Geo-Climatic Factors of Malaria Morbidity in the Democratic Republic of Congo from 2001 to 2019
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Areas and Population
2.2. Datasets
2.3. Climatic Parameters
2.4. Statistical Methods
- = Total evaporation under shelter;
- = Mean relative humidity;
- = Maximum temperature;
- = Minimum temperature;
- = Mean wind speed at 2 m above ground
- = Season
3. Results
3.1. Spatial and Temporal Distribution of Malaria Morbidity
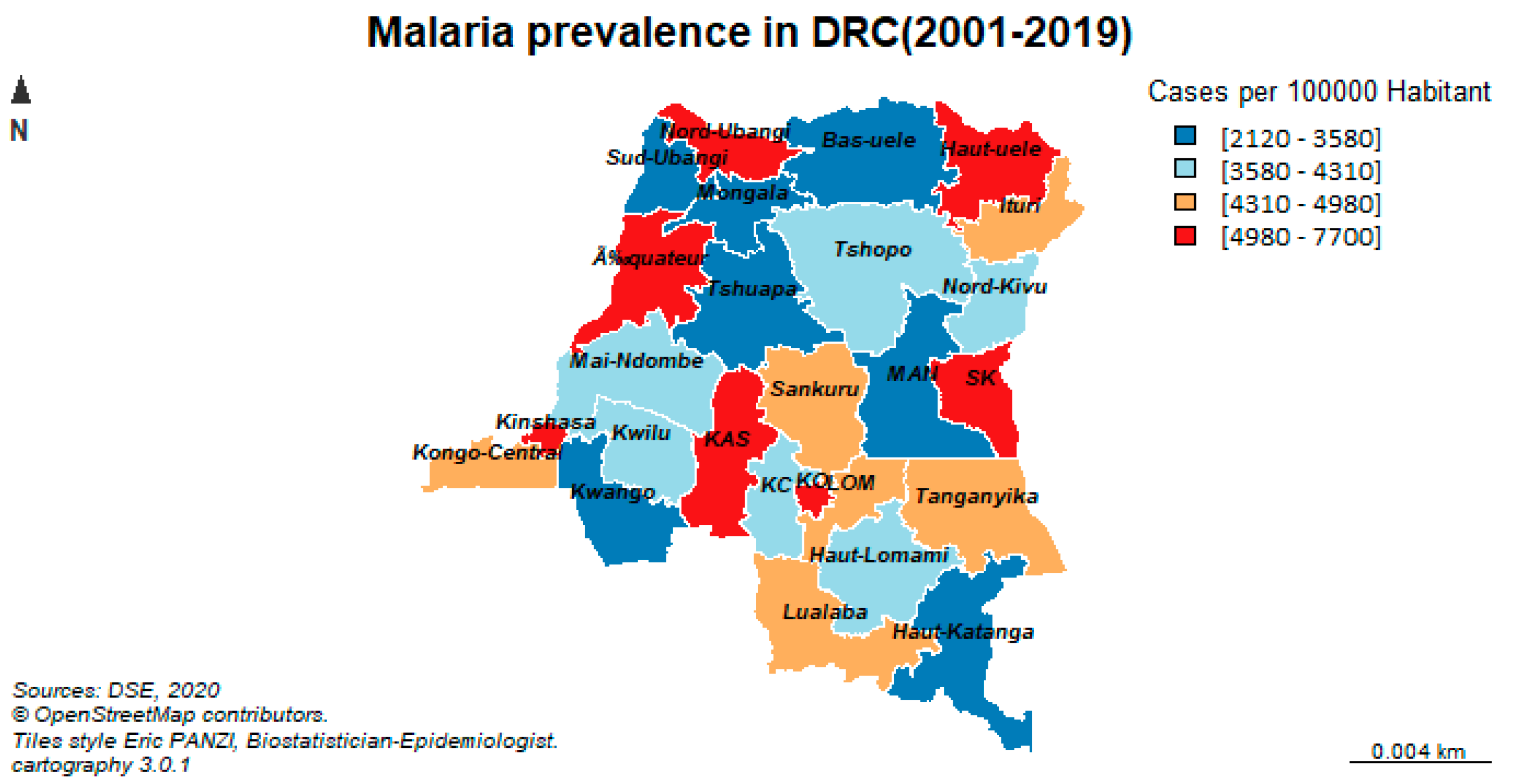
3.1.1. Spatial Distribution of Malaria Morbidity
3.1.2. Spatial and Temporal Distribution of Malaria Morbidity
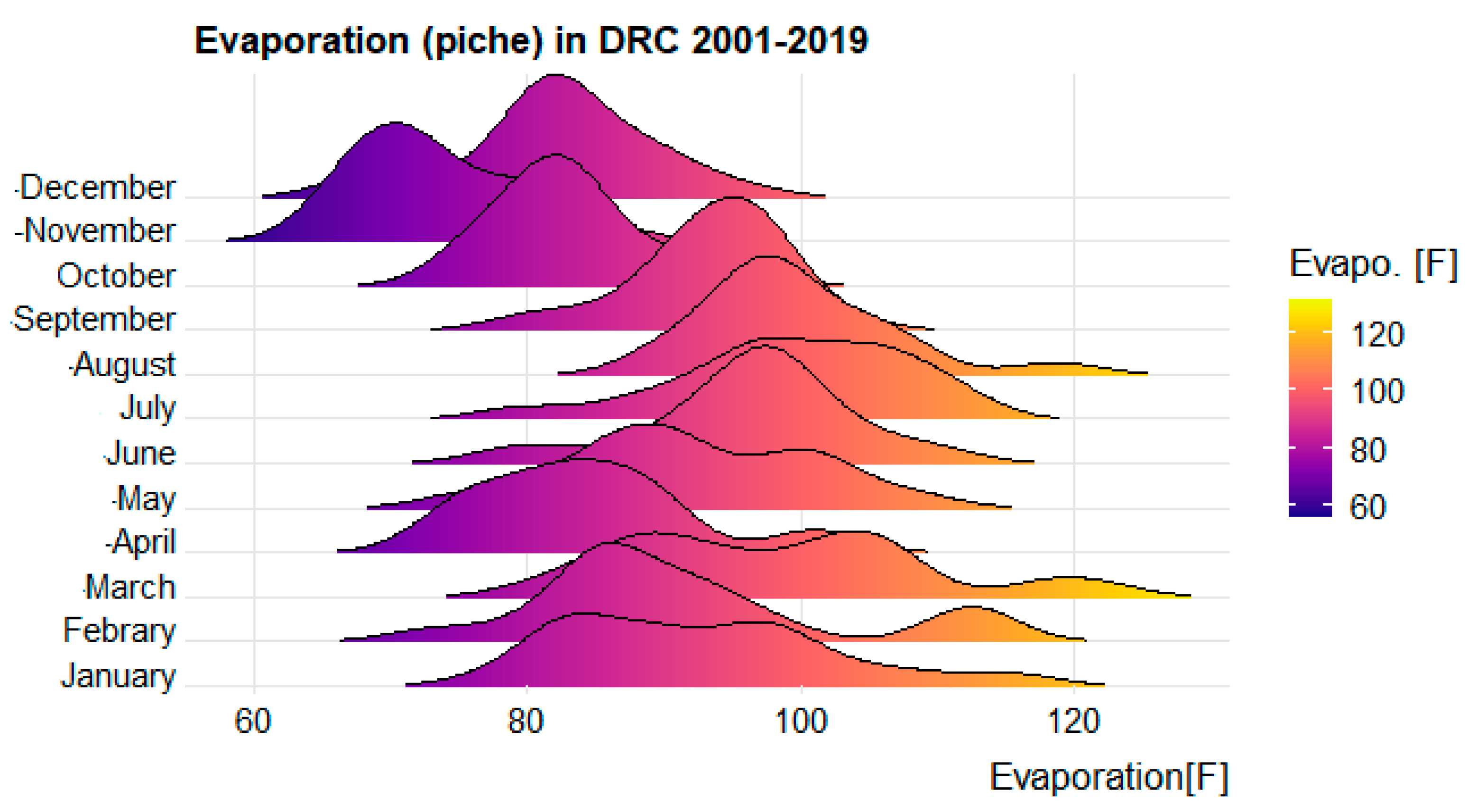
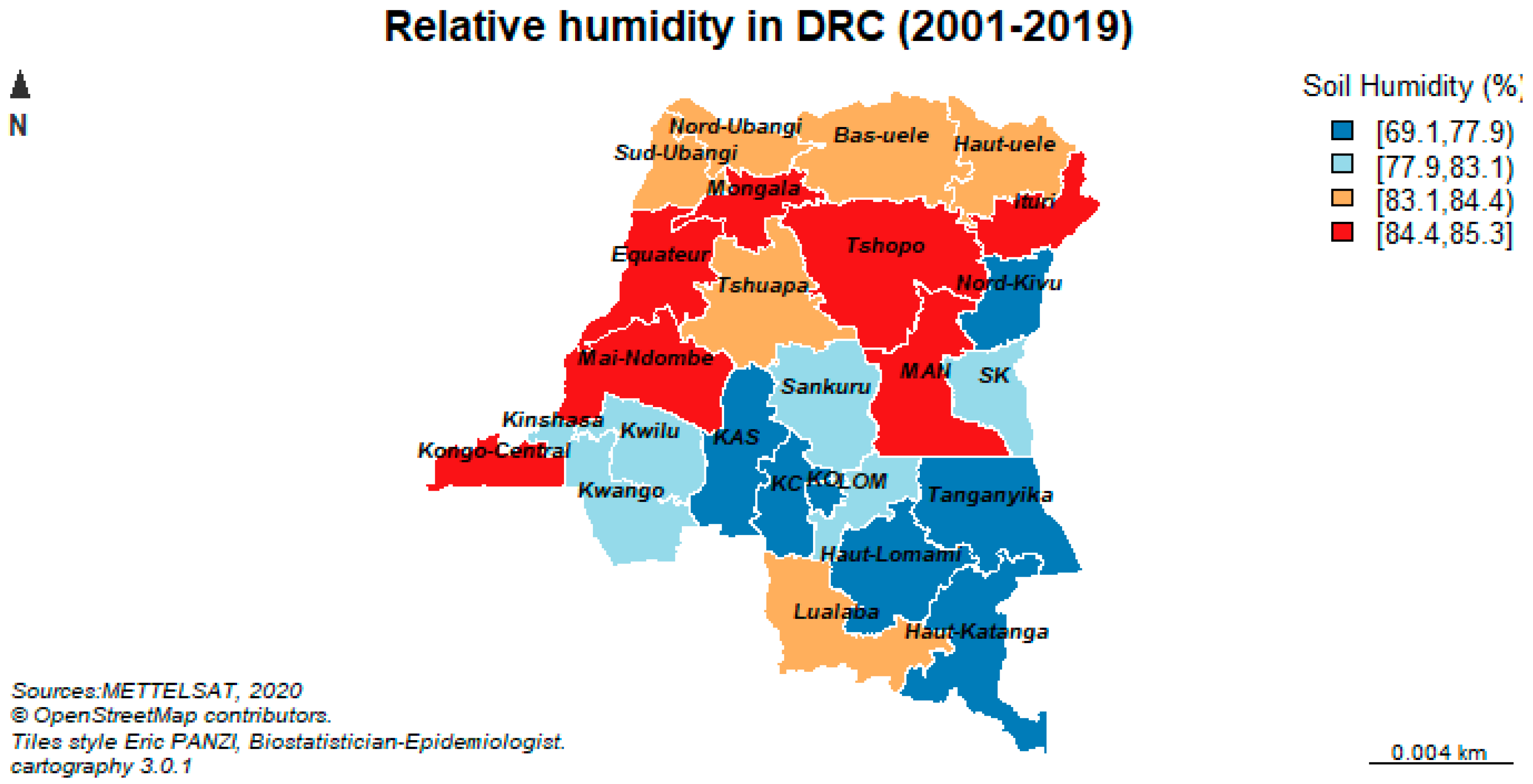
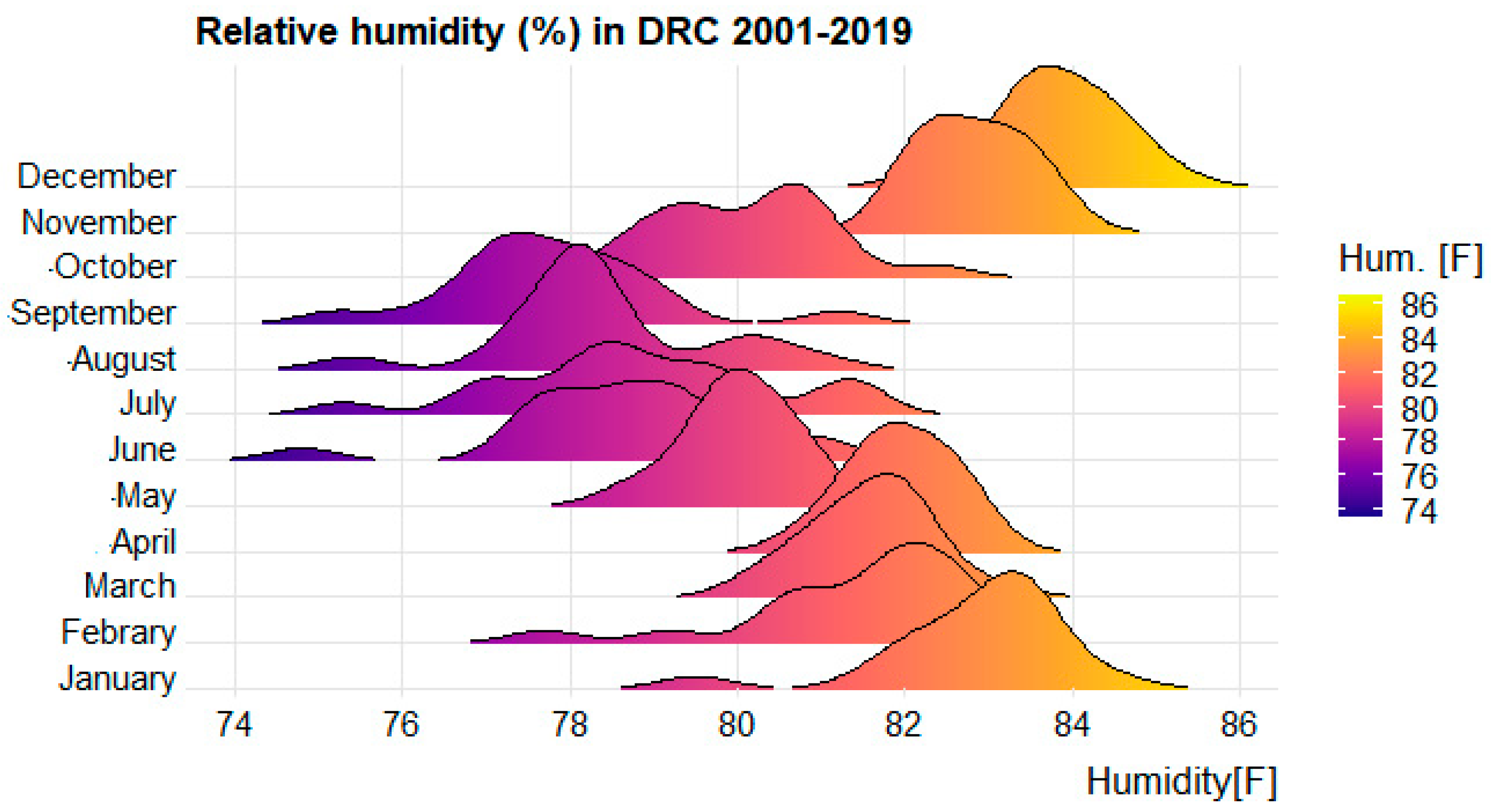
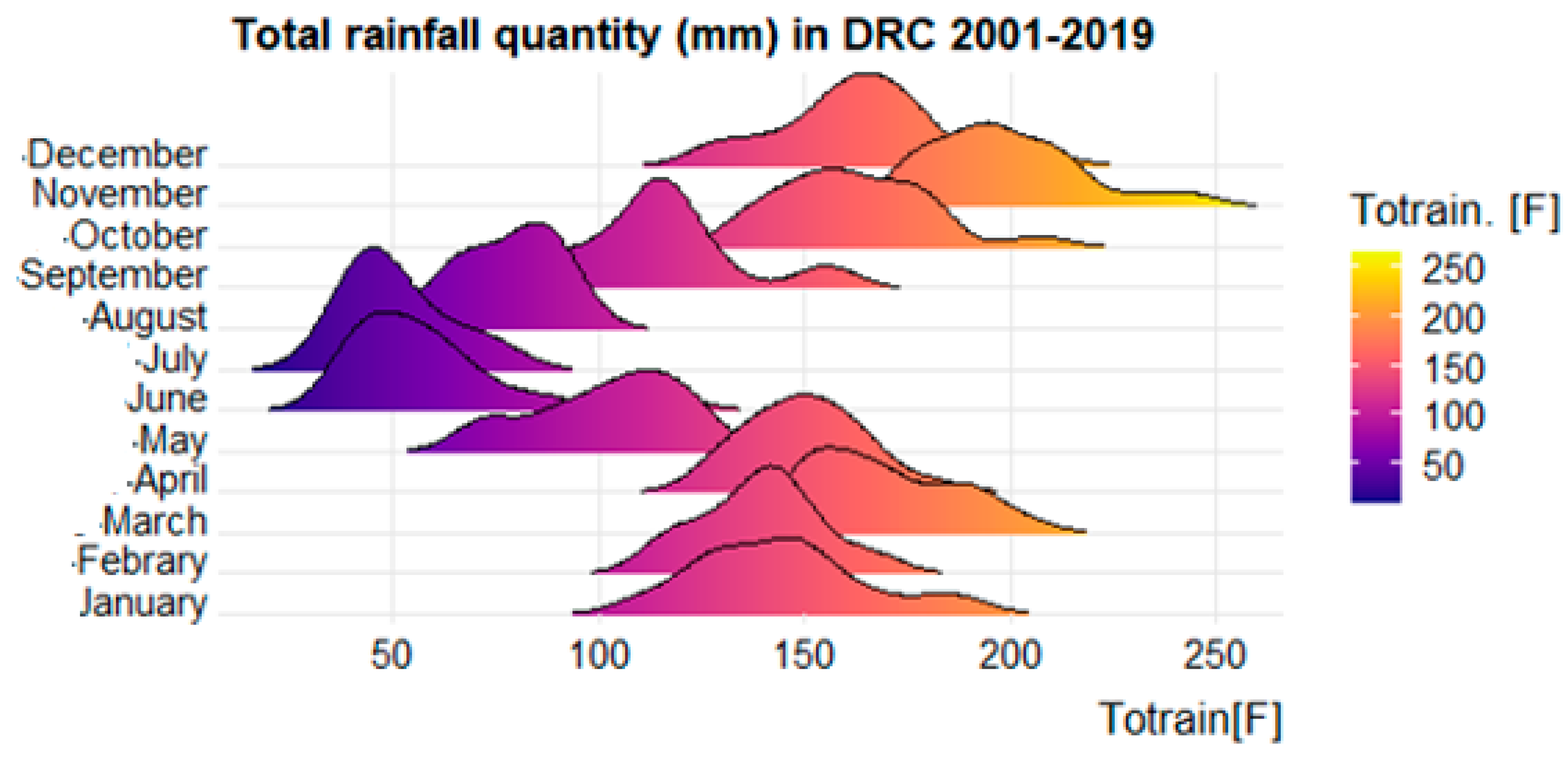
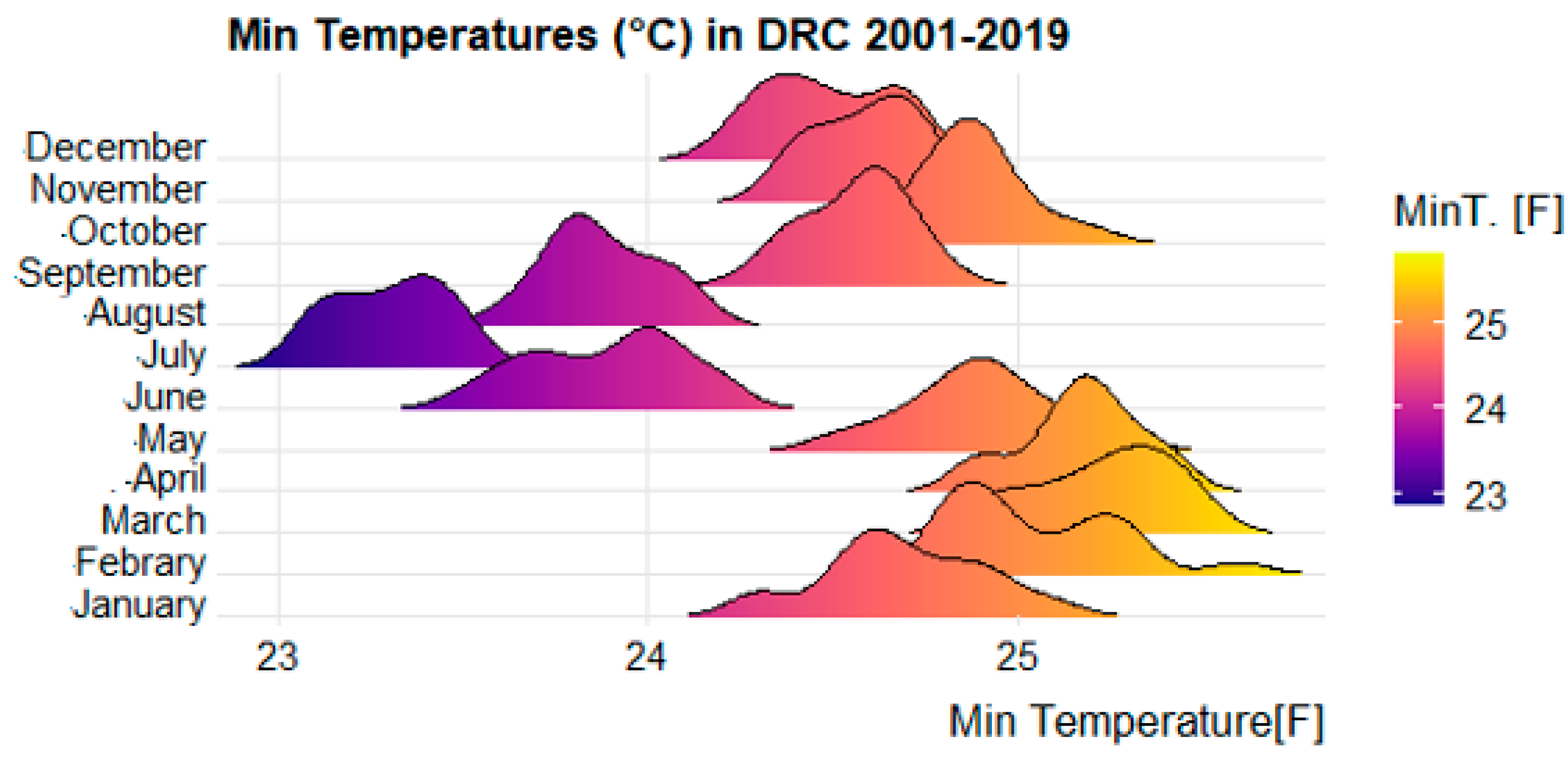
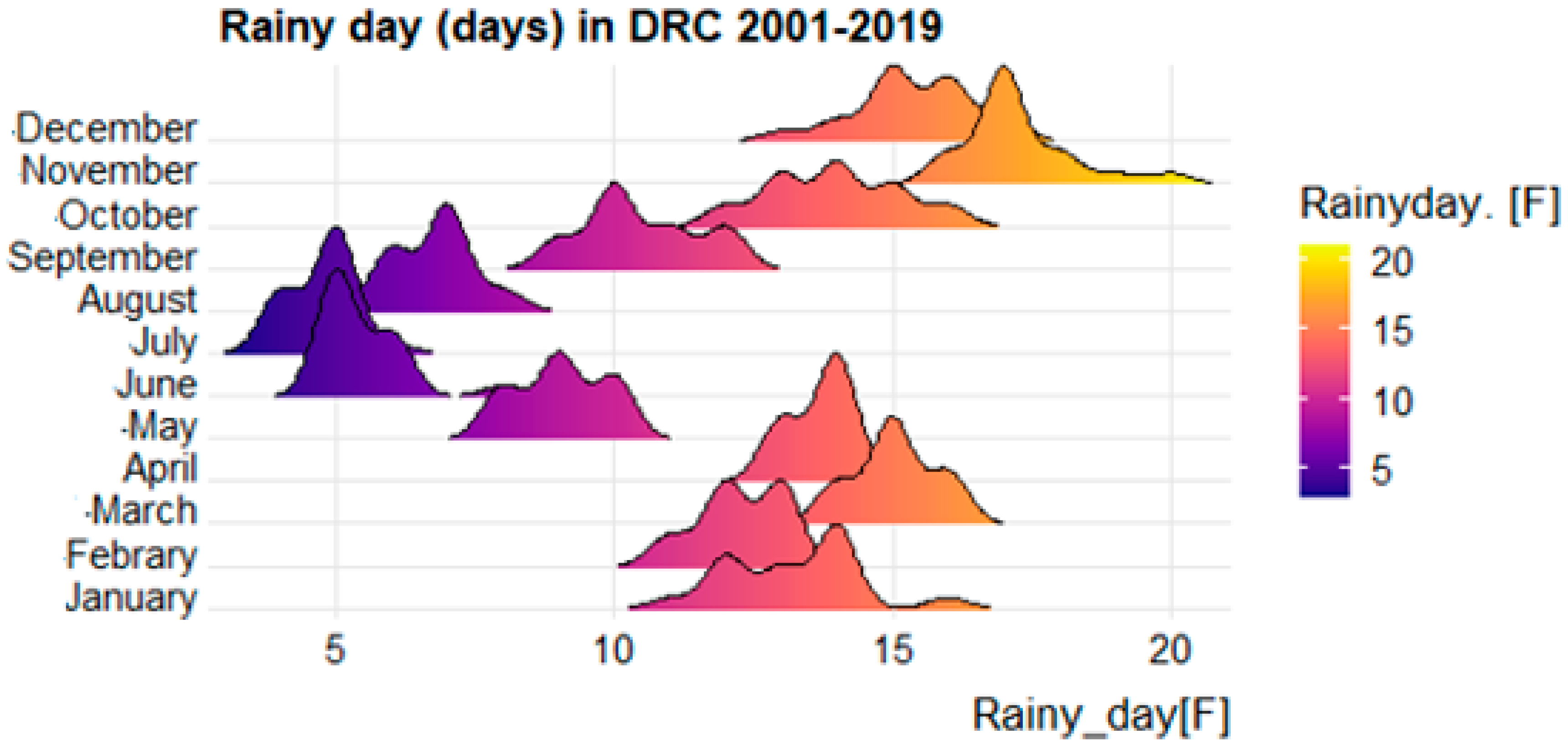
3.2. Weather Profile
3.3. Climate Predictors Associated with Malaria
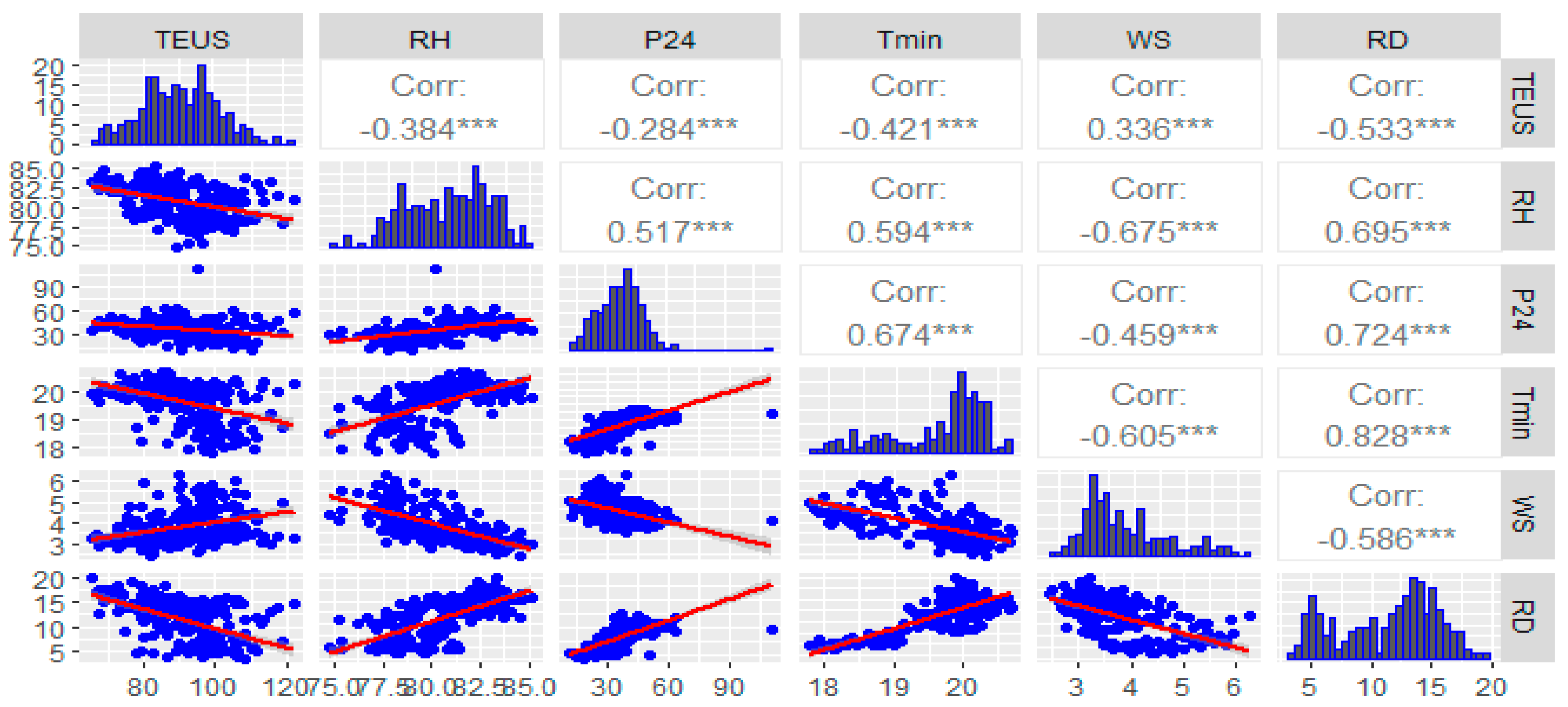
3.3.1. Matrix of Correlations
3.3.2. Generalized Linear Model of Poisson Regression
4. Discussion
Spatial and Temporal Distribution of Malaria Morbidity
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
References
- Howes, R.E.; Reiner, R.C., Jr.; Battle, K.E.; Longbottom, J.; Mappin, B.; Ordanovich, D.; Tatem, A.J.; Drakeley, C.; Gething, P.W.; Zimmerman, P.A.; et al. Plasmodium vivax transmission in Africa. PLoS Negl. Trop. 2015, 9, e0004222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Roucher, C.; Rogier, C.; Sokhna, C.; Tall, A.; Trape, J.F. A 20-year longitudinal study of Plasmodium ovale and Plasmodium malariae prevalence and morbidity in a West African population. PLoS ONE 2014, 9, e87169. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Deschênes, A. Régression Logistique Bayésienne: Comparaison de Densités a Priori Par. Master’s Thesis, Université de Montréal, Montreal, QC, Canada, 2015. [Google Scholar]
- WHO. Climate Change and Human Health—Risks and Responses. Summary; WHO: Geneva, Switzerland, 2003.
- Dumnot, G.-F.; Etchelecou, A. Environnement et santé, une évidence pour l’opinion et un défi pour la connaissance. In Programme du Colloque “Les Populations Vulnérables” en 2007; CUDEP: Bordeaux, France, 2010; pp. 429–435. [Google Scholar]
- WHO. World Malaria Report 2019 at a Glance; WHO: Geneva, Switzerland, 2019.
- WHO. Global Health Risks. Mortality and Burden of Disease Attributable to Selected Major Risks; WHO: Geneva, Switzerland, 2009.
- WHO. WHO Public Health and Environment in the African Region: Report on the Work of WHO (2008–2009); WHO: Geneva, Switzerland, 2010.
- UNICEF; WHO. Progress on Drinking Water and Sanitation; WHO: Geneva, Switzerland; UNICEF: New York, NY, USA, 2014; 78p.
- Paaijmans, K.P.; Read, A.F.; Thomas, M.B. Understanding the link between malaria risk and climate. Proc. Natl. Acad. Sci. USA 2009, 106, 13844–13849. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Briet, O.J.; Vounatsou, P.; Amerasinghe, P.H. Malaria seasonality and rainfall seasonality in Sri Lanka are correlated in space. Geospat. Health 2008, 2, 183–190. [Google Scholar] [CrossRef]
- Coghlan, B.; Ngoy, P.; Mulumba, F.; Hardy, C.; Bemo, V.N.; Stewart, T.; Lewis, J.; Brennan, R. Mortality in the Democratic Republic of Congo: An Ongoing Crisis. Int. Rescue Comm. 2007, 21. Available online: http://www.theirc.org/news/irc-study-shows-congos-neglected-crisis-leaves-54-million-dead-peace-deal-n-kivu-increased-aid--4331 (accessed on 7 March 2022).
- UNOHCHR. DRC: Mapping Human Rights Violations 1993–2003; United Nations Human Rights Office of the High Commissioner (OHCHR): Geneva, Switzerland, 2010.
- Famoye, F. On the Generalized Poisson Regression Model with an Application to Accident Data. J. Data Sci. 2021, 2, 287–295. [Google Scholar] [CrossRef]
- Zeileis, A.; Kleiber, C.; Jackman, S. Regression models for count data in R. J. Stat. Softw. 2008, 27, 1–25. [Google Scholar] [CrossRef] [Green Version]
- Saurwein, D. Analyse des Tendances Passées et Futures de Variables Météorologiques Pour des Stations de Mesure de Moyenne. Bachelor’s Thesis, University of Fribourg, Fribourg, Switzerland, 2016; pp. 1–74. [Google Scholar]
- Adeola, A.M.; Botai, J.O.; Rautenbach, H.; Adisa, O.M.; Ncongwane, K.P.; Botai, C.M.; Adebayo-Ojo, T.C. Climatic variables and malaria morbidity in mutale local municipality, South Africa: A 19-year data analysis. Int. J. Environ. Res. Public Health 2017, 14, 1360. [Google Scholar] [CrossRef] [Green Version]
- Wilson, M. Abnormal forms of Plasmodium vivax. Trans. R. Soc. Trop. Med. Hyg. 1949, 43, 97–98. [Google Scholar] [CrossRef]
- Ngomane, L.; De Jager, C. Changes in malaria morbidity and mortality in Mpumalanga Province, South Africa (2001–2009): A retrospective study. Malar. J. 2012, 11, 19. [Google Scholar] [CrossRef] [Green Version]
- Lindsay, S.W.; Birley, M.H. Climate change and malaria transmission. Ann. Trop. Med. Parasitol. 1996, 90, 573–588. [Google Scholar] [CrossRef] [PubMed]
- Lindsay, S.W.; Bodker, R.; Malima, R.; Msangeni, H.A.; Kisinza, W. Effect of 1997–98 El Nino on highland malaria in Tanzania. Lancet 2000, 355, 989–990. [Google Scholar] [CrossRef]
- Grieco, J.P.; Rejmánková, E.; Achee, N.L.; Klein, C.N.; Andre, R.; Roberts, D. Habitat suitability for three species of Anopheles mosquitoes: Larval growth and survival in reciprocal placement experiments. J. Vector. Ecol. 2007, 32, 176–187. [Google Scholar] [CrossRef]
- Vittor, A.Y.; Pan, W.; Gilman, R.H.; Tielsch, J.; Glass, G.; Shields, T.; Sánchez-Lozano, W.; Pinedo, V.V.; Salas-Cobos, E.; Flores, S.; et al. Linking deforestation to malaria in the Amazon: Characterization of the breeding habitat of the principal malaria vector, Anopheles darlingi. Am. J. Trop. Med. Hyg. 2009, 81, 5–12. [Google Scholar] [PubMed]
- Confalonieri, U.E.C.; Menne, B.; Akhtar, R.; Ebi, K.L.; Hauengue, M.; Kovats, R.S. Impacts, Adaptation and Vulnerability Contribution of Working Group II to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change; Parry, M.L., Canziani, O.F., Palutikof, J.P., van der Linden, P.J., Hanson, C.E., Eds.; Cambridge University Press: Cambridge, UK, 2007; pp. 391–431. Available online: https://www.ipcc.ch/report/ar4/wg2/ (accessed on 7 March 2022).
- Pascual, M.; Ahumadata, J.; Chaves, L.F.; Rodo, X.; Bouma, M. Malaria resurgence in the East African highlands: Temperature trends revisited. Proc. Natl. Acad. Sci. USA 2006, 103, 15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Efe, S.I.; Ojoh, C.O. Climate variation and malaria prevalence in Warri Metropolis. Atmos. Clim. Sci. 2013, 3, 27584. [Google Scholar] [CrossRef] [Green Version]
- Gomez-Elipe, A.; Otero, A.; Van Herp, M.; Aguirre-Jaime, A. Forecasting malaria incidence based on monthly case reports and environmental factors in Karuzi, Burundi. Malar. J. 2007, 6, 129. [Google Scholar] [CrossRef] [Green Version]
- Keiser, J.; Utzinger, J.; De Castro, M.C.; Smith, T.A.; Tanner, M.; Singer, B.H. Urbanization in sub-Saharan Africa and implication for malaria control. Am. J. Trop. Med. Hyg. 2004, 71, 118–127. [Google Scholar] [CrossRef] [Green Version]
- Omonijo, A.G.; Matzarakis, A.; Oguntoke, O.; Adeofun, C.O. Influence of weather and climate on malaria occurrence based on human-biometeorological methods in Ondo State, Nigeria. J. Environ. Sci. Eng. 2011, 5, 15–25. [Google Scholar]
- Krefis, A.C.; Schwarz, N.G.; Krüger, A.; Fobil, J.; Nkrumah, B.; Acquah, S.; Loag, W.; Sarpong, N.; Adu-Sarkodie, Y.; Ranft, U.; et al. Modeling the relationship between precipitation and malaria incidence in children from a holoendemic area in Ghana. Am. J. Trop. Med. Hyg. 2011, 84, 285. [Google Scholar] [CrossRef]
- Hales, S.; Edwards, S.J.; Kovats, R.S. Impacts on health of climate extremes. Clim. Chang. Hum. Health Risks Responses 2003, 79–102. Available online: https://www.who.int/globalchange/publications/climatechangechap5.pdf (accessed on 7 March 2022).
| Year | n | Prevalence | 95% Confidence Interval | |||
|---|---|---|---|---|---|---|
| Total Cases | Person-Years at Risk | Lower Bound | Upper Bound | |||
| 2001 | 26 | 29,310 | 575,363 | 509 | 2918 | 7182 |
| 2002 | 26 | 173,182 | 594,350 | 29,138 | 12,095 | 38,305 |
| 2003 | 26 | 150,213 | 613,964 | 24,466 | 12,110 | 38,873 |
| 2004 | 26 | 42,518 | 634,224 | 6704 | 4407 | 8317 |
| 2005 | 26 | 80,413 | 655,154 | 12,274 | 7332 | 14,727 |
| 2006 | 26 | 55,812 | 676,774 | 8247 | 5065 | 10,857 |
| 2007 | 26 | 56,627 | 699,108 | 8100 | 5248 | 9887 |
| 2008 | 26 | 56,321 | 722,178 | 7799 | 5543 | 9439 |
| 2009 | 26 | 73,720 | 746,010 | 9882 | 7074 | 11,717 |
| 2010 | 26 | 85,153 | 770,628 | 11,050 | 7854 | 12,937 |
| 2011 | 26 | 89,301 | 796,059 | 11,218 | 8249 | 13,793 |
| 2012 | 26 | 93,771 | 822,329 | 11,403 | 9165 | 13,859 |
| 2013 | 26 | 98,428 | 849,466 | 11,587 | 9420 | 13,569 |
| 2014 | 26 | 109,644 | 877,498 | 12,495 | 10,555 | 15,395 |
| 2015 | 26 | 118,909 | 906,456 | 13,118 | 10,669 | 16,136 |
| 2016 | 26 | 141,464 | 936,369 | 15,108 | 13,126 | 18,197 |
| 2017 | 26 | 159,141 | 967,269 | 16,453 | 13,168 | 22,395 |
| 2018 | 26 | 167,609 | 998,169 | 16,792 | 14,362 | 20,382 |
| 2019 | 26 | 188,362 | 1,030,056 | 18,287 | 15,794 | 23,097 |
| Total | 494 | 1,969,897 | 14,871,424 | 13,246 | 11,784 | 14,175 |
| Year | n | Lethality | 95% Confidence Interval | |
|---|---|---|---|---|
| Lower Bound | Lower Bound | |||
| 2001 | 26 | 0.67 | 0.43 | 0.91 |
| 2002 | 26 | 0.68 | 0.53 | 0.83 |
| 2003 | 26 | 0.52 | 0.38 | 0.67 |
| 2004 | 26 | 0.45 | 0.34 | 0.56 |
| 2005 | 26 | 0.33 | 0.25 | 0.42 |
| 2006 | 26 | 0.33 | 0.26 | 0.40 |
| 2007 | 26 | 0.33 | 0.26 | 0.39 |
| 2008 | 26 | 0.32 | 0.25 | 0.40 |
| 2009 | 26 | 0.28 | 0.22 | 0.34 |
| 2010 | 26 | 0.25 | 0.17 | 0.32 |
| 2011 | 26 | 0.29 | 0.21 | 0.37 |
| 2012 | 26 | 0.27 | 0.19 | 0.36 |
| 2013 | 26 | 0.29 | 0.19 | 0.40 |
| 2014 | 26 | 0.27 | 0.20 | 0.34 |
| 2015 | 26 | 0.23 | 0.18 | 0.29 |
| 2016 | 26 | 0.20 | 0.16 | 0.24 |
| 2017 | 26 | 0.15 | 0.11 | 0.18 |
| 2018 | 26 | 0.12 | 0.09 | 0.15 |
| 2019 | 26 | 0.11 | 0.09 | 0.14 |
| Total | 494 | 0.32 | 0.30 | 0.35 |
| Weather Parameters | Mean | sd |
|---|---|---|
| Rainy day (day/month), mean(sd) | 11.4 | 2.8 |
| Total evaporation under shelter (pitcher) | 90.5 | 20.5 |
| Humidity (%) | 80.7 | 5.6 |
| Total rainfall (mm) | 127.6 | 35.5 |
| Precipitation of 24 h | 37.4 | 12.3 |
| Max. temperature (°C) | 29.5 | 2.3 |
| Min. temperature (°C) | 19.6 | 2.1 |
| Wind speed at 2 m from the soil (m/s) | 3.8 | 0.5 |
| Variables/Distance | p-Value | |
|---|---|---|
| (Intercept) | 127,424 | 0.0001 |
| ln (Time) | 10,000 | |
| Regions | ||
| Northwest (reference class) | 10,000 | |
| West | 15,936 | 0.0001 |
| Central | 0.9823 | 0.0001 |
| North-East | 0.9492 | 0.0001 |
| Evaporation | −0.0191 | 0.0001 |
| Soil moisture | −0.0043 | 0.0001 |
| Average number of rainy days | 0.0645 | 0.0001 |
| Total rainfall quantity | 0.0002 | 0.0001 |
| Precipitation 24 h | −0.0010 | 0.0001 |
| Minimum temperature | −0.1302 | 0.0001 |
| Maximum temperature | 0.0726 | 0.0001 |
| Wind speed | −0.2017 | 0.0001 |
| sigma | 10,800 | 0.0001 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Panzi, E.K.; Okenge, L.N.; Kabali, E.H.; Tshimungu, F.; Dilu, A.K.; Mulangu, F.; Kandala, N.-B. Geo-Climatic Factors of Malaria Morbidity in the Democratic Republic of Congo from 2001 to 2019. Int. J. Environ. Res. Public Health 2022, 19, 3811. https://doi.org/10.3390/ijerph19073811
Panzi EK, Okenge LN, Kabali EH, Tshimungu F, Dilu AK, Mulangu F, Kandala N-B. Geo-Climatic Factors of Malaria Morbidity in the Democratic Republic of Congo from 2001 to 2019. International Journal of Environmental Research and Public Health. 2022; 19(7):3811. https://doi.org/10.3390/ijerph19073811
Chicago/Turabian StylePanzi, Eric Kalunda, Léon Ngongo Okenge, Eugénie Hamuli Kabali, Félicien Tshimungu, Angèle Keti Dilu, Felix Mulangu, and Ngianga-Bakwin Kandala. 2022. "Geo-Climatic Factors of Malaria Morbidity in the Democratic Republic of Congo from 2001 to 2019" International Journal of Environmental Research and Public Health 19, no. 7: 3811. https://doi.org/10.3390/ijerph19073811
APA StylePanzi, E. K., Okenge, L. N., Kabali, E. H., Tshimungu, F., Dilu, A. K., Mulangu, F., & Kandala, N.-B. (2022). Geo-Climatic Factors of Malaria Morbidity in the Democratic Republic of Congo from 2001 to 2019. International Journal of Environmental Research and Public Health, 19(7), 3811. https://doi.org/10.3390/ijerph19073811







