Talking about Climate Change and Environmental Degradation with Patients in Primary Care: A Cross-Sectional Survey on Knowledge, Potential Domains of Action and Points of View of General Practitioners
Abstract
1. Introduction
2. Method
2.1. Study Design
2.2. Contact Procedure
2.3. Variables of Interest
2.3.1. Environmental Degradation Knowledge and the Impact on Health
2.3.2. Willingness to Address Climate Change with Patients
2.3.3. Exemplarity and Role Model
2.3.4. Demographic Characteristics
3. Data Analysis
4. Results
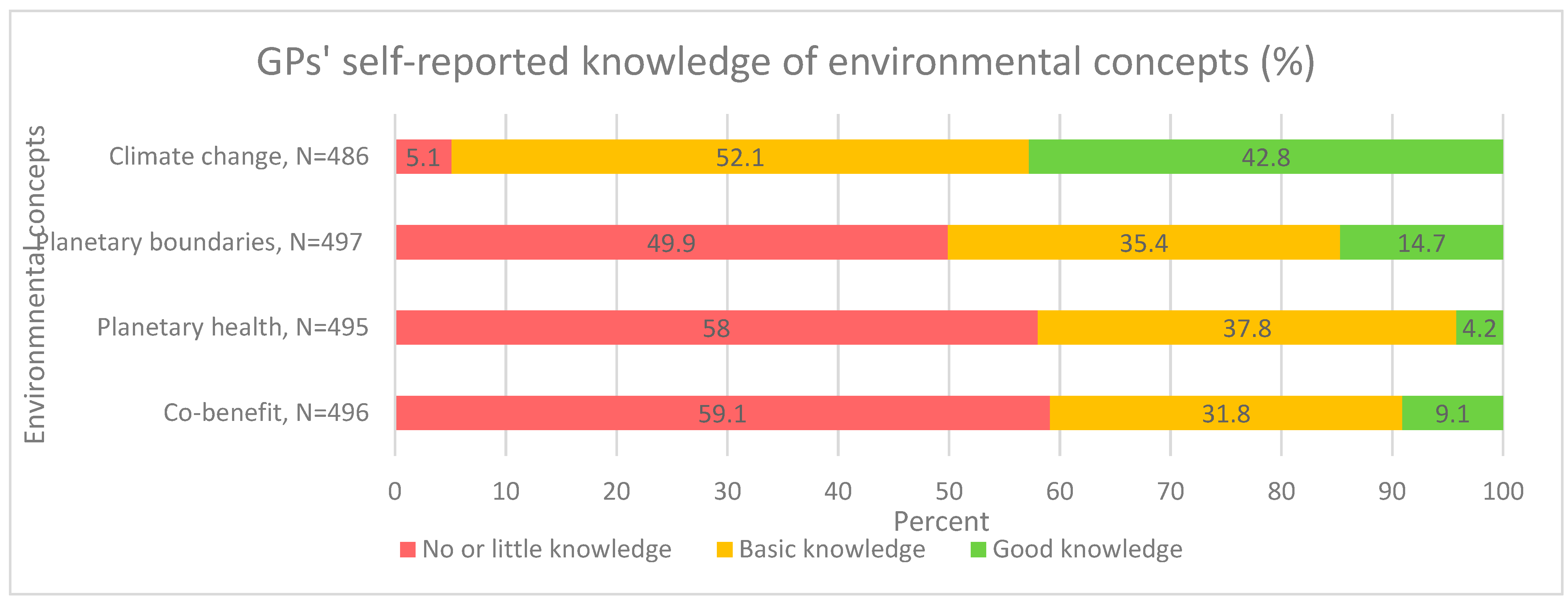
4.1. General Knowledge of Environmental Issues
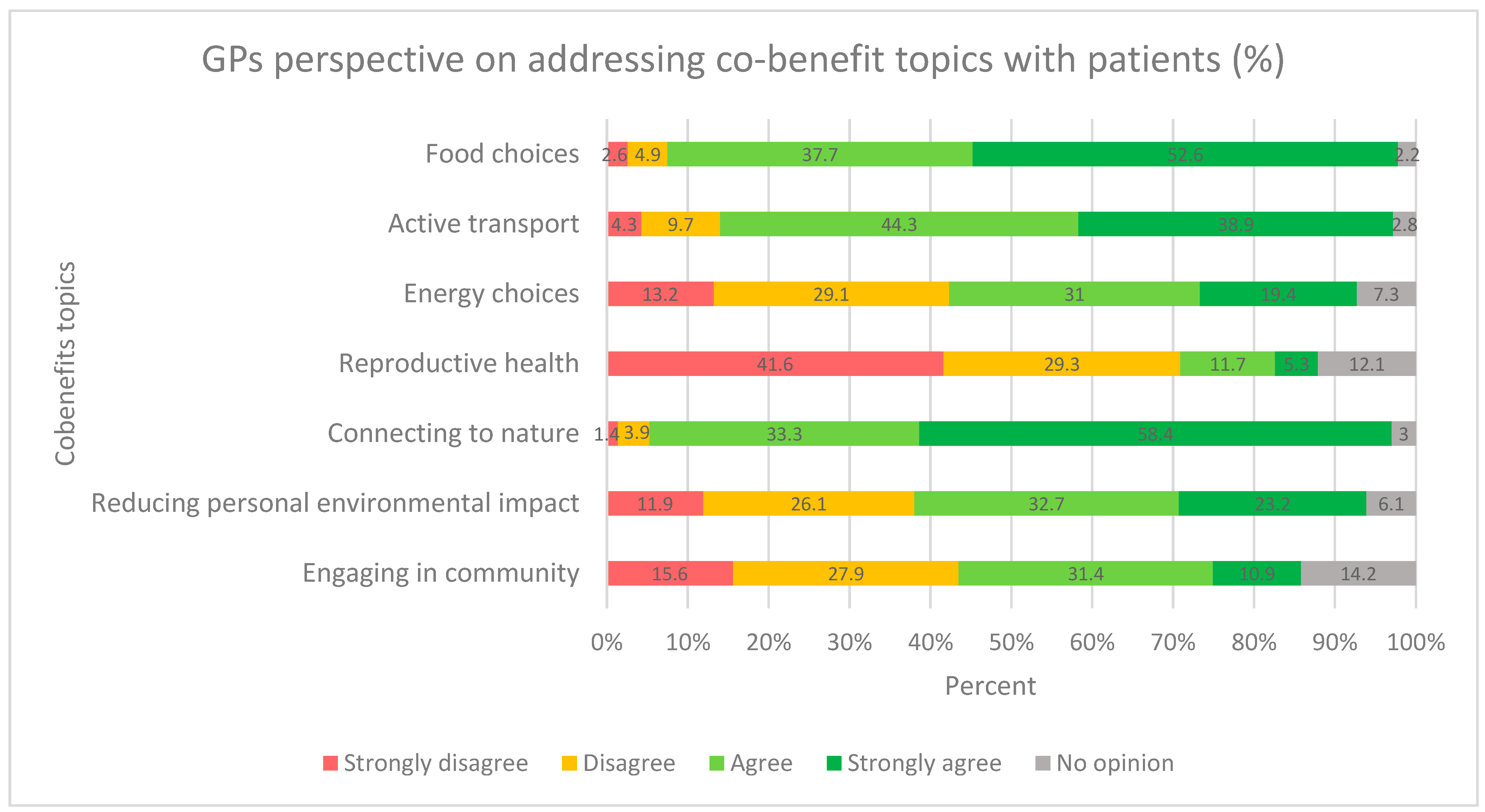
4.2. Willingness to Address Climate Change with Patients
4.3. Training and Source of Information
4.3.1. Exemplarity and Role Models
4.3.2. Influence of Demographic Factors on Respondents’ Answers
5. Discussion
5.1. Concerns and Knowledge Regarding Climate and the Ecological Emergency
5.2. Developing Interventions for the Clinical Setting
6. Strength and Limitations
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Berry, H.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; et al. The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. Lancet Lond Engl. 2018, 392, 2479–2514. [Google Scholar] [CrossRef]
- Steffen, W.; Richardson, K.; Rockstrom, J.; Cornell, S.E.; Fetzer, I.; Bennett, E.M.; Biggs, R.; Carpenter, S.R.; De Vries, W.; De Wit, C.A.; et al. Planetary boundaries: Guiding human development on a changing planet. Science 2015, 347, 1259855. [Google Scholar] [CrossRef] [PubMed]
- Intergovernmental Panel on Climate Change. Global Warming of 1.5 °C. 2019. Available online: http://www.ipcc.ch/report/sr15/ (accessed on 18 April 2020).
- Maibach, E.W.; Kreslake, J.M.; Roser-Renouf, C.; Rosenthal, S.; Feinberg, G.; Leiserowitz, A.A. Do Americans Understand That Global Warming Is Harmful to Human Health? Evidence From a National Survey. Ann. Glob. Health 2015, 81, 396–409. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Chen, R.; Sera, F.; Vicedo-Cabrera, A.M.; Guo, Y.; Tong, S.; Coelho, M.S.Z.S.; Saldiva, P.H.N.; Lavigne, E.; Matus, P.; et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019, 381, 705–715. [Google Scholar] [CrossRef]
- Kim, Y.; Kim, H.; Gasparrini, A.; Armstrong, B.; Honda, Y.; Chung, Y.; Ng, C.F.; Tobias, A.; Íñiguez, C.; Lavigne, E.; et al. Suicide and Ambient Temperature: A Multi-Country Multi-City Study. Environ. Health Perspect. 2019, 127, 117007. [Google Scholar] [CrossRef]
- Karliner, J.; Slotterback, S.; Boyd, R.; Ashby, B.; Steele, K. Health Care’s Climate Footprint: How the Health Sector Contributes to the Global Climate Crisis and Opportunities for Action. Eur. J. Public Health 2020, 30, ckaa165.843. [Google Scholar] [CrossRef]
- Thiel, C.; Duncan, P.; Woods, N. Attitude of US obstetricians and gynaecologists to global warming and medical waste. J. Health Serv. Res. Policy 2017, 22, 162–167. [Google Scholar] [CrossRef]
- Storz, M.A. A Practical Guide for Physicians and Health Care Workers to Reduce Their Carbon Footprint in Daily Clinical Work. Perm. J. 2018, 22. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5882189/ (accessed on 6 October 2020). [CrossRef]
- MacNeill, A.J.; McGain, F.; Sherman, J.D. Planetary health care: A framework for sustainable health systems. Lancet Planet Health 2021, 5, e66–e68. [Google Scholar] [CrossRef]
- Rockström, J.; Steffen, W.; Noone, K.; Persson, Å.; Chapin, F.S.I.; Lambin, E.; Lenton, T.M.; Scheffer, M.; Folke, C.; Schellnhuber, H.J.; et al. Planetary Boundaries: Exploring the Safe Operating Space for Humanity. Ecol. Soc. 2009, 14, 32. [Google Scholar] [CrossRef]
- Kotcher, J.; Maibach, E.; Miller, J.; Campbell, E.; Alqodmani, L.; Maiero, M.; Wyns, A. Views of health professionals on climate change and health: A multinational survey study. Lancet Planet. Health 2021, 5, e316–e323. [Google Scholar] [CrossRef]
- Maibach, E.W.; Sarfaty, M.; Mitchell, M.; Gould, R. Limiting global warming to 1.5 to 2.0 °C—A unique and necessary role for health professionals. PLoS Med. 2019, 16, e1002804. [Google Scholar] [CrossRef] [PubMed]
- Xie, E.; de Barros, E.F.; Abelsohn, A.; Stein, A.T.; Haines, A. Challenges and opportunities in planetary health for primary care providers. Lancet Planet Health 2018, 2, e185–e187. [Google Scholar] [CrossRef]
- Holguera, J.G.; Niwa, N.; Senn, P.N. Health & Environment Co-benefits: Concepts and recommendations for clinical practice. Rev. Médicale Suisse 2020, 8, 5–35. [Google Scholar]
- Quam, V.G.M.; Rocklöv, J.; Quam, M.B.M.; Lucas, R.A.I. Assessing Greenhouse Gas Emissions and Health Co-Benefits: A Structured Review of Lifestyle-Related Climate Change Mitigation Strategies. Int. J. Environ. Res. Public Health 2017, 14, 468. [Google Scholar] [CrossRef]
- Ekins, P.; Gupta, J. Perspective: A healthy planet for healthy people. Glob. Sustain. 2019, 2, e20. [Google Scholar] [CrossRef]
- Willett, W.; Rockström, J.; Loken, B.; Springmann, M.; Lang, T.; Vermeulen, S.; Garnett, T.; Tilman, D.; DeClerck, F.; Wood, A.; et al. Food in the Anthropocene: The EAT–Lancet Commission on healthy diets from sustainable food systems. Lancet 2019, 393, 447–492. [Google Scholar] [CrossRef]
- WONCA; Planetary Health Alliance; Clinicians for Planetary Health. Declaration Calling for Family Doctors of the World to Act on Planetary Health. 2019. Available online: www.globalfamilydoctor.com/Decplanethealth (accessed on 6 April 2020).
- Sibbald, B. Physicians’ roles on the front line of climate change. CMAJ Can. Med. Assoc. J. 2013, 185, 195. [Google Scholar] [CrossRef][Green Version]
- Temte, J.L.; McCall, J.C. Patient attitudes toward issues of environmental health. Wilderness Environ. Med. 2001, 12, 86–92. [Google Scholar] [CrossRef]
- Sarfaty, M.; Mitchell, M.; Bloodhart, B.; Maibach, E.W. A Survey of African American Physicians on the Health Effects of Climate Change. Int. J. Environ. Res. Public Health 2014, 11, 12473–12485. [Google Scholar] [CrossRef]
- Sarfaty, M.; Kreslake, J.M.; Casale, T.B.; Maibach, E.W. Views of AAAAI members on climate change and health. J. Allergy Clin. Immunol. Pract. 2016, 4, 333–335.e26. [Google Scholar] [CrossRef]
- Sarfaty, M.; Bloodhart, B.; Ewart, G.; Thurston, G.D.; Balmes, J.R.; Guidotti, T.L.; Maibach, E. American Thoracic Society Member Survey on Climate Change and Health. Ann. Am. Thorac. Soc. 2015, 12, 274–278. [Google Scholar] [CrossRef]
- Boland, T.M.; Temte, J.L. Family Medicine Patient and Physician Attitudes Toward Climate Change and Health in Wisconsin. Wilderness Environ. Med. 2019, 30, 386–393. [Google Scholar] [CrossRef]
- Crowley, R.A.; Health and Public Policy Committee of the American College of Physicians. Climate Change and Health: A Position Paper of the American College of Physicians. Ann. Intern. Med. 2016, 164, 608–610. [Google Scholar] [CrossRef]
- Iacobucci, G. Planetary Health: WONCA Urges Family Doctors to Commit to Action. BMJ 2019, 364, l1002. Available online: https://www.bmj.com/content/364/bmj.l1002 (accessed on 18 April 2020). [CrossRef]
- Veidis, E.M.; Myers, S.S.; Almada, A.A.; Golden, C.D. A call for clinicians to act on planetary health. Lancet 2019, 393, 2021. [Google Scholar] [CrossRef]
- Gardner, C.J.; Thierry, A.; Rowlandson, W.; Steinberger, J.K. From Publications to Public Actions: The Role of Universities in Facilitating Academic Advocacy and Activism in the Climate and Ecological Emergency. Front. Sustain. 2021, 2, 42. Available online: https://www.frontiersin.org/articles/10.3389/frsus.2021.679019/full (accessed on 11 August 2021). [CrossRef]
- Rieser, R.; Quinto, C.B.; Weil, B. Le chemin se fait en marchant. Bull Médecins Suisses 2021, 102, 1394–1396. [Google Scholar] [CrossRef]
- Dupraz, J.; Burnand, B. Role of Health Professionals Regarding the Impact of Climate Change on Health—An Exploratory Review. Int. J. Environ. Res. Public Health 2021, 18, 3222. [Google Scholar] [CrossRef]
- Redvers, N. Patient-Planetary Health Co-Benefit Prescribing: Emerging Considerations for Health Policy and Health Professional Practice. Front. Public Health. 2021, 9, 499. Available online: https://www.frontiersin.org/articles/10.3389/fpubh.2021.678545/full (accessed on 11 August 2021). [CrossRef]
- Brown, B.P.; Chor, J. What Are Risks and Benefits of Not Incorporating Information about Population Growth and Its Impact on Climate Change into Reproductive Care? AMA J. Ethics 2017, 19, 1157–1163. [Google Scholar] [PubMed]
- Gifford, R. The Dragons of Inaction: Psychological Barriers That Limit Climate Change Mitigation and Adaptation. Am. Psychol. 2011, 66, 290–302. [Google Scholar] [CrossRef] [PubMed]
- Joinson, A. Social desirability, anonymity, and Internet-based questionnaires. Behav. Res. Methods Instrum Comput. J. Psychon. Soc. Inc. 1999, 31, 433–438. [Google Scholar] [CrossRef] [PubMed]
- Sebo, P.; Maisonneuve, H.; Cerutti, B.; Fournier, J.P.; Senn, N.; Haller, D.M. Rates, Delays, and Completeness of General Practitioners’ Responses to a Postal Versus Web-Based Survey: A Randomized Trial. J. Med. Internet Res. 2017, 19, e83. [Google Scholar] [CrossRef]
| N (%) | Total of Respondents N | |
|---|---|---|
| Age (y) mean ± SD | 52 ± 11.4 | 493 |
| 30–45 | 167 (33, 9) | |
| 46–60 | 207 (42) | |
| >60 | 116 (24, 1) | |
| Gender | ||
| Female | 261 (52, 7) | 495 |
| Male | 234 (47, 3) | |
| Years in practice (y) mean ± SD | 25 ± 11 | 484 |
| Primary work site | ||
| Urban | 284 (57, 4) | 495 |
| Semi-urban | 124 (25) | |
| Rural | 87 (17, 6) | |
| Type of office | ||
| Alone | 155 (31, 6) | 491 |
| Group office | 336 (68, 4) | |
| Primary work setting | ||
| Private | 471 (96, 1) | 491 |
| Public | 19 (3, 9) | |
| Active in associative activity | ||
| Private | 98 (20) | 490 |
| Professional | 32 (6, 6) | 487 |
| Political affiliation | ||
| Right wing/Conservative | 106 (21, 3) | 432 |
| Left wing/Liberal | 172 (34, 6) | |
| Other political affiliation | 11 (2, 2) | |
| No political affiliation | 143 (28, 8) |
| Strongly Agree | Agree | Disagree | Strongly Disagree | No Opinion | N | |
|---|---|---|---|---|---|---|
| Clinical practice should be adapted to health impacts of climate change | 100 (20.1) | 295 (59.4) | 52 (10.5) | 14 (2.8) | 36 (7.2) | 497 |
| GPs have a role in providing information to patients about climate change and its links to human health | 187 (37.6) | 224 (45.1) | 46 (9.3) | 20 (4) | 20 (4) | 497 |
| I feel comfortable advising patients about the health impact of climate change | 35 (7.1) | 169 (34.1) | 194 (39.1) | 62 (12.5) | 36 (7.3) | 496 |
| Variables | Feels Comfortable Addressing Climate Change with Patients | Willingness to Integrate the Theme of Climate Change into the Clinical Care Setting | Willingness to Adapt the Clinical Setting to Climate Change Consequences | Willingness to Be a Model Role for the Population in Terms of Sustainability | Willingness to Provide Patients Information about Health Impact of Climate Change | Climate Change Topic Addressed in Consultation | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | OR (95% CI) | p-Value | |
| Age (by 5 years) | 1.05 (1.03–1.07) | <0.01 | 1.04 (1.02–1.07) | <0.01 | 1.01 (0.98–1.04) | 0.50 | 1.03 (1.01–1.06) | 0.01 | 1.04 (1.01–1.07) | 0.01 | 1.07 (1.04–1.1) | <0.01 |
| Sex (Reference = women) | 0.81 (0.52–1.27) | 0.36 | 1.31 (0.77–2.23) | 0.32 | 1.21 (0.65–2.28) | 0.55 | 1.13 (0.63–2.04) | 0.69 | 1.64 (0.88–3.13) | 0.13 | 1.62 (0.87–3.05) | 0.13 |
| Place of practice (Reference = Urban) | ||||||||||||
| Semi-urban | 1.21 (0.73–2.02) | 0.46 | 1.25 (0.69–2.32) | 0.47 | 1.34 (0.68–2.80) | 0.42 | 1.1 (0.58–2.15) | 0.77 | 1.10 (0.58–2.24) | 0.79 | 0.87 (0.43–1.71) | 0.7 |
| Rural | 1.14 (0.64–2.02) | 0.65 | 0.76 (0.4–1.48) | 0.41 | 1.36 | 0.47 | 1.74 (0.79–4.29) | 0.19 | 1.74 (0.79–2.99) | 0.58 | 0.97 (0.43–2.03) | 0.93 |
| Political orientation (Reference = Without) | ||||||||||||
| Left wing | 1.94 (1.19–3.20) | <0.01 | 2.34 (1.29–4.30) | <0.01 | 2.93 (1.47–6.06) | <0.01 | 3.66 (1.79–7.87) | <0.001 | 3.66 (1.79–5.90) | 0.009 | 1.15 (0.62–2.17) | 0.65 |
| Right wing | 0.94 (0.53–1.66) | 0.83 | 0.66 (0.36–1.19) | 0.17 | 1.52 (0.76–3.14) | 0.25 | 0.67 (0.36–1.25) | 0.21 | 0.67 (0.36–1.40) | 0.33 | 0.4 (0.16–0.89) | 0.03 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
André, H.; Gonzalez Holguera, J.; Depoux, A.; Pasquier, J.; Haller, D.M.; Rodondi, P.-Y.; Schwarz, J.; Senn, N. Talking about Climate Change and Environmental Degradation with Patients in Primary Care: A Cross-Sectional Survey on Knowledge, Potential Domains of Action and Points of View of General Practitioners. Int. J. Environ. Res. Public Health 2022, 19, 4901. https://doi.org/10.3390/ijerph19084901
André H, Gonzalez Holguera J, Depoux A, Pasquier J, Haller DM, Rodondi P-Y, Schwarz J, Senn N. Talking about Climate Change and Environmental Degradation with Patients in Primary Care: A Cross-Sectional Survey on Knowledge, Potential Domains of Action and Points of View of General Practitioners. International Journal of Environmental Research and Public Health. 2022; 19(8):4901. https://doi.org/10.3390/ijerph19084901
Chicago/Turabian StyleAndré, Hélène, Julia Gonzalez Holguera, Anneliese Depoux, Jérôme Pasquier, Dagmar M. Haller, Pierre-Yves Rodondi, Joëlle Schwarz, and Nicolas Senn. 2022. "Talking about Climate Change and Environmental Degradation with Patients in Primary Care: A Cross-Sectional Survey on Knowledge, Potential Domains of Action and Points of View of General Practitioners" International Journal of Environmental Research and Public Health 19, no. 8: 4901. https://doi.org/10.3390/ijerph19084901
APA StyleAndré, H., Gonzalez Holguera, J., Depoux, A., Pasquier, J., Haller, D. M., Rodondi, P.-Y., Schwarz, J., & Senn, N. (2022). Talking about Climate Change and Environmental Degradation with Patients in Primary Care: A Cross-Sectional Survey on Knowledge, Potential Domains of Action and Points of View of General Practitioners. International Journal of Environmental Research and Public Health, 19(8), 4901. https://doi.org/10.3390/ijerph19084901






