Body Fat Percentage and Normal-Weight Obesity in the Chinese Population: Development of a Simple Evaluation Indicator Using Anthropometric Measurements
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropometric Measurements
2.3. Body Composition
2.4. Grouping
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics and Body Composition
3.2. Circumference and Circumference Ratio
3.3. Correlation with BFP
3.4. Binary Logistic Regression Analysis
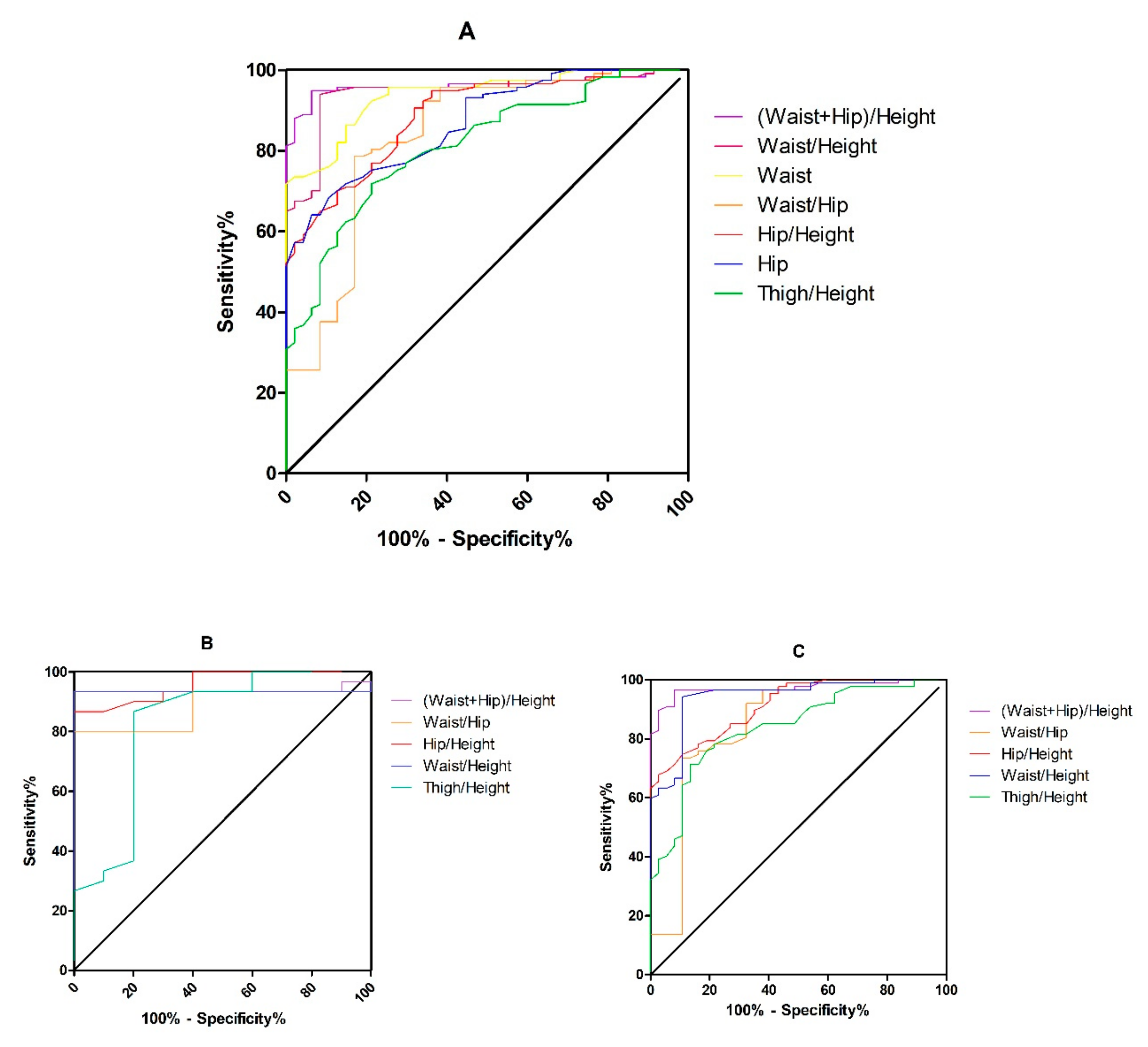
3.5. ROC Analysis and Cutoff Values
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Pan, X.-F.; Wang, L.; Pan, A. Epidemiology and determinants of obesity in China. Lancet Diabetes Endocrinol. 2021, 9, 373–392. [Google Scholar] [CrossRef]
- Wang, L.; Zhou, B.; Zhao, Z.; Yang, L.; Zhang, M.; Jiang, Y.; Li, Y.; Zhou, M.; Wang, L.; Huang, Z.; et al. Body-mass index and obesity in urban and rural China: Findings from consecutive nationally representative surveys during 2004–18. Lancet 2021, 398, 53–63. [Google Scholar] [CrossRef]
- Alammar, M.; Alsoghayer, S.; El-Abd, K.; Alkhenizan, A. Diagnostic Accuracy of Body Mass Index (BMI) When Diagnosing Obesity in a Saudi Adult Population in a Primary Care Setting, Cross Sectional, Retrospective Study. Diabetes Metab. Syndr. Obesity Targets Ther. 2020, 13, 2515–2520. [Google Scholar] [CrossRef] [PubMed]
- Jo, A.; Mainous, A.G., III. Informational value of percent body fat with body mass index for the risk of abnormal blood glucose: A nationally representative cross-sectional study. BMJ Open 2018, 8, e019200. [Google Scholar] [CrossRef]
- Okorodudu, D.O.; Jumean, M.F.; Montori, V.M.; Romero-Corral, A.; Somers, V.K.; Erwin, P.J.; Lopez-Jimenez, F. Diagnostic performance of body mass index to identify obesity as defined by body adiposity: A systematic review and meta-analysis. Int. J. Obes. 2010, 34, 791–799. [Google Scholar] [CrossRef] [PubMed]
- Romero-Corral, A.; Somers, V.K.; Sierra-Johnson, J.; Korenfeld, Y.; Boarin, S.; Korinek, J.; Jensen, M.D.; Parati, G.; Lopez-Jimenez, F. Normal weight obesity: A risk factor for cardiometabolic dysregulation and cardiovascular mortality. Eur. Heart J. 2009, 31, 737–746. [Google Scholar] [CrossRef]
- Diverse Populations Collaborative Group Weight-height relationships and body mass index: Some observations from the diverse populations collaboration. Am. J. Phys. Anthr. 2005, 128, 220–229. [CrossRef]
- Nogueira-De-Almeida, C.A.; Del Ciampo, L.A.; Ferraz, I.S.; Del Ciampo, I.R.L.; Contini, A.A.; da V Ued, F. COVID-19 and obesity in childhood and adolescence: A clinical review. J. Pediatr. 2020, 96, 546–558. [Google Scholar] [CrossRef]
- Ghosh, A.; Arora, B.; Gupta, R.; Anoop, S.; Misra, A. Effects of nationwide lockdown during COVID-19 epidemic on lifestyle and other medical issues of patients with type 2 diabetes in north India. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 917–920. [Google Scholar] [CrossRef]
- Bhutani, S.; Cooper, J.A. COVID-19–Related Home Confinement in Adults: Weight Gain Risks and Opportunities. Obesity 2020, 28, 1576–1577. [Google Scholar] [CrossRef]
- Zhu, Y.; Wang, Z.; Maruyama, H.; Onoda, K.; Huang, Q.; Hu, C.; Zhou, Y. Effect of the COVID-19 lockdown period on the physical condition, living habits, and physical activity of citizens in Beijing, China. J. Phys. Ther. Sci. 2021, 33, 632–636. [Google Scholar] [CrossRef] [PubMed]
- WHO/IASO/IOTF. Asia-Pacific Perspective: Redefining Obesity and Its Treatment; Health Communications Australia Pty Ltd.: Melbourne, Australia, 2000. [Google Scholar]
- Deurenberg, P.; Yap, M.; Van Staveren, W. Body mass index and percent body fat: A meta analysis among different ethnic groups. Int. J. Obes. 1998, 22, 1164–1171. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Byrne, N.; Kagawa, M.; Ma, G.; Poh, B.K.; Ismail, M.N.; Kijboonchoo, K.; Nasreddine, L.; Trinidad, T.P.; Hills, A.P. Ethnic differences in the relationship between body mass index and percentage body fat among Asian children from different backgrounds. Br. J. Nutr. 2011, 106, 1390–1397. [Google Scholar] [CrossRef] [PubMed]
- WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004, 363, 157–163. [Google Scholar] [CrossRef]
- Kagawa, M.; Kerr, D.; Uchida, H.; Binns, C.W. Differences in the relationship between BMI and percentage body fat between Japanese and Australian-Caucasian young men. Br. J. Nutr. 2006, 95, 1002–1007. [Google Scholar] [CrossRef] [PubMed]
- Gill, T. Epidemiology and health impact of obesity: An Asia Pacific perspective. Asia Pac. J. Clin. Nutr. 2006, 15, 3–14. [Google Scholar]
- Kim, S.; Kyung, C.; Park, J.S.; Lee, S.-P.; Kim, H.K.; Ahn, C.W.; Kim, K.R.; Kang, S. Normal-weight obesity is associated with increased risk of subclinical atherosclerosis. Cardiovasc. Diabetol. 2015, 14, 1–9. [Google Scholar] [CrossRef]
- Kim, J.Y.; Han, S.-H.; Yang, B.-M. Implication of high-body-fat percentage on cardiometabolic risk in middle-aged, healthy, normal-weight adults. Obesity 2012, 21, 1571–1577. [Google Scholar] [CrossRef]
- Levitt, D.G.; Heymsfield, S.B.; Pierson, R.N.; Shapses, S.A.; Kral, J.G. Erratum to: Physiological models of body composition and human obesity. Nutr. Metab. 2009, 6, 7. [Google Scholar] [CrossRef]
- Cao, L.; Jiang, Y.; Li, Q.; Wang, J.; Tan, S. Exercise Training at Maximal Fat Oxidation Intensity for Overweight or Obese Older Women: A Randomized Study. J. Sports Sci. Med. 2019, 18, 413–418. [Google Scholar]
- Woolcott, O.O.; Bergman, R.N. Relative fat mass (RFM) as a new estimator of whole-body fat percentage ─ A cross-sectional study in American adult individuals. Sci. Rep. 2018, 8, 10980. [Google Scholar] [CrossRef] [PubMed]
- Mørkedal, B.; Romundstad, P.R.; Vatten, L.J. Informativeness of indices of blood pressure, obesity and serum lipids in relation to ischaemic heart disease mortality: The HUNT-II study. Eur. J. Epidemiol. 2011, 26, 457–461. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Schneider, H.J.; Friedrich, N.; Klotsche, J.; Pieper, L.; Nauck, M.; John, U.; Dorr, M.; Felix, S.; Lehnert, H.; Pittrow, D.; et al. The Predictive Value of Different Measures of Obesity for Incident Cardiovascular Events and Mortality. J. Clin. Endocrinol. Metab. 2010, 95, 1777–1785. [Google Scholar] [CrossRef] [PubMed]
- Gradmark, A.M.I.; Rydh, A.; Renström, F.; De Lucia-Rolfe, E.; Sleigh, A.; Nordström, P.; Brage, S.; Franks, P. Computed tomography-based validation of abdominal adiposity measurements from ultrasonography, dual-energy X-ray absorptiometry and anthropometry. Br. J. Nutr. 2010, 104, 582–588. [Google Scholar] [CrossRef]
- Swainson, M.G.; Batterham, A.; Tsakirides, C.; Rutherford, Z.; Hind, K. Prediction of whole-body fat percentage and visceral adipose tissue mass from five anthropometric variables. PLoS ONE 2017, 12, e0177175. [Google Scholar] [CrossRef]
- Shafiee, G.; Qorbani, M.; Heshmat, R.; Djalalinia, S.; Motlagh, M.E.; Arefirad, T.; Gorabi, A.M.; Najafi, F.; Asayesh, H.; Kelishadi, R. Wrist circumference as a novel predictor of obesity in children and adolescents: The CASPIAN-IV study. J. Pediatr. Endocrinol. Metab. 2018, 31, 717–725. [Google Scholar] [CrossRef]
- Mercan, Y.; Kafadar, G.C.; Arikan, S.H.; Pancar, N. An investigation of anthropometric measurements of early adolescents and determination of BMI-for-age-based neck circumference and BMI-for-age-based mid-upper-arm circumference cut-off points. Clin. Nutr. ESPEN 2022, 48, 414–420. [Google Scholar] [CrossRef]
- Jung, K.J.; Kimm, H.; Yun, J.E.; Jee, S.H. Thigh Circumference and Diabetes: Obesity as a Potential Effect Modifier. J. Epidemiol. 2013, 23, 329–336. [Google Scholar] [CrossRef]
- Yang, S.S.; Wang, S.S.; Jia, W.P.; Han, K.; Tai, P.G.; Kou, F.Y.; Li, J.; Cao, W.Z.; Zhao, Y.L.; Zhu, Q.; et al. Relationship between obesity related anthropometric indicators and depression risk in Hainan centenarians. Zhonghua Liu Xing Bing Xue Za Zhi 2021, 42, 113–120. [Google Scholar]
- Wang, J.; Thornton, J.C.; Kolesnik, S.; Pierson, R.N. Anthropometry in Body Composition: An Overview. Ann. N. Y. Acad. Sci. 2006, 904, 317–326. [Google Scholar] [CrossRef]
- Stewart, A.; Marfell-Jones, M.; Olds, T.; de Ridder, H. International Standards for Anthropometric Assessment; International Standards for Anthropometric Assessment (ISAK): Lower Hutt, New Zealand, 2011. [Google Scholar]
- Kagawa, M. Differences in the obesity screening ability of 19 anthropometric parameters in young Japanese females: Comparisons of direct measurements, conventional and novel indices. Int. J. Kinanthropometry 2021, 1, 41–52. [Google Scholar] [CrossRef]
- Jayawardena, R.; Ranasinghe, P.; Ranathunga, T.; Mathangasinghe, Y.; Wasalathanththri, S.; Hills, A. Novel anthropometric parameters to define obesity and obesity-related disease in adults: A systematic review. Nutr. Rev. 2019, 78, 498–513. [Google Scholar] [CrossRef] [PubMed]
- Kuczmarski, R.J. Bioelectrical impedance analysis measurements as part of a national nutrition survey. Am. J. Clin. Nutr. 1996, 64, 453S–458S. [Google Scholar] [CrossRef] [PubMed]
- Franco, L.P.; Morais, C.C.; Cominetti, C. Normal-weight obesity syndrome: Diagnosis, prevalence, and clinical implications. Nutr. Rev. 2016, 74, 558–570. [Google Scholar] [CrossRef]
- Kim, M.K.; Han, K.; Kwon, H.-S.; Song, K.-H.; Yim, H.W.; Lee, W.-C.; Park, Y.-M. Normal weight obesity in Korean adults. Clin. Endocrinol. 2013, 80, 214–220. [Google Scholar] [CrossRef]
- Teufel, F.; Seiglie, J.A.; Geldsetzer, P.; Theilmann, M.; Marcus, M.E.; Ebert, C.; Arboleda, W.A.L.; Agoudavi, K.; Andall-Brereton, G.; Aryal, K.K.; et al. Body-mass index and diabetes risk in 57 low-income and middle-income countries: A cross-sectional study of nationally representative, individual-level data in 685 616 adults. Lancet 2021, 398, 238–248. [Google Scholar] [CrossRef]
- Frankenfield, D.C.; Rowe, W.A.; Cooney, R.N.; Smith, J.; Becker, D. Limits of body mass index to detect obesity and predict body composition. Nutrition 2001, 17, 26–30. [Google Scholar] [CrossRef]
- Jabłonowska-Lietz, B.; Wrzosek, M.; Włodarczyk, M.; Nowicka, G. New indexes of body fat distribution, visceral adiposity index, body adiposity index, waist-to-height ratio, and metabolic disturbances in the obese. Kardiol. Pol. 2017, 75, 1185–1191. [Google Scholar] [CrossRef]
- Demura, S.; Sato, S. Nonlinear relationships between visceral fat area and percent regional fat mass in the trunk and the lower limbs in Japanese adults. Eur. J. Clin. Nutr. 2007, 62, 1395–1404. [Google Scholar] [CrossRef]
- Elffers, T.W.; De Mutsert, R.; Lamb, H.J.; De Roos, A.; Van Dijk, K.W.; Rosendaal, F.R.; Jukema, J.W.; Trompet, S. Body fat distribution, in particular visceral fat, is associated with cardiometabolic risk factors in obese women. PLoS ONE 2017, 12, e0185403. [Google Scholar] [CrossRef]
- Frank, A.P.; Santos, R.d.S.; Palmer, B.F.; Clegg, D.J. Determinants of body fat distribution in humans may provide insight about obesity-related health risks. J. Lipid Res. 2019, 60, 1710–1719. [Google Scholar] [CrossRef] [PubMed]
- Stults-Kolehmainen, M.A.; Stanforth, P.R.; Bartholomew, J.B.; Lu, T.; Abolt, C.J.; Sinha, R. DXA estimates of fat in abdominal, trunk and hip regions varies by ethnicity in men. Nutr. Diabetes 2013, 3, e64. [Google Scholar] [CrossRef] [PubMed]
| Anthropometric Measurement | Method | % TEM |
|---|---|---|
| wrist | The wrist girth is the minimum girth measurement perpendicular to the long axis of the forearm and distal to the ulnar styloid processes | 1.06 |
| upper arm | The maximum girth of the upper arm. The subject assumes a relaxed position with the arms hanging by the side of the body. The tape should be positioned perpendicular to the long axis of the humerus while the muscles of the arm are relaxed | 1.16 |
| neck | The circumference of the neck is measured immediately superior to the thyroid cartilage and perpendicular to the long axis of the neck | 1.45 |
| waist | The circumference of the waist at the level of umbilicus, perpendicular to the long axis of the trunk | 1.39 |
| hip | The circumference of the hip at the level of their greatest posterior protuberance, perpendicular to the long axis of the trunk | 1.34 |
| thigh | The girth of the thigh is taken 1 cm below the level of the gluteal fold, perpendicular to the long axis of the thigh | 1.27 |
| calf | The mid-calf circumference is defined as the maximum girth of the calf | 1.09 |
| BMI kg/m2 | Male (%) n = 40 | Female (%) n = 124 |
|---|---|---|
| <18.5 | 0 (0%) | 4 (3.2%) |
| 18.5–25 | 16 (40%) | 56 (45.2%) |
| 25–30 | 22 (55%) | 55 (44.4%) |
| >30 | 2 (5%) | 9 (7.2%) |
| Normal-Weight Lean | Normal-Weight Obese | Overweight and Obesity | F | p | |
|---|---|---|---|---|---|
| Allparticipants | n = 47 (28.7%) | n = 30 (18.3%) | n = 87 (53.0%) | ||
| Age (years) | 56.2 ± 8.8 | 54.9 ± 8.4 | 55.5 ± 8.5 | 0.242 | 0.785 |
| Height (cm) | 163.8 ± 5.4 | 162.9 ± 6.2 | 164.2 ± 8.3 | 0.376 | 0.687 |
| Weight (kg) | 57.3 ± 6.4 #* | 63.9 ± 4.3 #⬙ | 74.4 ± 9.3 *⬙ | 77.295 | <0.001 |
| Body mass index (kg/m2) | 21.3 ± 1.5 #* | 24.1 ± 0.7 #⬙ | 27.5 ± 1.9 *⬙ | 225.250 | <0.001 |
| Grip strength (kg) | 26.7 ± 6.9 | 23.4 ± 4.9 ⬙ | 27.7 ± 7.4 ⬙ | 4.370 | 0.014 |
| Body muscle mass (kg) | 39.9 ± 6.5 * | 40.3 ± 6.1 ⬙ | 44.8 ± 9.5 *⬙ | 7.042 | <0.001 |
| Body fat mass (kg) | 14.8 ± 3.6 #* | 20.9 ± 2.4 #⬙ | 26.9 ± 5.3 *⬙ | 117.011 | <0.001 |
| Body fat percentage (%) | 26.0 ± 6.0 #* | 33.0 ± 5.3 #⬙ | 36.7 ± 6.7 *⬙ | 44.966 | <0.001 |
| Body water mass (kg) | 29.6 ± 5.1 * | 30.5 ± 4.1 ⬙ | 34.9 ± 6.2 *⬙ | 16.240 | <0.001 |
| Body water percentage (%) | 51.4 ± 4.8 #* | 47.6 ± 3.8 # | 46.6 ± 3.7 * | 21.412 | <0.001 |
| Visceral fat index | 6.0 ± 2.0 #* | 7.7 ± 1.6 #⬙ | 10.5 ± 3.1 *⬙ | 49.244 | <0.001 |
| Mid-upper Arm (cm) | 25.0 ± 3.9 #* | 28.7 ± 6.2 #⬙ | 31.6 ± 3.6 *⬙ | 36.995 | <0.001 |
| Waist (cm) | 76.6 ± 7.9 #* | 87.1 ± 7.4 #⬙ | 94.9 ± 7.4 *⬙ | 90.937 | <0.001 |
| Hip (cm) | 94.1 ± 4.7 #* | 97.7 ± 3.3 #⬙ | 103.8 ± 5.2 *⬙ | 67.006 | <0.001 |
| Thigh (cm) | 49.1 ± 5.6 #* | 53.4 ± 2.5 #⬙ | 56.1 ± 5.6 *⬙ | 28.384 | <0.001 |
| Height/Mid-upper Arm | 6.77 ± 1.45 #* | 6.00 ± 1.72 #⬙ | 5.27 ± 0.69 *⬙ | 25.178 | <0.001 |
| Waist/Height | 0.47 ± 0.05 #* | 0.54 ± 0.05 #⬙ | 0.58 ± 0.04 *⬙ | 98.165 | <0.001 |
| Hip/Height | 0.57 ± 0.02 #* | 0.60 ± 0.02 #⬙ | 0.63 ± 0.04 *⬙ | 48.802 | <0.001 |
| (Waist + Hip)/Height | 1.04 ± 0.06 #* | 1.14 ± 0.07 #⬙ | 1.21 ± 0.07 *⬙ | 94.092 | <0.001 |
| Waist/Hip | 0.81 ± 0.07 #* | 0.89 ± 0.06 # | 0.91 ± 0.05 * | 42.401 | <0.001 |
| Thigh/Hip | 0.52 ± 0.05 #* | 0.55 ± 0.02 # | 0.54 ± 0.04 * | 4.578 | 0.012 |
| Thigh/Height | 0.30 ± 0.03 #* | 0.33 ± 0.02 # | 0.34 ± 0.04 * | 26.596 | <0.001 |
| Calf/Waist | 0.45 ± 0.05 #* | 0.40 ± 0.03 # | 0.40 ± 0.03 * | 37.554 | <0.001 |
| Wrist (cm) | 15.3 ± 0.9 * | 15.4 ± 1.5 ⬙ | 16.8 ± 1.5 *⬙ | 21.731 | <0.001 |
| Neck (cm) | 33.6 ± 2.9 * | 34.8 ± 5.3 ⬙ | 36.9 ± 3.8 *⬙ | 11.449 | <0.001 |
| Calf (cm) | 34.2 ± 2.7 * | 35.1 ± 2.4 ⬙ | 37.7 ± 3.0 *⬙ | 26.336 | <0.001 |
| Male group | n = 10 (25%) | n = 6 (15%) | n = 24 (60%) | ||
| Age (years) | 55.7 ± 10.1 # | 44.2 ± 2.6 # | 50.0 ± 8.5 | 3.635 | 0.036 |
| Height (cm) | 169.0 ± 4.7 * | 173.8 ± 1.6 | 175.0 ± 5.3 * | 5.573 | 0.008 |
| Weight (kg) | 63.8 ± 6.3 #* | 71.7 ± 3.4 #⬙ | 84.9 ± 4.5 *⬙ | 71.299 | <0.001 |
| Body mass index (kg/m2) | 22.3 ± 1.0 #* | 23.7 ± 0.7 #⬙ | 27.7 ± 1.0 *⬙ | 132.274 | <0.001 |
| Grip strength (kg) | 37.7 ± 3.4 # | 29.4 ± 4.1 #⬙ | 37.2 ± 4.9 ⬙ | 8.153 | 0.001 |
| Body muscle mass (kg) | 50.7 ± 4.6 * | 51.9 ± 2.3 ⬙ | 58.7 ± 5.5 *⬙ | 11.240 | <0.001 |
| Body fat mass (kg) | 10.0 ± 1.9 #* | 16.4 ± 1.3 #⬙ | 23.9 ± 5.6 *⬙ | 34.997 | <0.001 |
| Body fat percentage (%) | 15.6 ± 1.8 #* | 22.9 ± 0.8 #⬙ | 28.9 ± 7.4 *⬙ | 18.311 | <0.001 |
| Body water mass (kg) | 37.9 ± 4.1 * | 38.3 ± 1.0 ⬙ | 43.3 ± 3.3 *⬙ | 12.320 | <0.001 |
| Body water percentage (%) | 59.4 ± 2.9 #* | 53.6 ± 4.0 # | 50.8 ± 3.9 * | 23.346 | <0.001 |
| Visceral fat index | 9.0 ± 0.8 * | 9.4 ± 3.1 ⬙ | 14.8 ± 2.0 *⬙ | 38.066 | <0.001 |
| Wrist (cm) | 16.0 ± 0.8 * | 16.9 ± 1.4 ⬙ | 18.1 ± 0.9 *⬙ | 17.799 | <0.001 |
| Mid-upper Arm (cm) | 27.8 ± 1.7 # | 34.6 ± 5.8 #⬙ | 30.0 ± 2.3 ⬙ | 10.345 | <0.001 |
| Neck (cm) | 37.1 ± 2.2# | 42.4 ± 6.3 # | 40.2 ± 2.8 | 5.232 | 0.010 |
| Waist (cm) | 93.1 ± 2.6 #* | 100.3 ± 3.7 #⬙ | 105.6 ± 2.7 *⬙ | 82.974 | <0.001 |
| Hip (cm) | 79.0 ± 6.0 #* | 86.3 ± 10.1 #⬙ | 102.0 ± 2.0 *⬙ | 67.397 | <0.001 |
| Thigh (cm) | 45.6 ± 6.6 #* | 55.9 ± 6.6 # | 56.1 ± 6.7 * | 10.629 | <0.001 |
| Calf (cm) | 36.2 ± 2.2 * | 37.1 ± 1.5 ⬙ | 40.1 ± 2.1 *⬙ | 15.312 | <0.001 |
| (Waist + Hip)/Height | 1.02 ± 0.02 #* | 1.07 ± 0.07 #⬙ | 1.19 ± 0.04 *⬙ | 69.640 | <0.001 |
| Hip/Height | 0.55 ± 0.02 #* | 0.58 ± 0.02 #⬙ | 0.60 ± 0.02 *⬙ | 29.452 | <0.001 |
| Thigh/Height | 0.27 ± 0.04 #* | 0.32 ± 0.01 # | 0.33 ± 0.04 * | 8.485 | 0.001 |
| Waist/Hip | 0.85 ± 0.07 * | 0.86 ± 0.07 ⬙ | 0.97 ± 0.02 *⬙ | 32.324 | <0.001 |
| Waist/Height | 0.47 ± 0.03 * | 0.50 ± 0.05 ⬙ | 0.58 ± 0.02 *⬙ | 72.095 | <0.001 |
| Female group | n = 37 (29.8%) | n = 24 (19.4%) | n = 63 (50.8%) | ||
| Age (years) | 56.4 ± 8.6 | 57.5 ± 7.2 | 57.6 ± 7.5 | 0.328 | 0.721 |
| Height (cm) | 162.4 ± 4.8 * | 160.2 ± 3.0 | 160.1 ± 4.7 * | 3.446 | 0.035 |
| Weight (kg) | 55.6 ± 5.3 #* | 61.9 ± 1.2 #⬙ | 70.4 ± 7.2 *⬙ | 74.604 | <0.001 |
| Body mass index (kg/m2) | 21.1 ± 1.5 #* | 24.2 ± 0.7 #⬙ | 27.5 ± 2.2 *⬙ | 151.568 | <0.001 |
| Grip strength (kg) | 23.7 ± 3.8 | 21.9 ± 3.9 | 24.1 ± 4.2 | 2.489 | 0.087 |
| Body muscle mass (kg) | 36.9 ± 2.6 * | 37.4 ± 1.3 ⬙ | 39.5 ± 3.2 *⬙ | 12.038 | <0.001 |
| Body fat mass (kg) | 16.1 ± 2.8 #* | 22.0 ± 0.8 #⬙ | 28.1 ± 4.7 *⬙ | 124.723 | <0.001 |
| Body fat percentage (%) | 28.7 ± 2.7 #* | 35.5 ± 1.5 #⬙ | 39.7 ± 3.1 *⬙ | 187.913 | <0.001 |
| Body water mass (kg) | 27.4 ± 2.2 * | 28.6 ± 1.2 ⬙ | 31.6 ± 3.2 *⬙ | 34.037 | <0.001 |
| Body water percentage (%) | 49.2 ± 2.2 #* | 46.1 ± 1.7 # | 45.0 ± 2.9 * | 42.940 | <0.001 |
| Visceral fat index | 5.1 ± 0.9 #* | 7.3 ± 0.8 #⬙ | 7.4 ± 1.9 *⬙ | 150.835 | <0.001 |
| Mid-upper Arm (cm) | 24.2 ± 4.0 #* | 27.3 ± 5.5 #⬙ | 32.2 ± 3.8 *⬙ | 43.650 | <0.001 |
| Waist (cm) | 76.0 ± 8.3 #* | 87.4 ± 6.8 #⬙ | 92.2 ± 6.8 *⬙ | 58.250 | <0.001 |
| Wrist (cm) | 15.1 ± 0.8 * | 15.1 ± 1.4 ⬙ | 16.3 ± 1.4 *⬙ | 13.779 | <0.001 |
| Neck (cm) | 32.7 ± 2.3 * | 32.9 ± 2.9 ⬙ | 35.7 ± 3.4 *⬙ | 14.195 | <0.001 |
| Hip (cm) | 94.4 ± 5.1 * | 97.1 ± 2.8 ⬙ | 103.1 ± 5.7 *⬙ | 36.617 | <0.001 |
| Thigh (cm) | 50.0 ± 5.0 * | 52.8 ± 2.4 ⬙ | 56.1 ± 5.1 *⬙ | 20.253 | <0.001 |
| Calf (cm) | 33.6 ± 2.6 * | 34.6 ± 2.4 ⬙ | 36.7 ± 2.7 *⬙ | 17.490 | <0.001 |
| (Waist + Hip)/Height | 1.05 ± 0.06 #* | 1.15 ± 0.06 #⬙ | 1.22 ± 0.08 *⬙ | 65.686 | <0.001 |
| Waist/Height | 0.47 ± 0.05 #* | 0.55 ± 0.05 #⬙ | 0.58 ± 0.05 *⬙ | 63.144 | <0.001 |
| Hip/Height | 0.58 ± 0.02 #* | 0.61 ± 0.02 #⬙ | 0.65 ± 0.04 *⬙ | 46.909 | <0.001 |
| Thigh/Height | 0.31 ± 0.03 #* | 0.33 ± 0.02 #⬙ | 0.35 ± 0.03 *⬙ | 26.803 | <0.001 |
| Waist/Hip | 0.80 ± 0.07 #* | 0.89 ± 0.06 # | 0.90 ± 0.05 * | 32.474 | <0.001 |
| Waist/Height | BMI | Thigh/Height | Hip/Height | (Waist + Hip)/Height | |
|---|---|---|---|---|---|
| All participants | |||||
| r | 0.556 | 0.619 | 0.639 | 0.646 | 0.668 |
| Male group | |||||
| BMI | Waist/Height | (Waist + Hip)/Height | Waist/Hip | ||
| r | 0.684 | 0.617 | 0.594 | 0.593 | |
| Female group | |||||
| (Waist + Hip)/Height | Waist/Height | Thigh/Height | Hip/Height | Waist/Hip | |
| r | 0.806 | 0.781 | 0.753 | 0.739 | 0.613 |
| OR | 95% CI | p | |
|---|---|---|---|
| All participants | |||
| BMI | 3.130 | 3.954–27.616 | 0.001 |
| (Waist + hip)/height | 5.205 | 3.004–9.018 | 0.013 |
| Thigh/height | 8.121 | 2.413–2.733 | 0.008 |
| Male group | |||
| Waist/height | 1.208 | 1.037–1.407 | 0.001 |
| (Waist + hip)/height | 4.174 | 1.826–2.991 | 0.001 |
| Waist/hip | 4.894 | 1.409–1.699 | 0.002 |
| Female group | |||
| (Waist + hip)/height | 8.059 | 2.407–2.698 | 0.001 |
| Waist/hip | 5.439 | 5.317–5.564 | 0.001 |
| Hip/height | 3.665 | 2.737–4.909 | 0.001 |
| Waist/height | 1.731 | 1.460–2.052 | 0.001 |
| Thigh/height | 1.216 | 2.503–5.907 | 0.001 |
| BMI | 2.543 | 3.824–6.910 | 0.001 |
| AUC | Sensitivity (%) | Specificity (%) | Youden Index | Cutoff | p | 95% CI | |
|---|---|---|---|---|---|---|---|
| All participants | |||||||
| BMI | 0.992 | 95.7 | 97.9 | 0.936 | 23.369 | <0.001 | 0.984–0.999 |
| (Waist + hip)/height | 0.964 | 94.9 | 93.6 | 0.885 | 1.115 | <0.001 | 0.936–0.992 |
| Waist/height | 0.944 | 94.0 | 91.5 | 0.855 | 0.512 | <0.001 | 0.908–0.980 |
| Waist | 0.938 | 73.5 | 97.9 | 0.714 | 88.25 | <0.001 | 0.904–0.973 |
| Waist/hip | 0.837 | 78.6 | 83.0 | 0.616 | 0.869 | <0.001 | 0.763–0.912 |
| Hip/height | 0.888 | 94.9 | 63.8 | 0.587 | 0.582 | <0.001 | 0.838–0.939 |
| Hip | 0.869 | 68.4 | 89.4 | 0.578 | 99.25 | <0.001 | 0.816–0.923 |
| Thigh/height | 0.812 | 71.8 | 78.1 | 0.499 | 0.323 | 0.035 | 0.744–0.880 |
| Male group | |||||||
| (Waist + hip)/height | 0.937 | 93.3 | 90 | 0.833 | 1.048 | 0.001 | 0.851–0.999 |
| Waist/hip | 0.880 | 80 | 90 | 0.700 | 0.932 | 0.001 | 0.773–0.987 |
| Hip/height | 0.957 | 86.7 | 90 | 0.767 | 0.576 | 0.001 | 0.900–0.998 |
| Waist/height | 0.933 | 93.3 | 90 | 0.833 | 0.496 | 0.001 | 0.844–0.997 |
| Thigh/height | 0.835 | 90 | 80 | 0.700 | 0.276 | 0.002 | 0.665–0.998 |
| Female group | |||||||
| (Waist + hip)/height | 0.971 | 96.6 | 91.9 | 0.885 | 1.115 | 0.001 | 0.944–0.998 |
| Waist/hip | 0.845 | 73.6 | 89.2 | 0.628 | 0.869 | 0.001 | 0.755–0.934 |
| Hip/height | 0.914 | 77 | 89.2 | 0.662 | 0.604 | 0.001 | 0.866–0.962 |
| Waist/height | 0.942 | 94.3 | 89.2 | 0.835 | 0.512 | 0.001 | 0.899–0.985 |
| Thigh/height | 0.836 | 71.3 | 86.5 | 0.578 | 0.329 | 0.001 | 0.762–0.980 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhu, Y.; Wang, Z.; Maruyama, H.; Onoda, K.; Huang, Q. Body Fat Percentage and Normal-Weight Obesity in the Chinese Population: Development of a Simple Evaluation Indicator Using Anthropometric Measurements. Int. J. Environ. Res. Public Health 2022, 19, 4238. https://doi.org/10.3390/ijerph19074238
Zhu Y, Wang Z, Maruyama H, Onoda K, Huang Q. Body Fat Percentage and Normal-Weight Obesity in the Chinese Population: Development of a Simple Evaluation Indicator Using Anthropometric Measurements. International Journal of Environmental Research and Public Health. 2022; 19(7):4238. https://doi.org/10.3390/ijerph19074238
Chicago/Turabian StyleZhu, Yuetong, Zimin Wang, Hitoshi Maruyama, Ko Onoda, and Qiuchen Huang. 2022. "Body Fat Percentage and Normal-Weight Obesity in the Chinese Population: Development of a Simple Evaluation Indicator Using Anthropometric Measurements" International Journal of Environmental Research and Public Health 19, no. 7: 4238. https://doi.org/10.3390/ijerph19074238
APA StyleZhu, Y., Wang, Z., Maruyama, H., Onoda, K., & Huang, Q. (2022). Body Fat Percentage and Normal-Weight Obesity in the Chinese Population: Development of a Simple Evaluation Indicator Using Anthropometric Measurements. International Journal of Environmental Research and Public Health, 19(7), 4238. https://doi.org/10.3390/ijerph19074238






