Relationship between Depressive Symptoms and Weather Conditions
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Description
2.2. Statistical Analysis
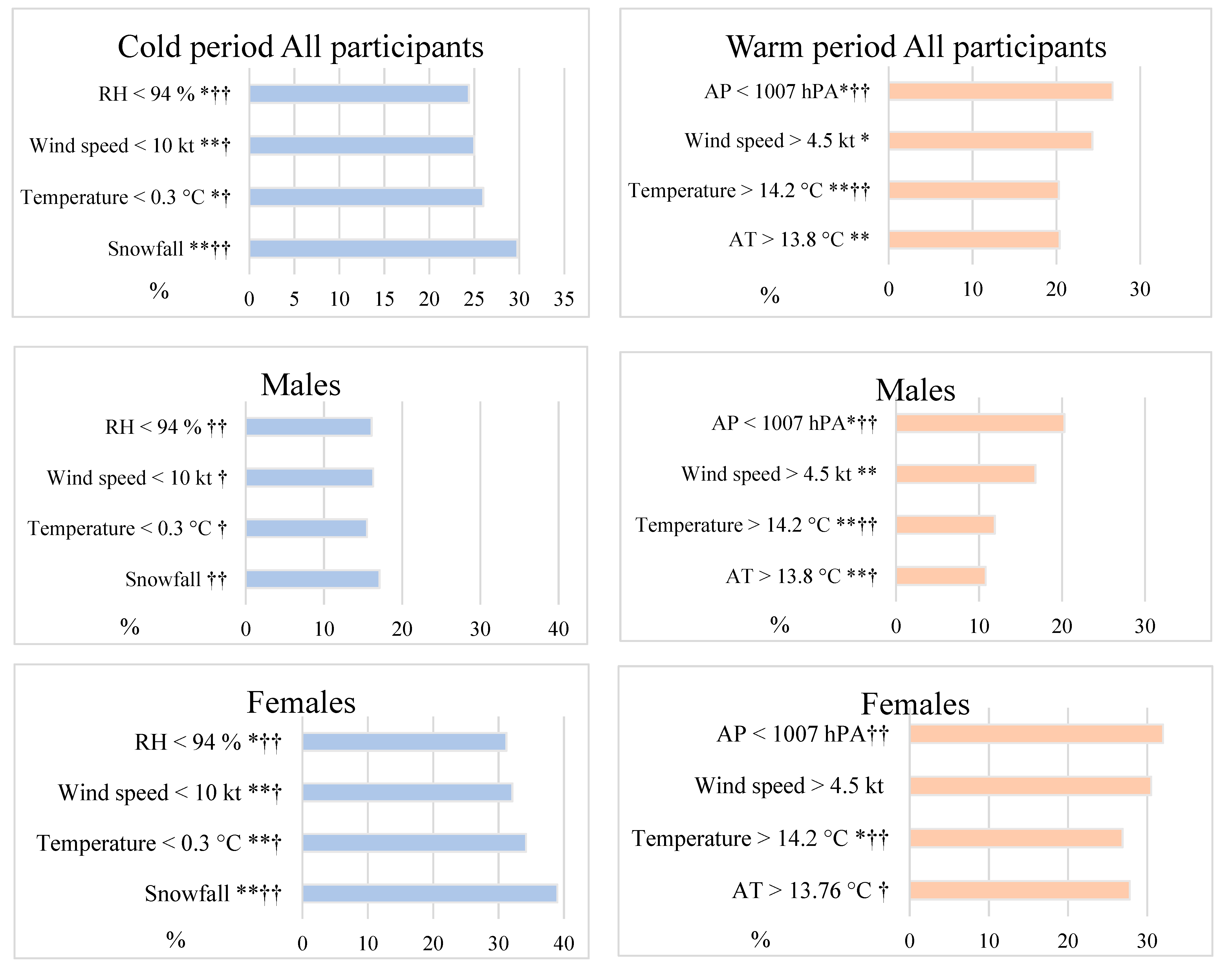
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pourshaikhian, M.; Moghadamnia, M.T.; Yekaninejad, M.S.; Ghanbari, A.; Rashti, A.S.; Kamachli, S.A. The effects of meteorological variables on ambulance attendance for cardiovascular diseases in Rasht, Iran. J. Therm. Biol. 2019, 83, 150–156. [Google Scholar] [CrossRef]
- Hu, J.; Hou, Z.; Xu, Y.; Zhou, M.; Zhou, C.; Xiao, Y.; Yu, M.; Huang, B.; Xu, X.; Lin, L.; et al. Life loss of cardiovascular diseases per death attributable to ambient temperature: A national time series analysis based on 364 locations in China. Sci. Total Environ. 2021, 756, 142614. [Google Scholar] [CrossRef] [PubMed]
- Ma, P.; Wang, S.; Zhou, J.; Li, T.; Fan, X.; Fan, J.; Wang, S. Meteorological rhythms of respiratory and circulatory diseases revealed by Harmonic Analysis. Heliyon 2020, 6, e04034. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.-S.; He, J.; Gao, S.-H.; Hu, B.-K.; Ma, S.-L. Correlation analysis for the attack of respiratory diseases and meteorological factors. Chin. J. Integr. Med. 2011, 17, 600–606. [Google Scholar] [CrossRef] [PubMed]
- Qi, X.; Wang, Z.; Xia, X.; Xue, J.; Gu, Y.; Han, S.; Wang, L.; Li, X.; Leng, S.X. Potential Impacts of Meteorological Variables on Acute Ischemic Stroke Onset. Risk Manag. Health Policy 2020, 13, 615–621. [Google Scholar] [CrossRef] [PubMed]
- Tamasauskiene, L.; Rastenyte, D.; Radisauskas, R.; Tamosiunas, A.; Tamasauskas, D.; Vaiciulis, V.; Kranciukaite-Butylkiniene, D.; Milinaviciene, E. Relationship of meteorological factors and acute stroke events in Kaunas (Lithuania) in 2000–2010. Environ. Sci. Pollut. Res. 2017, 24, 9286–9293. [Google Scholar] [CrossRef] [PubMed]
- Scheidt, J.; Koppe, C.; Rill, S.; Reinel, D.; Wogenstein, F.; Drescher, J. Influence of temperature changes on migraine occurrence in Germany. Int. J. Biometeorol. 2012, 57, 649–654. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wang, S.; Zhang, X.; Xie, M.; Zhao, D.; Zhang, H.; Zhang, Y.; Cheng, Q.; Bai, L.; Su, H. Effect of increasing temperature on daily hospital admissions for schizophrenia in Hefei, China: A time-series analysis. Public Health 2018, 159, 70–77. [Google Scholar] [CrossRef]
- Bulbena, A.; Pailhez, G.; Cunillera, J.; Rius, A.; Garcia-Ribera, C.; Rojo, C. Panic anxiety, under the weather? Int. J. Biometeorol. 2005, 49, 238–243. [Google Scholar] [CrossRef]
- Cruz-Pereira, J.S.; Rea, K.; Nolan, Y.M.; O’Leary, O.F.; Dinan, T.G.; Cryan, J.F. Depression’s Unholy Trinity: Dysregulated Stress, Immunity, and the Microbiome. Annu. Rev. Psychol. 2020, 71, 49–78. [Google Scholar] [CrossRef]
- Szyszkowicz, M.; Willey, J.B.; Grafstein, E.; Rowe, B.H.; Colman, I. Air Pollution and Emergency Department Visits for Suicide Attempts in Vancouver, Canada. Environ. Health Insights 2010, 4, EHIS5662. [Google Scholar] [CrossRef]
- Roberts, S.; Arseneault, L.; Barratt, B.; Beevers, S.; Danese, A.; Odgers, C.; Moffitt, T.; Reuben, A.; Kelly, F.J.; Fisher, H.L. Exploration of NO2 and PM2.5 air pollution and mental health problems using high-resolution data in London-based children from a UK longitudinal cohort study. Psychiatry Res. 2019, 272, 8–17. [Google Scholar] [CrossRef]
- Tsai, S.-S.; Chiu, Y.-W.; Weng, Y.-H.; Yang, C.-Y. Association between ozone air pollution levels and hospitalizations for depression in Taipei: A time-stratified case-crossover study. J. Toxicol. Environ. Health A 2020, 83, 596–603. [Google Scholar] [CrossRef]
- Kay, R.W. Geomagnetic Storms: Association with Incidence of Depression as Measured by Hospital Admission. Br. J. Psychiatry 1994, 164, 403–409. [Google Scholar] [CrossRef]
- O’Hare, C.; Sullivan, V.O.; Flood, S.; Kenny, R.A. Seasonal and meteorological associations with depressive symptoms in older adults: A geo-epidemiological study. J. Affect. Disord. 2016, 191, 172–179. [Google Scholar] [CrossRef]
- Díaz, J.; López-Bueno, J.A.; López-Ossorio, J.; Gónzález, J.; Sánchez, F.; Linares, C. Short-term effects of traffic noise on suicides and emergency hospital admissions due to anxiety and depression in Madrid (Spain). Sci. Total Environ. 2020, 710, 136315. [Google Scholar] [CrossRef]
- Zhang, Y.; Chen, Y.; Ma, L. Depression and cardiovascular disease in elderly: Current understanding. J. Clin. Neurosci. 2018, 47, 1–5. [Google Scholar] [CrossRef]
- Raič, M. Depression and Heart Diseases: Leading Health Problems. Psychiatr. Danub. 2017, 4, 770–777. [Google Scholar]
- Celano, C.M.; Huffman, J.C. Depression and Cardiac Disease. Cardiol. Rev. 2011, 19, 130–142. [Google Scholar] [CrossRef]
- Pinquart, M.; Duberstein, P. Depression and cancer mortality: A meta-analysis. Psychol. Med. 2010, 40, 1797–1810. [Google Scholar] [CrossRef]
- Bennett, S.; Thomas, A.J. Depression and dementia: Cause, consequence or coincidence? Maturitas 2014, 79, 184–190. [Google Scholar] [CrossRef] [PubMed]
- Connolly, M.; Yohannes, A. The impact of depression in older patients with chronic obstructive pulmonary disease and asthma. Maturitas 2016, 92, 9–14. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, S.; Nagayama, H. Depression in Parkinson’s disease. Seishin Shinkeigaku Zasshi 2013, 115, 1135–1141. [Google Scholar] [PubMed]
- Sivertsen, H.; Bjørkløf, G.H.; Engedal, K.; Selbaek, G.; Helvik, A.-S. Depression and Quality of Life in Older Persons: A Review. Dement. Geriatr. Cogn. Disord. 2015, 40, 311–339. [Google Scholar] [CrossRef]
- Han, K.; Yang, S.; Jia, W.; Wang, S.; Song, Y.; Cao, W.; Wang, J.; Liu, M.; He, Y. Health-Related Quality of Life and Its Correlation With Depression Among Chinese Centenarians. Front. Public Health 2020, 8, 580757. [Google Scholar] [CrossRef]
- Øverland, S.; Woicik, W.; Sikora, L.; Whittaker, K.; Heli, H.; Skjelkvåle, F.S.; Sivertsen, B.; Colman, I. Seasonality and symptoms of depression: A systematic review of the literature. Epidemiol. Psychiatr. Sci. 2019, 29, 1–15. [Google Scholar] [CrossRef]
- Park, D.; Kripke, D.F.; Cole, R.J. More Prominent Reactivity in Mood Than Activity and Sleep Induced by Differential Light Exposure Due to Seasonal and Local Differences. Chronobiol. Int. 2007, 24, 905–920. [Google Scholar] [CrossRef]
- Kerr, D.C.R.; Shaman, J.; Washburn, I.J.; Vuchinich, S.; Neppl, T.K.; Capaldi, D.M.; Conger, R.D. Two longterm studies of seasonal variation in depressive symptoms among community participants. J. Affect. Disord. 2013, 151, 837–842. [Google Scholar] [CrossRef]
- Winthorst, W.H.; Post, W.J.; Meesters, Y.; Penninx, B.W.; Nolen, W.A. Seasonality in depressive and anxiety symptoms among primary care patients and in patients with depressive and anxiety disorders; results from the Netherlands Study of Depression and Anxiety. BMC Psychiatry 2011, 11, 198. [Google Scholar] [CrossRef]
- Schlager, D.; Schwartz, J.E.; Bromet, E.J. Seasonal Variations of Current Symptoms in a Healthy Population. Br. J. Psychiatry 1993, 163, 322–326. [Google Scholar] [CrossRef]
- Harmatz, M.G.; Well, A.D.; Overtree, C.E.; Kawamura, K.Y.; Rosal, M.C.; Ockene, I.S. Seasonal Variation of Depression and Other Moods: A Longitudinal Approach. J. Biol. Rhythm. 2000, 15, 344–350. [Google Scholar] [CrossRef]
- Cianconi, P.; Betrò, S.; Janiri, L. The Impact of Climate Change on Mental Health: A Systematic Descriptive Review. Front. Psychiatry 2020, 11, 74. [Google Scholar] [CrossRef]
- González, P.; Nuñez, A.; Merz, E.; Brintz, C.; Weitzman, O.; Navas, E.L.; Camacho, A.; Buelna, C.; Penedo, F.J.; Wassertheil-Smoller, S.; et al. Measurement properties of the Center for Epidemiologic Studies Depression Scale (CES-D 10): Findings from HCHS/SOL. Psychol. Assess. 2017, 29, 372–381. [Google Scholar] [CrossRef]
- Mohebbi, M.; Nguyen, V.; McNeil, J.; Woods, R.L.; Nelson, M.R.; Shah, R.C.; Storey, E.; Murray, A.M.; Reid, C.M.; Kirpach, B.; et al. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. Gen. Hosp. Psychiatry 2018, 51, 118–125. [Google Scholar] [CrossRef]
- Irwin, M.; Artin, K.H.; Oxman, M.N. ASPREE Investigator Group. Psychometric properties of a short form of the Center for Epidemiologic Studies Depression (CES-D-10) scale for screening depressive symptoms in healthy community dwelling older adults. Arch. Intern. Med. 1999, 159, 1701–1704. [Google Scholar] [CrossRef]
- Zanobetti, A.; Schwartz, J. Temperature and Mortality in Nine US Cities. Epidemiology 2008, 19, 563–570. [Google Scholar] [CrossRef]
- Breiman, L.; Friedman, J.H.; Olshen, R.A.; Stone, C.J. Classification and Regression Trees, 1st ed.; Routledge: Boca Raton, FL, USA, 2017. [Google Scholar] [CrossRef]
- Perez, V.; Alexander, D.D.; Bailey, W.H. Air ions and mood outcomes: A review and meta-analysis. BMC Psychiatry 2013, 13, 29. [Google Scholar] [CrossRef]
- Li, Y.; Guo, X.; Wang, T.; Zhao, Y.; Zhang, H.; Wang, W. Characteristics of Atmospheric Small Ions and Their Application to Assessment of Air Quality in a Typical Semi-Arid City of Northwest China. Aerosol Air Qual. Res. 2015, 15, 865–874. [Google Scholar] [CrossRef]
- Jiang, S.-Y.; Ma, A.; Ramachandran, S. Negative Air Ions and Their Effects on Human Health and Air Quality Improvement. Int. J. Mol. Sci. 2018, 19, 2966. [Google Scholar] [CrossRef]
- Ryushi, T.; Kita, I.; Sakurai, T.; Yasumatsu, M.; Isokawa, M.; Aihara, Y.; Hama, K. The effect of exposure to negative air ions on the recovery of physiological responses after moderate endurance exercise. Int. J. Biometeorol. 1998, 41, 132–136. [Google Scholar] [CrossRef]
- Garcia-Carretero, L.; Llorca, G.; Villoria, M.J.; Blazquez, J.M.; Ledesma, A. Relaciones entre las urgencias psiquiatricas y losfactores meteorologicos. Actas Luso Esp. Neurol. Psiquiatr. 1989, 17, 59–67. [Google Scholar]
- Schory, T.J.; Piecznski, N.; Nair, S.; El-Mallakh, R.S. Barometric Pressure, Emergency Psychiatric Visits, and Violent Acts. Can. J. Psychiatry 2003, 48, 624–627. [Google Scholar] [CrossRef]
- Okuma, H.; Okuma, Y.; Kitagawa, Y. Examination of fluctuations in atmospheric pressure related to migraine. SpringerPlus 2015, 4, 1–4. [Google Scholar] [CrossRef]
- Frutos, A.M.; Sloan, C.D.; Merrill, R.M. Modeling the effects of atmospheric pressure on suicide rates in the USA using geographically weighted regression. PLoS ONE 2018, 13, e0206992. [Google Scholar] [CrossRef]
- Hiltunen, L.; Ruuhela, R.; Ostamo, A.; Lönnqvist, J.; Suominen, K.; Partonen, T. Atmospheric pressure and suicide attempts in Helsinki, Finland. Int. J. Biometeorol. 2012, 56, 1045–1053. [Google Scholar] [CrossRef]
- Mizoguchi, H.; Fukaya, K.; Mori, R.; Itoh, M.; Funakubo, M.; Sato, J. Lowering barometric pressure aggravates depression-like behavior in rats. Behav. Brain Res. 2011, 218, 190–193. [Google Scholar] [CrossRef]
- Kesserwani, H. Migraine Triggers: An Overview of the Pharmacology, Biochemistry, Atmospherics, and Their Effects on Neural Networks. Cureus 2021, 13, 14243. [Google Scholar] [CrossRef]
- Hajat, S. Health effects of milder winters: A review of evidence from the United Kingdom. Environ. Health 2017, 16, 109. [Google Scholar] [CrossRef]
- Donaldson, G.; Witt, C.; Näyhä, S. Changes in cold-related mortalities between 1995 and 2016 in South East England. Public Health 2019, 169, 36–40. [Google Scholar] [CrossRef]
- Silveira, I.H.; Cortes, T.R.; Oliveira, B.F.A.; Junger, W.L. Temperature and cardiovascular mortality in Rio de Janeiro, Brazil: Effect modification by individual-level and neighbourhood-level factors. J. Epidemiol. Community Health 2020, 75, 69–75. [Google Scholar] [CrossRef]
- Culbertson, F.M. Depression and gender: An international review. Am. Psychol. 1997, 52, 25–31. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.-Y.; Park, J.-H.; Lee, M.Y.; Oh, K.-S.; Shin, D.-W.; Shin, Y.-C. Physical activity and the prevention of depression: A cohort study. Gen. Hosp. Psychiatry 2019, 60, 90–97. [Google Scholar] [CrossRef] [PubMed]
- Villarreal-Zegarra, D.; Cabrera-Alva, M.; Carrillo-Larco, R.M.; Bernabe-Ortiz, A. Trends in the prevalence and treatment of depressive symptoms in Peru: A population-based study. BMJ Open 2020, 10, e036777. [Google Scholar] [CrossRef] [PubMed]
- Huibers, M.J.; de Graaf, L.E.; Peeters, F.; Arntz, A. Does the weather make us sad? Meteorological determinants of mood and depression in the general population. Psychiatry Res. 2010, 180, 143–146. [Google Scholar] [CrossRef]
- Jayamohananan, H.; Kumar, M.K.M.; P, A.T. 5-HIAA as a Potential Biological Marker for Neurological and Psychiatric Disorders. Adv. Pharm. Bull. 2019, 9, 374–381. [Google Scholar] [CrossRef]
- Luykx, J.J.; Bakker, S.C.; Van Geloven, N.; Eijkemans, M.J.C.; Horváth, S.; Lentjes, E.; Boks, M.P.M.; Strengman, E.; Deyoung, J.E.; Buizer-Voskamp, J.; et al. Seasonal variation of serotonin turnover in human cerebrospinal fluid, depressive symptoms and the role of the 5-HTTLPR. Transl. Psychiatry 2013, 3, e311. [Google Scholar] [CrossRef]
- Oniszczenko, W. Affective Temperaments and Meteoropathy Among Women: A Cross-sectional Study. PLoS ONE 2020, 15, e0232725. [Google Scholar] [CrossRef]
- Infortuna, C.; Gratteri, F.; Benotakeia, A.; Patel, S.; Fleischman, A.; Muscatello, M.R.A.; Bruno, A.; Zoccali, R.A.; Chusid, E.; Han, Z.; et al. Exploring the Gender Difference and Predictors of Perceived Stress among Students Enrolled in Different Medical Programs: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 6647. [Google Scholar] [CrossRef]
- Infortuna, C.; Mineo, L.; Buffer, S.; Thomas, F.P.; Muscatello, M.R.A.; Aguglia, E.; Bruno, A.; Zoccali, R.A.; Sheikh, A.; Chusid, E.; et al. Acute social and somatic stress alters cortical metaplasticity probed with non-invasive brain stimulation in humans. Int. J. Psychophysiol. 2021, 170, 1–5. [Google Scholar] [CrossRef]

| Characteristic | Depressive Symptoms N (%) | p Value | ||
|---|---|---|---|---|
| No | Yes | |||
| Sex | Male | 2655 (84.4) | 490 (15.6) | <0.001 |
| Female | 2659 (70.1) | 1133 (29.9) | ||
| Age groups (years) | <50 | 635 (79.1) | 168 (20.9) | 0.037 |
| 50–69 | 3994 (76.7) | 1213 (23.3) | ||
| ≥70 | 685 (73.9) | 242 (26.1) | ||
| * BMI (kg/m²) | <25 | 1095 (76.9) | 329 (23.1) | <0.001 |
| 25–29.9 | 2153 (78.8) | 579 (21.2) | ||
| ≥30 | 2066 (74.3) | 715 (25.7) | ||
| Smoking status (male) | Never | 1052 (86.7) | 163 (13.3) | 0.012 |
| Former | 813 (83.7) | 158 (16.3) | ||
| Regular/occasional | 790 (82.2) | 171 (17.8) | ||
| Smoking status (female) | Never | 2221 (70.5) | 931 (29.5) | 0.533 |
| Former | 183 (67.5) | 88 (32.5) | ||
| Regular/occasional | 254 (69.0) | 114 (31.0) | ||
| Marital status | Single | 200 (71.9) | 78 (28.1) | <0.001 |
| Married | 3889 (81.6) | 878 (18.4) | ||
| Divorced | 565 (67.0) | 278 (33.0) | ||
| Widowed | 597 (61.8) | 369 (38.2) | ||
| Cohabiting without marriage | 63 (75.9) | 20 (24.1) | ||
| Education | Primary | 350 (71.0) | 143 (29.0) | <0.001 |
| Vocational | 469 (72.2) | 181 (27.8) | ||
| Secondary | 1454 (75.4) | 475 (24.6) | ||
| Advanced vocational | 1193 (74.9) | 400 (25.1) | ||
| University | 1848 (81.3) | 424 (18.7) | ||
| Ischemic heart disease | Yes | 935 (70.1) | 399 (29.9) | <0.001 |
| No | 4379 (78.2) | 1224 (21.8) | ||
| Medications taken for high blood pressure during the last 2 weeks | Yes | 1993 (73.0) | 739 (27.0) | <0.001 |
| No | 3310 (79.0) | 881 (21.0) | ||
| Physical activity | Yes | 4047 (78.1) | 1136 (21.9) | <0.001 |
| No | 1264 (72.3) | 485 (27.7) | ||
| Variable | OR (95% CI) | p |
|---|---|---|
| Female sex | 2.19 (1.90–2.54) | <0.001 |
| Smoking (former/regular/occasional) | 1.19 (1.03–1.37) | 0.015 |
| Cohabiting without marriage | 1 | |
| Single | 1.40 (1.06–1.86) | 0.020 |
| Divorced/widowed | 1.92 (1.69–2.18) | <0.001 |
| Education (university) | 1 | |
| Education (primary/vocational) | 1.57 (1.31–1.88) | <0.001 |
| Education (secondary/advanced vocational) | 1.36 (1.19–1.56) | <0.001 |
| IHD | 1.39 (1.21–1.61) | <0.001 |
| AH | 1.25 (1.11–1.41) | <0.001 |
| Physical inactivity | 1.49 (1.31–1.70) | <0.001 |
| November-December | 1.25 (1.06–1.48) | 0.008 |
| Relative humidity < 94% with a lag of 2 days | 1.32 (1.07–1.61) | 0.009 |
| Rising wind (WS on the previous day < 6 & WS > 4.5) | 1.31 (1.14–1.49) | <0.001 |
| Snowfall during the cold period 2 days before | 1.28 (1.01–1.64) | 0.042 |
| Temperature > 14.2 °C with a lag of 2 days | 0.79 (0.67–0.93) | 0.006 |
| Variable | OR (95% CI) | p |
|---|---|---|
| Males | ||
| Rising wind (WS on the previous day < 6 & WS > 4.5) | 1.40 (1.11–1.75) | 0.004 |
| Temperature > 14.2 °C with a lag of 2 days | 0.69 (0.51–0.93) | 0.013 |
| Atmospheric pressure < 1009 hPa with a lag of 2 days | 1.28 (1.04–1.59) | 0.023 |
| Females | ||
| March–April | 1.24 (1.04–1.49) | 0.020 |
| November–December | 1.38 (1.12–1.70) | 0.002 |
| Rising wind (WS on the previous day < 6 & WS > 4.5) | 1.28 (1.09–1.51) | 0.003 |
| Snowfall at cold period before 2 days | 1.55 (1.16–2.07) | 0.004 |
| Relative humidity < 83% on the previous day | 1.26 (1.08–1.48) | 0.004 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brazienė, A.; Venclovienė, J.; Vaičiulis, V.; Lukšienė, D.; Tamošiūnas, A.; Milvidaitė, I.; Radišauskas, R.; Bobak, M. Relationship between Depressive Symptoms and Weather Conditions. Int. J. Environ. Res. Public Health 2022, 19, 5069. https://doi.org/10.3390/ijerph19095069
Brazienė A, Venclovienė J, Vaičiulis V, Lukšienė D, Tamošiūnas A, Milvidaitė I, Radišauskas R, Bobak M. Relationship between Depressive Symptoms and Weather Conditions. International Journal of Environmental Research and Public Health. 2022; 19(9):5069. https://doi.org/10.3390/ijerph19095069
Chicago/Turabian StyleBrazienė, Agnė, Jonė Venclovienė, Vidmantas Vaičiulis, Dalia Lukšienė, Abdonas Tamošiūnas, Irena Milvidaitė, Ričardas Radišauskas, and Martin Bobak. 2022. "Relationship between Depressive Symptoms and Weather Conditions" International Journal of Environmental Research and Public Health 19, no. 9: 5069. https://doi.org/10.3390/ijerph19095069
APA StyleBrazienė, A., Venclovienė, J., Vaičiulis, V., Lukšienė, D., Tamošiūnas, A., Milvidaitė, I., Radišauskas, R., & Bobak, M. (2022). Relationship between Depressive Symptoms and Weather Conditions. International Journal of Environmental Research and Public Health, 19(9), 5069. https://doi.org/10.3390/ijerph19095069









