A Protocol for a Mixed-Methods Process Evaluation of a Local Population Health Management System to Reduce Inequities in COVID-19 Vaccination Uptake
Abstract
:1. Introduction
- ‑
- To understand how staff use a specific population health management system tool to inform decisions and ways of working that reduce inequities in order to help the local area further develop their system;
- ‑
- To develop the capacity for wider evaluation of PHM systems.
1.1. Context: The Population Health Management Innovation
1.2. Objectives
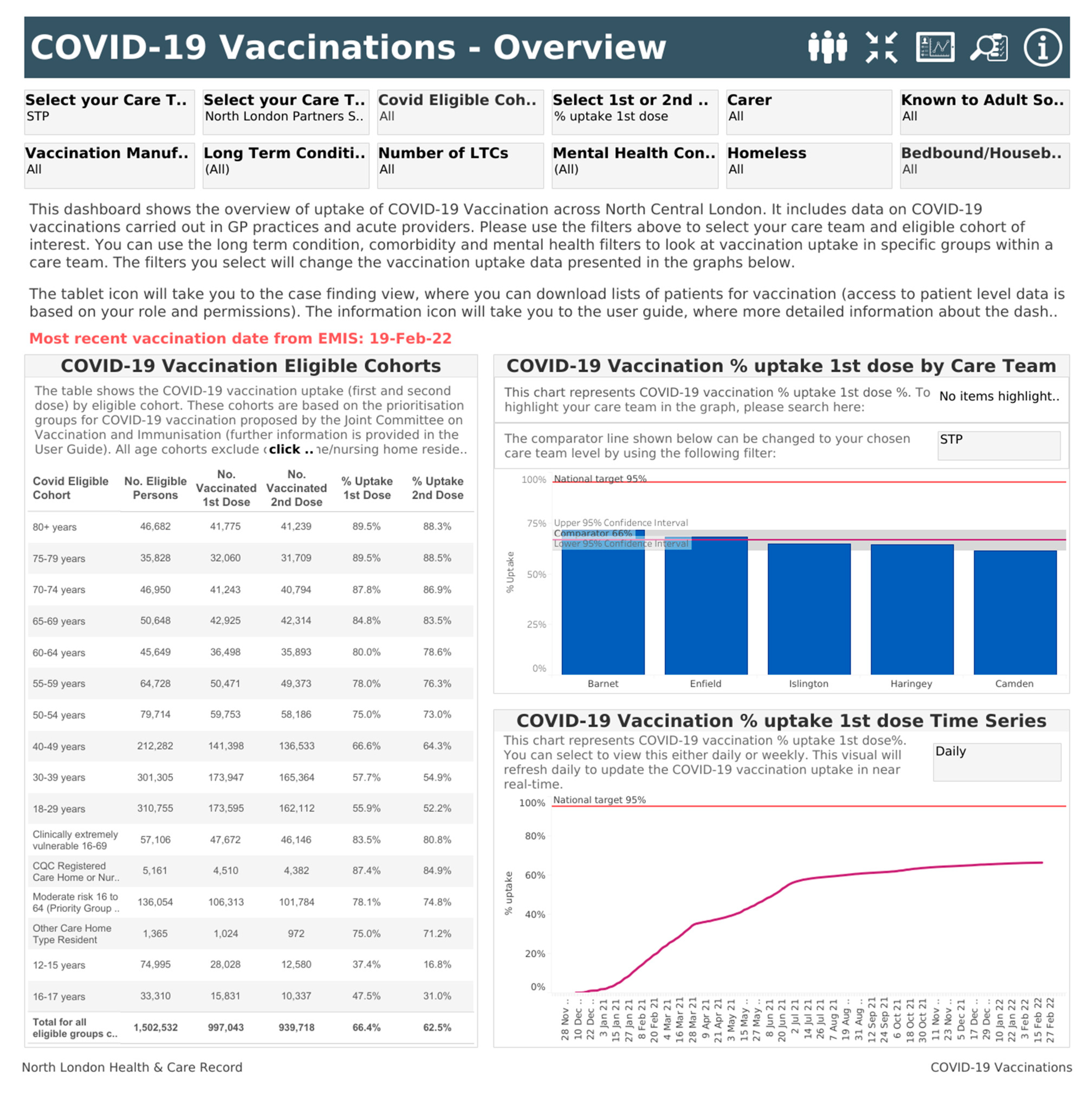
- To describe how (or whether) staff report using evidence of inequities in uptake available in the HealtheIntent COVID-19 Vaccination Dashboard to address inequities;
- To describe staff usage of the HealtheIntent COVID-19 Vaccination Dashboard, particularly those parts of the Dashboard that display evidence of inequities in uptake.
2. Materials and Methods
2.1. Proposed Qualitative Data Collection and Analysis
- ‑
- Motivation to use the Dashboard;
- ‑
- Specific features of the Dashboard and their advantages or limitations for the user;
- ‑
- Contextual enablers or barriers to using the Dashboard;
- ‑
- How the participants considered that usage of the Dashboard influenced ways of working and decisions, e.g., about COVID-19 vaccination planning or delivery.
2.2. Proposed Quantitative Data Extraction and Analysis
2.3. Combining Qualitative and Quantitative Data: Proposed Approach
3. Discussion
Strengths and Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- NHS England. NHS Long Term Plan. 2019. Available online: https://www.longtermplan.nhs.uk/ (accessed on 28 February 2022).
- Department of Health and Social Care. Integration and Innovation: Working Together to Improve Health and Social Care for All. 2021. Available online: https://www.gov.uk/government/publications/working-together-to-improve-health-and-social-care-for-all (accessed on 28 February 2022).
- Rosen, R.; Mountford, J.; Lewis, G.; Lewis, R.; Shand, J.; Shaw, S. Integration in Action: Four International Case Studies The Nuffield Trust: London, UK. 2011. Available online: https://www.nuffieldtrust.org.uk/research/integration-in-action-four-international-case-studies (accessed on 28 February 2022).
- Bottle, A.; Cohen, C.; Lucas, A.; Saravanakumar, K.; Ul-Haq, Z.; Smith, W.; Majeed, A.; Aylin, P. How an electronic health record became a real-world research resource: Comparison between London’s Whole Systems Integrated Care database and the Clinical Practice Research Datalink. BMC Med. Inform. Decis. Mak. 2020, 20, 71. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ingram, E.; Cooper, S.; Beardon, S.; Körner, K.; McDonald, H.I.; Hogarth, S.; Gomes, M.; Sheringham, J. Barriers and facilitators of use of analytics for strategic health and care decision-making: A qualitative study of senior health and care leaders’ perspectives. BMJ Open 2022, 12, e055504. [Google Scholar] [CrossRef] [PubMed]
- Scott, P.; Emerson, K.; Henderson-Reay, T. Data saves lives. BMJ 2021, 374, n1694. [Google Scholar] [CrossRef] [PubMed]
- Bhuiya, A.D.; Hajimirsadeghi, S.O.; North, H. When Population Health Meets General Practice—A Brief Introduction to Dashboards and Registries BJGP Life [Online]. 2022. Available online: https://bjgplife.com/when-population-health-meets-general-practice-a-brief-introduction-to-dashboards-and-registries/ (accessed on 28 February 2022).
- NHS England. Population Health and the Population Health Management Programme. Available online: https://www.england.nhs.uk/integratedcare/what-is-integrated-care/phm/ (accessed on 28 February 2022).
- MICO Consultancy. The Leeds Care Record: Benefits Review & Evaluation. Available online: https://www.leedscarerecord.org/content/uploads/2020/04/Leeds-Care-Record-Benefits-19-20.pdf (accessed on 28 February 2022).
- Alam, R.; Cheraghi-Sohi, S.; Panagioti, M.; Esmail, A.; Campbell, S.; Panagopoulou, E. Managing diagnostic uncertainty in primary care: A systematic critical review. BMC Fam. Pract. 2017, 18, 79. [Google Scholar] [CrossRef] [PubMed]
- Moore, G.F.; Audrey, S.; Barker, M.; Bond, L.; Bonell, C.; Hardeman, W.; Moore, L.; O’Cathain, A.; Tinati, T.; Wight, D.; et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ 2015, 350, h1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Department of Health and Social Care. Priority Groups for Coronavirus (COVID-19) Vaccination: Advice from the JCVI, 30 December 2020. Available online: https://www.gov.uk/government/publications/priority-groups-for-coronavirus-covid-19-vaccination-advice-from-the-jcvi-30-december-2020 (accessed on 7 January 2022).
- Department of Health and Social Care. JCVI Final Statement on Phase 2 of the COVID-19 Vaccination Programme: 13 April 2021. Available online: https://www.gov.uk/government/publications/priority-groups-for-phase-2-of-the-coronavirus-covid-19-vaccination-programme-advice-from-the-jcvi/jcvi-final-statement-on-phase-2-of-the-covid-19-vaccination-programme-13-april-2021 (accessed on 6 January 2022).
- The Scientific Advisory Group for Emergencies (SAGE). Factors Influencing COVID-19 Vaccine Uptake among Minority Ethnic Groups; DHSC: London, UK, 2021. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/952716/s0979-factors-influencing-vaccine-uptake-minority-ethnic-groups.pdf (accessed on 28 February 2022).
- Williamson, E.J.; Walker, A.J.; Bhaskaran, K.; Bacon, S.; Bates, C.; Morton, C.E.; Curtis, H.J.; Mehrkar, A.; Evans, D.; Inglesby, P.; et al. Factors associated with COVID-19-related death using OpenSAFELY. Nature 2020, 584, 430–436. [Google Scholar] [CrossRef] [PubMed]
- Smith, K.B.; Hill, C.S.E. Background and Introduction: UK Experiences of Health Inequalities. In Health Inequalities: Critical Perspectives; Smith, K.B., Hill, C.S.E., Eds.; Oxford Scholarship Online: Online, 2016. [Google Scholar]
- Vindrola-Padros, C.; Johnson, G.A. Rapid Techniques in Qualitative Research: A Critical Review of the Literature. Qual. Health Res. 2020, 30, 1596–1604. [Google Scholar] [CrossRef] [PubMed]
- May, C.; Finch, T. Implementing, Embedding, and Integrating Practices: An Outline of Normalization Process Theory. Sociology 2009, 43, 535–554. [Google Scholar] [CrossRef]
- Gale, N.K.; Heath, G.; Cameron, E.; Rashid, S.; Redwood, S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med. Res. Methodol. 2013, 13, 117. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- StataCorp Stata Statistical Software: Release 16; StataCorp LP: College Station, TX, USA, 2016.
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watson, G.; Moore, C.; Aspinal, F.; Boa, C.; Edeki, V.; Hutchings, A.; Raine, R.; Sheringham, J. A Protocol for a Mixed-Methods Process Evaluation of a Local Population Health Management System to Reduce Inequities in COVID-19 Vaccination Uptake. Int. J. Environ. Res. Public Health 2022, 19, 4588. https://doi.org/10.3390/ijerph19084588
Watson G, Moore C, Aspinal F, Boa C, Edeki V, Hutchings A, Raine R, Sheringham J. A Protocol for a Mixed-Methods Process Evaluation of a Local Population Health Management System to Reduce Inequities in COVID-19 Vaccination Uptake. International Journal of Environmental Research and Public Health. 2022; 19(8):4588. https://doi.org/10.3390/ijerph19084588
Chicago/Turabian StyleWatson, Georgia, Cassie Moore, Fiona Aspinal, Claudette Boa, Vusi Edeki, Andrew Hutchings, Rosalind Raine, and Jessica Sheringham. 2022. "A Protocol for a Mixed-Methods Process Evaluation of a Local Population Health Management System to Reduce Inequities in COVID-19 Vaccination Uptake" International Journal of Environmental Research and Public Health 19, no. 8: 4588. https://doi.org/10.3390/ijerph19084588
APA StyleWatson, G., Moore, C., Aspinal, F., Boa, C., Edeki, V., Hutchings, A., Raine, R., & Sheringham, J. (2022). A Protocol for a Mixed-Methods Process Evaluation of a Local Population Health Management System to Reduce Inequities in COVID-19 Vaccination Uptake. International Journal of Environmental Research and Public Health, 19(8), 4588. https://doi.org/10.3390/ijerph19084588





