: Aveiro, Portugal, 2011. [Google Scholar]
- Burr, H.; Berthelsen, H.; Moncada, S.; Nübling, M.; Dupret, E.; Demiral, Y.; Oudyk, J.; Kristensen, T.S.; Llorens, C.; Navarro, A.; et al. The Third Version of the Copenhagen Psychosocial Questionnaire. Saf. Health Work 2019, 10, 482–503. [Google Scholar] [CrossRef] [PubMed]
- Berthelsen, H.; Westerlund, H.; Bergström, G.; Burr, H. Validation of the Copenhagen Psychosocial Questionnaire Version III and Establishment of Benchmarks for Psychosocial Risk Management in Sweden. Int. J. Environ. Res. Public Health 2020, 17, 3179. [Google Scholar] [CrossRef] [PubMed]
- ALLEA—All European Academies. The European Code of Conduct for Research Integrity (Revised Edition), Revised ed.; ALLEA—All European Academies: Berlin, Germany, 2017. [Google Scholar]
- Krippendorff, K. Content Analysis. An Introduction to Its Methodology, 3rd ed.; Sage Publications: Thousand Oaks, CA, USA, 2013. [Google Scholar]
- Jain, A.; Leka, S.; Zwetsloot, G. Work, Health, Safety and Well-Being: Current State of the Art. In Managing Health, Safety and Wellbeing: Ethics, Responsibility and Sustainability; Jain, A., Leka, S., Zwetsloot, G., Eds.; Springer Science: Dordrecht, The Netherlands, 2018; pp. 1–32. [Google Scholar]
- World Health Organiztion [WHO]. WHO Global Plan of Action on Workers’ Health (2008–2017): Baseline for Implementation; World Health Organiztion: Geneva, Switzerland, 2013.
- Cotrim, T.; Silva, C.F.D.; Amaral, V.; Bem-Haja, P.; Pereira, A. Work Ability and Psychosocial Factors in Healthcare Settings: Results from a National Study. In Proceedings of the 5th International Conference on Applied Human Factors and Ergonomics AHFE, Kraków, Poland, 19–23 July 2014; Ahram, T., Karwowski, W., Marek, T., Eds.; pp. 19–23. [Google Scholar]
- Cotrim, T.; Soares, G.; Ferreira, P.; Barnabé, R.; Teles, J.; Prata, N. Measuring Psychosocial Factors and Predicting Work Ability among Cemetery Workers. In Work; IOS Press: Fairfax, VA, USA, 2020; Volume 65, pp. 111–119. [Google Scholar] [CrossRef]
- Davison, C.; Cotrim, T.P.; Gonçalves, S. Perception of Musculoskeletal Symptoms and Psychosocial Risk Factors among a Sample of Portuguese Emergency Medical Technicians. In Advances in Intelligent Systems and Computing; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1012, pp. 46–55. [Google Scholar] [CrossRef]
- Guimarães, J.P.D.; Rodrigues, F.A.; Dias, A.K.; Guimarães, A.P.M.; Couto, G.B.F.D.; Pereira, R.A.; Markus, G.W.S.; Santos, J.M. dos. COVID-19: Impactos Ocasionados Na Saúde Mental Em Estudantes Do Ensino Superior Brasileiro. Res. Soc. Dev. 2021, 10, e3410917385. [Google Scholar] [CrossRef]
- Ilmarinen, J. From Work Ability Research to Implementation. Int. J. Environ. Res. Public Health 2019, 16, 2882. [Google Scholar] [CrossRef] [PubMed]
- International Labour Organization [ILO]. Workplace Stress: A Collective Challenge; International Labour Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Mostardinha, A.R.; Pereira, A. Drinking, Smoking and Type a Polydrug Behaviours: Psychosocial Factors among Portuguese University Students. Psychol. Community Health 2020, 8, 158–175. [Google Scholar] [CrossRef][Green Version]
- Pacheco, E.C.R.L.; Bártolo, A.; Rodrigues, F.; Pereira, A.; Duarte, J.C.; Silva, C.F. Impact of Psychological Aggression at the Workplace on Employees’ Health: A Systematic Review of Personal Outcomes and Prevention Strategies. Psychol. Rep. 2021, 124, 929–976. [Google Scholar] [CrossRef] [PubMed]
- Queirós, C.; Passos, F.; Bártolo, A.; Faria, S.; Fonseca, S.M.; Marques, A.J.; Silva, C.F.; Pereira, A. Job Stress, Burnout and Coping in Police Officers: Relationships and Psychometric Properties of the Organizational Police Stress Questionnaire. Int. J. Environ. Res. Public Health 2020, 17, 6718. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, C.A.; Cotrim, T.P.; Reis, V.; Guerreiro, M.J.; Candeias, S.M.; Janicas, A.S.; Costa, M. Work Ability, Ageing and Musculoskeletal Symptoms among Portuguese Municipal Workers. In Occupational Safety and Hygiene VI—Selected Contributions from the International Symposium Occupational Safety and Hygiene, SHO 2018; CRC Press/Balkema: Leiden, The Netherlands, 2018; pp. 91–95. [Google Scholar] [CrossRef]
- Souto, I.; Pereira, A.; Brito, E.; Sancho, L.; Barros, S. Occupational Health Risk Among Teachers in Higher Education. In Advances in Intelligent Systems and Computing; Springer: Berlin/Heidelberg, Germany, 2019; Volume 1012, pp. 311–322. [Google Scholar] [CrossRef]
- World Health Organization [WHO]. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018.
- Wolf, J.; Ivanov, I.; Mugdal, S.; Bos, R.; Neira, M. Preventing Disease through a Healthier and Safer Worplace; World Health Organization: Geneva, Switzerland, 2018.
- European Agency for Safety and Health at Work [EU-OSHA]. Psychosocial Risks and Stress at Work—Safety and Health at Work—EU-OSHA. Available online: https://osha.europa.eu/en/themes/psychosocial-risks-and-stress (accessed on 30 January 2018).
- European Commission. Horizon Europe Strategic Plan (2021–2024), 1st ed.; Office of the European Union: Luxembourg, 2021. [Google Scholar] [CrossRef]
- Pereira, A.; Oliveira, C.A.; Vagos, P.; Bártolo, A.; Jardim, J.; Monteiro, S. Reliability and Factor Structure of the 10-Item Kessler Psychological Distress Scale (K10) among Portuguese Adults. Rev. Ciência e Saúde Coletiva 2019, 24, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Lopes, M.J.; Fonseca, C.; Barbosa, P. The Individual Care Plan as Electronic Health Record. In Exploring the Role of ICTs in Healthy Aging; Mendes, D., Fonseca, C., Lopes, M.J., García-Alonso, J., Murillo, J.M., Eds.; IGI Global: Pennsylvania, PA, USA, 2020; pp. 1–12. [Google Scholar] [CrossRef]
- Drissi, N.; Ouhbi, S.; Marques, G.; De La Torre Díez, I.; Ghogho, M.; Janati Idrissi, M.A. A Systematic Literature Review on E-Mental Health Solutions to Assist Health Care Workers during COVID-19. Telemed. E-Health 2021, 27, 594–602. [Google Scholar] [CrossRef] [PubMed]
- Marques, D.R.; Castilho, P.; Allen Gomes, A.; Pereira, A. Mindfulness and Self-Compassion along the Chronotype: A Cross-Sectional Study. Chronobiol. Int. 2019, 36, 541–547. [Google Scholar] [CrossRef] [PubMed]
- Rush, K.S.; Golden, M.E.; Mortenson, B.P.; Albohn, D.; Horger, M. The Effects of a Mindfulness and Biofeedback Program on the On- and Off-Task Behaviors of Students with Emotional Behavioral Disorders. Contemp. Sch. Psychol. 2017, 21, 347–357. [Google Scholar] [CrossRef]
- Burgess, M.G.; Brough, P.; Biggs, A.; Hawkes, A.J. Why Interventions Fail: A Systematic Review of Occupational Health Psychology Interventions. Int. J. Stress Manag. 2020, 27, 195–207. [Google Scholar] [CrossRef]
- Queirós, C.; Passos, F.; Bártolo, A.; Marques, A.J.; da Silva, C.F.; Pereira, A. Burnout and Stress Measurement in Police Officers: Literature Review and a Study With the Operational Police Stress Questionnaire. Front. Psychol. 2020, 11, 587. [Google Scholar] [CrossRef] [PubMed]
- Mutambudzi, M.; Henkens, K. Chronic Health Conditions and Work-Related Stress in Older Adults Participating in the Dutch Workforce. Eur. J. Ageing 2020, 17, 499–508. [Google Scholar] [CrossRef] [PubMed]
- WHO Regional Office for Europe. The Toolkit for a Sustainable Health Workforce in the WHO European Region; WHO Regional Office for Europe: Bonn, Germany, 2018; p. 88. [Google Scholar]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pereira, A.; Brito, E.; Souto, I.; Alves, B. Healthcare Services and Formal Caregiver’s Psychosocial Risk Factors: An Observational Study. Int. J. Environ. Res. Public Health 2022, 19, 5009. https://doi.org/10.3390/ijerph19095009
Pereira A, Brito E, Souto I, Alves B. Healthcare Services and Formal Caregiver’s Psychosocial Risk Factors: An Observational Study. International Journal of Environmental Research and Public Health. 2022; 19(9):5009. https://doi.org/10.3390/ijerph19095009
Chicago/Turabian StylePereira, Anabela, Elisabeth Brito, Isabel Souto, and Bruno Alves. 2022. "Healthcare Services and Formal Caregiver’s Psychosocial Risk Factors: An Observational Study" International Journal of Environmental Research and Public Health 19, no. 9: 5009. https://doi.org/10.3390/ijerph19095009
APA StylePereira, A., Brito, E., Souto, I., & Alves, B. (2022). Healthcare Services and Formal Caregiver’s Psychosocial Risk Factors: An Observational Study. International Journal of Environmental Research and Public Health, 19(9), 5009. https://doi.org/10.3390/ijerph19095009





