Client’s Experiences Using a Location-Based Technology ICT System during Gambling Treatments’ Crucial Components: A Qualitative Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Therapist
2.3. Measures
2.3.1. Diagnosis Measures and Measures for the Target Behaviors
2.3.2. Measures for Expectations and Satisfaction with the LBT-Based ICT System
2.3.3. Measures for Acceptability and Usability of the LBT-based ICT System
2.3.4. LBT-Based ICT System Qualitative Interview
2.4. Treatment
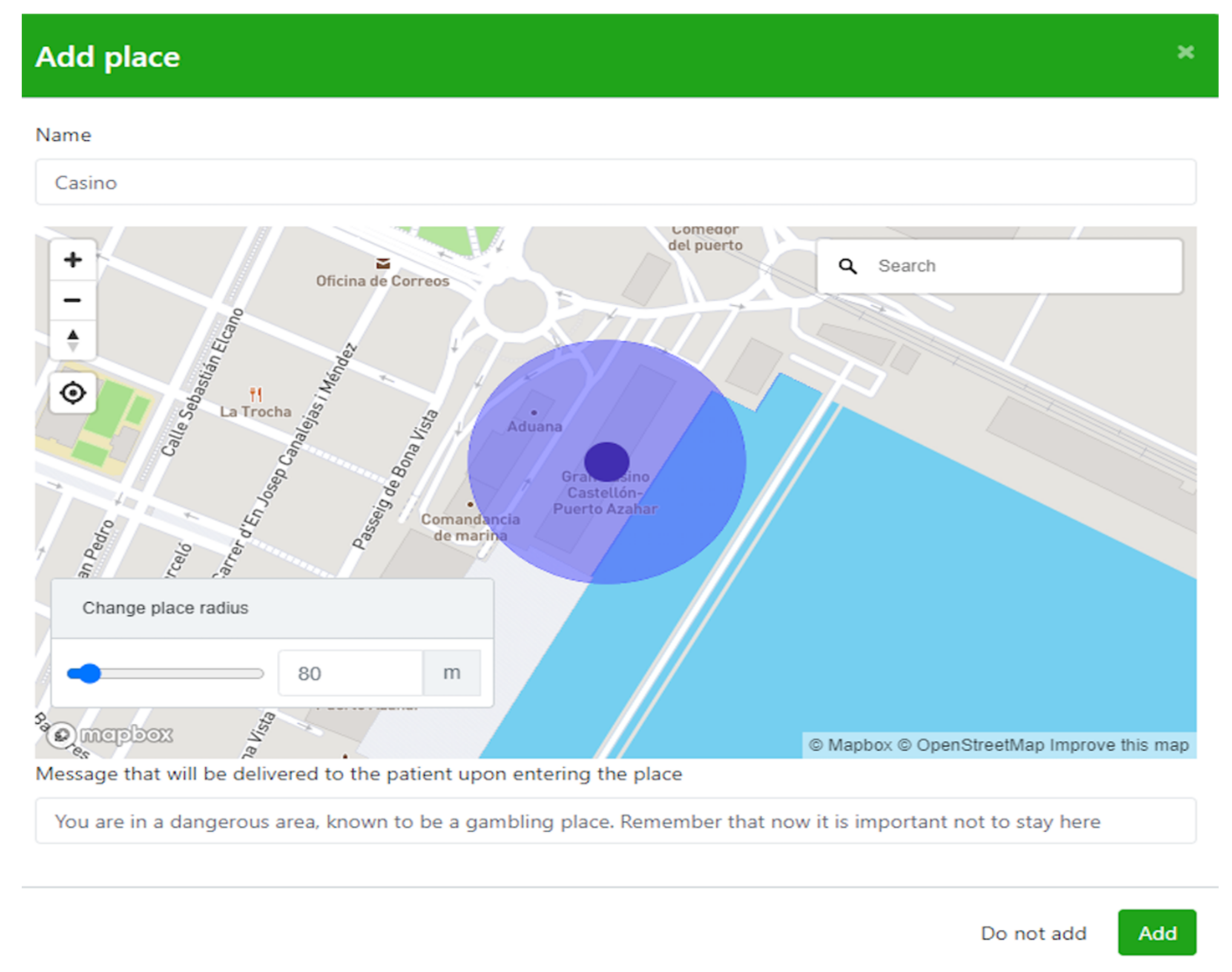
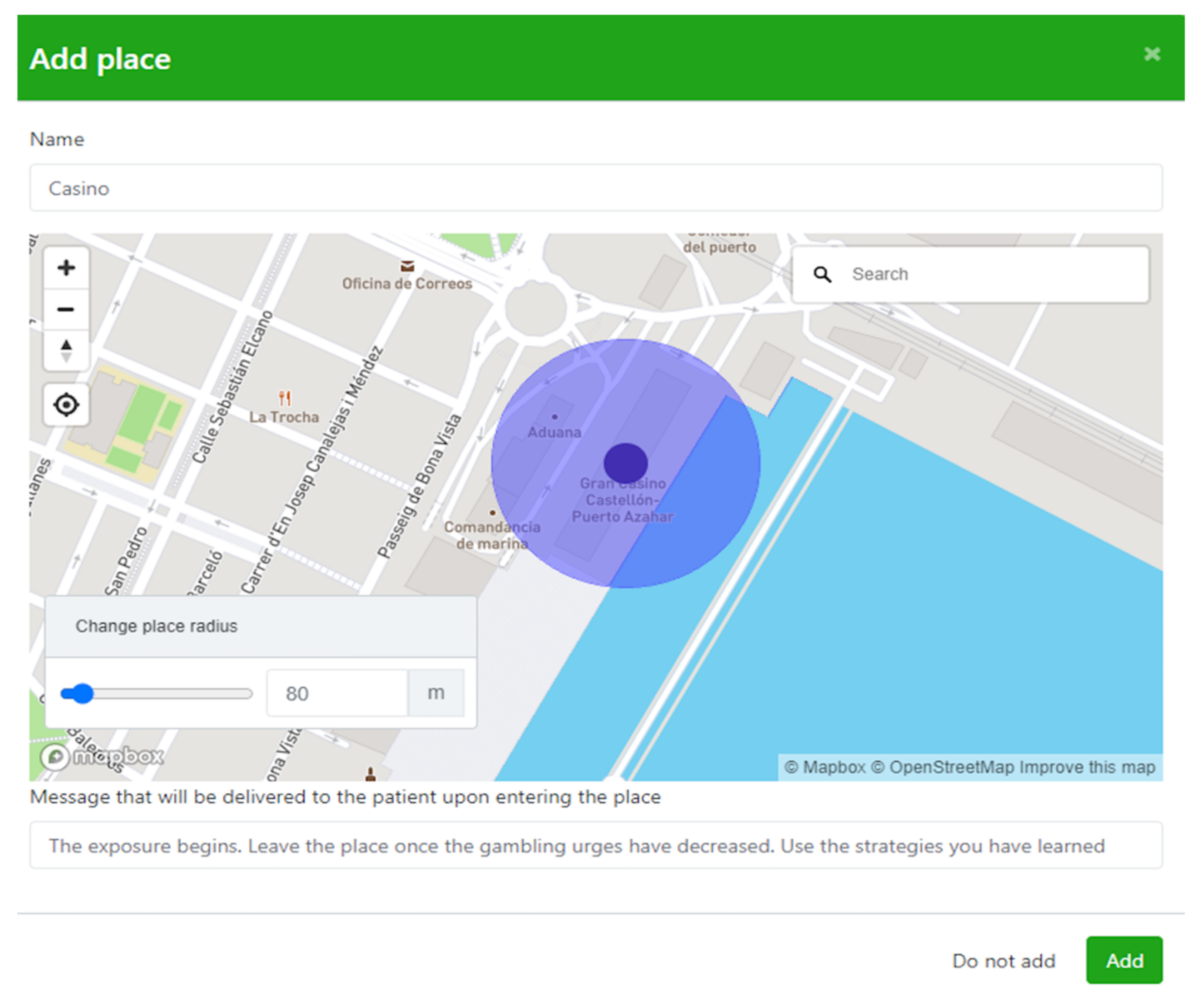
2.5. System Description
2.6. Design
2.7. Data Analysis
2.8. Procedure
3. Results
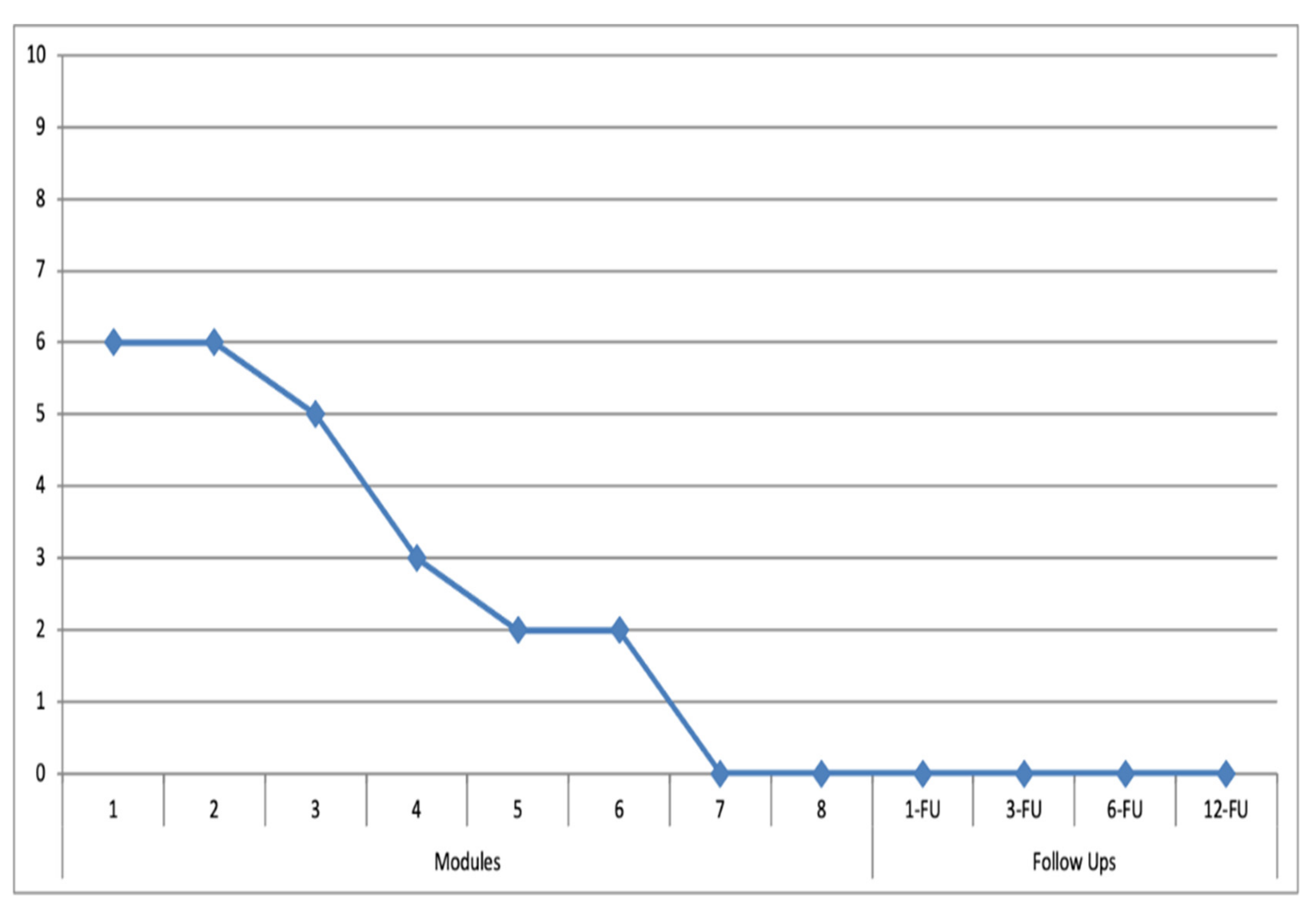
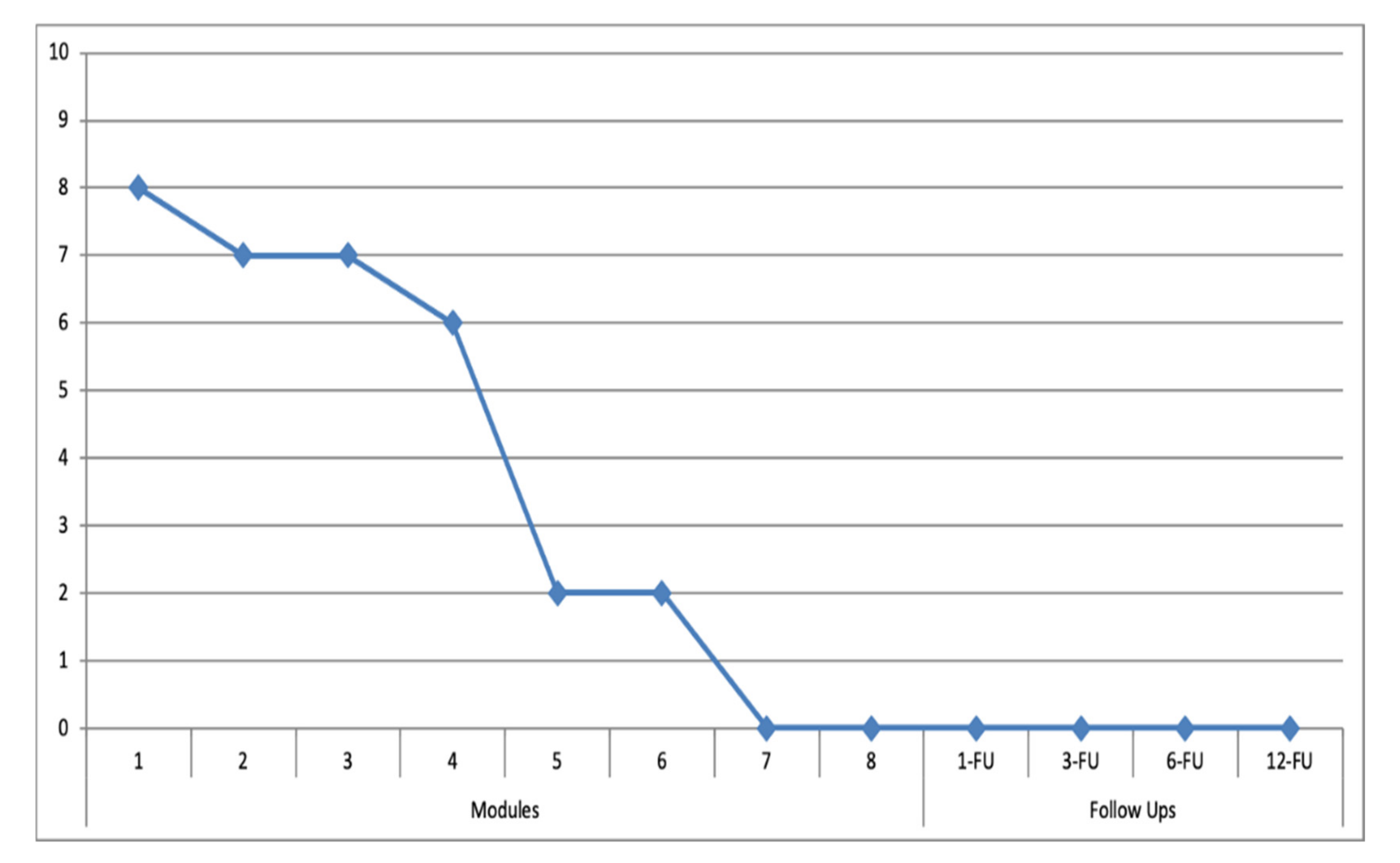
3.1. Target Behaviors
3.2. Expectations and Satisfaction regarding the SC/ERP + LBT-Based ICT System Components
3.2.1. Patient 1
3.2.2. Patient 2
3.3. Qualitative Interview
3.3.1. Domain 1: Usefulness
3.3.2. Domain 2: Improvements
3.3.3. Domain 3: Recommendation to Other People
3.3.4. Domain 4: Safety
3.3.5. Domain 5: Usability
3.3.6. Domain 6: Opinion for Using the App after Completing the Intervention
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Dowling, N.; Cowlishaw, S.; Jackson, A.C.; Merkouris, S.S.; Francis, K.; Christensen, D.R. Prevalence of Psychiatric Co-Morbidity in Treatment-Seeking Problem Gamblers: A Systematic Review and Meta-Analysis. Aust. N. Z. J. Psychiatry 2015, 49, 519–539. [Google Scholar] [CrossRef] [PubMed]
- Lorains, F.K.; Cowlishaw, S.; Thomas, S.A. Prevalence of Comorbid Disorders in Problem and Pathological Gambling: Systematic Review and Meta-Analysis of Population Surveys. Addiction 2011, 106, 490–498. [Google Scholar] [CrossRef]
- Håkansson, A.; Karlsson, A.; Widinghoff, C. Primary and Secondary Diagnoses of Gambling Disorder and Psychiatric Comorbidity in the Swedish Health Care System-A Nationwide Register Study. Front. Psychiatry 2018, 9, 426. [Google Scholar] [CrossRef] [PubMed]
- Rash, C.; Weinstock, J.; Van Patten, R. A Review of Gambling Disorder and Substance Use Disorders. Subst. Abus. Rehabil. 2016, 7, 3–13. [Google Scholar] [CrossRef] [PubMed]
- Chóliz, M.; Marcos, M.; Lázaro-Mateo, J. The Risk of Online Gambling: A Study of Gambling Disorder Prevalence Rates in Spain. Int. J. Ment. Health Addict. 2019, 19, 404–417. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-V), 5th ed.; APA: Washington, DC, USA, 2013. [Google Scholar]
- Becoña, E. Prevalencia Del Juego Patológico En Galicia Mediante El NODS. ¿Descenso de La Prevalencia o Mejor Evaluación Del Trastorno? Adicciones 2004, 16, 173–184. [Google Scholar] [CrossRef]
- Dirección General de Ordenación del Juego. Estudio Sobre Prevalencia, Comportamiento y Características de los Usuarios de Juegos de Azar en España. 2015. Available online: https://www.ordenacionjuego.es/es/estudio-prevalencia (accessed on 3 December 2019).
- Cowlishaw, S.; Merkouris, S.; Dowling, N.; Anderson, C.; Jackson, A.; Thomas, S. Psychological Therapies for Pathological and Problem Gambling. Cochrane Database Syst. Rev. 2012, 11, CD008937. [Google Scholar] [CrossRef]
- Choi, S.W.; Shin, Y.C.; Kim, D.J.; Choi, J.S.; Kim, S.; Kim, S.H.; Youn, H.C. Treatment Modalities for Patients with Gambling Disorder. Ann. Gen. Psychiatry 2017, 16, 23. [Google Scholar] [CrossRef]
- Labrador, M.; Labrador, F.J.; Crespo, M.; Echeburúa, E.; Becoña, E. Cognitive Distortions in Gamblers and Non-Gamblers of a Representative Spanish Sample. J. Gambl. Stud. 2020, 36, 207–222. [Google Scholar] [CrossRef]
- Menchon, J.M.; Mestre-Bach, G.; Steward, T.; Fernández-Aranda, F.; Jiménez-Murcia, S. An Overview of Gambling Disorder: From Treatment Approaches to Risk Factors. Wellcome Open Res. 2018, 7, 434. [Google Scholar] [CrossRef]
- Gooding, P.; Tarrier, N. A Systematic Review and Meta-Analysis of Cognitive-Behavioural Interventions to Reduce Problem Gambling: Hedging Our Bets? Behav. Res. Ther. 2009, 47, 592–607. [Google Scholar] [CrossRef]
- Goslar, M.; Leibetseder, M.; Muench, H.M.; Hofmann, S.G.; Laireiter, A.R. Efficacy of Face-to-Face versus Self-Guided Treatments for Disordered Gambling: A Meta-Analysis. J. Behav. Addict. 2017, 6, 142–162. [Google Scholar] [CrossRef] [PubMed]
- Riley, B.J.; Baigent, M.; Harris, S.; Larsen, A.; Nye, T.; Battersby, M. Extinction of Gambling Cue-Reactivity: A Pilot Study in a Problem Gambling Treatment Setting. J. Addict. Recover. 2018, 2, 1010. [Google Scholar] [CrossRef]
- Dowling, N.; Jackson, C.; Thomas, A. Behavioral Interventions in the Treatment of Pathological Gambling: A Review of Activity Scheduling and Desensitization. Int. J. Behav. Consult. Ther. 2008, 4, 172–187. [Google Scholar] [CrossRef]
- Riley, B.J.; Harris, S.; Nye, T.; Javidi-Hosseinabad, Z.; Baigent, M. Graded Exposure Therapy for Online Mobile Smartphone Sports Betting Addiction: A Case Series Report. J. Gambl. Stud. 2021, 37, 1263–1275. [Google Scholar] [CrossRef] [PubMed]
- Tolchard, B. Cognitive-Behaviour Therapy for Problem Gambling: A Critique of Current Treatments and Proposed Unified Approach. J. Ment. Health 2017, 26, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Symes, B.A.; Nicki, R.M. A preliminary consideration of cue-exposure, response-prevention treatment for pathological gambling behaviour: Two case studies. J. Gambl. Stud. 1997, 13, 145–157. [Google Scholar] [CrossRef]
- Tolchard, B.; Thomas, L.; Battersby, M. Single-session exposure therapy for problem gambling: A single-case experimental design. Behav. Chang. 2006, 23, 148–155. [Google Scholar] [CrossRef]
- Ginley, M.; Rash, C.; Petry, N. Psychological Interventions in Gambling Disorder. In Gambling Disorder; Heinz, A., Romanczuk-Seiferth, N., Potenza, M.N., Eds.; Springer International Publishing: Cham, Switzerland, 2019; pp. 181–194. [Google Scholar] [CrossRef]
- Buckingham, D. Media education and the end of the critical consumer. Harv. Educ. Rev. 2003, 73, 309–327. [Google Scholar] [CrossRef]
- Lozano-Blasco, R.; Latorre-Martínez, M.; Cortes-Pascual, A. Analizing Teens an Analysis from the Perspective of Gamers in Youtube. Sustainability 2021, 13, 11391. [Google Scholar] [CrossRef]
- Lozano-Blasco, R.; Quilez-Robres, A.; Delgado-Bujedo, D.; Latorre-Martínez, M.P. YouTube’s growth in use among children 0–5 during COVID19: The Occidental European case. Technol. Soc. 2021, 66, 101648. [Google Scholar] [CrossRef] [PubMed]
- Argyriou, E.; Davison, C.B.; Lee, T.T. Response inhibition and internet gaming disorder: A meta-analysis. Addict. Behav. 2017, 71, 54–60. [Google Scholar] [CrossRef]
- Wang, H.Y.; Cheng, C. The Associations Between Gaming Motivation and Internet Gaming Disorder: Systematic Review and Meta-analysis. JMIR Ment. Health 2022, 9, e23700. [Google Scholar] [CrossRef] [PubMed]
- Bouchard, S.; Robillard, G.; Giroux, I.; Jacques, C.; Loranger, C.; St-Pierre, M.; Chrétien, M.; Goulet, A. Using Virtual Reality in the Treatment of Gambling Disorder: The Development of a New Tool for Cognitive Behavior Therapy. Front. Psychiatry 2017, 8, 27. [Google Scholar] [CrossRef] [PubMed]
- García-Palacios, A.; Lasso, N.; Botella, C.; Baños, R.M.; Quero, S. Virtual Reality in the Treatment of Pathological Gambling. In Cyberpsychology & Behavior; Mary ann liebert Inc.: New Rochelle, NY, USA, 2006; Volume 9, pp. 706–707. [Google Scholar] [CrossRef]
- Park, C.B.; Park, S.M.; Gwak, A.R.; Sohn, B.K.; Lee, J.Y.; Jung, H.Y.; Choi, S.W.; Kim, D.J.; Choi, J.S. The effect of repeated exposure to virtual gambling cues on the urge to gamble. Addict. Behav. 2015, 41, 61–64. [Google Scholar] [CrossRef] [PubMed]
- González-Perellón, J.M.; Durón-Figueroa, R.; Bouchard, S.; Cárdenas-López, G. Evaluación de usabilidad, deseo de jugar y sentido de presencia en ambientes virtuales para el tratamiento del juego compulsivo. Psicol. Iberoam. 2021, 29, 1–18. [Google Scholar] [CrossRef]
- Bücker, L.; Bierbrodt, J.; Hand, I.; Wittekind, C.; Moritz, S. Effects of a Depression-Focused Internet Intervention in Slot Machine Gamblers: A Randomized Controlled Trial. PLoS ONE 2018, 13, e0198859. [Google Scholar] [CrossRef]
- Carlbring, P.; Smit, F. Randomized Trial of Internet-Delivered Self-Help with Telephone Support for Pathological Gamblers. J. Consult. Clin. Psychol. 2008, 76, 1090–1094. [Google Scholar] [CrossRef]
- Casey, L.M.; Oei, T.P.S.; Raylu, N.; Horrigan, K.; Day, J.; Ireland, M.; Clough, B.A. Internet-Based Delivery of Cognitive Behaviour Therapy Compared to Monitoring, Feedback and Support for Problem Gambling: A Randomised Controlled Trial. J. Gambl. Stud. 2017, 33, 993–1010. [Google Scholar] [CrossRef]
- Hodgins, D.C.; Cunningham, J.A.; Murray, R.; Hagopian, S. Online Self-Directed Interventions for Gambling Disorder: Randomized Controlled Trial. J. Gambl. Stud. 2019, 35, 635–651. [Google Scholar] [CrossRef]
- Nilsson, A.; Magnusson, K.; Carlbring, P.; Andersson, G.; Gumpert, C.H. The Development of an Internet-Based Treatment for Problem Gamblers and Concerned Significant Others: A Pilot Randomized Controlled Trial. J. Gambl. Stud. 2018, 34, 539–559. [Google Scholar] [CrossRef]
- Bücker, L.; Gehlenborg, J.; Moritz, S.; Westermann, S. A randomized controlled trial on a self-guided Internet-based intervention for gambling problems. Sci. Rep. 2021, 11, 13033. [Google Scholar] [CrossRef]
- Yakovenko, I.; Hodgins, D.C. Effectiveness of a voluntary casino self-exclusion online self-management program. Internet Interv. 2021, 23, 100354. [Google Scholar] [CrossRef]
- Dowling, N.A.; Merkouris, S.S.; Rodda, S.N.; Smith, D.; Aarsman, S.; Lavis, T.; Battersby, M.W. GamblingLess: A randomised trial comparing guided and unguided internet-based gambling interventions. J. Clin. Med. 2021, 10, 2224. [Google Scholar] [CrossRef] [PubMed]
- Jonas, B.; Leuschner, F.; Eiling, A.; Schoelen, C.; Soellner, R.; Tossmann, P. Web-based intervention and email-counseling for problem gamblers: Results of a randomized controlled trial. J. Gambl. Stud. 2020, 36, 1341–1358. [Google Scholar] [CrossRef] [PubMed]
- Petry, N.M.; Ginley, M.K.; Rash, C.J. A Systematic Review of Treatments for Problem Gambling. Psychol. Addict. Behav. 2017, 31, 951–961. [Google Scholar] [CrossRef] [PubMed]
- Paterson, M.; Whitty, M.; Boyer, C. An overview of digital and online strategies to reduce gambling harm. Health Promot. J. Aust. 2021, 32, 248–257. [Google Scholar] [CrossRef]
- Sagoe, D.; Griffiths, M.D.; Erevik, E.K.; Høyland, T.; Leino, T.; Lande, I.A.; Pallesen, S. Internet-based treatment of gambling problems: A systematic review and meta-analysis of randomized controlled trials. J. Behav. Addict. 2021, 10, 546–565. [Google Scholar] [CrossRef]
- Rodda, S.N. A Systematic Review of Internet Delivered Interventions for Gambling: Prevention, Harm Reduction and Early Intervention. J. Gambl. Stud. 2021, 1–25. [Google Scholar] [CrossRef]
- Santana, L.; Fontenelle, L. A Review of Studies Concerning Treatment Adherence of Patients with Anxiety Disorders. Patient Prefer. Adherence 2011, 5, 427–439. [Google Scholar] [CrossRef]
- Rush, B.; Scott, R.E. Approved Telehealth Outcome Indicator Guidelines: Quality, Access, Acceptability and Cost; University of Calgary: Calgary, Canada, 2004. [Google Scholar]
- Campos, D.; Mira, A.; Bretón-López, J.; Castilla, D.; Botella, C.; Baños, R.M.; Quero, S. The Acceptability of an Internet-Based Exposure Treatment for Flying Phobia with and without Therapist Guidance: Patients’ Expectations, Satisfaction, Treatment Preferences, and Usability. Neuropsychiatr. Dis. Treat. 2018, 14, 879–892. [Google Scholar] [CrossRef]
- Wallin, E.E.K.; Mattsson, S.; Olsson, E.M.G. The Preference for Internet-Based Psychological Interventions by Individuals Without Past or Current Use of Mental Health Treatment Delivered Online: A Survey Study with Mixed-Methods Analysis. JMIR Ment. Health 2016, 3, e25. [Google Scholar] [CrossRef] [PubMed]
- Greenberg, R.P.; Constantino, M.J.; Bruce, N. Are Patient Expectations Still Relevant for Psychotherapy Process and Outcome. Clin. Psychol. Rev. 2006, 26, 657–678. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.; García-Palacios, A.; Villa, H.; Baños, R.M.; Quero, S.; Alcañiz, M.; Riva, G. Virtual Reality Exposure in the Treatment of Panic Disorder and Agoraphobia: A Controlled Study. Clin. Psychol. Psychother. 2007, 14, 164–175. [Google Scholar] [CrossRef]
- Quero, S.; Pérez-Ara, M.A.; Bretón-López, J.; García-Palacios, A.; Baños, R.M.; Botella, C. Acceptability of Virtual Reality Interoceptive Exposure for the Treatment of Panic Disorder with Agoraphobia. Br. J. Guid. Counc. 2014, 42, 123–137. [Google Scholar] [CrossRef]
- Villa, H.; Botella, C.; García-Palacios, A.; Osma, J. Virtual Reality Exposure in the Treatment of Panic Disorder with Agoraphobia: A Case Study. Cogn. Behav. Pract. 2007, 14, 58–69. [Google Scholar] [CrossRef]
- Anderson, P.; Zimand, E.; Schmertz, S.K.; Ferrer, M. Usability and Utility of a Computerized Cognitive-Behavioral Self-Help Program for Public Speaking Anxiety. Cogn. Behav. Pract. 2007, 14, 198–207. [Google Scholar] [CrossRef]
- Botella, C.; Mira, A.; Moragrega, I.; García-Palacios, A.; Bretón-López, J.; Castilla, D.; Riera López del Amo, A.; Soler, C.; Molinari, G.; Quero, S.; et al. An Internet-Based Program for Depression Using Activity and Physiological Sensors: Efficacy, Expectations, Satisfaction, and Ease of Use. Neuropsychiatr. Dis. Treat. 2016, 12, 393–406. [Google Scholar] [CrossRef] [PubMed]
- Taylor, K.; Silver, L. Smartphone Ownership Is Growing Rapidly around the World, but Not Always Equally. Available online: https://www.pewresearch.org/global/2019/02/05/smartphone-ownership-is-growing-rapidly-around-the-world-but-not-always-equally/ (accessed on 26 February 2021).
- Rizvi, S.L.; Dimeff, L.A.; Skutch, J.; Carroll, D.; Linehan, M.M. A Pilot Study of the DBT Coach: An Interactive Mobile Phone Application for Individuals with Borderline Personality Disorder and Substance Use Disorder. Behav. Ther. 2011, 42, 589–600. [Google Scholar] [CrossRef]
- Linardon, J.; Cuijpers, P.; Carlbring, P.; Messer, M.; Fuller-Tyszkiewicz, M. The efficacy of app-supported smartphone interventions for mental health problems: A meta-analysis of randomized controlled trials. World Psychiatry 2019, 18, 325–336. [Google Scholar] [CrossRef]
- Hawker, C.O.; Merkouris, S.S.; Youssef, G.J.; Dowling, N.A. A smartphone-delivered ecological momentary intervention for problem gambling (GamblingLess: Curb Your Urge): Single-arm acceptability and feasibility trial. J. Med. Internet Res. 2021, 23, e25786. [Google Scholar] [CrossRef]
- Pfund, R.A.; Whelan, J.P.; Meyers, A.W.; Peter, S.C.; Ward, K.D.; Horn, T.L. The Use of a Smartphone Application to Complete Therapeutic Homework in Cognitive-Behavioral Therapy for Gambling Disorder: A Pilot Study of Acceptability and Feasibility. J. Technol. Behav. Sci. 2019, 5, 156–163. [Google Scholar] [CrossRef]
- So, R.; Furukawa, T.A.; Matsushita, S.; Baba, T.; Matsuzaki, T.; Furuno, S.; Okada, H.; Higuchi, S. Unguided Chatbot-Delivered Cognitive Behavioural Intervention for Problem Gamblers Through Messaging App: A Randomised Controlled Trial. J. Gambl. Stud. 2020, 36, 1391–1407. [Google Scholar] [CrossRef] [PubMed]
- Humphrey, G.; Chu, J.; Dowling, N.; Rodda, S.; Merkouris, S.; Parag, V.; Newcombe, D.; Ho, E.; Nosa, V.; Ruwhui-Collins, R.; et al. Manaaki–A cognitive behavioral therapy mobile health app to support people experiencing gambling problems: A randomized control trial protocol. BMC Public Health 2020, 20, 191. [Google Scholar] [CrossRef] [PubMed]
- Diaz-Sanahuja, L.; Campos, D.; Mira, A.; Castilla, D.; García-Palacios, A.; Bretón-López, J.M. Efficacy of an internet-based psychological intervention for problem gambling and gambling disorder: Study protocol for a randomized controlled trial. Internet Interv. 2021, 26, 100466. [Google Scholar] [CrossRef] [PubMed]
- Addepally, S.A.; Purkayastha, S. Mobile-Application Based Cognitive Behavior Therapy (CBT) for Identifying and Managing Depression and Anxiety. In International Conference on Digital Human Modeling and Applications in Health, Safety, Ergonomics and Risk Management; Springer: Cham, Switzerland; Vancouver, BC, Canada, 2017; pp. 3–12. [Google Scholar] [CrossRef]
- Olbrich, H.; Stengler, K.; Olbrich, S. Smartphone Based Geo-Feedback in Obsessive Compulsive Disorder as Facilitatory Intervention: A Case Report. J. Obs. Compuls. Relat. Disord. 2016, 8, 75–78. [Google Scholar] [CrossRef]
- Miralles, I.; Granell, C.; García-Palacios, A.; Castilla, D.; González-Pérez, A.; Casteleyn, S.; Bretón-López, J. Enhancing In Vivo Exposure in the Treatment of Panic Disorder and Agoraphobia Using Location-Based Technologies: A Case Study. Clin. Case Stud. 2019, 19, 145–159. [Google Scholar] [CrossRef]
- Humphrey, G.; Newcombe, D.; Whittaker, R.; Parag, V.; Bullen, C. SPGeTTI: A Smartphone-Based Problem Gambling Evaluation and Technology Testing Initiative Final Report; The Univeristy of Auckland: Wellington, New Zealand, 2019. [Google Scholar]
- Gerstein, D.; Volberg, R.A.; Toce, M.T.; Harwood, H.; Johnson, R.A.; Buie, T.; Sinclair, S. Gambling Impact and Behavior Study: Report to the National Gambling Impact Study Commission; National Opinion Research Center: Chicago, IL, USA, 1999. [Google Scholar]
- Marks, I.M.; Mathews, A.M. Brief Standard Self-Rating for Phobic Patients. Behav. Res. Ther. 1979, 17, 263–267. [Google Scholar] [CrossRef]
- Borkovec, T.D.; Nau, S.D. Credibility of Analogue Therapy Rationales. J. Behav. Ther. Exp. Psychiatry 1972, 3, 257–260. [Google Scholar] [CrossRef]
- Botella, C.; Gallego, M.J.; Garcia-Palacios, A.; Baños, R.M.; Quero, S.; Alcañiz, M. The Acceptability of an Internet-Based Self-Help Treatment for Fear of Public Speaking. Br. J. Guid. Couns. 2009, 37, 297–311. [Google Scholar] [CrossRef]
- Brooke, J. System Usability Scale (SUS). Usability Evaluation in Industry; Taylor and Francis: London, UK, 1996. [Google Scholar]
- Hill, C.E.; Knox, S.; Thompson, B.J.; Williams, E.N.; Hess, S.A.; Ladany, N. Consensual qualitative research: An update. J. Couns. Psychol. 2005, 52, 196–205. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Hill, C.E.; Thompson, B.J.; Williams, E.N. A guide to conducting consensual qualitative research. Couns. Psychol. 1997, 25, 517–572. [Google Scholar] [CrossRef]
- Bangor, A.; Kortum, P.T.; Miller, J.T. An Empirical Evaluation of the System Usability Scale. Int. J. Hum. Comput. Interact. 2008, 24, 574–594. [Google Scholar] [CrossRef]
- Oakes, J.; Pols, R.; Lawn, S. The ‘Merry-Go-Round’of Habitual Relapse: A Qualitative Study of Relapse in Electronic Gaming Machine Problem Gambling. Int. J. Environ. Res. Public Health 2019, 16, 2858. [Google Scholar] [CrossRef]
- Hodgins, D.C.; el-Guebaly, N. The influence of substance dependence and mood disorders on outcome from pathological gambling: Five-Year follow-up. J. Gamb. Stud. 2010, 26, 117–127. [Google Scholar] [CrossRef]
- Jiménez-Murcia, S.; Tremblay, J.; Stinchfield, R.; Granero, R.; Fernández-Aranda, F.; Mestre-Bach, G.; Steward, T.; Del Pino-Gutiérrez, A.; Baño, M.; Moragas, L.; et al. The involvement of a concerned significant other in gambling disorder treatment outcome. J. Gambl. Stud. 2017, 33, 937–953. [Google Scholar] [CrossRef]
- Hawker, C.O.; Merkouris, S.S.; Youssef, G.J.; Dowling, N.A. Exploring the associations between gambling cravings, self-efficacy, and gambling episodes: An Ecological Momentary Assessment study. Addict. Behav. 2021, 112, 106574. [Google Scholar] [CrossRef]
- Mira, A.; Soler, C.; Alda, M.; Baños, R.; Castilla, D.; Castro, A.; García-Campayo, J.; García-Palacios, A.; Gili, M.; Hurtado, M.; et al. Exploring the Relationship between the Acceptability of an Internet-Based Intervention for Depression in Primary Care and Clinical Outcomes: Secondary Analysis of a Randomized Controlled Trial. Front. Psychiatry 2019, 10, 325. [Google Scholar] [CrossRef]
- Carvalho, M.D.; Guimarães, H.; Ferreira, J.B.; Freitas, A. Intention to Use M-Learning: An Extension of the Technology Acceptance Model. In 19th International Conference on Recent Advances in Retailing and Consumer Services Science; ANPAD: Maringá, Brazil, 2012; pp. 9–12. [Google Scholar]
- Huang, T.-L.; Liao, S. A Model of Acceptance of Augmented-Reality Interactive Technology: The Moderating Role of Cognitive Innovativeness. Electron. Commer. Res. 2015, 15, 269–295. [Google Scholar] [CrossRef]
- Jokela, T.; Iivari, N.; Matero, J.; Karukka, M. The Standard of User-Centered Design and the Standard Definition of Usability: Analyzing ISO 13407 against ISO 9241-11. In Proceedings of the Latin American Conference on Human-Computer Interaction; Association for Computing Machinery: New York, NY, USA, 2003; pp. 53–60. [Google Scholar] [CrossRef]
- Marchica, L.; Derevensky, J.L. Examining Personalized Feedback Interventions for Gambling Disorders: A Systematic Review. J. Behav. Addict. 2016, 5, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Peter, S.C.; Brett, E.I.; Suda, M.T.; Leavens, E.L.S.; Miller, M.B.; Leffingwell, T.R.; Whelan, J.P.; Meyers, A.W. A meta-analysis of brief personalized feedback interventions for problematic gambling. J. Gambl. Stud. 2019, 35, 447–464. [Google Scholar] [CrossRef]
- Aragay, N.; Jiménez-Murcia, S.; Granero, R.; Fernández-Aranda, F.; Ramos-Grille, I.; Cardona, S.; Garrido, G.; Anisul Islam, M.; Menchón, J.M.; Vallès, V. Pathological Gambling: Understanding Relapses and Dropouts. Compr. Psychiatry 2015, 57, 58–64. [Google Scholar] [CrossRef]
- Miralles, I.; Granell, C.; Díaz-Sanahuja, L.; Van Woensel, W.; Bretón-López, J.; Mira, A.; Castilla, D.; Casteleyn, S. Smartphone Apps for the Treatment of Mental Disorders: Systematic Review. JMIR mHealth uHealth 2020, 8, e14897. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.M.; Juan, M.C.; Baños, R.M.; Alcañiz, M.; Guillén, V.; Rey, B. Mixing realities? An application of augmented reality for the treatment of cockroach phobia. Cyberpsychology Behav. 2005, 8, 162–171. [Google Scholar] [CrossRef]
- Wrzesien, M.; Botella, C.; Bretón-López, J.; del Río González, E.; Burkhardt, J.M.; Alcañiz, M.; Pérez-Ara, M.A. Treating small animal phobias using a projective-augmented reality system: A single case study. Comput. Hum. Behav. 2015, 49, 343–353. [Google Scholar] [CrossRef]
- Botella, C.; Bretón-López, J.; Quero, S.; Baños, R.; García-Palacios, A. Treating cockroach phobia with augmented reality. Behav. Ther. 2010, 41, 401–413. [Google Scholar] [CrossRef] [PubMed]
- Botella, C.; Pérez-Ara, M.A.; Bretón-López, J.; Quero, S.; García-Palacios, A.; Baños, R.M. In vivo versus augmented reality exposure in the treatment of small animal phobia: A randomized controlled trial. PLoS ONE 2016, 11, e0148237. [Google Scholar] [CrossRef]
- Campbell, D.T.; Stanley, J.C. Experimental and Quasi-Experimental Designs for Research; Rand McNally: Chicago, IL, USA, 1963. [Google Scholar]
- Kazdin, A.E. Drawing valid inferences from case studies. J. Consult. Clin. Psychol. 1981, 49, 183–192. [Google Scholar] [CrossRef]


| Module | Objectives | Contents |
|---|---|---|
| M1. Motivation for change. | Providing information about the specific program and increasing motivation for change. |
|
| M2. Psychoeducation. | Understanding gambling. |
|
| M3. Stimulus control and responsible return of debts. | Gambling cessation and commitment to returning debts responsibly. |
|
| M4. Cognitive restructuring | Identification and correction of thoughts that contribute to GD onset and maintenance. |
|
| M5. Emotion regulation | Identifying emotions and understanding its function and how to tolerate and change emotional responses. |
|
| M6. Planning of significant activities | Lifestyle balance. |
|
| M7. Coping skills and exposure with response prevention | Habituation to the gambling conditioned stimulus without gambling. |
|
| M8. Relapse prevention | Avoiding relapses and maintain changes gained through the intervention. |
|
| Items | First Use | After Intervention |
|---|---|---|
| 1: I think that I would like to use this system frequently | 4 | 4 |
| 2: I found the system unnecessarily complex | 1 | 1 |
| 3: I thought the system was easy to use | 5 | 5 |
| 4: I think that I would need the support of a technical person to be able to use this system | 1 | 1 |
| 5: I found that the various functions in this system were well integrated | 5 | 4 |
| 6: I thought that there was too much inconsistency in this system | 2 | 1 |
| 7: I would imagine that most people would learn to use this system very quickly | 5 | 5 |
| 8: I found the system very cumbersome to use | 1 | 1 |
| 9: I felt very confident using the system | 2 | 4 |
| 10: I needed to learn a lot of things before I could get going with this system | 1 | 1 |
| Items | First Use | After Intervention |
|---|---|---|
| 1: I think that I would like to use this system frequently | 5 | 5 |
| 2: I found the system unnecessarily complex | 1 | 1 |
| 3: I thought the system was easy to use | 5 | 5 |
| 4: I think that I would need the support of a technical person to be able to use this system | 1 | 1 |
| 5: I found that the various functions in this system were well integrated | 5 | 5 |
| 6: I thought that there was too much inconsistency in this system | 1 | 1 |
| 7: I would imagine that most people would learn to use this system very quickly | 5 | 5 |
| 8: I found the system very cumbersome to use | 1 | 1 |
| 9: I felt very confident using the system | 5 | 5 |
| 10: I needed to learn a lot of things before I could get going with this system | 1 | 1 |
| Domains | Categories (Frequency) | Illustrative Core Idea |
|---|---|---|
| Usefulness | Vigilance (13) | The sensation the app offers of being observed is an advantage, and it gives one the confidence to be abstinent. |
| Lapse/relapse prevention (11) | Messages such as “It is not a good idea to be here” or “we recommend you leave this place” were useful to cope with gambling urges when risk situations were present and to avoid lapses. | |
| Stimuli control (10) | The tool helps prevent being at risk situations such as gambling-related venues. | |
| Accompaniment/protection (6) | It supports one throughout the intervention and protects from gambling activities. | |
| Reduction of the lapse/relapse duration (5) | The fact that one receives support messages for leaving the gambling activity when a lapse is produced could be useful to reduce the lapse’s duration and to avoid a relapse. | |
| Gambling urges habituation (1) | The app helped to stay in the gambling situation without betting until the gambling urges decreased and the ability to cope with gambling urges increased. | |
| Improvements | Adding places to the app by contrasting the information with the co-therapist (5) | It could be interesting to contrast the information with the co-therapist about the different gambling venues patients used to go to. |
| Increasing the feedback to the therapist (4) | It would be relevant for therapists to know the amount of time patients spend at every site that could be related to gambling activities in order to increase control over patients and protect them. | |
| Rise of the emotional impact of the messages (3) | Messages could be related to the negative consequences of gambling with a higher emotional effect in order to influence people to stop gambling when located at a gambling venue. | |
| Therapist assistance during a risky lapse situation (2) | The therapist could receive more information about the patient’s location for increasing support when they are in a risky situation or in the face-to-face therapy sessions. | |
| Recommendation to other people | Extra support for other people suffering gambling problems (3) | The use of the app would be recommended to other people with gambling problems because it has several advantages (e.g., accompaniment for increasing self-efficacy to cope with gambling urges and preventing lapses). |
| Assistance in the treatment of other psychological problems (1) | This tool could be useful for the treatment of other addictions, for instance, regarding cocaine, marijuana, or alcohol substances. | |
| Safety | Confidence (8) | The app gives one the confidence that it can help because it accomplishes the function of guiding in coping with gambling problems. |
| Intrusiveness (2) | The sensation of discomfort or insecurity due to aspects of threats to confidentiality using this technology only are present at the initial moment. | |
| Usability | Ease of installation (5) | The procedure to download and install the application was easy. |
| Ease of use throughout the intervention (7) | Once the app is installed and you have activated the location-based position it functions autonomously and it is easy. | |
| Opinion for using the app after completing the intervention | Support to be abstinent (6) | The use of the app after completing the intervention, it can help cope with gambling urges and to be abstinent. |
| Severity of gambling-related symptomatology (3) | Depending on the gambling severity symptoms it could be convenient to continue using the app after the intervention. In more severe cases it would be useful to remind patients when they are at risk situations and avoid lapses. | |
| Updating (2) | It could be convenient to use the app after the intervention updating the risky gambling-related places, because routines can change over time. |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Diaz-Sanahuja, L.; Miralles, I.; Granell, C.; Mira, A.; González-Pérez, A.; Casteleyn, S.; García-Palacios, A.; Bretón-López, J. Client’s Experiences Using a Location-Based Technology ICT System during Gambling Treatments’ Crucial Components: A Qualitative Study. Int. J. Environ. Res. Public Health 2022, 19, 3769. https://doi.org/10.3390/ijerph19073769
Diaz-Sanahuja L, Miralles I, Granell C, Mira A, González-Pérez A, Casteleyn S, García-Palacios A, Bretón-López J. Client’s Experiences Using a Location-Based Technology ICT System during Gambling Treatments’ Crucial Components: A Qualitative Study. International Journal of Environmental Research and Public Health. 2022; 19(7):3769. https://doi.org/10.3390/ijerph19073769
Chicago/Turabian StyleDiaz-Sanahuja, Laura, Ignacio Miralles, Carlos Granell, Adriana Mira, Alberto González-Pérez, Sven Casteleyn, Azucena García-Palacios, and Juana Bretón-López. 2022. "Client’s Experiences Using a Location-Based Technology ICT System during Gambling Treatments’ Crucial Components: A Qualitative Study" International Journal of Environmental Research and Public Health 19, no. 7: 3769. https://doi.org/10.3390/ijerph19073769
APA StyleDiaz-Sanahuja, L., Miralles, I., Granell, C., Mira, A., González-Pérez, A., Casteleyn, S., García-Palacios, A., & Bretón-López, J. (2022). Client’s Experiences Using a Location-Based Technology ICT System during Gambling Treatments’ Crucial Components: A Qualitative Study. International Journal of Environmental Research and Public Health, 19(7), 3769. https://doi.org/10.3390/ijerph19073769











