Differences in Puberty of Girls before and during the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Brito, V.N.; Latronico, A.C. Puberty: When Is It Normal? Arch. Endocrinol. Metab. 2015, 59, 93–94. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Feibelmann, T.C.M.; da Silva, A.P.; Resende, D.C.S.; de Resende, E.A.M.R.; Scatena, L.M.; Borges, M.d.F. Puberty in a Sample of Brazilian Schoolgirls: Timing and Anthropometric Characteristics. Arch. Endocrinol. Metab. 2015, 59, 105–111. [Google Scholar] [CrossRef] [PubMed]
- Khan, L. Puberty: Onset and Progression. Pediatric Ann. 2019, 48, e141–e145. [Google Scholar] [CrossRef] [PubMed]
- Brito, V.N.; Spinola-Castro, A.M.; Kochi, C.; Kopacek, C.; da Silva, P.C.A.; Guerra-Júnior, G. Central Precocious Puberty: Revisiting the Diagnosis and Therapeutic Management. Arch. Endocrinol. Metab. 2016, 60, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Reinehr, T.; Roth, C.L. Is There a Causal Relationship between Obesity and Puberty? Lancet Child Adolesc. Health 2019, 3, 44–54. [Google Scholar] [CrossRef]
- Stagi, S.; de Masi, S.; Bencini, E.; Losi, S.; Paci, S.; Parpagnoli, M.; Ricci, F.; Ciofi, D.; Azzari, C. Increased Incidence of Precocious and Accelerated Puberty in Females during and after the Italian Lockdown for the Coronavirus 2019 (COVID-19) Pandemic. Ital. J. Pediatrics 2020, 46, 165. [Google Scholar] [CrossRef]
- Durand, A.; Bashamboo, A.; McElreavey, K.; Brauner, R. Familial Early Puberty: Presentation and Inheritance Pattern in 139 Families. BMC Endocr. Disord. 2016, 16, 50. [Google Scholar] [CrossRef]
- Kim, Y.J.; Kwon, A.; Jung, M.K.; Kim, K.E.; Suh, J.; Chae, H.W.; Kim, D.H.; Ha, S.; Seo, G.H.; Kim, H.-S. Incidence and Prevalence of Central Precocious Puberty in Korea: An Epidemiologic Study Based on a National Database. J. Pediatrics 2019, 208, 221–228. [Google Scholar] [CrossRef]
- Bräuner, E.V.; Busch, A.S.; Eckert-Lind, C.; Koch, T.; Hickey, M.; Juul, A. Trends in the Incidence of Central Precocious Puberty and Normal Variant Puberty Among Children in Denmark, 1998 to 2017. JAMA Netw. Open 2020, 3, e2015665. [Google Scholar] [CrossRef]
- Eckert-Lind, C.; Busch, A.S.; Petersen, J.H.; Biro, F.M.; Butler, G.; Bräuner, E.V.; Juul, A. Worldwide Secular Trends in Age at Pubertal Onset Assessed by Breast Development Among Girls: A Systematic Review and Meta-Analysis. JAMA Pediatrics 2020, 174, e195881. [Google Scholar] [CrossRef]
- Abreu, A.P.; Macedo, D.B.; Brito, V.N.; Kaiser, U.B.; Latronico, A.C. A New Pathway in the Control of the Initiation of Puberty: The MKRN3 Gene. J. Mol. Endocrinol. 2015, 54, R131–R139. [Google Scholar] [CrossRef] [PubMed]
- Sultan, C.; Gaspari, L.; Maimoun, L.; Kalfa, N.; Paris, F. Disorders of Puberty. Best Pract. Res. Clin. Obstet. Gynaecol. 2018, 48, 62–89. [Google Scholar] [CrossRef] [PubMed]
- Kaplowitz, P.; Bloch, C.; Sills, I.N.; Bloch, C.A.; Casella, S.J.; Gonzalez, J.L.; Lynch, J.L.; Wintergerst, K.A. Evaluation and Referral of Children with Signs of Early Puberty. Pediatrics 2016, 137, e20153732. [Google Scholar] [CrossRef] [PubMed]
- Martins, W.P.; Nastri, C.O. Ultrasonographic Measurement of Ovarian Volume in the Diagnosis of Central Precocious Puberty. Ultrasound Obstet. Gynecol. 2009, 34, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Horby, P.W.; Hayden, F.G.; Gao, G.F. A Novel Coronavirus Outbreak of Global Health Concern. Lancet 2020, 395, 470–473. [Google Scholar] [CrossRef]
- Li, Q.; Guan, X.; Wu, P.; Wang, X.; Zhou, L.; Tong, Y.; Ren, R.; Leung, K.S.M.; Lau, E.H.Y.; Wong, J.Y.; et al. Early Transmission Dynamics in Wuhan, China, of Novel Coronavirus–Infected Pneumonia. N. Engl. J. Med. 2020, 382, 1199–1207. [Google Scholar] [CrossRef] [PubMed]
- Verzani, M.; Bizzarri, C.; Chioma, L.; Bottaro, G.; Pedicelli, S.; Cappa, M. Impact of COVID-19 Pandemic Lockdown on Early Onset of Puberty: Experience of an Italian Tertiary Center. Ital. J. Pediatrics 2021, 47, 52. [Google Scholar] [CrossRef]
- Bradley, S.H.; Lawrence, N.; Steele, C.; Mohamed, Z. Precocious Puberty. BMJ 2020, 368, l6597. [Google Scholar] [CrossRef]
- WHO Multicentre Growth Reference Study Group; De Onis, M. WHO Child Growth Standards Based on Length/Height, Weight and Age. Acta Paediatr. 2006, 95, 76–85. [Google Scholar] [CrossRef]
- Marshall, W.A.; Tanner, J.M. Variations in Pattern of Pubertal Changes in Girls. Arch. Dis. Child. 1969, 44, 291–303. [Google Scholar] [CrossRef]
- Reynolds, E. Radiographic Atlas of Skeletal Development of the Hand and Wrist; Greulich, W.W., Pyle, S.I., Eds.; Stanford University Press: Redwood City, CA, USA, 1950; Volume 8, pp. 518–520. [Google Scholar] [CrossRef]
- Dorn, L.D.; Susman, E.J.; Nottelmann, E.D.; Chrousos, G.P. Perceptions of Puberty: Adolescent and Parent Ratings of Pubertal Stage. Pediatric Res. 1987, 21, 173. [Google Scholar] [CrossRef][Green Version]
- Street, M.E.; Sartori, C.; Catellani, C.; Righi, B. Precocious Puberty and Covid-19 Into Perspective: Potential Increased Frequency, Possible Causes, and a Potential Emergency to Be Addressed. Front. Pediatrics 2021, 9, 978. [Google Scholar] [CrossRef] [PubMed]
- Karpati, A.M.; Rubin, C.H.; Kieszak, S.M.; Marcus, M.; Troiano, R.P. Stature and Pubertal Stage Assessment in American Boys: The 1988–1994 Third National Health and Nutrition Examination Survey. J. Adolesc. Health 2002, 30, 205–212. [Google Scholar] [CrossRef]
- Yackobovitch-Gavan, M.; Fisch Shvalb, N.; Bhutta, Z.A. Malnutrition and Catch-Up Growth during Childhood and Puperty. In World Review of Nutrition and Dietetics; Karger: Basel, Switzerland, 2019; Volume 120, ISBN 0084-2230. [Google Scholar] [CrossRef]
- Li, W.; Liu, Q.; Deng, X.; Chen, Y.; Liu, S.; Story, M. Association between Obesity and Puberty Timing: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2017, 14, 1266. [Google Scholar] [CrossRef] [PubMed]
- Sedlak, P.; Pařízková, J.; Samešová, D.; Musálek, M.; Dvořáková, H.; Novák, J. Secular Changes in Body Build and Body Composition in Czech Preschool Children in the Context of Latent Obesity. Children 2021, 8, 18. [Google Scholar] [CrossRef]
- Huber, B.C.; Steffen, J.; Schlichtiger, J.; Brunner, S. Altered Nutrition Behavior during COVID-19 Pandemic Lockdown in Young Adults. Eur. J. Nutr. 2021, 60, 2593–2602. [Google Scholar] [CrossRef]
- Teixeira, M.T.; Vitorino, R.S.; da Silva, J.H.; Raposo, L.M.; de Aquino, L.A.; Ribas, S.A. Eating Habits of Children and Adolescents during the COVID-19 Pandemic: The Impact of Social Isolation. J. Hum. Nutr. Diet. 2021, 34, 670–678. [Google Scholar] [CrossRef]
- Füzéki, E.; Schröder, J.; Carraro, N.; Merlo, L.; Reer, R.; Groneberg, D.; Banzer, W. Physical Activity during the First COVID-19-Related Lockdown in Italy. Int. J. Environ. Res. Public Health 2021, 18, 2511. [Google Scholar] [CrossRef]
- Chioma, L.; Bizzarri, C.; Verzani, M.; Fava, D.; Salerno, M.; Capalbo, D.; Guzzetti, C.; Penta, L.; di Luigi, L.; di Iorgi, N.; et al. Sedentary Lifestyle and Precocious Puberty in Girls during the COVID-19 Pandemic: An Italian Experience. Endocr. Connect. 2022, 11, e210650. [Google Scholar] [CrossRef]
- Wagner, I.V.; Sabin, M.A.; Pfäffle, R.W.; Hiemisch, A.; Sergeyev, E.; Körner, A.; Kiess, W. Effects of Obesity on Human Sexual Development. Nat. Rev. Endocrinol. 2012, 8, 246–254. [Google Scholar] [CrossRef]
- Kang, M.J.; Oh, Y.J.; Shim, Y.S.; Baek, J.W.; Yang, S.; Hwang, I.T. The Usefulness of Circulating Levels of Leptin, Kisspeptin, and Neurokinin B in Obese Girls with Precocious Puberty. Gynecol. Endocrinol. 2018, 34, 627–630. [Google Scholar] [CrossRef] [PubMed]
- El-Eshmawy, M.M.; Abdel Aal, I.A.; el Hawary, A.K. Association of Ghrelin and Leptin with Reproductive Hormones in Constitutional Delay of Growth and Puberty. Reprod. Biol. Endocrinol. 2010, 8, 153. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Chen, J.; Tang, Y.; Zhang, Q.; Wang, Y.; Li, Q.; Li, X.; Weng, Z.; Huang, J.; Wang, X.; et al. Difference of Precocious Puberty between before and during the COVID-19 Pandemic: A Cross-Sectional Study among Shanghai School-Aged Girls. Front. Endocrinol. 2022, 13, 839895. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Zhang, Y.; Sun, W.; Chen, Y.; Jiang, Y.; Song, Y.; Lin, Q.; Zhu, L.; Zhu, Q.; Wang, X.; et al. Investigating the Relationship between Precocious Puberty and Obesity: A Cross-Sectional Study in Shanghai, China. BMJ Open 2017, 7, e014004. [Google Scholar] [CrossRef] [PubMed]
- Jasik, C.B.; Lustig, R.H. Adolescent Obesity and Puberty: The “Perfect Storm”. Ann. N. Y. Acad. Sci. 2008, 1135, 265–279. [Google Scholar] [CrossRef] [PubMed]
- Nagu, P.; Parashar, A.; Behl, T.; Mehta, V. CNS Implications of COVID-19: A Comprehensive Review. Rev. Neurosci. 2021, 32, 219–234. [Google Scholar] [CrossRef] [PubMed]
- Naulé, L.; Maione, L.; Kaiser, U.B. Puberty, A Sensitive Window of Hypothalamic Development and Plasticity. Endocrinology 2021, 162, bqaa209. [Google Scholar] [CrossRef]
- Fudvoye, J.; Lopez-Rodriguez, D.; Franssen, D.; Parent, A.-S. Endocrine Disrupters and Possible Contribution to Pubertal Changes. Best Pract. Res. Clin. Endocrinol. Metab. 2019, 33, 101300. [Google Scholar] [CrossRef]
- Diamanti-Kandarakis, E.; Bourguignon, J.-P.; Giudice, L.C.; Hauser, R.; Prins, G.S.; Soto, A.M.; Zoeller, R.T.; Gore, A.C. Endocrine-Disrupting Chemicals: An Endocrine Society Scientific Statement. Endocr. Rev. 2009, 30, 293–342. [Google Scholar] [CrossRef]
- Kuiper, G.G.J.M.; Lemmen, J.G.; Carlsson, B.; Corton, J.C.; Safe, S.H.; van der Saag, P.T.; van der Burg, B.; Gustafsson, J.-A. Interaction of Estrogenic Chemicals and Phytoestrogens with Estrogen Receptor β. Endocrinology 1998, 139, 4252–4263. [Google Scholar] [CrossRef]
- Papadimitriou, A.; Papadimitriou, D.T. Endocrine-Disrupting Chemicals and Early Puberty in Girls. Children 2021, 8, 492. [Google Scholar] [CrossRef] [PubMed]
- Robinson, T.N.; Banda, J.A.; Hale, L.; Lu, A.S.; Fleming-Milici, F.; Calvert, S.L.; Wartella, E. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 2017, 140, S97–S101. [Google Scholar] [CrossRef] [PubMed]
- Stagi, S.; Ferrari, M.; Paiusco, G.; Moriondo, M.; Azzari, C. Possible Role of Melatonin in Precocious and Accelerated Puberty in Females during the COVID-19 Pandemic. Ital. J. Pediatrics 2021, preprint. [Google Scholar] [CrossRef]
| Variable | Pre-Pandemic n = 33 | During Pandemic n = 22 | p-Value |
|---|---|---|---|
| M2 age (in years) | |||
| Mean ± SD | 6.74 ± 0.85 | 7.15 ± 0.71 | 0.10 T |
| Age at diagnosis (in years) | |||
| Mean ± SD | 7.86 ± 0.82 | 7.70 ± 0.62 | 0.22 T |
| Time from M2 to diagnosis (in months) | |||
| Mean ± SD | 12.15 ± 9.96 | 6.63 ± 5.21 | 0.02 M |
| Z-score to height | |||
| Mean ± SD | 0.22 ± 0.98 | 0.76 ± 1.19 | 0.07 M |
| GV (in cm/year) | |||
| Mean ± SD | 8.59 ± 2.30 | 9.35 ± 2.93 | 0.14 T |
| Z-score to weight | |||
| Mean ± SD | 0.69 ± 0.83 | 1.08 ± 1.29 | 0.04 M |
| Z-score to BMI | |||
| Mean ± SD | 0.75 ± 0.86 | 0.96 ± 1.34 | 0.07 M |
| Normal | 21 (63.64%) | 9 (40.91%) | 0.20 Q |
| Overweight | 6 (18.18%) | 5 (22.73%) | |
| Obesity | 6 (18.18%) | 8 (36.36%) | |
| Tanner Stage | 0.16 E | ||
| 2 | 12 (36.36%) | 7 (31.82%) | |
| 3 | 18 (54.56%) | 15 (68.18%) | |
| 4 | 3 (9.09%) | 0 |
| Variable | Pre Pandemic n = 33 | During Pandemic n = 22 | p-Value |
|---|---|---|---|
| BA (in years) | |||
| Mean ± SD | 9.82 ± 1.19 | 9.55 ± 1.34 | 0.19 M |
| BA–CA (in years) | |||
| Mean ± SD | 1.96 ± 0.87 | 1.87 ± 1.00 | 0.36 T |
| LH (IU/L) | |||
| Mean ± SD | 1.35 ± 1.72 | 1.28 ± 2.17 | 0.45 M |
| FSH (IU/L) | |||
| Mean ± SD | 4.11 ± 2.64 | 4.33 ± 3.05 | 0.36 M |
| Estradiol (pmol/L) | |||
| Mean ± SD | 27.44 ± 18.80 | 25.61 ± 15.97 | 0.40 M |
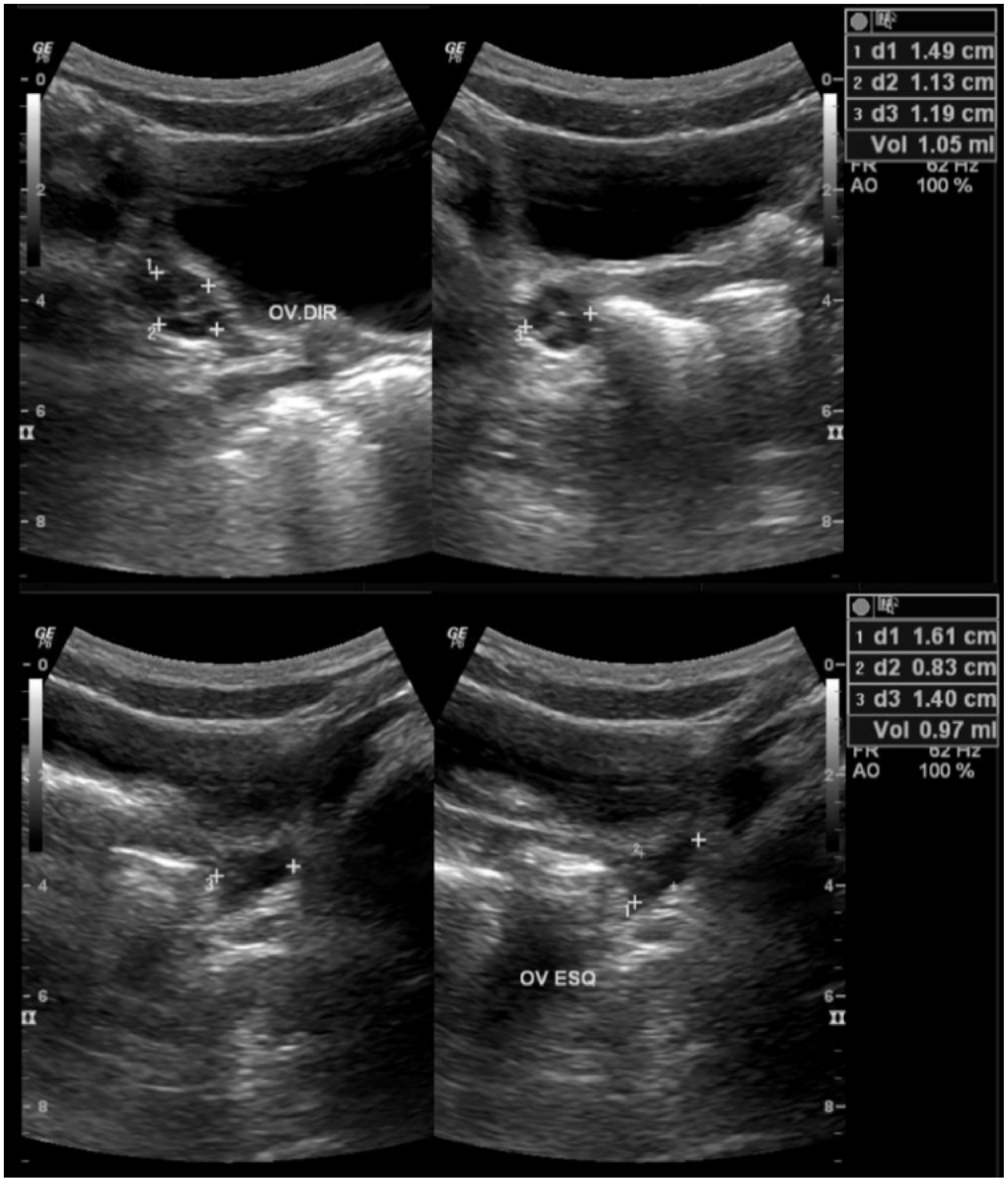
| Ovarian Volume (mL) | |||
| Mean ± SD | 3.15 ± 2.31 | 1.88 ± 0.95 | 0.01 M |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oliveira Neto, C.P.d.; Azulay, R.S.d.S.; Almeida, A.G.F.P.d.; Tavares, M.d.G.R.; Vaz, L.H.G.; Leal, I.R.L.; Gama, M.E.A.; Ribeiro, M.R.C.; Nascimento, G.C.; Magalhães, M.; et al. Differences in Puberty of Girls before and during the COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2022, 19, 4733. https://doi.org/10.3390/ijerph19084733
Oliveira Neto CPd, Azulay RSdS, Almeida AGFPd, Tavares MdGR, Vaz LHG, Leal IRL, Gama MEA, Ribeiro MRC, Nascimento GC, Magalhães M, et al. Differences in Puberty of Girls before and during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health. 2022; 19(8):4733. https://doi.org/10.3390/ijerph19084733
Chicago/Turabian StyleOliveira Neto, Clariano Pires de, Rossana Santiago de Sousa Azulay, Ana Gregória Ferreira Pereira de Almeida, Maria da Glória Rodrigues Tavares, Luciana Helena Gama Vaz, Ianik Rafaela Lima Leal, Monica Elinor Alves Gama, Marizélia Rodrigues Costa Ribeiro, Gilvan Cortês Nascimento, Marcelo Magalhães, and et al. 2022. "Differences in Puberty of Girls before and during the COVID-19 Pandemic" International Journal of Environmental Research and Public Health 19, no. 8: 4733. https://doi.org/10.3390/ijerph19084733
APA StyleOliveira Neto, C. P. d., Azulay, R. S. d. S., Almeida, A. G. F. P. d., Tavares, M. d. G. R., Vaz, L. H. G., Leal, I. R. L., Gama, M. E. A., Ribeiro, M. R. C., Nascimento, G. C., Magalhães, M., Santos, W. C. d., Facundo, A. N., Faria, M. d. S., & Lago, D. C. F. (2022). Differences in Puberty of Girls before and during the COVID-19 Pandemic. International Journal of Environmental Research and Public Health, 19(8), 4733. https://doi.org/10.3390/ijerph19084733







