A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications
Abstract
1. Introduction
1.1. COVID-19 and Mental Health
Adolescent Mental Health
1.2. Situating This Study in the Context of a Pandemic
2. Materials and Methods
2.1. Participants
2.2. Demographics and COVID-19 Questionnaire
2.3. Psychological Scales
2.3.1. Stress
2.3.2. Anxiety
2.3.3. Co-Rumination
2.3.4. Depression
2.4. Procedure
2.5. Statistical Analyses
3. Results
3.1. Sample Characteristics
3.2. COVID-19 Questionnaire
3.2.1. Frequency and Impact of Symptoms Resembling COVID-19
3.2.2. COVID-19 Discussions
3.2.3. Media Use
3.2.4. Stress and Concerns Related to COVID-19
3.3. Adolescent Mental Health in the Context of COVID-19
3.3.1. Stress
3.3.2. Anxiety
3.3.3. Co-rumination
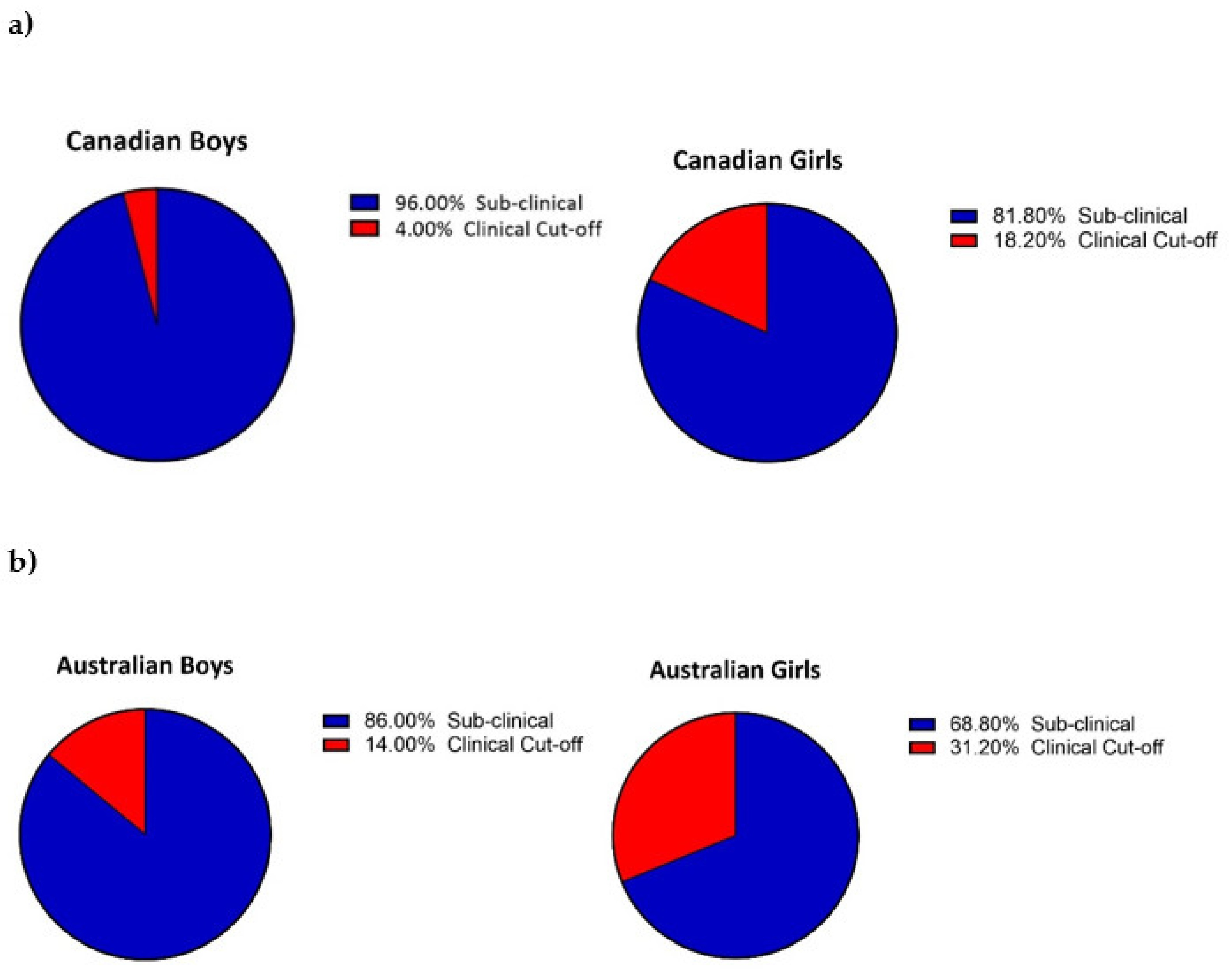
3.3.4. Depression
3.4. Exploratory Inter-Item Analysis on Perceived Stress
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Callaway, E.; Cyranoski, D.; Mallapaty, S.; Stoye, E.; Tollefson, J. The coronavirus pandemic in five powerful charts. Nature 2020, 579, 482–483. [Google Scholar] [CrossRef] [PubMed]
- Thombs, B.D.; Bonardi, O.; Rice, D.B.; Boruff, J.T.; Azar, M.; He, C.; Markham, S.; Sun, Y.; Wu, Y.; Krishnan, A.; et al. Curating evidence on mental health during COVID-19: A living systematic review. J. Psychosom. Res. 2020, 133, 110113. [Google Scholar] [CrossRef] [PubMed]
- World Health Organisation. Weekly Epidemiological Update on COVID-19—6 July 2021. Available online: https://www.who.int/publications/m/item/weekly-epidemiological-update-on-covid-19---6-july-2021 (accessed on 7 December 2021).
- Bell, G. Pandemic Passages: An Anthropological Account of Life and Liminality during COVID-19. Anthropol. Action 2021, 28, 79–84. [Google Scholar] [CrossRef]
- Kumar, A.; Nayar, K.R. COVID 19 and its mental health consequences. J. Ment. Health 2021, 30, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Ahmed, M.Z.; Ahmed, O.; Aibao, Z.; Hanbin, S.; Siyu, L.; Ahmad, A. Epidemic of COVID-19 in China and associated Psychological Problems. Asian J. Psychiatry 2020, 51, 102092. [Google Scholar] [CrossRef]
- Dong, F.; Liu, H.-L.; Dai, N.; Yang, M.; Liu, J.-P. A living systematic review of the psychological problems in people suffering from COVID-19. J. Affect. Disord. 2021, 292, 172–188. [Google Scholar] [CrossRef]
- Sturman, D.A.; Moghaddam, B. The neurobiology of adolescence: Changes in brain architecture, functional dynamics, and behavioral tendencies. Neurosci. Biobehav. Rev. 2011, 35, 1704–1712. [Google Scholar] [CrossRef]
- Kessler, R.C.; Amminger, G.P.; Aguilar-Gaxiola, S.; Alonso, J.; Lee, S.; Ustün, T.B. Age of onset of mental disorders: A review of recent literature. Curr. Opin. Psychiatry 2007, 204, 359–364. [Google Scholar] [CrossRef]
- Guessoum, S.B.; Lachal, J.; Radjack, R.; Carretier, E.; Minassian, S.; Benoit, L.; Moro, M.R. Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 2020, 291, 113264. [Google Scholar] [CrossRef]
- Viner, R.M.; Russell, S.J.; Croker, H.; Packer, J.; Ward, J.; Stansfield, C.; Mytton, O.; Bonell, C.; Booy, R. School closure and management practices during coronavirus outbreaks including COVID-19: A rapid systematic review. Lancet Child Adolesc. Health 2020, 4, 397–404. [Google Scholar] [CrossRef]
- Singh, S.; Roy, D.; Sinha, K.; Parveen, S.; Sharma, G.; Joshi, G. Impact of COVID-19 and lockdown on mental health of children and adolescents: A narrative review with recommendations. Psychiatry Res. 2020, 293, 113429. [Google Scholar] [CrossRef]
- Duan, L.; Shao, X.; Wang, Y.; Huang, Y.; Miao, J.; Yang, X.; Zhu, G. An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect. Disord. 2020, 275, 112–118. [Google Scholar] [CrossRef]
- Ma, Z.; Idris, S.; Zhang, Y.; Zewen, L.; Wali, A.; Ji, Y.; Pan, Q.; Baloch, Z. The impact of COVID-19 pandemic outbreak on education and mental health of Chinese children aged 7–15 years: An online survey. BMC Pediatrics 2021, 21, 95. [Google Scholar] [CrossRef]
- Giannopoulou, I.; Efstathiou, V.; Triantafyllou, G.; Korkoliakou, P.; Douzenis, A. Adding stress to the stressed: Senior high school students’ mental health amidst the COVID-19 nationwide lockdown in Greece. Psychiatry Res. 2021, 295, 113560. [Google Scholar] [CrossRef]
- Hafstad, G.S.; Sætren, S.S.; Wentzel-Larsen, T.; Augusti, E.-M. Adolescents’ symptoms of anxiety and depression before and during the Covid-19 outbreak—A prospective population-based study of teenagers in Norway. Lancet Reg. Health Eur. 2021, 5, 100093. [Google Scholar] [CrossRef]
- Liang, L.; Ren, H.; Cao, R.; Hu, Y.; Qin, Z.; Li, C.; Mei, S. The Effect of COVID-19 on Youth Mental Health. Psychiatr. Q. 2020, 91, 841–852. [Google Scholar] [CrossRef]
- Magson, N.R.; Freeman, J.Y.A.; Rapee, R.M.; Richardson, C.E.; Oar, E.L.; Fardouly, J. Risk and Protective Factors for Prospective Changes in Adolescent Mental Health during the COVID-19 Pandemic. J. Youth Adolesc. 2021, 50, 44–57. [Google Scholar] [CrossRef]
- Meda, N.; Pardini, S.; Slongo, I.; Bodini, L.; Zordan, M.A.; Rigobello, P.; Visioli, F.; Novara, C. Students’ mental health problems before, during, and after COVID-19 lockdown in Italy. J. Psychiatr. Res. 2021, 134, 69–77. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Otto, C.; Adedeji, A.; Devine, J.; Erhart, M.; Napp, A.-K.; Becker, M.; Blanck-Stellmacher, U.; Löffler, C.; et al. Mental Health and Quality of Life in Children and Adolescents During the COVID-19 Pandemic-Results of the Copsy Study. Dtsch. Arztebl. Int. 2020, 117, 828–829. [Google Scholar] [CrossRef]
- Rogers, A.A.; Ha, T.; Ockey, S. Adolescents’ Perceived Socio-Emotional Impact of COVID-19 and Implications for Mental Health: Results From a U.S.-Based Mixed-Methods Study. J. Adolesc. Health 2021, 68, 43–52. [Google Scholar] [CrossRef]
- Thorisdottir, I.E.; Asgeirsdottir, B.B.; Kristjansson, A.L.; Valdimarsdottir, H.B.; Jonsdottir Tolgyes, E.M.; Sigfusson, J.; Allegrante, J.P.; Sigfusdottir, I.D.; Halldorsdottir, T. Depressive symptoms, mental wellbeing, and substance use among adolescents before and during the COVID-19 pandemic in Iceland: A longitudinal, population-based study. Lancet Psychiatry 2021, 8, 663–672. [Google Scholar] [CrossRef]
- Zhou, S.-J.; Zhang, L.-G.; Wang, L.-L.; Guo, Z.-C.; Wang, J.-Q.; Chen, J.-C.; Liu, M.; Chen, X.; Chen, J.-X. Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 2020, 29, 749–758. [Google Scholar] [CrossRef]
- World Health Organisation. Rolling Updates on Coronavirus Disease (COVID-19). 2021. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/events-as-they-happen (accessed on 7 December 2021).
- Ministère de la Santé et des Services Sociaux. Historique du Portrait Quotidien des cas Confirmés. 2021. Available online: https://www.donneesquebec.ca/recherche/dataset/covid-19-portrait-quotidien-des-cas-confirmes/resource/d2cf4211-5400-46a3-9186-a81e6cd41de9 (accessed on 7 December 2021).
- Queensland Government. Queensland COVID-19 Statistics. 2021. Available online: https://www.qld.gov.au/health/conditions/health-alerts/coronavirus-covid-19/current-status/statistics#casesummary (accessed on 7 December 2021).
- Gouvernement du Québec. List of all Infographics Related to the Prime Minister’s Announcements (COVID-19). 2021. Available online: https://www.quebec.ca/en/premier/premier/access-to-publications-related-to-the-premiers-announcements-concerning-covid-19/liste-de-toutes-les-infographies-en-lien-avec-les-annonces-du-premier-ministre-covid-19 (accessed on 7 December 2021).
- Queensland Government. Roadmap to Easing Queensland’s Restrictions. 2020. Available online: https://www.torres.qld.gov.au/downloads/file/510/covid-19-restrictions-roadmap-3-july-2020 (accessed on 7 December 2021).
- White, B.P. The Perceived Stress Scale for Children: A pilot study in a sample of 153 children. Int. J. Pediatrics Child Health 2014, 2, 45–52. [Google Scholar] [CrossRef]
- Crum, A.J.; Salovey, P.; Achor, S. Rethinking stress: The role of mindsets in determining the stress response. J. Pers. Soc. Psychol. 2013, 104, 716–733. [Google Scholar] [CrossRef] [PubMed]
- Silverman, W.K.; Fleisig, W.; Rabian, B.; Peterson, R.A. Childhood anxiety sensitivity index. J. Clin. Child Adolesc. Psychol. 1991, 20, 162–168. [Google Scholar] [CrossRef]
- Stassart, C.; Etienne, A.M. A French translation of the Childhood Anxiety Sensitivity Index (CASI): Factor structure, reliability and validity of this scale in a nonclinical sample of children. Psychol. Belg. 2014, 54, 222–241. [Google Scholar] [CrossRef][Green Version]
- Spielberger, C. State-Trait Anxiety Inventory for Children Preliminary Manual; Consulting Psychologists Press: Palo Alto, CA, USA, 1973. [Google Scholar]
- Turgeon, L.; Chartrand, É. Reliability and Validity of the Revised Children’s Manifest Anxiety Scale in a French-Canadian Sample. Psychol. Assess. 2003, 15, 378–383. [Google Scholar] [CrossRef] [PubMed]
- Wren, D.G.; Benson, J. Measuring test anxiety in children: Scale development and internal construct validation. Anxiety Stress Coping 2004, 17, 227–240. [Google Scholar] [CrossRef]
- Arroyo, A. Fat Talk Among Female Friends: Do Friends’ Responses Buffer the Relationship between Fat Talk and Health-Related Outcomes? 2013. Available online: https://repository.arizona.edu/handle/10150/297031 (accessed on 7 January 2020).
- Rose, A.J. Co–Rumination in the Friendships of Girls and Boys. Child Dev. 2002, 73, 1830–1843. [Google Scholar] [CrossRef] [PubMed]
- Beck, A.T.; Steer, R.A.; Brown, G.K. Beck Depression Inventory (BDI-II); Pearson: London, UK, 1996; Volume 10. [Google Scholar]
- Bourque, P.; Beaudette, D. Étude psychometrique du questionnaire de dépression de Beck auprès d’un échantillon d’étudiants universitaires francophones [Psychometric study of the Beck Depression Inventory on a sample of French-speaking university students]. Can. J. Behav. Sci./Rev. Can. Sci. Comport. 1982, 14, 211–218. [Google Scholar] [CrossRef]
- Kroenke, K.; Spitzer, R.L.; Williams, J.B.W. The PHQ-9: Validity of a brief depression severity measure. J. Gen. Intern. Med. JGIM 2001, 16, 606–613. [Google Scholar] [CrossRef]
- Johnson, J.G.; Harris, E.S.; Spitzer, R.L.; Williams, J.B. The patient health questionnaire for adolescents: Validation of an instrument for the assessment of mental disorders among adolescent primary care patients. J. Adolesc. Health 2002, 30, 196–204. [Google Scholar] [CrossRef]
- Qualtrics. The Output for this Paper was Generated using Qualtrics Software, July 2020 Version of the Qualtrics Research Suite. Copyright © 2021 Qualtrics. Qualtrics and All Other Qualtrics Product or Service Names are Registered Trademarks or Trademarks of Qualtrics, Provo, UT, USA. Available online: http://www.qualtrics.com (accessed on 8 January 2020).
- Journault, A.; Lupien, S. Addendum to MATA’s Study: Stress Mindset Intervention; OSF: Charlottesville, VA, USA, 2020. [Google Scholar] [CrossRef]
- Byrne, B.M. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming, 2nd ed.; Routledge: New York, NY, USA, 2010. [Google Scholar] [CrossRef]
- Hair, J.F.; Black, W.C.; Babin, B.J.; Anderson, R.E. Multivariate Data Analysis: International Version; Pearson: Hoboken, NJ, USA, 2010. [Google Scholar]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences; Academic Press: Cambridge, MA, USA, 1988; 2013. [Google Scholar]
- Kim, H.-Y. Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restor. Dent. Endod. 2017, 42, 152–155. [Google Scholar] [CrossRef]
- Dolle, K.; Schulte-Körne, G.; O’Leary, A.M.; von Hofacker, N.; Izat, Y.; Allgaier, A.-K. The Beck Depression Inventory-II in adolescent mental health patients: Cut-off scores for detecting depression and rating severity. Psychiatry Res. 2012, 200, 843–848. [Google Scholar] [CrossRef]
- Richardson, L.P.; McCauley, E.; Grossman, D.C.; McCarty, C.A.; Richards, J.; Russo, J.E.; Rockhill, C.; Katon, W. Evaluation of the Patient Health Questionnaire-9 Item for detecting major depression among adolescents. Pediatrics 2010, 126, 1117–1123. [Google Scholar] [CrossRef]
- Elmer, T.; Mepham, K.; Stadtfeld, C. Students under lockdown: Comparisons of students’ social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS ONE 2020, 15, e0236337. [Google Scholar] [CrossRef]
- Dong, E.; Du, H.; Gardner, L. An interactive web-based dashboard to track COVID-19 in real time. Lancet Infect. Dis. 2020, 20, 533–534. [Google Scholar] [CrossRef]
- Liu, P.L. COVID-19 information seeking on digital media and preventive behaviors: The mediation role of worry. Cyberpsychol. Behav. Soc. Netw. 2020, 23, 677–682. [Google Scholar] [CrossRef]
- McCrindle. MyStrengths Youth Wellbeing Report 2021. 2021. Available online: https://s3.amazonaws.com/kajabi-storefronts-production/sites/163568/themes/2149125913/downloads/TnT1pVifTn62tOGicnyT_MyStrengths_Youth_Wellbeing_Report_2021.pdf (accessed on 8 January 2022).
- Kennedy, J.; Lynch, H. A shift from offline to online: Adolescence, the internet and social participation. J. Occup. Sci. 2016, 23, 156–167. [Google Scholar] [CrossRef]
- Petersen, A.C.; Sarigiani, P.A.; Kennedy, R.E. Adolescent depression: Why more girls? J. Youth Adolesc. 1991, 20, 247–271. [Google Scholar] [CrossRef]
- Jose, P.E.; Wilkins, H.; Spendelow, J.S. Does social anxiety predict rumination and co-rumination among adolescents? J. Clin. Child Adolesc. Psychol. 2012, 41, 86–91. [Google Scholar] [CrossRef]
- Carter, R.; Silverman, W.K.; Jaccard, J. Sex variations in youth anxiety symptoms: Effects of pubertal development and gender role orientation. J. Clin. Child Adolesc. Psychol. 2011, 40, 730–741. [Google Scholar] [CrossRef]
- MacLean, A.; Sweeting, H.; Egan, M.; Der, G.; Adamson, J.; Hunt, K. How robust is the evidence of an emerging or increasing female excess in physical morbidity between childhood and adolescence? Results of a systematic literature review and meta-analyses. Soc. Sci. Med. 2013, 78, 96–112. [Google Scholar] [CrossRef]
- Rosenman, R.; Tennekoon, V.; Hill, L.G. Measuring bias in self-reported data. Int. J. Behav. Healthc. Res. 2011, 2, 320–332. [Google Scholar] [CrossRef]

| Variable | Canada (N = 913) | Australia (N = 413) | Country p-Value | Gender p-Value | ||
| Boys (n = 198) | Girls (n = 708) | Boys (n = 172) | Girls (n = 234) | |||
| PSS-C | 12.21 (11.32, 13.11) | 15.39 (14.93, 15. 85) | 13.94 (12.93, 14.95) | 16.13 (15.28, 16.98) | 0.004 | <0.001 |
| N (Missing) | 178 (20) | 667 (41) | 140 (32) | 198 (36) | ||
| SMM-G | 1.61 (1.52, 1.70) | 1.54 (1.50, 1.59) | 1.81 (1.70, 1.92) | 1.75 (1.66, 1.84) | <0.001 | 0.167 |
| N (Missing) | 197 (1) | 689 (19) | 141 (31) | 202 (32) | ||
| CASI | 27.51 (26.54, 28.49) | 32.79 (32.27, 33.30) | 28.05 (26.92, 29.18) | 33.75 (32.78, 34.71) | 0.113 | <0.001 |
| N (Missing) | 192 (6) | 691 (17) | 144 (28) | 198 (36) | ||
| STAIC-S | 32.36 (31.38, 33.34) | 36.22 (35.71, 36.73) | 32.07 (30.94, 33.20) | 35.30 (34.36, 36.25) | 0.200 | <0.001 |
| N (Missing) | 188 (10) | 682 (26) | 140 (32) | 201 (33) | ||
| CTAS | 50.37 (47.90, 52.83) | 58.93 (57.66, 60.21) | 52.15 (49.45, 54.85) | 64.04 (61.75, 66.33) | 0.003 | <0.001 |
| N (Missing) | 169 (29) | 631 (77) | 141 (31) | 196 (38) | ||
| CRQ | 26.68 (25.55, 27.82) | 29.69 (29.12, 30.27) | 23.73 (22.45, 24.98) | 29.94 (28.89, 30.98) | 0.010 | <0.001 |
| N (Missing) | 170 (28) | 647 (61) | 139 (33) | 200 (34) | ||
| Depression Z Scores (BDI-II, PHQ9-A) | −0.43 (−0.57, −0.28) | 0.11 (0.04, 0.19) | −0.35 (0.51, −0.19) | 0.24 (0.10, 0.37) | 0.141 | <0.001 |
| N (Missing) | 173 (25) | 652 (56) | 137 (35) | 203 (31) | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marie, R.; Journault, A.-A.; Cernik, R.; Welch, P.; Lupien, S.; McDermott, B.; Moxon, J.V.; Sarnyai, Z. A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications. Int. J. Environ. Res. Public Health 2022, 19, 4407. https://doi.org/10.3390/ijerph19074407
Marie R, Journault A-A, Cernik R, Welch P, Lupien S, McDermott B, Moxon JV, Sarnyai Z. A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications. International Journal of Environmental Research and Public Health. 2022; 19(7):4407. https://doi.org/10.3390/ijerph19074407
Chicago/Turabian StyleMarie, Riana, Audrey-Ann Journault, Rebecca Cernik, Paul Welch, Sonia Lupien, Brett McDermott, Joseph V. Moxon, and Zoltan Sarnyai. 2022. "A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications" International Journal of Environmental Research and Public Health 19, no. 7: 4407. https://doi.org/10.3390/ijerph19074407
APA StyleMarie, R., Journault, A.-A., Cernik, R., Welch, P., Lupien, S., McDermott, B., Moxon, J. V., & Sarnyai, Z. (2022). A Cross-Sectional Study Investigating Canadian and Australian Adolescents’ Perceived Experiences of COVID-19: Gender Differences and Mental Health Implications. International Journal of Environmental Research and Public Health, 19(7), 4407. https://doi.org/10.3390/ijerph19074407








