Three Growth Spurts in Global Physical Activity Policies between 2000 and 2019: A Policy Document Analysis
Abstract
1. Introduction
- I.
- Explore the PA policy development trajectory and evolution across these two decades.
- II.
- Conduct a policy content analysis [20] to elucidate the current landscape of global policies for promotion of increased PA.
- III.
- Explore the extent to which policies targeted children and adolescents, given the importance of promoting PA as early as possible in the life course [21], as well as whether and how gender was addressed, given the gendered nature of PA opportunities and participation [22,23], especially in LMIC contexts.
2. Materials and Methods
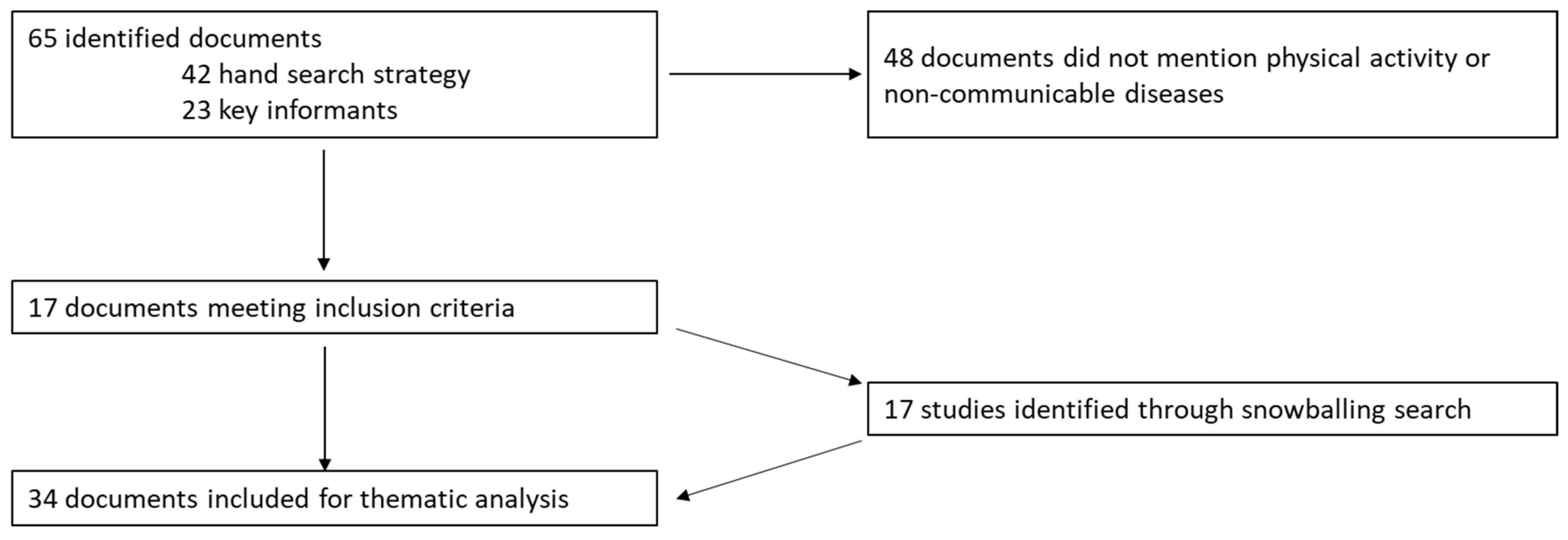
2.1. Document Search
2.2. Document Screening
2.3. Data Analysis
2.4. Policy Analysis Framework
3. Results
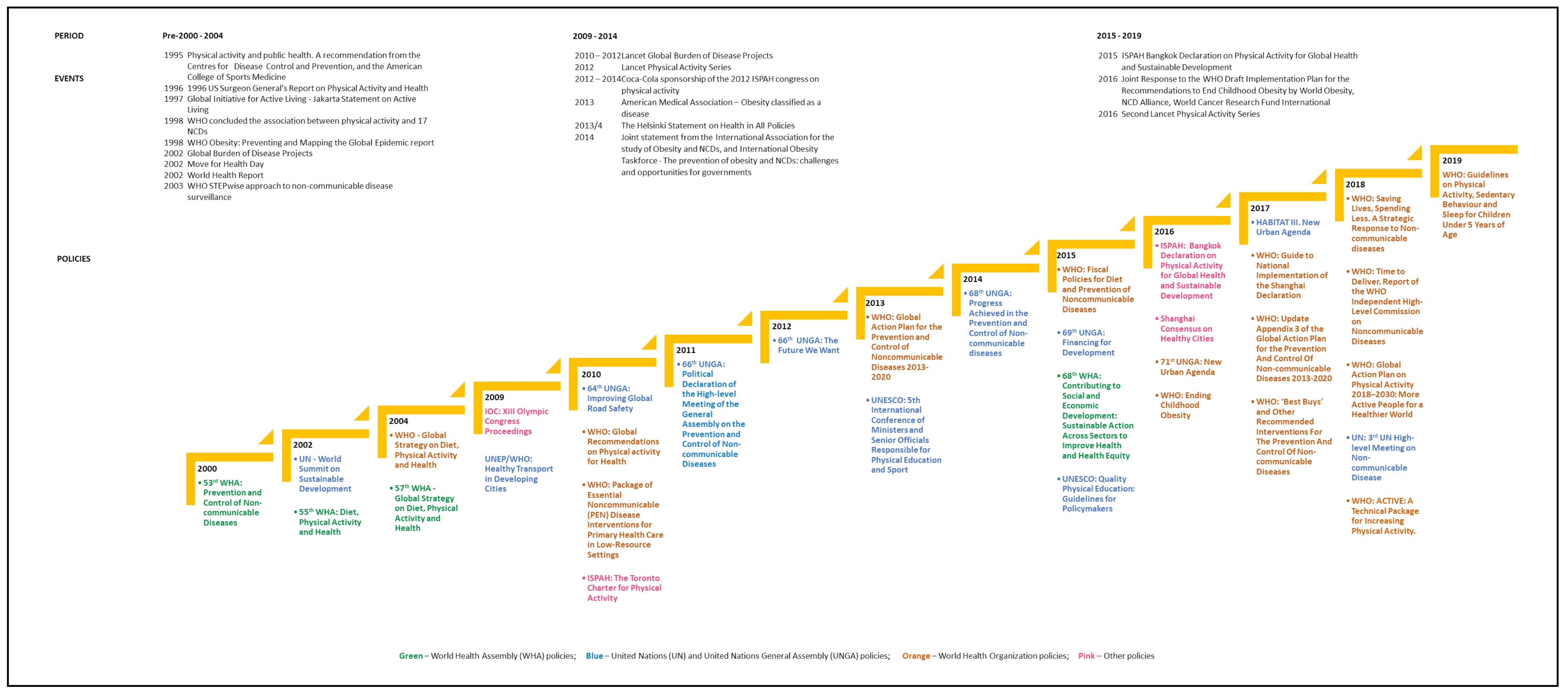
3.1. Policy Context: Global Physical Activity Policy Timeline and Sentinel Moments
3.1.1. First Growth Spurt: 2000–2004 Growth
3.1.2. Second Growth Spurt: 2009–2014
3.1.3. Third Growth Spurt: 2015–2019
3.2. Policy Content
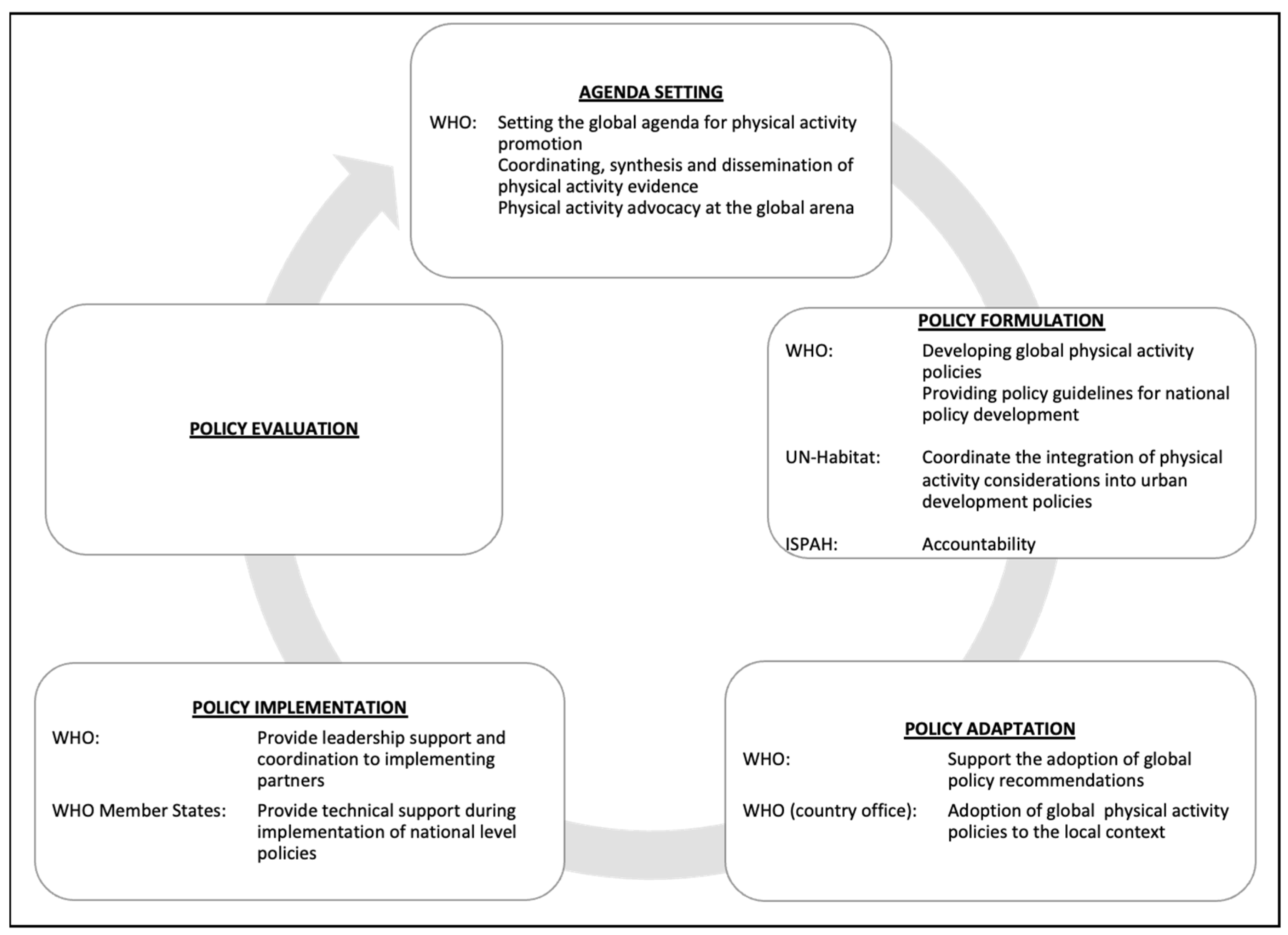
3.2.1. Key Global Physical Activity Policy Stakeholders
- World Health Organization
- The WHO leads the global PA policy development cycle via three main avenues: providing leadership and coordination, evidence synthesis and dissemination, and PA advocacy (Figure 3). Leadership by the WHO, as described in the 53rd WHA, is important for centralizing all efforts to improve global PA [34]. To this effect, the WHO has a dedicated high-level commission, which was established in 2017 to tackle the growing NCD problem, with a sub-focus on reducing the prevalence of key risk factors, notably unhealthy dietary practices and physical inactivity. Through this commission and in partnership with global and national, state, and non-state actors, the WHO coordinates evidence synthesis (to establish the importance and viability of addressing physical inactivity as a global health indicator and target), develops relevant policies, and guides global advocacy for PA [11,17,34,36,41]. To realize its global PA mandate, the WHO relies on strategic partnerships with other UN agencies, international associations, member state governments, research institutions, and academia [34].
“WHO, in cooperation with other organizations of the United Nations system, will provide the leadership, evidence-based recommendations and advocacy for international action to improve dietary practices and increase physical activity, in keeping with the guiding principles and specific recommendations contained in the Global Strategy.” 2004 57th World Health Assembly-Global strategy on diet, physical activity and health.
- WHO Member states
- WHO member state governments were identified as the key implementing agents of global PA policies [13,17,28,33,35,36]. There was agreement, across policies, that success of the global PA initiatives was reliant on the successful implementation of policies at the national level, in order to create a global synergy.
“The role of government is crucial in achieving lasting change in public health. Governments have a primary steering and stewardship role in initiating and developing the Strategy, ensuring that it is implemented and monitoring its impact in the long term”—2004 57th World Health Assembly-Global strategy on diet, physical activity and health.
- Civil Society and Community Engagement
“Civil society and nongovernment organizations have a central role in leading advocacy and monitoring accountability” 2018 World Health Organization-Global Action Plan for Physical Activity 2018–2030.
3.2.2. Structural Determinants and the Role of Intersectoral Approaches to Address Global Physical Activity
“The actions needed to increase physical activity require multi-sector leadership, partnerships, and sustained commitment as well as targeted allocation of resources”—2016 ISPAH-Bangkok Declaration on Physical Activity for Global Health and Sustainable Development.
“Action by sectors other than health, at the national, regional and local level can substantially contribute to improved health and health equity, for example, through policies involving social protection, food security, education, poverty reduction, transportation, environment, finance, trade and commerce, and taxation and legislation on the marketing of certain products. Some sectors work more closely with the health sector than others, depending on two key factors: common interests and co-benefits.”—2015 68th World Health Assembly-Contributing to social and economic development: sustainable action across sectors to improve health and health equity.
3.2.3. Policy Focus on Women and Adolescents
“Policy actions which promote physical activity through improved access to safe and affordable opportunities to participate in sport and physical activity by girls and women, particularly those in marginalised and disadvantaged communities, can contribute to ending discrimination (Target 5.1) in sports and physical activity as well as contribute to the prevention of NCDs and ensure healthy lives and promote wellbeing”—2016 ISPAH-Bangkok Declaration on Physical Activity for Global Health and Sustainable Development.
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Name | Description |
|---|---|
| Adolescents | Specific references to youth or adolescents are made |
| NCD diet | If adolescents are referenced in relation to NCD and diet |
| NCD diet physical activity | If adolescents are referenced in relation to NCD, diet, and physical activity |
| NCD only | If adolescents are referenced in relation to NCDs only |
| NCD physical activity | If adolescents are referenced in relation to NCD and physical activity |
| NMT physical activity | If adolescents are referenced in relation to non-motorized transport and physical activity |
| Gender | Specific references to gender are made |
| NCD diet | If gender is referenced in relation to NCD and diet |
| NCD diet physical activity | If gender is referenced in relation to NCD, diet, and physical activity |
| NCD only | If gender is referenced in relation to NCDs only |
| NCD physical activity | If gender is referenced in relation to NCD and physical activity |
| NMT physical activity | If gender is referenced in relation to non-motorized transport and physical activity |
| Global policy reference | Specific reference to global policy intentions, such as WHO Best Buys |
| Governance | |
| Accountability | Are there any suggestions regarding accountability? What are the accountability mechanisms for the countries assigned as responsible? |
| Leadership | Who has been identified as leaders for implementation? |
| Level of commitments | Reference to regional or international commitments? |
| Responsibility | Governance—who should coordinate a response? |
| Sectors | Which sectors are most important? |
| Implementation | Accompanying implementation plans and related timeframes |
| Challenges | E.g., what does the document say are challenges for implementing this strategy/policy? |
| Needs | What is needed regarding implementation? |
| Intersectoral | Specific mentions or encouragement of involvement of more than one sector |
| Ministry—Agency | Primary ministry/agency (e.g., WHO) responsible |
| Other | Other ministries named |
| NCD Action—Who | Who should take action on NCDs? (specific proposals) |
| NCD Problem—Why | Why are NCDs a problem? (How is this framed in the policy document?) |
| Cost | NCDs are a problem because they hamper countries’ economic growth and affect their finances |
| Mental health | |
| Mortality and morbidity | NCDs are a problem because they contribute to the burden of mortality, morbidity, and disability |
| Socio-economic inequalities | NCDs are a problem because they contribute to social and economic inequalities. |
| Other | Any other key/interesting aspects of relevance that we may not want to include in this study, but that might be worth noting |
| Physical activity NCD cause | Framing and beliefs specific to physical activity: what are the causes of physical activity-related NCDs? Beliefs about the problem |
| Physical activity proposal | Framing and beliefs specific to physical activity |
| Data collection and monitoring | |
| Education | Policy content specific to physical activity (What should be done?): physical activity education |
| Environment | Framing and beliefs specific to physical activity—specific proposals about the environment/air pollution |
| Health | Policy content—specific to physical activity (What should be done?): health systems |
| Promotion | Policy content specific to physical activity (What should be done?): social marketing and health promotion campaigns |
| Transport | Framing and beliefs specific to physical activity: specific proposals about transport |
| Urban planning | Framing and beliefs specific to physical activity: specific proposals about urban planning (including housing) |
| Purpose | Stated purpose of the document (in particular, note if a focus on NCD and, where present, if there is a focus on diet and physical activity) |
| NCD diet | If the purpose has a focus on NCD and diet |
| NCD diet physical activity | If the purpose has a focus on NCD, diet, and physical activity |
| NCD only | If the purpose has an NCD focus only |
| NCD physical activity | If the purpose has a focus on NCD and physical activity |
| NMT physical activity | If the purpose has a focus on physical activity tackled as part of non-motorized transport policy |
| Resource | Resourcing—both diet and physical activity—what commitments regarding resourcing are being made? |
| Source | Where should the money come from? |
| Target | Target population(s) (How is this construed?) |
Appendix B
| Year | Event | Description |
|---|---|---|
| Pre-2000–2004 | ||
| 1995 | Physical activity and public health; a recommendation from the (CDC) and the (ACSM) [55] | On the basis of epidemiological evidence published pre-1995, the CDC and ACSM (leading public health agencies in the USA), for the first time, released a joint message recommending that adults should engage in at least 30 minutes of physical activity on most days of the week as a health promotion and disease prevention measure. |
| 1996 | 1996 U.S. Surgeon General’s Report on Physical Activity and Health [56] | This report assessed the role of physical activity in NCD prevention. It was instrumental in highlighting that the benefits of physical activity engagement were extensive to include risk reduction for major NCDs, symptom alleviation for some mental health conditions, and weight control. |
| 1997 | GIAL—Jakarta Statement on Active Living [57] | The WHO, through the GIAL, instituted a physical activity health promotion drive based on research evidence, stating that daily physical activity enhanced overall health and that increases in sedentary lifestyles reduced opportunities for the population to engage in physical activity. |
| 1998 | The WHO concluded the association between physical activity and 17 NCD [86] | This viewpoint, published by a leading global health organization, advocated for physical activity as an important lever in the fight against increasing global incidence of NCDs. |
| 1998 | The WHO published the Obesity: Preventing and Mapping the Global Epidemic report [92] | Along with diet, the WHO identified physical activity as an amenable target reducing the worldwide incidence of obesity and subsequently NCDs. |
| 2002 | Global Burden of Disease Projects [59] | In 2002, the WHO updated findings from the World Bank-commissioned 1990 Global Burden of Disease Study. NCDs were posted as a major concern. |
| 2002 | Move for Health Day [60] | Campaign by the WHO to emphasize the importance of fitness and promote physical activity and healthy behaviours. |
| 2002 | World Health Report [61] | This report listed physical inactivity as one of the main risk factors contributing to global NCD morbidity and mortality. |
| 2003 | STEPWise [62] | The WHO launched a globally standardized data collection tool—STEPS—to report on NCD behavioural risk factors (including physical activity) trends across different contexts, particularly LMIC. |
| 2009–2014 | ||
| 2010–2012 | Lancet Global Burden of Disease Projects [93] | This report highlighted the continued increase in global NCD morbidity and mortality, as well as the growing double burden of disease challenge in LMIC contexts. This provided further evidence on the need for feasible interventions to improve health outcomes. |
| 2012 | Lancet Physical Activity Series [6,94] | Publication of this series was significant as this was the first series by a leading journal dedicated to addressing physical activity as a pandemic.This series further enunciated links between physical inactivity and health, and advocated for crosscutting interventions across all societal (micro, meso, and macro levels). |
| 2012–2014 | Coca-Cola sponsorship of the 2012 ISPAH congress on physical activity [63,64,72] | Coca-Cola—one of the leading producers of sugar-sweetened beverages—sponsored the 2012 ISPAH conference, which was focused on physical activity research and practices. This triggered global conversations on the ethical implications of large cooperation’s involvement in physical activity initiatives given their well-articulated contribution towards unhealthy behaviours. |
| 2013 | AMA—Obesity classified as a disease [95] | For the first time, obesity was recognized as a disease as opposed to being a condition by AMA. This was important for bringing more attention towards the disease and therefore more concerted efforts towards prevention and treatment. Diet and physical activity were highlighted as key areas for intervention. |
| 2013/4 | The Helsinki Statement on HAIP [96] | The HIAP approach advocated for the inclusion of health considerations across sectoral policies. This brought to the fore the need for more health behaviour considerations in other sectors, such as transport and urban planning, that directly influence opportunities to engage in physical activity. |
| 2014 | International Association for the study of Obesity: International Obesity Taskforce—The prevention of obesity and NCDs: challenges and opportunities for governments [97] | Key global consortiums focused on obesity highlighted physical activity as an important obesity and NCD prevention strategy and urged national governments to take action through a series of recommendations. |
| 2015–2019 | ||
| 2015 | ISPAH Bangkok Declaration on Physical Activity for Global Health and Sustainable Development [13] | ISPAH-linked physical activity to eight SDGs. This declaration framed physical activity in the context of economic development. |
| 2016 | World Obesity, NCD Alliance, World Cancer Research Fund International—Joint Response to the WHO Draft Implementation Plan for the Recommendations to End Childhood Obesity [58] | This was a joint response that was also co-signed by 20 other organisations working on varying aspects of NCD prevention. This signified the power inter-organizational alliances in critiquing WHO policies on obesity prevention measures. |
| 2016 | Second Lancet Physical Activity Series [83] | As a precursor to the 2012 series on physical activity, this series provided an update on the state of global physical inactivity and associated health effects. In line with transdisciplinary interest, the series, for the first time, also provided a global estimate for economic burden of physical inactivity. |
References
- Kohl, H.W., III; Craig, C.L.; Lambert, E.V.; Inoue, S.; Alkandari, J.R.; Leetongin, G.; Kahlmeier, S. The pandemic of physical inactivity: Global action for public health. Lancet 2012, 380, 294–305. [Google Scholar] [CrossRef]
- Van der Ploeg, H.P.; Hillsdon, M. Is sedentary behaviour just physical inactivity by another name? Int. J. Behav. Nutr. Phys. Act. 2017, 14, 142. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M. Sedentary behavior research network (SBRN)—Terminology consensus project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 1–17. [Google Scholar] [CrossRef] [PubMed]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Worldwide trends in insufficient physical activity from 2001 to 2016: A pooled analysis of 358 population-based surveys with 1,9 million participants. Lancet Glob. Health 2018, 6, e1077–e1086. [Google Scholar] [CrossRef]
- Guthold, R.; Stevens, G.A.; Riley, L.M.; Bull, F.C. Global trends in insufficient physical activity among adolescents: A pooled analysis of 298 population-based surveys with 1,6 million participants. Lancet Child Adolesc. Health 2020, 4, 23–35. [Google Scholar] [CrossRef]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T.; Kahlmeier, S. Effect of physical inactivity on major non-communicable diseases worldwide: An analysis of burden of disease and life expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Booth, F.W.; Roberts, C.K.; Laye, M.J. Lack of exercise is a major cause of chronic diseases. Compr. Physiol. 2011, 2, 1143–1211. [Google Scholar]
- Wagner, K.-H.; Brath, H. A global view on the development of non communicable diseases. Prev. Med. 2012, 54, S38–S41. [Google Scholar] [CrossRef]
- Beaglehole, R.; Yach, D. Globalisation and the prevention and control of non-communicable disease: The neglected chronic diseases of adults. Lancet 2003, 362, 903–908. [Google Scholar] [CrossRef]
- Beaglehole, R.; Bonita, R.; Horton, R.; Adams, C.; Alleyne, G.; Asaria, P.; Baugh, V.; Bekedam, H.; Billo, N.; Casswell, S. Priority actions for the non-communicable disease crisis. Lancet 2011, 377, 1438–1447. [Google Scholar] [CrossRef]
- World Health Organization. Global Action Plan on Physical Activity 2018–2030: More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- International Society of Physical Activity and Health. The Bangkok Declaration on Physical Activity for Global Health and Sustainable Development. In Proceedings of the 6th ISPAH Congress on Physical Activity and Public Health, Bangkok, Thailand, 16–19 November 2016; International Society of Physical Activity and Health (ISPAH): Bangkok, Thailand, 2016. [Google Scholar]
- Dishman, R.K.; Sallis, J.F.; Orenstein, D.R. The determinants of physical activity and exercise. Public Health Rep. 1985, 100, 158. [Google Scholar] [PubMed]
- Brownson, R.C.; Baker, E.A.; Housemann, R.A.; Brennan, L.K.; Bacak, S.J. Environmental and policy determinants of physical activity in the United States. Am. J. Public Health 2001, 91, 1995–2003. [Google Scholar] [CrossRef] [PubMed]
- Giles-Corti, B.; Donovan, R.J. The relative influence of individual, social and physical environment determinants of physical activity. Soc. Sci. Med. 2002, 54, 1793–1812. [Google Scholar] [CrossRef]
- World Health Organization. Global Strategy on Diet, Physical Activity and Health; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- World Health Organization. Global Recommendations on Physical Activity for Health; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- United Nations. HABITAT III: New Urban Agenda Ecuador; United Nations: New York, NY, USA, 2016. [Google Scholar]
- Walt, G.; Gilson, L. Reforming the health sector in developing countries: The central role of policy analysis. Health Policy Plan. 1994, 9, 353–370. [Google Scholar] [CrossRef]
- Hirvensalo, M.; Lintunen, T. Life-course perspective for physical activity and sports participation. Eur. Rev. Aging Phys. Act. 2011, 8, 13–22. [Google Scholar] [CrossRef]
- Azevedo, M.R.; Araújo, C.L.P.; Reichert, F.F.; Siqueira, F.V.; da Silva, M.C.; Hallal, P.C. Gender differences in leisure-time physical activity. Int. J. Public Health 2007, 52, 8–15. [Google Scholar] [CrossRef]
- Adlakha, D.; Parra, D.C. Mind the gap: Gender differences in walkability, transportation and physical activity in urban India. J. Transp. Health 2020, 18, 100875. [Google Scholar] [CrossRef]
- Oni, T.; Assah, F.; Erzse, A.; Foley, L.; Govia, I.; Hofman, K.J.; Lambert, E.V.; Micklesfield, L.K.; Shung-King, M.; Smith, J.; et al. The global diet and activity research (GDAR) network: A global public health partnership to address upstream NCD risk factors in urban low and middle-income contexts. Glob. Health 2020, 16, 1–11. [Google Scholar] [CrossRef]
- Shung-King, A.W.M.; McCreedy, N.; Tatah, L.; Mapa-Tassou, C.; Muzenda, T.; Govia, I.; Were, V.; Oni, T. Protocol for a Multi-Level Policy Analysis of Non-Communicable Disease Determinants of Diet and Physical Activity: Implications for Low- and Middle-Income Countries in Africa and the Caribbean. Int. J. Environ. Res. Public Health 2021, 18, 13061. [Google Scholar] [CrossRef]
- QSR International. NVivo 12. 2021. Available online: https://www.qsrinternational.com/nvivo-qualitative-data-analysis-software/support-services/nvivo-downloads (accessed on 1 July 2019).
- World Health Organization. Promoting Health: Guide to National Implementation of the Shanghai Declaration; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- United Nations. Time to Deliver: Third UN High-Level Meeting on Non-Communicable Diseases; United Nations: New York, NY, USA, 2018. [Google Scholar]
- United Nations Environment Programme and World Health Organization. Healthy Transport in Developing Cities; World Health Organization: Geneva, Switzerland, 2009. [Google Scholar]
- World Health Organization. Saving Lives, Spending Less: A Strategic Response to Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Package of Essential Noncommunicable (PEN) Disease Interventions for Primary Health Care in Low-Resource Settings; World Health Organization: Geneva, Switzerland, 2010. [Google Scholar]
- World Health Organization. ‘Best Buys’ and Other Recommended Interventions: Updated (2017) Appendix 3 of the Global Action Plan for the Prevention and Control of Noncommunicable Diseases 2013–2020; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization. ‘Best Buys’ and Other Recommended Interventions for The Prevention and Control of Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2017. [Google Scholar]
- World Health Organization. 53rd World Health Assembly: Resolutions and Decisions Annex; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- World Helath Organization. 55th World Health Assembly: Resolutions and Decisions Annexes; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- World Health Organization. 57th World Health Assembly: Resolutions and Decisions Annexes; World Health Organization: Geneva, Switzerland, 2004. [Google Scholar]
- World Health Organization. Fiscal Policies for Diet and Prevention of Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- World Health Organization. 68th World Health Assembly: Provisional Agenda Item 14.5 Contributing to Social and Economic Development: Sustainable Action across Sectors to Improve Health and Health Equity (Follow-Up of the 8th Global Conference on Health Promotion); World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- United Nations. World Summit on Sustainable Development Johannesburg, South Africa; United Nations: New York, NY, USA, 2002. [Google Scholar]
- United Nations. United Nations General Assembly: 64th Session—Resolutions Adopted by the General Assembly Improving Global Road Safety; United Nations: New York, NY, USA, 2010. [Google Scholar]
- United Nations. United Nations General Assembly: 66th Session Agenda Item 117 The Future We Want; United Nations: New York, NY, USA, 2012. [Google Scholar]
- United Nations. United Nations General Assembly: 68th Session Agenda Item 118 Outcome Document of the High-Level Meeting of the General Assembly on the Comprehensive Review and Assessment of the Progress Achieved in the Prevention and Control of Non-Communicable Diseases; United Nations: New York, NY, USA, 2014. [Google Scholar]
- United Nations. United Nations General Assembly: 69th Session Agenda Item 18 Addis Ababa Action Agenda of the Third International Conference on Financing for Development (Addis Ababa Action Agenda); United Nations: New York, NY, USA, 2015. [Google Scholar]
- United Nations Educational Scientific and Cultural Organization. Quality Physical Education (QPE) Guidelines for Policy-Makers; United Nations Educational, Scientific and Cultural Organization: Paris, France, 2015. [Google Scholar]
- United Nations. United Nations General Assembly: 71st Session Agenda Item 20 New Urban Agenda; United Nations: New York, NY, USA, 2017. [Google Scholar]
- United Nations Educational Scientific and Cultural Organization. 5th International Conference of Minister and Senior Officials Responsible for Physical Education and Sport; United Nations Educational, Scientific and Cultural Organization: Berlin, Germany, 2013. [Google Scholar]
- International Congress on Physical Activity and Public Health. The Toronto Charter for Physical Activity; International Congress on Physical Activity and Public Health: Toronto, ON, Canada, 2010. [Google Scholar]
- International Olympic Committee. The Olympic Movement in Society: 121st IOC Session & XIII Olympic Congress; International Olympic Committee: Copenhagen, Denmark, 2009. [Google Scholar]
- Healthy Cities Mayors Forum. Shanghai Consensus on Healthy Cities 2016. In Proceedings of the 9th Global Conference on Health Promotion, Shanghai, China, 21 November 2016; Available online: https://ncdalliance.org/sites/default/files/resource_files/9gchp-mayors-consensus-healthy-cities.pdf (accessed on 4 March 2022).
- World Health Organization. Time to Deliver: Report of the World Health Organization Independent High-Level Commission on Noncommunicable Diseases; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Active: A Technical Package for Increasing Physical Activity; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- World Health Organization. Guidelines on Physical Activity, Sedentary Behaviour and Sleep for Children under 5 Years of Age; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- United Nations. United Nations General Assembly: 66th Session Agenda Item 117 Political Declaration of the High-Level Meeting of the General Assembly on the Prevention and Control of Non-Communicable Diseases; United Nations: New York, NY, USA, 2011. [Google Scholar]
- World Health Organization. Ending Childhood Obesity; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Pate, R.R.; Pratt, M.; Blair, S.N.; Haskell, W.L.; Macera, C.A.; Bouchard, C.; Buchner, D.; Ettinger, W.; Heath, G.W.; King, A.C.; et al. Physical activity and public health: A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA 1995, 273, 402–407. [Google Scholar] [CrossRef]
- Surgeon General of the United States. US Surgeon General’s Report on Physical Activity and Health; US Department of Health and Human Services & Centers for Disease Control and Prevention: Atlanta, GA, USA, 1996; pp. 1–9. [Google Scholar]
- World Health Organization. Jakarta Statement on Active Living: 4th International Conference on Health Promotion; World Health Organization: Jakarta, Indonesia, 1997. [Google Scholar]
- World Health Organization. Obesity: Preventing and Managing the Global Epidemic—Report of a WHO Consultation (WHO Technical Report Series 894); World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Mathers, C.D.; Bernard, C.; Iburg, K.M.; Inoue, M.; Ma Fat, D.; Shibuya, K.; Stein, C.; Tomijima, N.; Xu, H. Global Burden of Disease in 2002: Data Sources, Methods and Results; World Health Organization: Geneva, Switzerland, 2003; p. 54. [Google Scholar]
- World Health Organization. World Health Day 7 April, 2002; Health World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- World Health Organization. The World Health Report 2002—Reducing Risks, Promoting Healthy Life; World Health Organization: Geneva, Switzerland, 2002. [Google Scholar]
- World Health Organization. The WHO STEPwise Approach to Surveillance of Noncommunicable Diseases (STEPS); World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- World Health Organization. Rio Political Declaration on Social Determinants of Health; World Conference on Social Determinants of Health Ed.; World Health Organization: Rio de Janeiro, Brazil, 2011. [Google Scholar]
- Khan, K.M.; Thompson, A.M.; Blair, S.N.; Sallis, J.F.; Powell, K.E.; Bull, F.C.; Bauman, A.E. Sport and exercise as contributors to the health of nations. Lancet 2012, 380, 59–64. [Google Scholar] [CrossRef]
- Foster, C.; Shilton, T.; Westerman, L.; Varney, J.; Bull, F. World Health Organisation to develop global action plan to promote physical activity: Time for action. BMJ 2018, 52, 484–485. [Google Scholar] [CrossRef] [PubMed]
- Gómez, L.; Jacoby, E.; Ibarra, L.; Lucumí, D.; Hernandez, A.; Parra, D.; Florindo, A.; Hallal, P. Sponsorship of physical activity programs by the sweetened beverages industry: Public health or public relations? Rev. De Saúde Pública 2011, 45, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Wood, B.; Ruskin, G.; Sacks, G. How Coca-Cola Shaped the International Congress on Physical Activity and Public Health: An Analysis of Email Exchanges between 2012 and 2014. Int. J. Environ. Res. Public Health 2020, 17, 8996. [Google Scholar] [CrossRef]
- Griffin, S. Coca-Cola sought to shift blame for obesity by funding public health conferences, study reports. Br. Med. J. Publ. Group 2020. [Google Scholar] [CrossRef]
- Russell, E. Exercise is medicine. Can. Med. Assoc. J. 2013, 185, E526. [Google Scholar] [CrossRef]
- Lobelo, F.; Stoutenberg, M.; Hutber, A. The exercise is medicine global health initiative: A 2014 update. Br. J. Sports Med. 2014, 48, 1627–1633. [Google Scholar] [CrossRef]
- Serodio, P.; Ruskin, G.; McKee, M.; Stuckler, D. Evaluating Coca-Cola’s attempts to influence public health ‘in their own words’: Analysis of Coca-Cola emails with public health academics leading the Global Energy Balance Network. Public Health Nutr. 2020, 23, 2647–2653. [Google Scholar] [CrossRef]
- United Nations. Transforming Our World: The 2030 Agenda for Sustainable Development; United Nations: New York, NY, USA, 2015. [Google Scholar]
- World Health Organization. Sustainable Development Goals: Health Targets—Physical Activity; World Health Organization Regional Office for Europe, Ed.; World Health Organization: Copenhagen, Denmark, 2019. [Google Scholar]
- Thai Health Promotion Foundation. Available online: https://en.thaihealth.or.th/WHO_WE_ARE/THAIHEALTH_INTRO/ (accessed on 4 March 2022).
- Pongutta, S.; Suphanchaimat, R.; Patcharanarumol, W.; Tangcharoensathien, V. Lessons from the Thai health promotion Foundation. Bull. World Health Organ. 2019, 97, 213. [Google Scholar] [CrossRef]
- Craig, L.; Fong, G.T.; Chung-Hall, J.; Puska, P. Impact of the WHO FCTC on tobacco control: Perspectives from stakeholders in 12 countries. Tob. Control 2019, 28, s129–s135. [Google Scholar] [CrossRef]
- Wisdom, J.P.; Juma, P.; Mwagomba, B.; Ndinda, C.; Mapa-Tassou, C.; Assah, F.; Nkhata, M.; Mohamed, S.F.; Oladimeji, O.; Oladunni, O.; et al. Influence of the WHO framework convention on tobacco control on tobacco legislation and policies in sub-Saharan Africa. BMC Public Health 2018, 18, 954. [Google Scholar] [CrossRef] [PubMed]
- Tatah, L.; Mapa-Tassou, C.; Shung-King, M.; Oni, T.; Woodcock, J.; Weimann, A.; McCreedy, N.; Muzenda, T.; Govia, I.; Mbanya, J.C.; et al. Analysis of Cameroon’s Sectoral Policies on Physical Activity for Noncommunicable Disease Prevention. Int. J. Environ. Res. Public Health 2021, 18, 12713. [Google Scholar] [CrossRef] [PubMed]
- Klepac Pogrmilovic, B.; Ramirez Varela, A.; Pratt, M.; Milton, K.; Bauman, A.; Biddle, S.J.; Pedisic, Z. National physical activity and sedentary behaviour policies in 76 countries: Availability, comprehensiveness, implementation, and effectiveness. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Ramirez, A.; Varela, M.P.; Borges, C.; Hallal, P. 1st. Physical Activity Almanac; Global Observatory for Physical Activity Working Group: Bogota, Colombia, 2016; Available online: https://indd.adobe.com/view/f8d2c921-4daf-4c96-9eaf-b8fb2c4de615 (accessed on 4 March 2022).
- Ramirez, A.; Hallal, P.; Pratt, M.; Bauman, A.; Borges, C.; Lee, I.-M.; Heath, G.; Powell, K.E.; Pedisic, Z.; Milton, K.; et al. 2nd Physical Activity Almanac; Global Observatory for Physical Activity Working Group: Bogota, Colombia, 2021; Available online: https://indd.adobe.com/view/cb74644c-ddd9-491b-a262-1c040caad8e3 (accessed on 4 March 2022).
- Bellew, B.; Bauman, A.; Bull, F.C.; Schoeppe, S. The rise and fall of Australian physical activity policy 1996–2006: A national review framed in an international context. Aust. N. Z. Health Policy 2008, 5, 18. [Google Scholar] [CrossRef] [PubMed]
- Sallis, J.F.; Bull, F.; Guthold, R.; Heath, G.W.; Inoue, S.; Kelly, P.; Oyeyemi, A.L.; Perez, L.G.; Richards, J.; Hallal, P.C. Progress in physical activity over the Olympic quadrennium. Lancet 2016, 388, 1325–1336. [Google Scholar] [CrossRef]
- Rabiei, K.; Kelishadi, R.; Sarrafzadegan, N.; Sadri, G.; Amani, A. Short-term results of community-based interventions for improving physical activity: Isfahan Healthy Heart Programme. Arch. Med. Sci. 2010, 6, 32. [Google Scholar] [CrossRef]
- Skaal, L.; Pengpid, S. The predictive validity and effects of using the transtheoretical model to increase the physical activity of healthcare workers in a public hospital in South Africa. Transl. Behav. Med. 2012, 2, 384–391. [Google Scholar] [CrossRef][Green Version]
- Jemmott, J.B., III; Jemmott, L.S.; Ngwane, Z.; Zhang, J.; Heeren, G.A.; Icard, L.D.; O’Leary, A.; Mtose, X.; Teitelman, A.; Carty, C. Theory-based behavioral intervention increases self-reported physical activity in South African men: A cluster-randomized controlled trial. Prev. Med. 2014, 64, 114–120. [Google Scholar] [CrossRef]
- Mendonça, B.C.; Oliveira, A.C.; Toscano, J.J.O.; Knuth, A.G.; Borges, T.T.; Malta, D.C.; Cruz, D.K.; Hallal, P.C.; Toscano, J.J.O. Exposure to a community-wide physical activity promotion program and leisure-time physical activity in Aracaju, Brazil. J. Phys. Act. Health 2010, 7, S223–S228. [Google Scholar] [CrossRef]
- Li, Y.P.; Hu, X.Q.; Schouten, E.G.; Liu, A.L.; Du, S.M.; Li, L.Z.; Cui, Z.H.; Wang, D.; Kok, F.J.; Hu, F.B.; et al. Report on childhood obesity in China (8): Effects and sustainability of physical activity intervention on body composition of Chinese youth. Biomed. Environ. Sci. 2010, 23, 180–187. [Google Scholar] [CrossRef]
- Almas, A.; Islam, M.; Jafar, T.H. School-based physical activity programme in preadolescent girls (9–11 years): A feasibility trial in Karachi, Pakistan. Arch. Dis. Child. 2013, 98, 515–519. [Google Scholar] [CrossRef] [PubMed]
- Torres, A.; Sarmiento, O.L.; Stauber, C.; Zarama, R. The Ciclovia and Cicloruta programs: Promising interventions to promote physical activity and social capital in Bogotá, Colombia. Am. J. Public Health 2013, 103, e23–e30. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization Regional Office for Africa. Global Action Plan on Physical Activity 2018–2030 in the WHO African Region; World Health Organization Regional Office for Africa: Brazzaville, Congo, 2020. [Google Scholar]
- World Health Organization Europe. Social Determinants of Health: The Solid Facts; World Health Organization: Copenhagen, Denmark, 1998. [Google Scholar]
- Lim, S.S.; Vos, T.; Flaxman, A.D.; Danaei, G.; Shibuya, K.; Adair-Rohani, H.; Al Mazroa, M.A.; Amann, M.; Anderson, H.R.; Andrews, K.G.; et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2224–2260. [Google Scholar] [CrossRef]
- Hallal, P.C.; Andersen, L.B.; Bull, F.C.; Guthold, R.; Haskell, W.; Ekelund, U. Global physical activity levels: Surveillance progress, pitfalls, and prospects. Lancet 2012, 380, 247–257. [Google Scholar] [CrossRef]
- American Medical Association House of Delegates. Resolution: 420: Recognition of Obesity as a Disease; American Medical Association House of Delegates: Chicago, IL, USA, 2013. [Google Scholar]
- World Health Organisation. The Helsinki Statement on Health in All Policies. In Proceedings of the 8th Global Conference on Health Promotion, Helsinki, Finland, 10–14 June 2013; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- International Association for the study of Obesity & International Obesity Taskforce. The Prevention of Obesity and NCDs: Challenges and Opportunities for Governments; International Association for the Study of Obesity: London, UK, 2014. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muzenda, T.; Shung-King, M.; Lambert, E.V.; Brugulat Panés, A.; Weimann, A.; McCreedy, N.; Tatah, L.; Mapa-Tassou, C.; Govia, I.; Were, V.; et al. Three Growth Spurts in Global Physical Activity Policies between 2000 and 2019: A Policy Document Analysis. Int. J. Environ. Res. Public Health 2022, 19, 3819. https://doi.org/10.3390/ijerph19073819
Muzenda T, Shung-King M, Lambert EV, Brugulat Panés A, Weimann A, McCreedy N, Tatah L, Mapa-Tassou C, Govia I, Were V, et al. Three Growth Spurts in Global Physical Activity Policies between 2000 and 2019: A Policy Document Analysis. International Journal of Environmental Research and Public Health. 2022; 19(7):3819. https://doi.org/10.3390/ijerph19073819
Chicago/Turabian StyleMuzenda, Trish, Maylene Shung-King, Estelle Victoria Lambert, Anna Brugulat Panés, Amy Weimann, Nicole McCreedy, Lambed Tatah, Clarisse Mapa-Tassou, Ishtar Govia, Vincent Were, and et al. 2022. "Three Growth Spurts in Global Physical Activity Policies between 2000 and 2019: A Policy Document Analysis" International Journal of Environmental Research and Public Health 19, no. 7: 3819. https://doi.org/10.3390/ijerph19073819
APA StyleMuzenda, T., Shung-King, M., Lambert, E. V., Brugulat Panés, A., Weimann, A., McCreedy, N., Tatah, L., Mapa-Tassou, C., Govia, I., Were, V., & Oni, T. (2022). Three Growth Spurts in Global Physical Activity Policies between 2000 and 2019: A Policy Document Analysis. International Journal of Environmental Research and Public Health, 19(7), 3819. https://doi.org/10.3390/ijerph19073819







