Infant Young Child Feeding Practices in an Indian Maternal–Child Birth Cohort in Belagavi, Karnataka
Abstract
:1. Introduction
2. Methods
2.1. Data Collection
2.2. Derived Variables
2.3. Statistical Analysis
3. Results
3.1. Early Breastfeeding Practices (at Birth)
3.2. Feeding in the First Month and Complementary Feeding Practices at Six Months
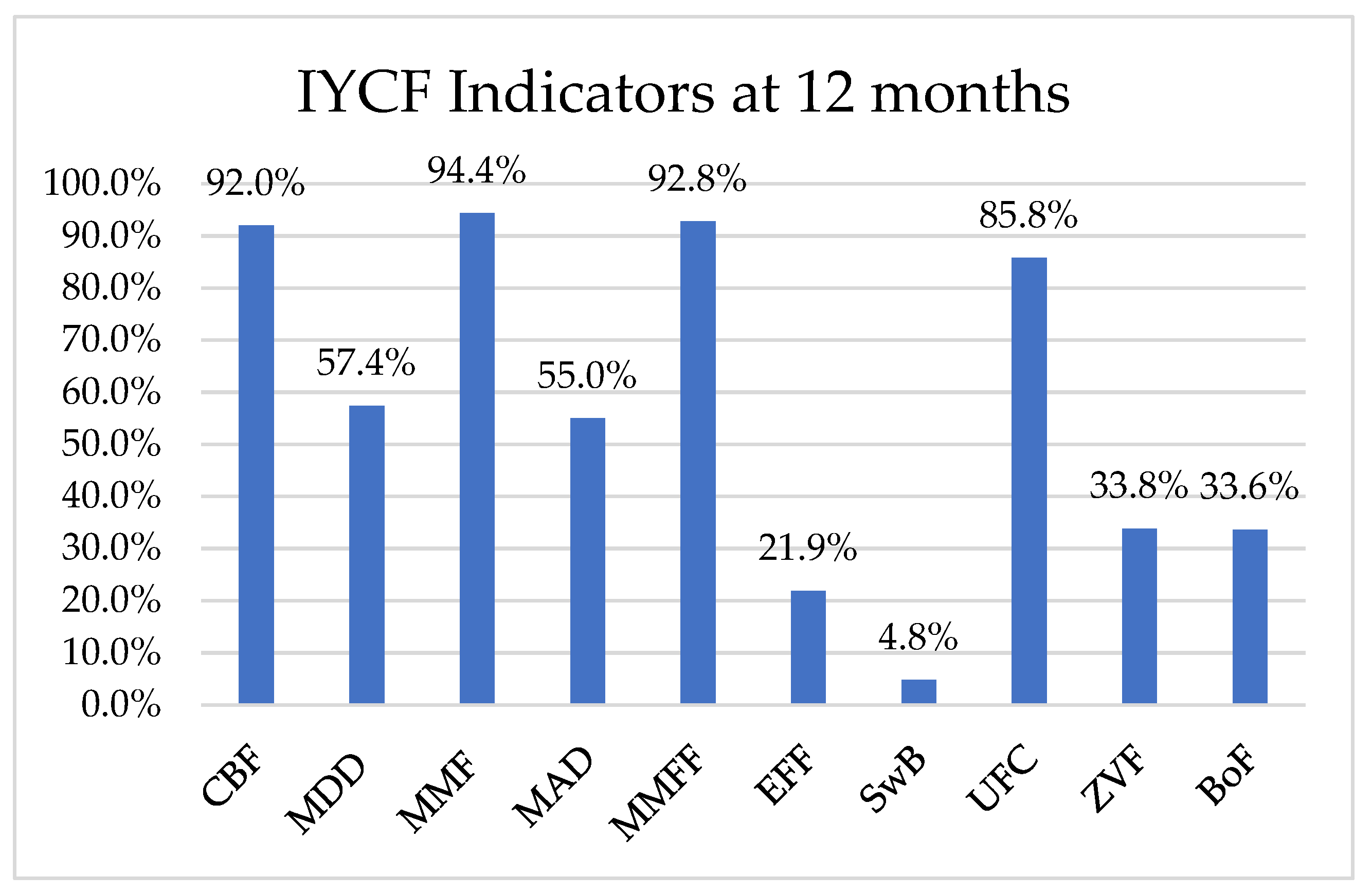
3.3. Feeding Practices at Twelve Months
3.4. Association of Exclusive Breastfeeding at 6 Months with Maternal and Infant Characteristics
3.5. Association of Exclusive Breastfeeding at 6 Months with Child Weight, Height and Head Circumference at 6 and 12 Months
3.6. Association of Diet Diversity (DD) Score with the Mother’s Characteristics
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; De Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451, Erratum in Lancet 2013, 382, 396. [Google Scholar] [CrossRef]
- Black, R.E.; Allen, L.H.; Bhutta, Z.A.; Caulfield, L.E.; De Onis, M.; Ezzati, M.; Mathers, C.; Rivera, J.; Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: Global and regional exposures and health consequences. Lancet 2008, 371, 243–260. [Google Scholar] [CrossRef]
- Jones, G.; Steketee, R.W.; Black, R.E.; Bhutta, Z.A.; Morris, S.S.; Bellagio Child Survival Study Group. How many child deaths can we prevent this year? Lancet 2003, 362, 65–71. [Google Scholar] [CrossRef]
- Fed to Fail? The Crisis of Children’s Diets in Early Life; Child Nutrition Report; UNICEF: New York, NY, USA, 2021.
- Daelmans, B.; Dewey, K.; Arimond, M. New and updated indicators for assessing infant and young child feeding. Food Nutr. Bull. 2009, 30 (Suppl. 2), S256–S262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Indicators for Assessing Infant and Young Child Feeding Practices: Definitions and Measurement Methods; World Health Organization: Geneva, Switzerland. Available online: https://www.who.int/publications/i/item/9789240018389 (accessed on 5 October 2021).
- Meshram, I.I.; Rao, K.M.; Balakrishna, N.; Harikumar, R.; Arlappa, N.; Sreeramakrishna, K.; Laxmaiah, A. Infant and young child feeding practices, sociodemographic factors and their association with nutritional status of children aged <3 years in India: Findings of the National Nutrition Monitoring Bureau survey (2011–2012). Public Health Nutr. 2019, 22, 104–114. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nguyen, P.H.; Scott, S.; Headey, D.; Singh, N.; Tran, L.M.; Menon, P.; Ruel, M.T. The double burden of malnutrition in India: Trends and inequalities (2006–2016). PLoS ONE 2021, 16, e0247856. [Google Scholar] [CrossRef]
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-4), (2015–2016); IIPS: Mumbai, India, 2017. [Google Scholar]
- Ministry of Health and Family Welfare (MoHFW), Government of India, UNICEF and Population Council. Comprehensive National Nutrition Survey (CNNS) National Report; MoHFW: New Delhi, India, 2019. [Google Scholar]
- Khandelwal, S.; Swamy, M.K.; Patil, K.; Kondal, D.; Chaudhry, M.; Gupta, R.; Divan, G.; Kamate, M.; Ramakrishnan, L.; Bellad, M.B.; et al. The impact of DocosaHexaenoic Acid supplementation during pregnancy and lactation on Neurodevelopment of the offspring in India (DHANI): Trial protocol. BMC Pediatr. 2018, 18, 261. [Google Scholar] [CrossRef] [Green Version]
- Khanna, A.; Kadeangadi, M.D.; Mallapur, M.D. Infant and young child feeding practices in Belgaum: A descriptive study. Indian J. Pract. Dr. 2014, 9, 24–29. [Google Scholar]
- Kogade, P.; Gaidhane, A.; Choudhari, S.; Khatib, M.N.; Kawalkar, U.; Gaidhane, S.; Zahiruddin, Q.S. Socio-cultural determinants of infant and young child feeding practices in rural India. Med. Sci. 2019, 23, 1015–1022. [Google Scholar]
- Mehlawat, U.; Puri, S.; Rekhi, T.K.; Yadav, B.S.; Tiwari, S.K. A study on Infant and Young Child feeding practices of mothers visiting District Civil Hospital. New Indian J. Pediatr. 2018, 7, 178. [Google Scholar]
- International Institute for Population Sciences (IIPS) and ICF. National Family Health Survey (NFHS-5), India, (2019–2021); IIPS: Mumbai, India, 2021. [Google Scholar]
- Zong, X.; Wu, H.; Zhao, M.; Magnussen, C.G.; Xi, B. Global prevalence of WHO infant feeding practices in 57 LMICs in 2010–2018 and time trends since 2000 for 44 LMICs. EClinicalMedicine 2021, 37, 100971. [Google Scholar] [CrossRef] [PubMed]
- Yadavannavar, M.C.; Patil, S.S. Socio cultural factors affecting breastfeeding practices and Decisions in rural women. Int. J. Plant Anim. Environ. Sci. 2011, 37, 100971. [Google Scholar]
- Ickes, S.B.; Hurst, T.E.; Flax, V.L. Maternal Literacy, Facility Birth, and Education Are Positively Associated with Better Infant and Young Child Feeding Practices and Nutritional Status among Ugandan Children. J. Nutr. 2015, 145, 2578–2586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mekonnen, M.; Kinati, T.; Bekele, K.; Tesfa, B.; Hailu, D.; Jemal, K. Infant and young child feeding practice among mothers of children age 6 to 23 months in Debrelibanos district, North Showa zone, Oromia region, Ethiopia. PLoS ONE 2021, 16, e0257758. [Google Scholar] [CrossRef]
- Neves, P.A.R.; Barros, A.J.D.; Gatica-Domínguez, G.; Vaz, J.S.; Baker, P.; Lutter, C.K. Maternal education and equity in breastfeeding: Trends and patterns in 81 low- and middle-income countries between 2000 and 2019. Int. J. Equity Health 2021, 20, 20. [Google Scholar] [CrossRef]
- Ministry of Health and Family Welfare. National Family Health Survey (NFHS-5): State Fact Sheet Karnataka; IIPS: Mumbai, India, 2021. [Google Scholar]
- Tahir, M.J.; Ejima, K.; Li, P.; Demerath, E.W.; Allison, D.B.; Fields, D.A. Associations of breastfeeding or formula feeding with infant anthropometry and body composition at 6 months. Matern. Child Nutr. 2021, 17, e13105. [Google Scholar] [CrossRef]
- Khan, A.M.; Kayina, P.; Agrawal, P.; Gupta, A.; Kannan, A.T. A study on infant and young child feeding practices among mothers attending an urban health centre in East Delhi. Indian J. Public Health 2012, 56, 301–304. [Google Scholar] [CrossRef]
- Javalkar, S.R. Assessing WHO’s IYCF Indicators in Mangalore Taluk-A Cross sectional Study. Indian J. Public Health Res. Dev. 2019, 10, 76–80. [Google Scholar] [CrossRef]
- Khan, N.; Mozumdar, A.; Kaur, S. Dietary Adequacy among Young Children in India: Improvement or Stagnation? An Investigation From the National Family Health Survey. Food Nutr. Bull. 2019, 40, 471–487. [Google Scholar] [CrossRef]
- Belew, A.K.; Ali, B.M.; Abebe, Z.; Dachew, B.A. Dietary diversity and meal frequency among infant and young children: A community based study. Ital. J. Pediatr. 2017, 43, 73. [Google Scholar] [CrossRef] [Green Version]
- Choudhury, S.; Headey, D.D.; Masters, W.A. First foods: Diet quality among infants aged 6–23 months in 42 countries. Food Policy 2019, 88, 101762. [Google Scholar] [CrossRef] [PubMed]
- Gatica-Domínguez, G.; Neves, P.A.R.; Barros, A.J.D.; Victora, C.G. Complementary feeding practices in 80 low- and middle-income countries: Prevalence and socioeconomic inequalities in dietary diversity, meal frequency and dietary adequacy. J. Nutr. 2021, 151, 1956–1964. [Google Scholar] [CrossRef] [PubMed]
- Lassi, Z.S.; Rind, F.; Irfan, O.; Hadi, R.; Das, J.K.; Bhutta, Z.A. Impact of Infant and Young Child Feeding (IYCF) Nutrition Interventions on Breastfeeding Practices, Growth and Mortality in Low- and Middle-Income Countries: Systematic Review. Nutrition 2020, 12, 722. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Puri, S. Transition in Infant and Young Child Feeding Practices in India. Curr. Diabetes Rev. 2016, 17, 477–481. [Google Scholar] [CrossRef] [PubMed]
| Mother | n = 902, n (%) |
|---|---|
| Mother’s age (years), mean (SD) | 23.5 (3.6) |
| Gestation age (week), median (IQR) | 15.0 (12.0, 18.0) |
| Parity | |
| Multiparous | 469 (52.0) |
| Nulliparous | 433 (48.0) |
| Education | |
| College graduate and above | 163 (18.1) |
| High school/Secondary | 712 (78.9) |
| Up to primary | 27 (3.0) |
| Employment Status | |
| Working | 216 (23.9) |
| Homemakers | 686 (76.1) |
| Household income per month (INR) | |
| <10,000 (USD 133.46) | 216 (23.9) |
| 10,001 (USD 133.47)–20,000 (USD 266.91) | 249 (27.6) |
| >20,000 (USD 266.91) | 108 (12.0) |
| Don’t Know | 21 (2.3) |
| Vegetarian (self-reported) | 152 (16.9) |
| Height (cm), mean (SD) | 153.9 (5.6) |
| Weight (kg), mean (SD) | 48.9 (8.8) |
| BMI (kg/m2), mean (SD) | 20.6 (3.6) |
| Mid-arm circumference (mm), mean (SD) | 24.3 (3.1) |
| Haemoglobin, mean (SD) | 11.1 (1.3) |
| Gestation age at delivery (Weeks), median (IQR) * | 39.0 (38.0, 40.0) |
| Preterm (Gestation age < 37 weeks) | 61 (6.8) |
| Children | n = 902 Live singleton births |
| Male sex | 477 (52.9) |
| Birth weight (grams), median (IQR) | 2740.0 (2500.0, 3011.0) (n = 880) |
| Birth length (cm), median (IQR) | 47.2 (46.1, 48.5) (n = 823) |
| Head circumference (cm), median (IQR) | 34.0 (33.0, 34.5) (n = 823) |
| Apgar score at 1 min, median (IQR) | 7.0 (6.0, 7.0) (n = 748) |
| Apgar score at 5 min, median (IQR) | 8.0 (8.0, 8.0) (n = 751) |
| Feeding Practices | n = 902 n (%) |
|---|---|
| Early initiation of Breastfeeding (within 1 h) Not available | 703 (77.9) 32 (3.5) |
| Reason for delay of Early initiation of breastfeeding (n = 167) Breastmilk was not expressed within 1 h of birth Mother was shifted to the ward after 1 h of delivery After delivery, baby was shifted to NICU Others * Reason not available | 38 (4.2) 63 (6.9) 29 (3.2) 31 (3.5) 6 (0.8) |
| Colostrum fed to the baby | 859 (95.2) |
| Baby given pre-lacteal feed | 77 (8.5) |
| Kind of pre-lacteal feed (n = 77) Cow’s Milk Dates Ghutti Gripe Water Honey Sugar Water Warm Water Water Not available | 1 (1.3) 1 (1.3) 1 (1.3) 1 (1.3) 35 (45.5) 31 (40.3) 1 (1.3) 1 (1.3) 5 (6.5) |
| Mode of feeding prior to hospital discharge Exclusive Breast Milk Mixed Feeding Exclusive formula feeding Expressed milk Any other Not available | 843 (93.5) 9 (1.0) 11 (1.2) 1 (0.1) 1 (0.1) 37 (4.1) |
| Mother and Child Characteristics | Exclusive Breastfed at 6 Month | ||||||
|---|---|---|---|---|---|---|---|
| Yes | No | p-Value | Relative Risk (95% CI) | ||||
| 427 | 417 | Unadjusted | Adjusted * | Adjusted ** | |||
| Mother’s characteristics | |||||||
| Mother’s age | |||||||
| 18–20 | 197 | 97 (49.2) | 90 (45.7) | 0.51 | 1.0 | 1.0 | 1.0 |
| 21–25 | 461 | 218 (47.3) | 209 (45.3) | 0.98 (0.83, 1.16) | 1.00 (0.84, 1.21) | 1.00 (0.83, 1.21) | |
| 26–30 | 208 | 97 (46.6) | 98 (47.1) | 0.96 (0.79, 1.17) | 1.00 (0.81, 1.25) | 1.01 (0.81, 1.26) | |
| 31–35 | 38 | 15 (41.7) | 20 (55.6) | 0.83 (0.55, 1.24) | 0.90 (0.56, 1.3) | 0.84 (0.55, 1.28) | |
| Mother’s education | |||||||
| ≤Secondary | 467 | 241 (51.6) | 196 (42) | 0.006 | 1.21 (1.05, 1.38) | 1.15 (1.00, 1.32) | 1.16 (1.01, 1.33) |
| Senior Secondary or Professional | 435 | 186 (42.8) | 221 (50.8) | 1.0 | 1.0 | 1.0 | |
| Monthly Income (INR) | |||||||
| <10,000 | 524 | 251 (47.9) | 238 (45.4) | 0.61 | 1.0 | 1.0 | 1.0 |
| 10,000–20,000 | 249 | 112 (45) | 123 (49.4) | 0.93 (0.79, 1.09) | 0.95 (0.81, 1.11) | 0.95 (0.82, 1.11) | |
| >20,000 | 108 | 52 (48.1) | 48 (44.4) | 1.01 (0.82, 1.25) | 1.20 (0.97, 1.48) | 1.22 (0.99, 1.51) | |
| BMI (kg/m2), mean (SD) | 20.3 (3.2) (n = 427) | 21.1 (3.9) (n = 417) | 0.002 | 0.97 (0.95, 0.99) | 0.97 (0.95, 0.99) | 0.97 (0.95, 0.99) | |
| Parity (no. of live children) | |||||||
| Multiparous | 469 | 239 (51) | 202 (43.1) | 0.029 | 1.16 (1.01, 1.33) | 1.21 (1.05, 1.41) | 1.23 (1.06, 1.43) |
| Nulliparous | 433 | 188 (43.4) | 215 (49.7) | 1.0 | 1.0 | 1.0 | |
| Type of Delivery | |||||||
| Vaginal normal/instrument | 551 | 288 (52.3) | 242 (43.9) | 0.005 | 1.23 (1.06, 1.42) | 1.17 (1.01, 1.37) | 1.18 (1.01, 1.37) |
| Caesarean | 329 | 139 (42.2) | 175 (53.2) | 1.0 | 1.0 | 1.0 | |
| Child characteristics | |||||||
| Hospitalisation at 1, 6 or 12 months | |||||||
| Yes | 21 | 6 (28.6) | 13 (61.9) | 0.044 | 0.62 (0.32, 1.2) | 0.60 (0.31, 1.15) | 0.59 (0.30, 1.16) |
| No | 874 | 421 (48.2) | 404 (46.2) | 1.0 | 1.0 | 1.0 | |
| Exclusive Breastfed at 6 Months | p-Value | Difference (95% CI) | β Coefficient * (95% CI) | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Weight (grams) at 6 months, mean (SD) | 6956.5 (854.7) | 6882.2 (911.3) | 0.22 | 74.2 (−45.1, 193.6) | 91.8 (−29.9, 213.5) |
| Height (cm) at 6 months, mean (SD) | 64.6 (2.8) | 64.7 (2.9) | 0.74 | −0.07 (−0.46, 0.32) | 0.004 (−0.39, 0.4) |
| Head Circumference (cm) at 6 months, mean (SD) | 42.0 (1.4) | 42.1 (1.4) | 0.19 | −0.13 (−0.31, 0.06) | −0.07 (−0.26, 0.12) |
| Weight (grams) at 12 months, mean (SD) | 8415.1 (1022.4) | 8392.7 (1024.1) | 0.75 | 22.4 (−116.3, 161.1) | 56.5 (−83.2, 196.2) |
| Height (cm) at 12 months, mean (SD) | 72.2 (3.0) | 72.4 (3.3) | 0.44 | −0.17 (−0.59, 0.26) | −0.074 (−0.51, 0.36) |
| Head Circumference(cm) at 12 months, mean (SD) | 44.6 (1.3) | 44.6 (1.4) | 0.30 | −0.10 (−0.28, 0.09) | −0.04 (−0.23, 0.14) |
| DD | p-Value | ||
|---|---|---|---|
| n | mean (SD) | ||
| Overall | 878 | 4.66 (1.15) | |
| Mother’s age, years | 0.335 | ||
| 18–20 | 193 | 4.53 (1.13) | |
| 21–25 | 448 | 4.68 (1.18) | |
| 26–30 | 202 | 4.73 (1.10) | |
| 31–35 | 35 | 4.71 (1.15) | |
| Mother’s education | |||
| ≤Secondary | 427 | 4.62 (1.14) | 0.218 |
| Senior Secondary or Professional | 451 | 4.71 (1.16) | |
| Monthly Income (INR) | |||
| <10,000 | 507 | 4.55 (1.16) | 0.002 |
| 10,000–20,000 | 244 | 4.76 (1.09) | |
| >20,000 | 106 | 4.93 (1.17) | |
| Parity (no. of live children) | |||
| Multiparous | 455 | 4.65 (1.13) | 0.655 |
| Nulliparous | 423 | 4.68 (1.17) | |
| Type of Delivery | |||
| Vaginal normal/instrument | 537 | 4.68 (1.15) | 0.414 |
| Caesarean | 319 | 4.61 (1.15) | |
| Exclusive breastfed | |||
| Yes | 425 | 4.65 (1.15) | 0.803 |
| No | 414 | 4.67 (1.16) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Khandelwal, S.; Kondal, D.; Chakravarti, A.R.; Dutta, S.; Banerjee, B.; Chaudhry, M.; Patil, K.; Swamy, M.K.; Ramakrishnan, U.; Prabhakaran, D.; et al. Infant Young Child Feeding Practices in an Indian Maternal–Child Birth Cohort in Belagavi, Karnataka. Int. J. Environ. Res. Public Health 2022, 19, 5088. https://doi.org/10.3390/ijerph19095088
Khandelwal S, Kondal D, Chakravarti AR, Dutta S, Banerjee B, Chaudhry M, Patil K, Swamy MK, Ramakrishnan U, Prabhakaran D, et al. Infant Young Child Feeding Practices in an Indian Maternal–Child Birth Cohort in Belagavi, Karnataka. International Journal of Environmental Research and Public Health. 2022; 19(9):5088. https://doi.org/10.3390/ijerph19095088
Chicago/Turabian StyleKhandelwal, Shweta, Dimple Kondal, Anindita Ray Chakravarti, Soumam Dutta, Bipsa Banerjee, Monica Chaudhry, Kamal Patil, Mallaiah Kenchaveeraiah Swamy, Usha Ramakrishnan, Dorairaj Prabhakaran, and et al. 2022. "Infant Young Child Feeding Practices in an Indian Maternal–Child Birth Cohort in Belagavi, Karnataka" International Journal of Environmental Research and Public Health 19, no. 9: 5088. https://doi.org/10.3390/ijerph19095088
APA StyleKhandelwal, S., Kondal, D., Chakravarti, A. R., Dutta, S., Banerjee, B., Chaudhry, M., Patil, K., Swamy, M. K., Ramakrishnan, U., Prabhakaran, D., Tandon, N., & Stein, A. D. (2022). Infant Young Child Feeding Practices in an Indian Maternal–Child Birth Cohort in Belagavi, Karnataka. International Journal of Environmental Research and Public Health, 19(9), 5088. https://doi.org/10.3390/ijerph19095088







