Anemia in Pregnant Women and Children Aged 6 to 59 Months Living in Mozambique and Portugal: An Overview of Systematic Reviews
Abstract
1. Introduction
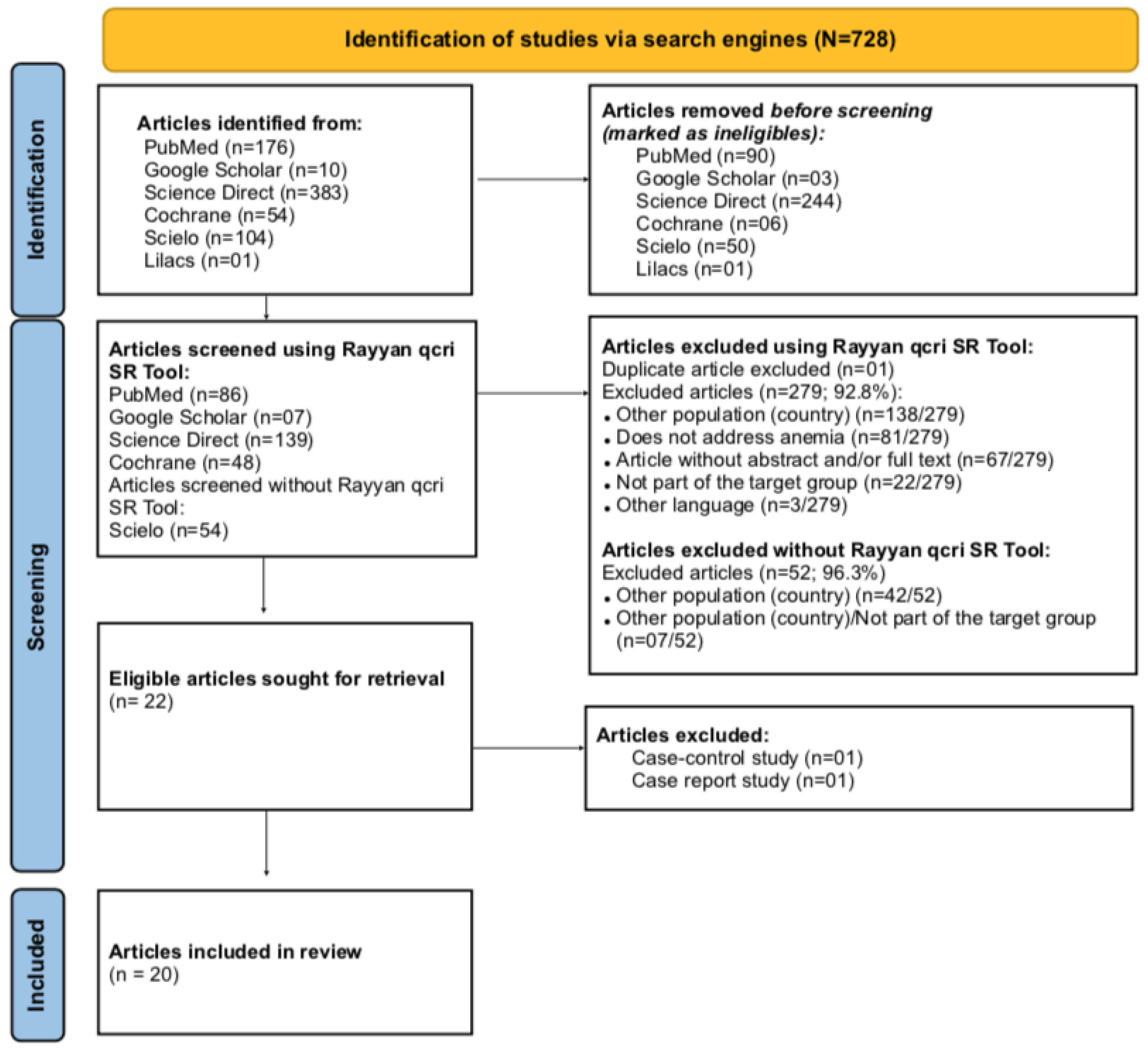
2. Materials and Methods
2.1. Search Strategy and Selection Criteria
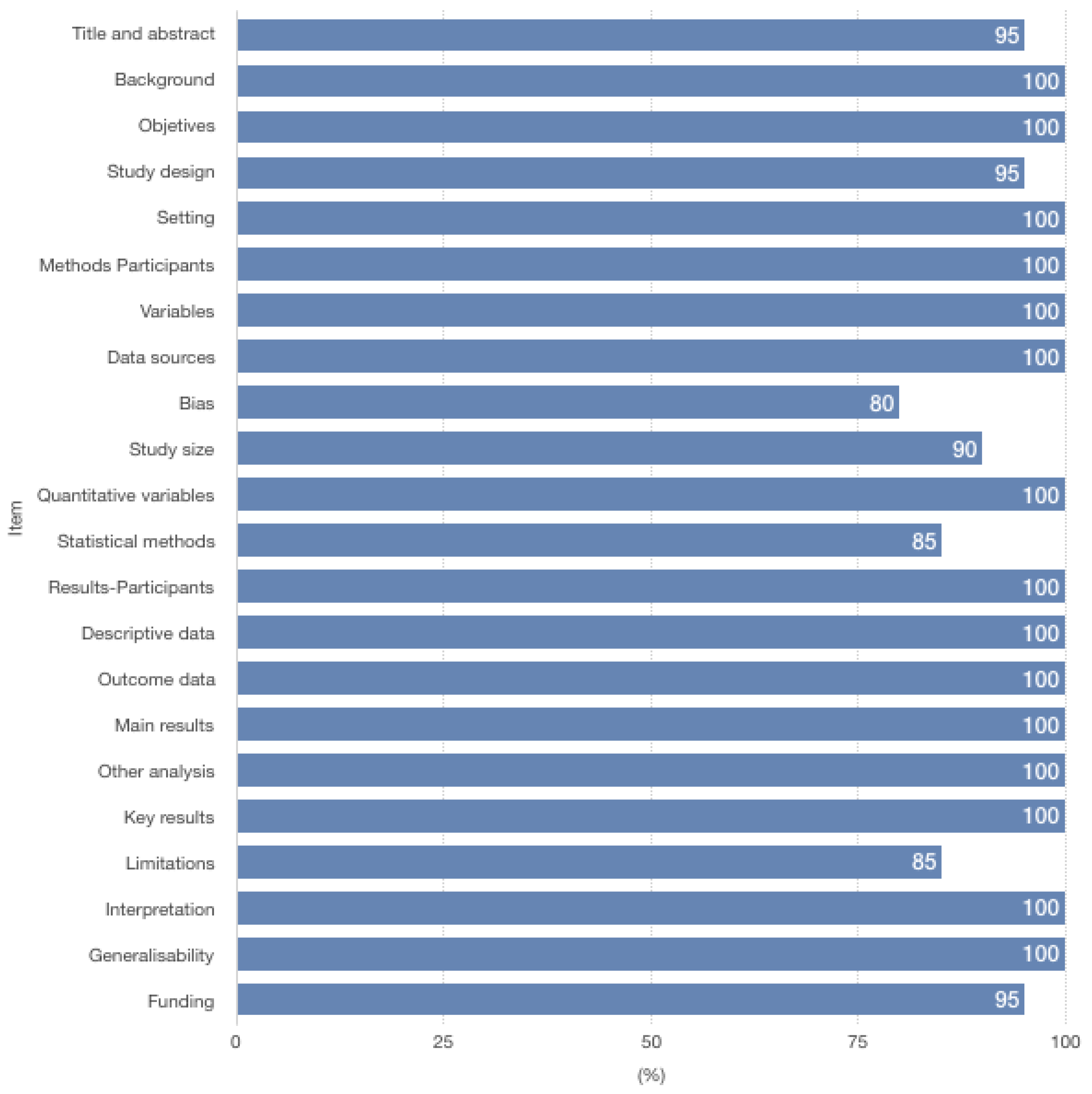
2.2. Quality Assessment and Data Extraction
3. Results
3.1. Anemia and Iron Deficiency Anemia (IDA) Prevalence
3.2. Years Lived with Disability (YLDs) and Disability-Adjusted Life-Years (DALYs)
3.3. Malaria and HIV/AIDS
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CPLP | Community of Portuguese Language Countries |
| AMSTAR | A Measurement Tool to Assess systematic Reviews |
| DALYs | Attributable Disadjusted Life Years |
| EMPIRE | Epidemiological study to determine the prevalence of anemia and iron deficit in the Portuguese population |
| HELENA | Healthy Lifestyle in Europe by Nutrition in Adolescence |
| IDA | Iron deficiency anemia |
| PRISMA | Preferred Reporting Items for Systematic review and Meta-Analysis |
| PROSPERO | The International Prospective Register of Systematic Reviews |
| SDI | Social Demographic Index |
| SDGSs | Sustainable Development Goals |
| SP | Sulfadoxine-pyrimethamine |
| STROBE | Strengthening the Reporting of Observational Studies in Epidemiology |
| UHC | Universal Health Coverage |
| YLDs | Years Lived with a Disability |
References
- Global Nutrition Report (GNR). Glossary 2020 Global Nutrition Report—Global Nutrition Report. 2020. Available online: https://globalnutritionreport.org/reports/2020-global-nutrition-report/glossary/ (accessed on 8 May 2021).
- World Health Organization (WHO). Micronutrient Indicators: Haemoglobin Concentrations for the Diagnosis of Anaemia and Assessment of Severity. 2015. Available online: https://www.who.int/vmnis/indicators/haemoglobin.pdf (accessed on 24 March 2022).
- Impieri De Souza, A.; Filho, M.B. Diagnóstico e tratamento das anemias carenciais na gestação: Consensos e controvérsias. Rev. Bras. Saúde Matern. Infant 2003, 3, 473–479. [Google Scholar] [CrossRef][Green Version]
- World Health Organization (WHO). What’s at Stake Target: 50% Reduction of Anaemia in Women of Reproductive Age Box 1: What Is Anemia? 2014. Available online: https://webcache.googleusercontent.com/search?q=cache:v-c-CP2GLN4J:https://apps.who.int/iris/rest/bitstreams/663653/retrieve+&cd=1&hl=es&ct=clnk&gl=pt (accessed on 6 May 2021).
- Elmardi, K.A.; Adam, I.; Malik, E.M.; Abdelrahim, T.A.; Elhag, M.S.; Ibrahim, A.A.; Babiker, M.A.; Elhassan, A.H.; Kafy, H.T.; Elshafie, A.T.; et al. Prevalence and determinants of anaemia in women of reproductive age in Sudan: Analysis of a cross-sectional household survey. BMC Public Health 2020, 20, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Merck Manual of Diagnosis (MSD). Perinatal Anemia—Pediatrics. MSD Manual Professional Edition. 2020. Available online: https://www.msdmanuals.com/en-pt/professional/pediatrics/perinatal-hematologic-disorders/perinatal-anemia (accessed on 26 April 2021).
- Nagata, J.M.; Gatti, L.R.; Barg, F. Social determinants of iron supplementation among women of reproductive age: A systematic review of qualitative data. Matern. Child Nutr. 2011, 8, 1–18. [Google Scholar] [CrossRef] [PubMed]
- Gardner, W.; Kassebaum, N. Global, Regional, and National Prevalence of Anemia and Its Causes in 204 Countries and Territories, 1990–2019. Curr. Dev. Nutr. 2020, 4, 830. [Google Scholar] [CrossRef]
- Instituto Nacional de Estatística (INE). Moçambique—Inquérito Demográfico e de Saúde. 2011. Available online: https://dhsprogram.com/pubs/pdf/fr266/fr266.pdf (accessed on 5 May 2021).
- Ministério da Agricultura e Segurança Alimentar (MASA). Impacto Social e Económico da Desnutrição Infantil No Desenvolvimento a Longo Prazo de Moçambique. Secretariado Técnico de Segurança Alimentar e Nutricional. 2017. Available online: https://www.setsan.gov.mz/wp-content/uploads/2018/07/Estudo-COHA.pdf (accessed on 5 May 2021).
- Anemia Working Group Portugal (AWGP). A Problemática da Anemia Na Sociedade Portuguesa. 2019. Available online: https://app.parlamento.pt/Webutils/docs/doc.pdf?path=6148523063446f764c324679626d56304c334e706447567a4c31684a53556c4d5a5763765130394e4c7a6c445579394562324e31625756756447397a51574e3061585a705a47466b5a554e7662576c7a633246764c7a67304e54426b5a6a426c4c546730595749744e4449774f4331694e6a4e6a4c54646c59324577593255314e444130596935775a47593d&fich=8450df0e-84ab-4208-b63c-7eca0ce5404b.pdf&Inline=true (accessed on 7 May 2021).
- World Health Organization. Global Health Observatory Data Repository: By Category, Anaemia in Pregnant Women—Estimates by Country. 2021. Available online: https://apps.who.int/gho/data/view.main.ANAEMIAWOMENPWREG (accessed on 6 May 2021).
- World Health Organization. Global Health Observatory Data Repository: By Category, Anaemia in Children—Estimates by Country. 2021. Available online: https://apps.who.int/gho/data/view.main.ANEMIACHILDRENREGv (accessed on 6 May 2021).
- World Health Organization (WHO). Evidence-Based Nutrition Interventions Included in the WHO e-Library of Evidence for Nutrition Actions (eLENA) that May Contribute to the Achievement of the WHO Global Nutrition and Diet-Related NCD Targets Global Nutrition Targets 2025 Global NCD Targets. 2018. Available online: https://www.who.int/elena/titles/summary_eLENA_interventions_linked_global_targets.pdf (accessed on 6 May 2021).
- World Health Organization (WHO). Interventions by Global Target. 2018. Available online: http://www.who.int/elena/global-targets/en/ (accessed on 7 May 2021).
- Fonseca, C.; Marques, F.; Nunes, A.R.; Belo, A.; Brilhante, D.; Cortez, J. Prevalence of anaemia and iron deficiency in Portugal: The EMPIRE study. Intern. Med. J. 2016, 46, 470–478. [Google Scholar] [CrossRef]
- Marques, F.; Fonseca, C.; Nunes, A.R.; Belo, A.; Brilhante, D.; Cortez, J. Contextualizando a Elevada Prevalência de Anemia na População Portuguesa: Perceção, Caracterização e Preditores: Um Sub-Estudo do EMPIRE. Medicina Interna. Rev. Da Soc. Port. De Med. Interna 2016, 4, 26–38. [Google Scholar]
- Ministério da Saúde (MISAU); Instituto Nacional de Saúde (INS). Inquérito Nutricional a Crianças de 0 a 24 Meses de Idade, Adolescentes e Mulheres em Idade Fértil Nas Províncias de Niassa, Cabo Delgado e Nampula 2015. 2017. Available online: https://ped-hcm-ucla.weebly.com/uploads/8/0/6/0/80607382/15-8-18_inquerito_nutricao.pdf (accessed on 20 May 2021).
- Ministério da Saúde (MISAU); Instituto Nacional de Estatística (INE); ICF Internacional. Inquérito de Indicadores de Imunização, Malária e HIV/SIDA em Moçambique 2015. 2016. Available online: https://mz.usembassy.gov/wp-content/uploads/sites/182/2017/06/IMASIDA-2016_Relatorio-de-Indicadores-Basicos-for-Web.pdf (accessed on 20 May 2021).
- World Health Organization (WHO). Nutritional Anaemias: Tools for Effective Prevention and Control. 2017. Available online: https://www.who.int/publications/i/item/9789241513067?sequence=1 (accessed on 7 May 2021).
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef]
- Library, M. Rayyan for Systematic Reviews: Collaboration. (n.d.). Available online: https://libraryguides.mcgill.ca/rayyan/collaboration#s-lg-box-13326656 (accessed on 26 April 2021).
- Cajal, B.; Jiménez, R.; Gervilla, E.; Montaño, J.J. Doing a Systematic Review in Health Sciences. Clínica Y Salud 2020, 31, 77–83. [Google Scholar] [CrossRef]
- Cevallos, M.; Egger, M. Chapter 17: STROBE (Strengthening the Reporting of Observational studies in Epidemiology). In Guidelines for Reporting Health Research: A User’s Manual, 1st ed.; John Wiley & Sons: Hoboken, NJ, USA, 2014; Volume 17, pp. 169–179. [Google Scholar]
- Bern, I.U. STROBE Strengthening the Reporting of Observational Studies in Epidemiology Statement: Available Checklists. 2009. Available online: https://www.strobe-statement.org/index.php?id=available-checklists (accessed on 26 April 2021).
- Shea, B.J. AMSTAR: Assessing the Methodological Quality of Systematic Reviews. The Development of AMSTAR. 2021. Available online: https://amstar.ca/index.php (accessed on 7 May 2021).
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef]
- González, R.; Pons-Duran, C.; Piqueras, M.; Aponte, J.J.; Ter Kuile, F.; Menéndez, C. Mefloquine for preventing malaria in pregnant women. Cochrane Database Syst. Rev. 2018, 3, CD011444. [Google Scholar] [CrossRef]
- Radeva-Petrova, D.; Kayentao, K.; Ter Kuile, F.O.; Sinclair, D.; Garner, P. Drugs for preventing malaria in pregnant women in endemic areas: Any drug regimen versus placebo or no treatment. Cochrane Database Syst. Rev. 2014, 10, 1–120. [Google Scholar] [CrossRef] [PubMed]
- Balarajan, Y.; Ramakrishnan, U.; Ozaltin, E.; Shankar, A.H.; Subramanian, S.V. Anaemia in low-income and middle-income countries. Lancet 2011, 378, 2123–2135. [Google Scholar] [CrossRef]
- Arsenault, C.; Jordan, K.; Lee, D.; Dinsa, G.; Manzi, F.; Marchant, T.; Kruk, M.E. Equity in antenatal care quality: An analysis of 91 national household surveys. Lancet Glob. Health 2018, 6, e1186–e1195. [Google Scholar] [CrossRef]
- Bhutta, Z.A.; Das, J.K.; Rizvi, A.; Gaffey, M.F.; Walfer, N.; Horton, S.; Webb, P.; Lartey, A.; Black, R.E. Evidence-based interventions for improvement of maternal and child nutrition: What can be done and at what cost? Lancet 2013, 9890, 452–477. [Google Scholar] [CrossRef]
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef]
- Duncan, B. Global Child Health: Promises Made to Children—Not Yet Kept. Adv. Pediatr. 2009, 56, 301–339. [Google Scholar] [CrossRef]
- Gaffey, M.F.; Das, J.K.; Bhutta, Z.A. Millennium Development Goals 4 and 5: Past and future progress. Semin. Fetal Neonatal Med. 2015, 20, 285–292. [Google Scholar] [CrossRef]
- Ruel, M.T.; Quisumbing, A.R.; Balagamwala, M. Nutrition-sensitive agriculture: What have we learned so far? Glob. Food Sec. 2018, 17, 128–153. [Google Scholar] [CrossRef]
- Langer, A.; Meleis, A.; Knaul, F.M.; Atun, R.; Aran, M.; Arreola-Ornelas, H.; Bhutta, Z.A.; Binagwaho, A.; Bonita, R.; Caglia, J.M.; et al. Women and Health: The key for sustainable development. Lancet 2015, 386, 1165–1210. [Google Scholar] [CrossRef]
- Diaz, V.; Abalos, E.; Carroli, G. Methods for blood loss estimation after vaginal birth. Cochrane Database Syst. Rev. 2018, 2018, CD010980. [Google Scholar] [CrossRef]
- De-Regil, L.M.; Peña-Rosas, J.P.; Fernández-Gaxiola, A.C.; Rayco-Solon, P. Effects and safety of periconceptional oral folate supplementation for preventing birth defects. Cochrane Database Syst. Rev. 2015, 2015, CD007950. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Barber, R.M.; Bell, B.; Bertozzi-Villa, A.; Biryukov, S.; Bolliger, I.; Charlson, F.; Davis, A.; Degenhardt, L.; Dicker, D.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 743–800. [Google Scholar] [CrossRef]
- Forouzanfar, M.H.; Alexander, L.; Bachman, V.F.; Biryukov, S.; Brauer, M.; Casey, D.; Coates, M.M.; Delwiche, K.; Estep, K.; Frostad, J.J.; et al. Global, regional, and national comparative risk assessment of 79 behavioural, environmental and occupational, and metabolic risks or clusters of risks in 188 countries, 1990–2013: A systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015, 386, 2287–2323. [Google Scholar] [CrossRef]
- Vos, T.; Allen, C.; Arora, M.; Barber, R.M.; Bhutta, Z.A.; Brown, A.; Carter, A.; Casey, D.C.; Charlson, F.J.; Chen, A.Z.; et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1545–1602. [Google Scholar] [CrossRef]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- GBD 2015 Mortality and Causes of Death Collaborators. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: A systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016, 388, 1459–1544. [Google Scholar] [CrossRef]
- Naghavi, M.; Abajobir, A.A.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Aboyans, V.; Adetokunboh, O.; Afshin, A.; Agrawal, A.; et al. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1151–1210. [Google Scholar] [CrossRef]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Global Burden Diseases (GBD 2016) Risk Factors Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 10100, 1345–1422. [Google Scholar] [CrossRef]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Global Burden Diseases (BD 2017) Risk Factor Collaborators. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 10159, 1923–1994. [Google Scholar]
- Da Costa, A.G.; Vargas, S.; Clode, N.; Graça, L.M. Prevalence and Risk Factors for Iron Deficiency Anemia and Iron Depletion during Pregnancy: A Prospective Study. Acta Médica Port. 2016, 29, 514. [Google Scholar] [CrossRef]
- Mavale, S.; Alburqueque, O.; Mondlane, R.; Guerra, A. Prevalência de anemia numa população infantil da Cidade de Maputo. Acta Pediatr. Port 2000, 31, 33–39. [Google Scholar]
- De Andrade, C.C.; Rodrigues, S.L.; Carneiro, B.N.; Ferreira, M.D. Iron deficiency anemia in adolescents; a literature review. Nutr. Hosp. 2014, 6, 1240–1249. [Google Scholar] [CrossRef]
- Ferrari, M.; on behalf of the HELENA Study Group; Mistura, L.; Patterson, E.; Sjostrom, M.; Díaz, L.E.; Stehle, P.; Gonzalez-Gross, M.; Kersting, M.; Widhalm, K.; et al. Evaluation of iron status in European adolescents through biochemical iron indicators: The HELENA Study. Eur. J. Clin. Nutr. 2011, 65, 340–349. [Google Scholar] [CrossRef] [PubMed]
- Moreno, L.A. Adolescence. In Pediatric Nutrition in Practice; Koletzko, B., Ed.; Karger Publishers: Basel, Switzerland, 2008; pp. 114–117. [Google Scholar] [CrossRef]
- Wharton, B.; Wharton, P. Nutrition in Adolescence. Nutr. Health 1987, 4, 195–203. [Google Scholar] [CrossRef]
- Anemia Working Group Portugal (AWGP). Anemia: Conheça o Problema Que Afeta Os Adolescentes. 2019. Available online: https://awgp.pt/anemia-conheca-o-problema-que-afeta-os-adolescentes/ (accessed on 7 May 2021).
- Moreira, I.M. Anemia em Adolescentes, Prevalência e Factores Associados: O Papel do Helicobacter Pylori. (Tese de Mestrado). Universidade do Porto, Faculdade de Medicina, Instituto de Ciências Biomédicas Abel Salazar. 2010. Available online: https://repositorio-aberto.up.pt/bitstream/10216/55395/2/Dissertao%20Tese.pdf (accessed on 12 May 2021).
- Grupo de Eritropatología de la Sociedad Española de Hematología y Hemoterapia (SEHH). El 20% de las Mujeres en Edad Fértil, el 40% de las Gestantes y el 15% de los Adolescentes Tienen Anemia Ferropénica en España. 2018. Available online: https://www.sehh.es/sala-prensa/notas-prensa/122752-el-20-de-las-mujeres-en-edad-fertil-el-40-de-las-gestantes-y-el-15-de-los-adolescentes-tienen-anemia-ferropenica-en-espanahighlight=WyJhbmVtaWEiLCInYW5lbWlhIl0= (accessed on 28 October 2021).
- Hall, A.; Bobrow, E.; Brooker, S.; Jukes, M.; Nokes, K.; Lambo, J.; Guyatt, H.; Bundy, D.; Adjei, S.; Wen, S.T.; et al. Anaemia in schoolchildren in eight countries in Africa and Asia. Public Health Nutr. 2001, 4, 749–756. [Google Scholar] [CrossRef]
- Habib, N.; Abbasi, S.-U.S.; Aziz, W. An Analysis of Societal Determinant of Anemia among Adolescent Girls in Azad Jammu and Kashmir, Pakistan. Anemia 2020, 2020, 1–9. [Google Scholar] [CrossRef]
- Caetano, J.S.; Azevedo, J.; Saturnino, H.; Manco, L.; Benedito, M.; Bento, C.; Ribeiro, M.L. Défice de glicose-6-fosfato desidrogenase: Breve revisão teórica a propósito de um caso clínico. Saude-Infant 2015, 2, 58–63. [Google Scholar]
- Neves, A.L.; Guimarães, A.I.; Rolão, C. Suplementação preventiva com ferro oral em grávidas não anémicas. Acta Obs. Ginecol. Port 2012, 1, 16–19. [Google Scholar]
- Macedo, A.; Cardoso, S. Suplementação de rotina com ferro na gravidez. Acta Med. Port 2010, 5, 785–792. [Google Scholar]
- Nascimento, P.; Oliveira, M.; Simão, T.S.; Dias, A.; Ferreira, C. Hábitos alimentares em idade pré-escolar. Saude-Infant 2010, 2, 83–88. [Google Scholar]
- Valente, I.; Lima, R.; Antunes, M.; Barbot, J.; Pereira, F. Gastrite atrófica auto-imune—Anemia refractária ao ferro oral. ENDO-News 2010, 30, 14–16. [Google Scholar]
- Vilan, A.; Cunha, J.; Brandão, C.; Cleto, E. Anemia de Diamond-Blackfan. Acta Pediatr. Port 2008, 2, 72–74. [Google Scholar] [CrossRef]
- The Global Goals (TGG). The Global Goals for Sustainable Development. Global Goals. Available online: https://www.globalgoals.org/ (accessed on 28 October 2021).
- Universal Health Coverage (UHC2030). UHC2030: Our Mission. Available online: https://www.uhc2030.org/our-mission/ (accessed on 28 October 2021).
- Worldbank (WB). Data for Portugal, Mozambique. Available online: https://data.worldbank.org/?locations=PT-MZ (accessed on 28 October 2021).
- Malta, D.C.; Cardoso, L.M.; Teixeira, R.A.; de Carvalho, Q.H.; Ribeiro, A.P.; de Freitas, P.C.; Hartz, Z. Avaliação das metas dos Objetivos de Desenvolvimento Sustentável relacionadas à saúde nos países de língua portuguesa. Evaluation of the health-related targets of the Sustainable Development Goals in Portuguese-speaking countries. An. Do IHMT 2019, 18, 30–41. [Google Scholar] [CrossRef]
- Costa, C.; Santana, P.; Dimitroulopoulou, S.; Burström, B.; Borrell, C.; Schweikart, J.; Dzúrová, D.; Zangarini, N.; Katsouyanni, K.; Deboosere, P.; et al. Population Health Inequalities Across and Within European Metropolitan Areas through the Lens of the EURO-HEALTHY Population Health Index. Int. J. Environ. Res. Public Health 2019, 16, 836. [Google Scholar] [CrossRef] [PubMed]
- Keats, E.C.; Das, J.K.; Salam, R.A.; Lassi, Z.S.; Imdad, A.; Black, R.E.; Bhutta, Z.A. Effective interventions to address maternal and child malnutrition: An update of the evidence. Lancet Child Adolesc. Health 2021, 5, 367–384. [Google Scholar] [CrossRef]
- Aggett, P.J. Chapter 22—Iron. In Present Knowledge in Nutrition, 11th ed.; Academic Press: Cambridge, MA, USA, 2020; Volume 1, pp. 375–392. [Google Scholar] [CrossRef]
- Heidkamp, R.A.; Piwoz, E.; Gillespie, S.; Keats, E.C.; D’Alimonte, M.R.; Menon, P.; Das, J.K.; Flory, A.; Clift, J.W.; Ruel, M.T.; et al. Mobilising evidence, data, and resources to achieve global maternal and child undernutrition targets and the Sustainable Development Goals: An agenda for action. Lancet 2021, 397, 1400–1418. [Google Scholar] [CrossRef]
- Hollis, J.L.; Collins, C.E.; DeClerck, F.; Chai, L.K.; McColl, K.; Demaio, A.R. Defining healthy and sustainable diets for infants, children and adolescents. Glob. Food Secur. 2020, 27, 100401. [Google Scholar] [CrossRef]
- González-Rábago, Y.; La Parra, D.; Puigpinós-Riera, R.; Pons-Vigués, M. ¿Cómo medir el estatus migratorio de la población infantil y juvenil? Estudios sobre salud y desigualdades en salud en Europa. Gac. Sanit. 2019, 35, 81–90. [Google Scholar] [CrossRef]

| Electronic Databases | Terms and Operators |
|---|---|
| PubMed | MATERNAL ANEMIA OR MATERNAL ANAEMIA OR ANEMIA MATERNA AND CHILDREN FROM SIX TO 59 MONTHS OF AGE OR CRIANCAS DOS SEIS AOS 59 MESES DE IDADE OR NIÑOS DE SEIS A 59 MESES DE EDAD AND IRON DEFICIENCY OR DEFICIENCIA DE FERRO OR DEFICIENCIA DE HIERRO AND NUTRITIONAL INDICATORS OR INDICADORES NUTRICIONAIS OR INDICADORES NUTRICIONALES AND SOCIAL DETERMINANTS OR DETERMINANTES SOCIAIS OR DETERMINANTES SOCIALES |
| GoogleScholar | MATERNAL ANEMIA OR MATERNAL ANAEMIA OR ANEMIA MATERNA AND CHILDREN FROM SIX TO 59 MONTHS OF AGE OR CRIANCAS DOS SEIS AOS 59 MESES DE IDADE OR NIÑOS DE SEIS A 59 MESES DE EDAD AND IRON DEFICIENCY OR DEFICIENCY DE FERRO OR DEFICIENCIA DE HIERRO AND NUTRITIONAL INDICATORS OR INDICADORES NUTRICIONAIS OR INDICADORES NUTRICIONALES AND SOCIAL DETERMINANTS OR DETERMINANTES SOCIAIS OR DETERMINANTES SOCIALES |
| Science Direct | MATERNAL ANEMIA (OR) MATERNAL ANAEMIA (AND) CHILDREN FROM SIX TO 59 MONTHS OF AGE (AND) IRON DEFICIENCY ((AND) NUTRITIONAL INDICATORS (AND) SOCIAL DETERMINANTS |
| Cochrane | MATERNAL ANEMIA OR MATERNAL ANAEMIA OR ANEMIA MATERNA AND CHILDREN FROM SIX TO 59 MONTHS OF AGE OR CRIANCAS DOS SEIS AOS 59 MESES DE IDADE OR NIÑOS DE SEIS A 59 MESES DE EDAD AND IRON DEFICIENCY OR DEFICIENCIA DE FERRO OR DEFICIENCIA DE HIERRO AND NUTRITIONAL INDICATORS OR INDICADORES NUTRICIONAIS OR INDICADORES NUTRICIONALES AND SOCIAL DETERMINANTS OR DETERMINANTES SOCIAIS OR DETERMINANTES SOCIALES |
| Scielo | MATERNAL ANEMIA (AND) CHILDREN FROM SIX TO 59 MONTHS OF AGE (AND) IRON DEFICIENCY |
| Lilacs | (MATERNAL ANEMIA) OR (MATERNAL ANAEMIA) OR (ANEMIA MATERNA) AND (CHILDREN FROM SIX TO 59 MONTHS OF AGE) OR (NIÑOS DE SEIS A 59 MESES DE EDAD) AND (DEFICIENCIA DE HIERRO) OR (IRON DEFICIENCY) AND (NUTRITIONAL INDICATORS) OR (INDICADORES NUTRICIONALES) |
| Inclusion Criteria | Exclusion Criteria |
|---|---|
|
|
| Reference No. | Author | Year of Publication | Mentions on Mozambique/Portugal | Target Group | Mozambique/Portugal Specific Findings | Period of Analysis/Analysis Performed | General Findings Related to Anemia |
|---|---|---|---|---|---|---|---|
| [28] | González et al. | 2018 | Mozambique | Pregnant women (trials, antenatal care clinic settings) | Mefloquine probably results in fewer women anemic at delivery (when compared with sulfadoxine-pyrimethamine);Mefloquine plus cotrimoxazole probably results in little or no difference in maternal anemia cases at delivery | 2010–2013; Systematic review: Dichotomous outcomes were compared using risk ratios (RRs), count outcomes as incidence rate ratios (IRRs), and continuous outcomes using mean differences (MDs). | When compared with sulfadoxine-pyrimethamine, mefloquine decreased maternal anemia at delivery (RR 0.84, 95% CI 0.76 to 0.94; 5469 participants, 2 studies; moderate-certainty evidence). When compared with cotrimoxazole, there was no probably effect on maternal anemia at delivery (RR 0.94, 95% CI 0.73 to 1.20; 1197 participants, 2 studies; moderate-certainty evidence). |
| [29] | Radeva-Petrova et al. | 2014 | Mozambique | Pregnant women (Trials, conducted between 1957 and 2008) | Of the two most recent trials, both large, and both administering two doses of sulfadoxine-pyrimethamine (SP), one trial from Mozambique demonstrated a benefit with chemoprevention(ofr maternal outcomes); One trial in Mozambique found a large effect in reducing the risk of cord blood anemia (RR 0.49, 95% CI 0.30 to 0.80; one trial, 870 participants). | Systematic review: Dichotomous outcomes were compared using risk ratios (RR), and continuous outcomes using mean differences (MDs). | “For women in their first or second pregnancy, malaria chemoprevention reduces the risk of moderate to severe anemia by around 40% (RR 0.60, 95% CI 0.47 to 0.75; three trials, 2503 participants, high quality evidence), and the risk of any anemia by around 17% (RR 0.83, 95% CI 0.74 to 0.93; five trials,, 3662 participants, high quality evidence).” |
| [30] | Balarajan et al. | 2011 | Mozambique | Children of preschool age (0–5 years) and Pregnant women | Anemia prevalence in mozambican children of preschool age (0–5 years) was severe (≥40.0%) | 1993–2005; Revision, including discussion of the multifactorial causes of anemia and the co-occurrence of multiple risk factors in different populations and identify potential barriers to effective anemia prevention and control. | “Africa and Asia were the most heavily affected regions, with Africa having the highest prevalence of anemia, and Asia bearing the greater absolute burden.” |
| [31] | Arsenault et al. | 2018 | Mozambique | Pregnant women, Women of reproductive age (15–49 years) who had at least one live birth in the past 2 years (MICS) or 5 years (DHS) | No specific country findings for anemia were presented; In Mozambique, more than 90% of women accessed skilled antenatal care but less than 60% reported the three services (quality antenatal care). Mozambique had high levels of coverage but low and inequitable levels of quality | The availability of potential indicators of ante-natal care quality in household surveys was assessed. | “Quality antenatal care involves the provision of respectful, evidence-based care including appropriate patient assessments such appropriate preventive and curative treatments (eg, iron supplementation); and patient counseling and education.” |
| [32] | Bhutta et al. | 2013 | Mozambique | Pregnant women and Children | No specific country findings for anemia were presented | Comprehensive review: the potential effect of delivery of nutrition specific interventions on lives saved in the 34 countries with 90% of the global burden of stunted children was modeled | Folic acid supplementation during pregnancy improved means birth weight, with a 79% reduction in the incidence of megaloblastic anemia; and iron supplementation to women during pregnancy contributed to 70% reduction in anemia at term, a 67% reduction in iron deficiency anemia (IDA), and 19% reduction in the incidence of low birthweight. |
| [33] | Black et al. | 2013 | Mozambique | Children < 5 years and Pregnant women | No specific country findings for anemia were presented. Prevalence of stunting (HAZ < –2 Z scores below median) and overweight (BAZ > 2 Z scores above median) for highest and lowest wealth quintiles for Mozambique (MICS 2006) were presented | 2013; Proportion of pregnant women with anemia whose blood hemoglobin would increase to at least 110 g/L was calculated. The proportion of severe anemia that would increase to at least 70 g/L was also calculated. | Iron deficiency contribute substantially to maternal deaths and maternal iron deficiency is associated with babies with low weight (<2500 g) at birth; anaemia (haemoglobin <110 g/L), which might be attributable to low consumption or absorption in the diet or to blood loss, such as from intestinal worms, is highly prevalent during pregnancy. In Africa, the prevalence of iron deficiency anaemia (haemoglobin <110 g/L) was of 20.2% (18.6–21.7) and 20.3% (18.3–22.4) in children < 5 years and pregnant women, respectively. In Europe, the prevalence of iron deficiency anaemia (haemoglobin < 110 g/L) was of 12.1% (7.8–16.2) and 16.2% (12.6–19.7) in children < 5 years and pregnant women, respectively. |
| [34] | Duncan, Burris | 2009 | Mozambique | Pregnant women and infants | No specific country findings for anemia were presented. | Overview of the state of the world’s children from the late 1970s until the year 2008. | “Complications from a teen pregnancy are numerous and include high prevalence of anemia. Universal supplementation of calcium, iron, and folic acid during pregnancy can prevent almost one-fourth of all maternal deaths.” |
| [35] | Gaffey et al. | 2015 | Mozambique | Children aged < 12 years | No specific country findings for anemia were presented | 1990–2015; Revision of global and regional progress towards Millennium Development Goals (MDGs) 4 and 5 with respect to their indicators | Intermittent iron supplementation in children aged < 12 years is associated with a 49% lower risk of anemia and a 76% lower risk of iron deficiency. The evidence on the use of micronutrient powders (MNPs) for home fortification suggests a 33% reduction in anemia, a 57% reduction in iron deficiency anemia. |
| [36] | Ruel et al. | 2018 | Mozambique | Children (0–3 years for Mozambique’s specific studies) | No specific country findings for anemia were presented | Revision of the nutrition impacts of agricultural programs with new empirical evidence published from 2014 onwards. | - |
| [37] | Langer et al. | 2015 | Portugal | Adolescent girls (10–19 years) | No specific country findings for anemia were presented; In 2013, iron deficiency anemia was among the top ten causes of disadjusted life years (DALYs) for 10–19 years-old adolescents girls (DALYs = 5.1). | Analysis of the major economic, environmental, social, political, demographic, and epidemiological transitions happening worldwide, their implications on the health system, and their effects on women and health; | Iron deficiency anemia is among the most important risk factors for mortality for girls aged 15–19 years, accounting for a substantial portion of DALYs through its contribution to cognitive impairment, susceptibility to infection, and limited work capacity. It is also a major factor in more than 115 000 maternal deaths and 591,000 perinatal deaths worldwide every year. |
| [38] | Diaz et al. | 2018 | Portugal | Pregnant women (more specifically women with vaginal deliveries who were admitted in labour; Trial conducted between 2006 and 2007) | There was not report on postpartum anemia (defined as Hb lower than 9 mg/dL). | Systematic review | “Depending on the rate of blood loss and other factors, such as pre-existing anemia, untreated postpartum hemorrhage can lead to hypovolemic shock, multi-organ dysfunction, and maternal death, within two to six hours. The cluster-randomized trial (Zhang 2010), was conducted between 2006 and 2007 and included 25,381 women with vaginal deliveries who were admitted in labour to the 78 maternity units participating in the study (included 05 maternity units in Portugal).” |
| [39] | De-Regil et al. | 2015 | Portugal | Cohort study of births (1988–1988) in 10 countries (including Portugal) | No specific country findings for anemia were presented, as the study design of the research was out of the scope of the review. | Systematic review | - |
| [40] | Vos Theo et al. | 2015 | Mozambique and Portugal | Childhood and Individuals aged 15–49 years and 50–69 years | Iron deficiency anemia was among the ten causes of years lived with disability in Mozambique (in 2013). Anemia wasn’t among the 10 leading causes of disability in Portugal | 1990–2013; Estimations of anemia prevalence and distribution of mild, moderate, and severe anemia by cause; Disaggregation of marginal estimates of anemia severity and cause; years lived with disability(YLD) computations | “By 2013, 49·2% of individuals had mild anaemia, 46·9% had moderate anaemia, and 3·9% had severe anaemia. Iron deficiency anaemia accounted for 62·6% of all cases and 31·5% of mild, 28·7% of moderate, and 2·4% of severe anaemia.” |
| [40] | Wang et al. | 2016 | Mozambique and Portugal | Children under 5 years and Young adults and adults (15–70 years) | Neither iron deficiency anemia nor nutritional deficiencies were among the ten leading causes of YLLs (with the ratio of observed YLLs to YLLs expected on the basis of SDI in 2015) in Mozambique and Portugal; no specific country findings for anemia were presented. | 1990–2015; Estimations of global age-standardised death rates for males versus females, by GBD cause; Estimations of years of lost life(YLLs); social demographic index(SDI) computations | “Hookworm infections can cause iron deficiency anemia, which is then recorded as the underlying cause of death.” |
| [41] | Forouzanfar et al. | 2015 | Mozambique and Portugal | Females and Males | Iron deficiency was not among the ten leading risk factors in terms of attributable DALYs for Portugal and Mozambique in 2013 for both sexes combined. | 1990–2013; Attributable deaths, years of life lost, years lived with disability, and disability-adjusted life-years (DALYs); estimations of the distribution of exposure | “Iron deficiency accounted for less than 200,000 deaths but was a major cause of DALYs due to its crucial role as a cause of anemia.” |
| [42] | Vos Theo et al. | 2016 | Mozambique and Portugal | Children younger that 5 years old and Older children; Young adults (15–39 years old) | Ratio of observed YLDs to YLDs on basis of SDI in 2015 = 0.71 (anemia was among the 10 leading causes of disability in Mozambique). Anemia was not among the 10 leading causes of disability in Portugal. | 1990–2015; estimations of anemia prevalence and at different levels of severity; years lived with disability (YLDS) and Social demographic index(SDI) computations | First leading cause in children younger than 5 years and among top 10 causes in older children and adolescents and young adults(15–39 years old) |
| [43] | Vos Theo et al. | 2017 | Mozambique and Portugal | Childhood and Women in reproductive age and older women | Ratio of observed YLDs to YLDs on basis of SDI in 2016 = 0.98 (anemia was among the 10 leading causes of disability in Mozambique). Anemia was not among the 10 leading causes of disability in Portugal. | 2006–2016; estimations of anemia prevalence; years lived with disability(YLD) and Social demographic index(SDI) computations | Iron deficiency anemia was among the leading level 4 causes of age-standardized YLD for Mozambican females in 2016; iron deficiency anemia was among the main conditions contributing to higher YLD rates in women; In childhood, nutritional deficiencies (mostly iron deficiency anemia) were among the main causes of YLDs. |
| [45] | Naghavi et al. | 2017 | Mozambique and Portugal | Children under 5 years and Young adults and adults (15–70 years) | Neither iron deficiency anemia nor nutritional deficiencies were among the ten leading causes of total YLLs (with the ratio of observed YLLs to YLLs expected on the basis of SDI in 2016) in Mozambique and Portugal; no specific country findings for anemia were presented. | 2006–2016; estimations of cause-specific deaths and years of life lost (YLLs) | “Age-standardized mortality rates for all nutritional deficiencies decreased by 23·7% (95% UI 15·4–30·8) from 7·26 deaths (6·75–7·86) per 100,000 in 2006 to 5·54 deaths (5·04–6·34) per 100 000 in 2016.” |
| [46] | Gakidou et al. | 2017 | Mozambique and Portugal | Pregnant women, Children and Adults | No specific country findings for anemia were presented. | 1990–2016; estimations of levels and trends in exposure, attributable deaths, and attributable disability-adjusted life-years (DALYs), by age group, sex, year. | “For deaths, the proportion attributable to measured risk factors, such as communicable, maternal, neonatal, and nutritional causes was 57·9% (55·4–61·0). Risk modification was an important contributor to reductions in communicable, maternal, neonatal, and nutritional causes.” |
| [47] | Stanaway et al. | 2018 | Mozambique and Portugal | Children under 5 years and Women of reproductive age | No specific country findings for anemia were presented; globally in 2017, dietary risks were the leading Level 2 risk factor for deaths. | 2017; dietary iron deficiency (expressed in terms of prevalence and YLDs); exposure to iron deficiency remained expressed as the counterfactual hemoglobin concentration | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Maulide Cane, R.; Chidassicua, J.B.; Varandas, L.; Craveiro, I. Anemia in Pregnant Women and Children Aged 6 to 59 Months Living in Mozambique and Portugal: An Overview of Systematic Reviews. Int. J. Environ. Res. Public Health 2022, 19, 4685. https://doi.org/10.3390/ijerph19084685
Maulide Cane R, Chidassicua JB, Varandas L, Craveiro I. Anemia in Pregnant Women and Children Aged 6 to 59 Months Living in Mozambique and Portugal: An Overview of Systematic Reviews. International Journal of Environmental Research and Public Health. 2022; 19(8):4685. https://doi.org/10.3390/ijerph19084685
Chicago/Turabian StyleMaulide Cane, Réka, José Braz Chidassicua, Luís Varandas, and Isabel Craveiro. 2022. "Anemia in Pregnant Women and Children Aged 6 to 59 Months Living in Mozambique and Portugal: An Overview of Systematic Reviews" International Journal of Environmental Research and Public Health 19, no. 8: 4685. https://doi.org/10.3390/ijerph19084685
APA StyleMaulide Cane, R., Chidassicua, J. B., Varandas, L., & Craveiro, I. (2022). Anemia in Pregnant Women and Children Aged 6 to 59 Months Living in Mozambique and Portugal: An Overview of Systematic Reviews. International Journal of Environmental Research and Public Health, 19(8), 4685. https://doi.org/10.3390/ijerph19084685







