Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire–Based Study
Abstract
:1. Introduction
- -
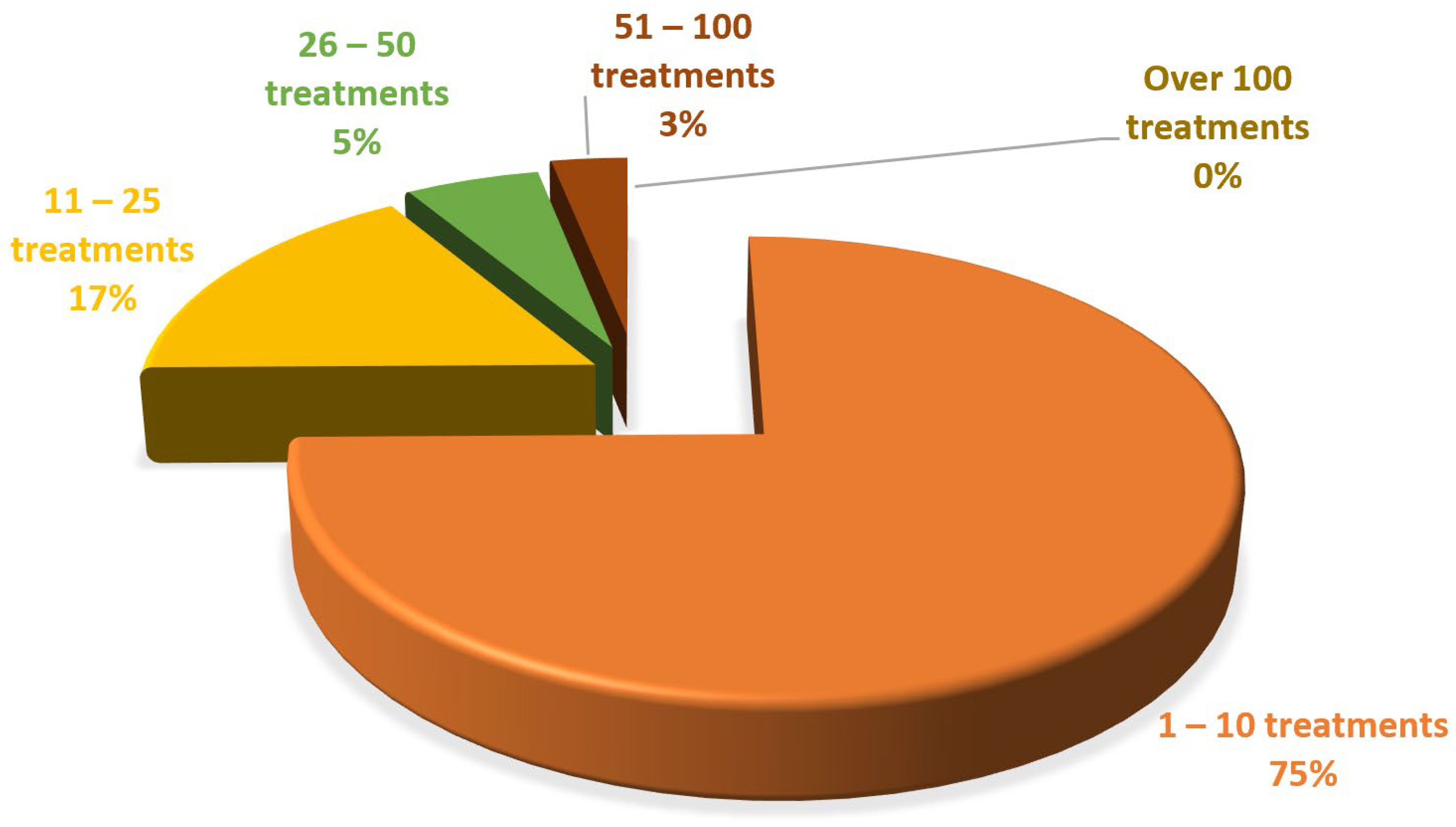
- Different whitening methods, recommended mainly by dentists and chosen by patients.
- -
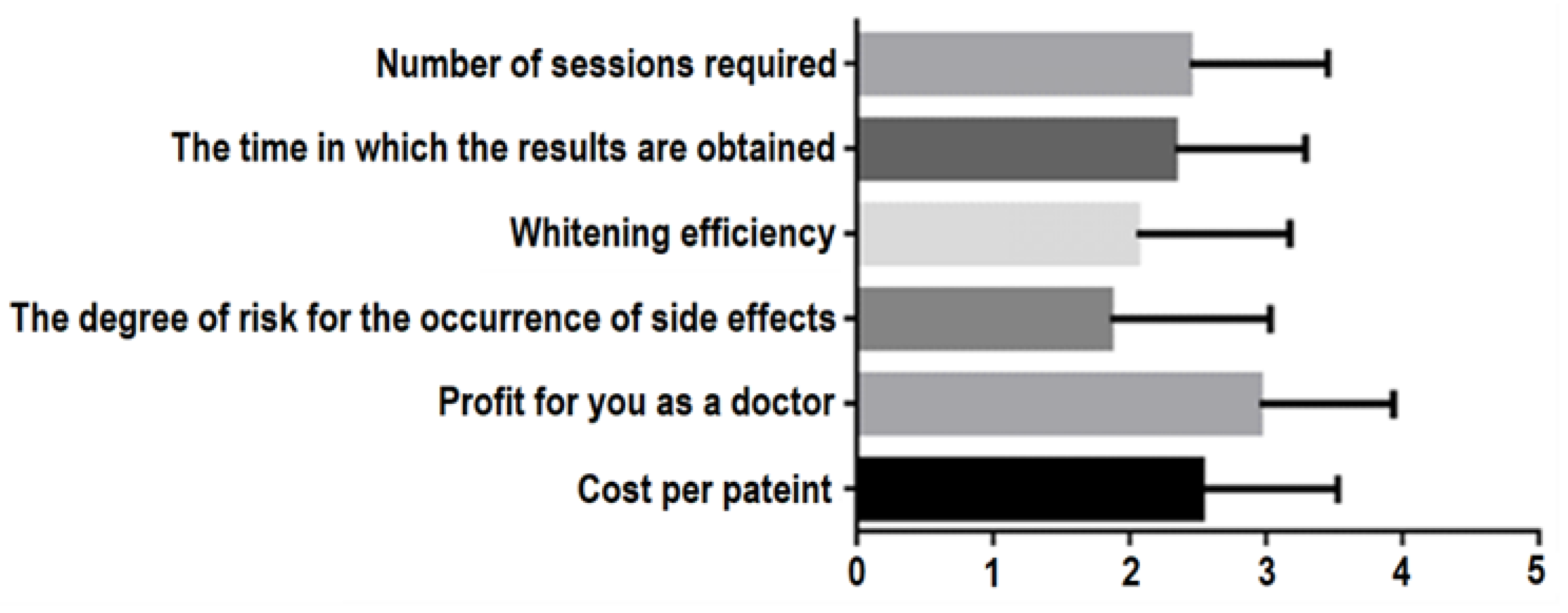
- Factors involved in recommending and using tooth-bleaching methods and bleaching materials.
- -
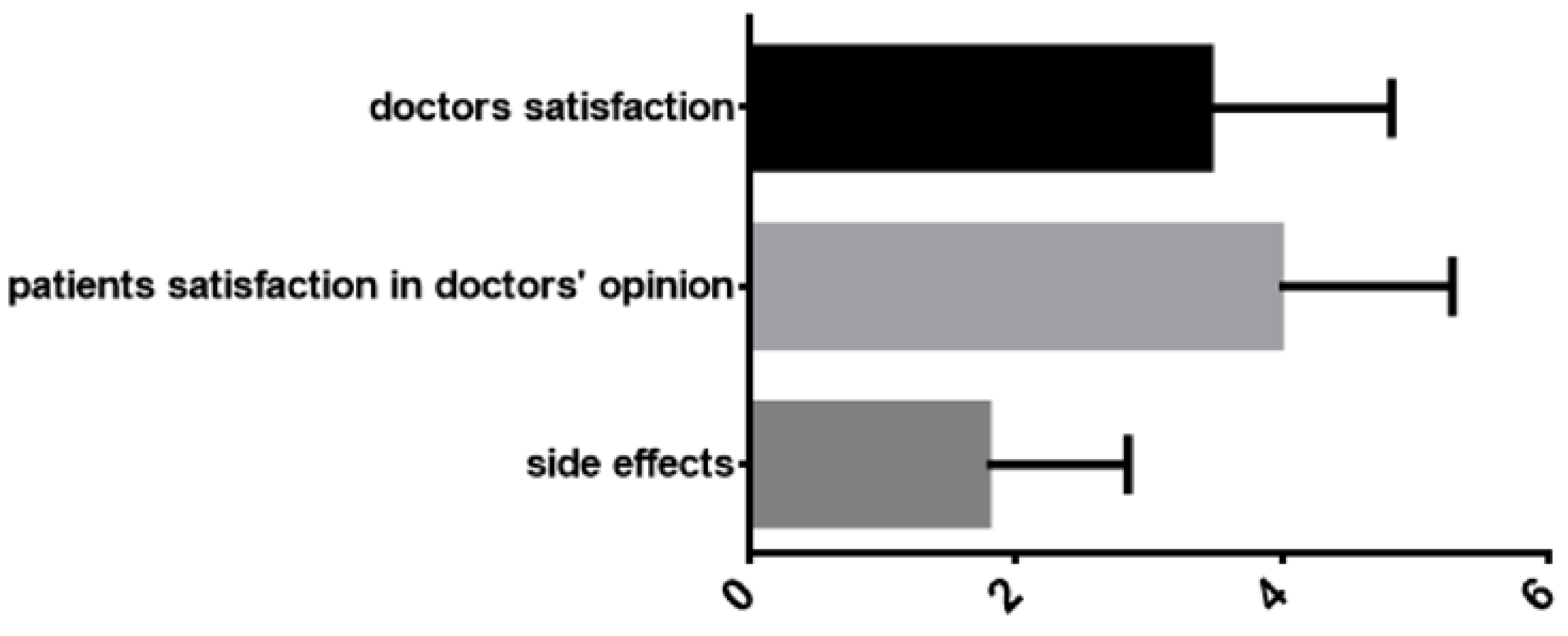
- Satisfaction with the bleaching methods and materials used.
- -
- Patients’ self-perception of the aesthetic appearance of their dental arches, especially regarding tooth color.
2. Materials and Methods
2.1. Study Design
2.2. Statistical Analysis
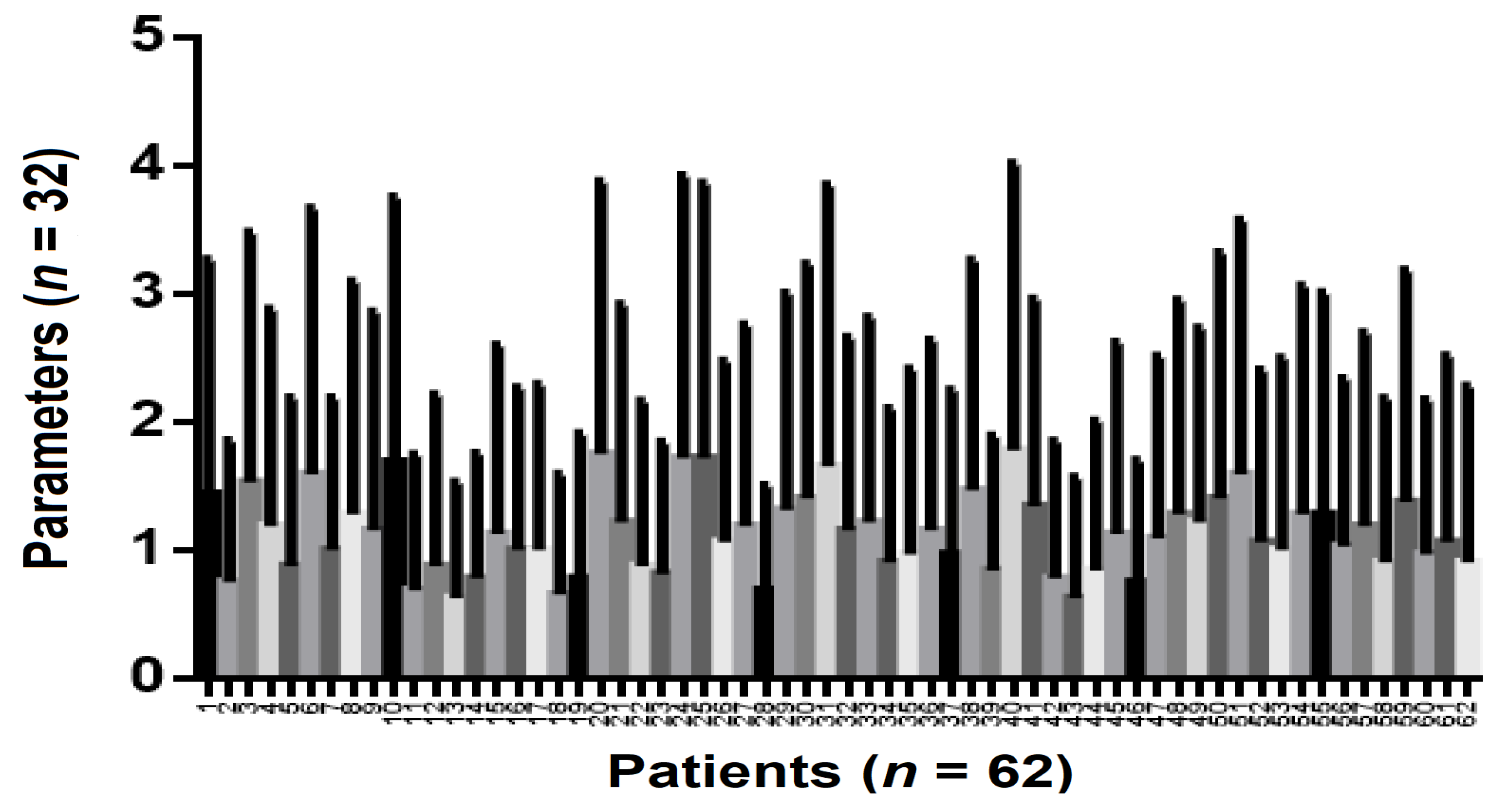
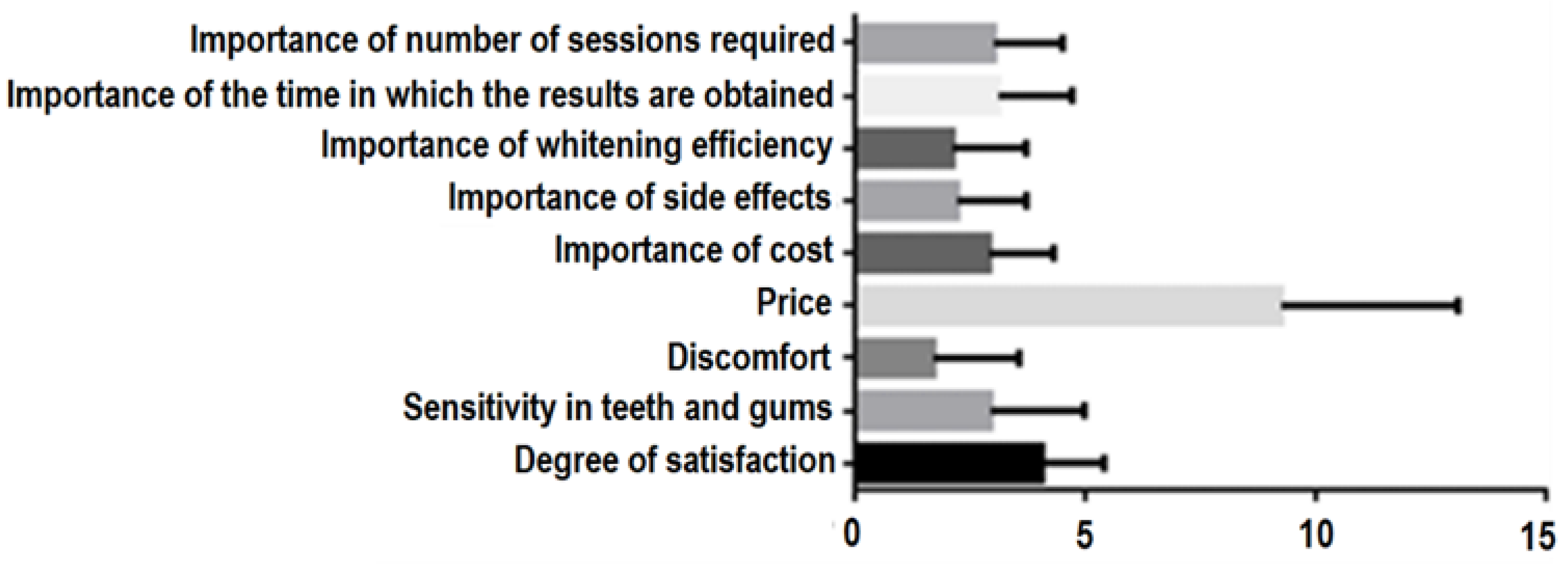
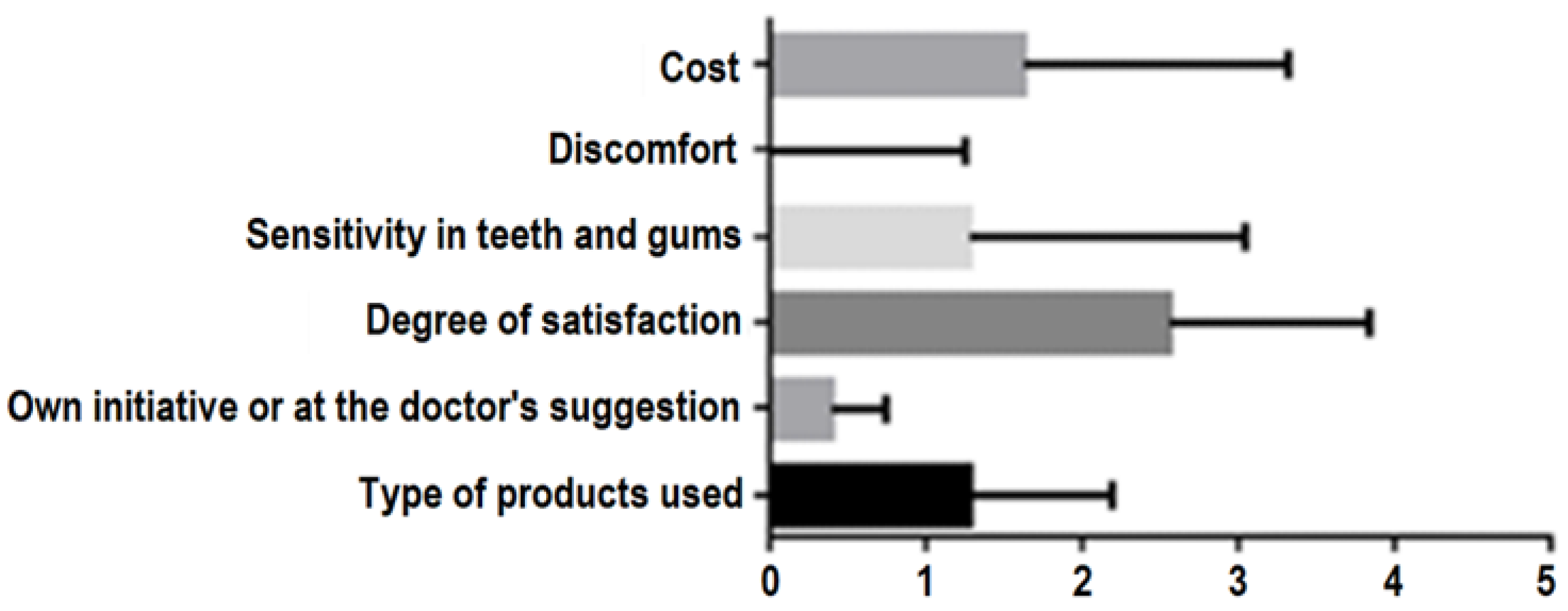
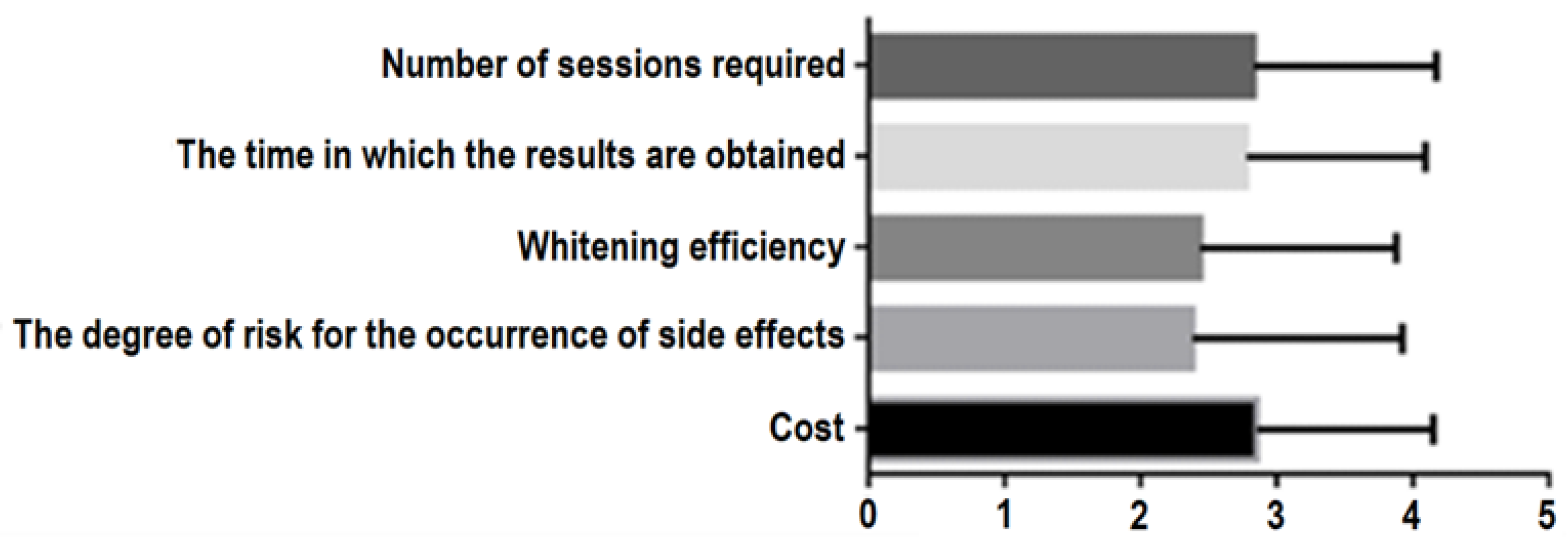
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Martin, J.; Rivas, V.; Vildósola, P.; Moncada, L.; Oliveira Junior, O.B.; Saad, J.R.; Fernandez, E.; Moncada, G. Personality style in patients looking for tooth bleaching and its correlation with treatment satisfaction. Braz. Dent. J. 2016, 27, 60–65. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Chiche, G.; Bahat, O.; Roblee, R.; Coachman, C.; Heymann, H.O. Evolution of Aesthetic Dentistry. J. Dent. Res. 2019, 98, 1294–1304. [Google Scholar] [CrossRef] [PubMed]
- Afrashtehfar, K.I.; Assery, M.K.A.; Bryant, S.R. Aesthetic parameters and patient-perspective assessment tools for maxillary anterior single implants. Int. J. Dent. 2021, 17, 6684028. [Google Scholar] [CrossRef] [PubMed]
- Reddy, S.V.; Madineni, P.K.; Sudheer, A.; Gujjarlapudi, M.C.; Sreedevi, B.; Reddy, P.S. Comparative analysis of rationale used by dentists and patient for final esthetic outcome of dental treatment. J. Contemp. Dent. Pract. 2013, 14, 532–535. [Google Scholar]
- Samorodnitzky-Naveh, G.R.; Grossman, Y.; Bachner, Y.G.; Levin, L. Patients’ self-perception of tooth shade in relation to professionally objective evaluation. Quintessence Int. 2010, 41, 80–83. [Google Scholar]
- Manipal, S.; Anand Mohan, C.S.; Kumar, D.L.; Cholan, P.K.; Ahmed, A.; Adusumilli, P. The importance of dental aesthetics among dental student’s assessment of knowledge. J. Int. Soc. Prevent. Communit. Dent. 2014, 4, 48–51. [Google Scholar] [CrossRef] [Green Version]
- Alhammadi, M.S.; Halboub, E.; Al-Mashraqi, A.A.; Al-Homoud, M.; Wafi, S.; Zakari, A. Perception of facial, dental, and smile esthetics by dental students. J. Esthet. Restor. Dent. 2018, 30, 415–426. [Google Scholar] [CrossRef]
- Kopycka-Kedzierawski, D.T.; Meyerowitz1, C.; Litaker, M.S.; Chonowski, S.; Heft, W.M.; Gordan, V.V.; Yardic, R.L.; Madden, T.E.; Reyes, S.C.; Gilbert, G.H. National Dental PBRN Collaborative Group. Management of dentin hypersensitivity by National Dental Practice-Based Research Network practitioners: Results from a questionnaire administered prior to initiation of a clinical study on this topic. BMC Oral Health 2017, 17, 41. [Google Scholar] [CrossRef] [Green Version]
- Afrashtehfar, K.I.; Bryant, S.R. Understanding the lived experience of North American dental patients with a single-tooth implant in the upper front region of the mouth: Protocol for a qualitative study. JMIR Res. Protoc. 2021, 10, e25767. [Google Scholar] [CrossRef]
- Khan, M.; Kazmi, S.M.R.; Khan, F.R.; Samejo, I. Analysis of different characteristics of smile. BDJ Open 2020, 6, 1–5. [Google Scholar] [CrossRef]
- Ingber, F.K. You are never fully dressed without a smile. J. Esthet. Restor. Dent. 2006, 18, 59–60. [Google Scholar] [PubMed]
- Watts, A.; Addy, M. Tooth discolouration and staining: A review of the literature. Br. Dent. J. 2001, 190, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Newton, J.T.; Subramanian, S.S.; Westland, S.; Gupta, A.K.; Luo, W.; Joiner, A. The impact of tooth colour on the perceptions of age and social judgements. J. Dent. 2021, 112, 103771. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, E.; Bersezio, C.; Bottner, J.; Avalos, F.; Godoy, I.; Inda, D.; Vildósola, P.; Saad, J.; Oliveira, O.B., Jr.; Martín, J. Longevity, esthetic perception, and psychosocial impact of teeth bleaching by low (6%) hydrogen peroxide concentration for in-office treatment: A randomized clinical trial. Oper. Dent. 2017, 42, 41–52. [Google Scholar] [CrossRef]
- Joiner, A. The bleaching of teeth: A review of the literature. J. Dent. 2006, 34, 412–419. [Google Scholar] [CrossRef]
- Martínez, R.J.; Valiente, M.; Sánchez-Martín, M.J. Tooth whitening: From the established treatments to novelapproaches to prevent side effects. J. Esthet. Restor. Dent. 2019, 31, 431–440. [Google Scholar] [CrossRef]
- Eimar, H.; Siciliano, R.; Abdallah, M.N.; Nader, S.A.; Amin, W.M.; Martinez, P.P.; Celemin, A.; Cerruti, M.; Tamimi, F. Hydrogen peroxide whitens teeth by oxidizing the organic structure. J. Dent. 2012, 40, 25–33. [Google Scholar] [CrossRef]
- Available online: https://forms.office.com/Pages/ResponsePage.aspx?id=Ja-p_IQ7bEyXNp1c3OIQxV20hjJ7YLZGijIfpVQUNYpUODdJNDkzWVhQRUY4SzhHUDZJMENMOElHWi4u; https://forms.office.com/Pages/ResponsePage.aspx?id=Ja-p_IQ7bEyXNp1c3OIQxV20hjJ7YLZGijIfpVQUNYpUNVM0UUhaWFpMNVI2VFpNSEdMS0RLUldVMS4u (accessed on 1 March 2022).
- Alshiddi, I.F.; BinSaleh, S.M.; Alhawas, Y. Patient’s perception on the esthetic outcome of anterior fixed prosthetic treatment. J. Contemp. Dent. Pract. 2015, 16, 845–849. [Google Scholar]
- Cotrim, E.R.; Vasconcelos, A.V., Jr.; Haddad, A.C.; Reis, S.A. Perception of adults’ smile esthetics among orthodontists, clinicians and laypeople. Dental Press J. Orthod. 2015, 20, 40–47. [Google Scholar] [CrossRef] [Green Version]
- AlOtaibi, G.; AlMutairi, M.S.; AlShammari, M.Z.; AlJafar, M.; AlMaraikhi, T.F. Prevalence and public knowledge regarding tooth bleaching in Saudi Arabia. J. Fam. Med. Prim. Care 2020, 9, 3729. [Google Scholar] [CrossRef]
- Aldakheel, R. Patients desire and previous experience of dental bleaching. EC Dent. Sci. 2018, 17, 1633–1644. [Google Scholar]
- Ahmed, Y.T.; Al-Fkeih, A.F.; Alrejaie, L.M.; Al Barazi, J.G.; Alhaffar, D.R.; AlQarni, G.S.; Alhajibrahim, D.A. Evaluation and knowledge in choice of at home dental bleaching versus in-office bleaching in Riyadh, Saudi Arabia. J. Adv. Med. Dent. Sci. Res. 2020, 8, 23–26. [Google Scholar]
- Voina, C.; Delean, A.; Muresan, A.; Valeanu, M.; Moldovan, A.M.; Popescu, V.; Petean, I.; Ene, R.; Moldovan, M.; Pandrea, S. Antimicrobial Activity and the Effect of Green Tea Experimental Gels on Teeth Surfaces. Coatings 2020, 10, 537. [Google Scholar] [CrossRef]
- Tonea, A.; Oana, L.; Badea, M.; Sava, S.; Voina, C.; Ranga, F.; Vodnar, D. HPLC analysis, antimicrobial and antifungal activity of an experimental plant based gel, for endodontic usage. Studia Univ. Babes-Bolyai Chem. 2016, 61, 53. [Google Scholar]
- Silva, B.G.; Gouveia, T.H.; da Silva, M.D.; Ambrosano, G.M.; Aguiar, F.H.; Lima, D.A. Evaluation of home bleaching gel modified by different thickeners on the physical properties of enamel: An in situ study. Eur. J. Dent. 2018, 12, 523–527. [Google Scholar] [CrossRef] [Green Version]
- Pimentel de Oliveira, R.; Baia, J.C.P.; Ribeiro, M.E.S.; Junior, M.H.D.S.E.S.; Loretto, S.C. Influence of time intervals between bleaching procedures on enamel microhardness and surface roughness. Open Dent. J. 2018, 12, 555. [Google Scholar] [CrossRef]
- Joiner, A.; Luo, W. Tooth colour and whiteness: A review. J. Dent. 2017, 67, 3–10. [Google Scholar] [CrossRef]
- de Abreu, D.R.; Sasaki, R.T.; Amaral, F.L.; Florio, F.M.; Basting, R.T. Effect of home-use and in-office bleaching agents containing hydrogen peroxide associated with amorphous calcium phosphate on enamel microhardness and surface roughness. J. Esthet. Restor. Dent. 2011, 23, 158–168. [Google Scholar] [CrossRef]
- Tam, L. The safety of home bleaching techniques. J. Can. Dent. Assoc. 1999, 65, 453–455. [Google Scholar]
- González-López, S.; Torres-Rodríguez, C.; Bolanos-Carmona, V.; Sanchez-Sanchez, P.; Rodríguez-Navarro, A.; Alvarez-Lloret, P.; Garcia, M.D. Effect of 30% hydrogen peroxide on mineral chemical composition and surface morphology of bovine enamel. Odontology 2016, 104, 44. [Google Scholar] [CrossRef]
- Zhang, H.; Shao, S.; Du, A.; Wang, Y.; Cheng, B.; Zhang, Z. Comparative evaluation of two antioxidants on reversing the immediate bond strength of bleached enamel: In vitro study. Med. Sci. Monit. 2020, 26, e9204481. [Google Scholar] [CrossRef] [PubMed]
- Colón, V.E.; Márquez, M.O.; Carrillo-Cotto, R.A.; Demarco, F.F.; Chisini, L.A. Dentists preferences on vital and nonvital tooth bleaching: Findings from a Guatemalan survey. Braz. J. Oral Sci. 2021, 20. [Google Scholar] [CrossRef]
- Bersezio, C.; Martín, J.; Herrera, A.; Loguercio, A.; Fernández, E. The effects of at-home whitening on patients’ oral health, psychology, and aesthetic perception. BMC Oral Health 2018, 18, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Zucoloto, M.L.; Maroco, J.; Campos, J.A.D.B. Impact of oral health on health-related quality of life: A cross-sectional study. BMC Oral Health 2016, 16, 16–55. [Google Scholar] [CrossRef] [PubMed]
- Albarqawy, K.; Alotaibi, T.; Meska, R.; Altuwairqy, L.; Aldraian, R.; Tarek, Y. The impact of social media on Laypersons’ Perception’s and use of teeth whitening home remedies. EC Dent. Sci. 2020, 19, 127–131. [Google Scholar]
- Greenwall-Cohen, J.; Francois, P.; Silikas, N.; Greenwall, L.; Le Goff, S.; Attal, J.P. The safety and efficacy of’over the counter’bleaching products in the UK. Br. Dent. J. 2019, 226, 271–276. [Google Scholar] [CrossRef]
- Afrashtehfar, K.I.; Assery, M.K. Five considerations in cosmetic and esthetic dentistry. J. N. J. Dent. Assoc. 2014, 85(4), 14–15. [Google Scholar]
- Siddiqui, A.A.; Anwar, N.; AlIbrahim, I.K.; Alhumaid, M.E.; Mian, R.I. Measurements of various traditional methods of teeth whitening among people of hail, Kingdom of Saudi Arabia. World J. Dent. 2018, 9, 1–4. [Google Scholar] [CrossRef]
- Del Monte, S.; Afrashtehfar, K.I.; Emami, E.; Nader, S.A.; Tamimi, F. Lay preferences for dentogingival esthetic parameters: A systematic review. J. Prosthet. Dent. 2017, 118, 717–724. [Google Scholar] [CrossRef]
- Archana, S.; Abraham, J. Comparative analysis of antimicrobial activity of leaf extracts from fresh green tea, commercial green tea and black tea on pathogens. J. Appl. Pharm. Sci. 2011, 8, 149. [Google Scholar]
- Hirasawa, M.; Takada, K. Multiple effects of green tea catechin on the antifungal activity of antimycotics against Candida albicans. J. Antimicrob. Chemother. 2004, 53, 225–229. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voina, C.; Muresan, A.; Delean, A.; Moldovan, A.I.; Popescu, V.; Prodan, D.; Petean, I.; Voina-Tonea, A.N.; Valeanu, M. The Effects of an Experimental Green Tea Extract Gel on the Surface Roughness of Bleached Teeth with Carbamide Peroxide Gels. Rev. Chim. 2020, 71, 312–320. [Google Scholar] [CrossRef]
- Jose, P.; Sanjeev, K.; Sekar, M. Effect of green and white tea pretreatment on remineralization of demineralized dentin by CPP-ACFP-an invitro microhardness analysis. J. Clin. Diagn. Res. 2016, 10, ZC85. [Google Scholar] [PubMed]
- Yu, H.; Oho, T.; Xu, L.X. Effects of several tea components on acid resistance of human tooth enamel. J. Dent. 1995, 23, 103–105. [Google Scholar] [CrossRef]



| Practitioners | Patients | |
|---|---|---|
| Origin: | O (%) | O (%) |
| Romanian | 32 | 18 |
| English | 95 | 16 |
| French | 0 | 86 |
| Age: | Years (SD) | Years (SD) |
| Mean | 29 (8.6) | 25 (8.4) |
| Median | 31 | 29 |
| Range | 18–55 | 18–55 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mazilu Moldovan, A.; Popescu, V.; Ionescu, C.V.; Cuc, S.; Craciun, A.; Moldovan, M.; Dudea, D.; Mesaros, A.S. Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire–Based Study. Int. J. Environ. Res. Public Health 2022, 19, 3977. https://doi.org/10.3390/ijerph19073977
Mazilu Moldovan A, Popescu V, Ionescu CV, Cuc S, Craciun A, Moldovan M, Dudea D, Mesaros AS. Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire–Based Study. International Journal of Environmental Research and Public Health. 2022; 19(7):3977. https://doi.org/10.3390/ijerph19073977
Chicago/Turabian StyleMazilu Moldovan, Amalia, Violeta Popescu, Corina Violeta Ionescu, Stanca Cuc, Antarinia Craciun, Marioara Moldovan, Diana Dudea, and Anca Stefania Mesaros. 2022. "Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire–Based Study" International Journal of Environmental Research and Public Health 19, no. 7: 3977. https://doi.org/10.3390/ijerph19073977
APA StyleMazilu Moldovan, A., Popescu, V., Ionescu, C. V., Cuc, S., Craciun, A., Moldovan, M., Dudea, D., & Mesaros, A. S. (2022). Various Aspects Involved in the Study of Tooth Bleaching Procedure: A Questionnaire–Based Study. International Journal of Environmental Research and Public Health, 19(7), 3977. https://doi.org/10.3390/ijerph19073977







