VAD Patients’ Perception of Potential Telemedicine Support
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Ethical Approval
2.3. Description of the Questionnaire
2.4. Statistical Analysis
3. Results
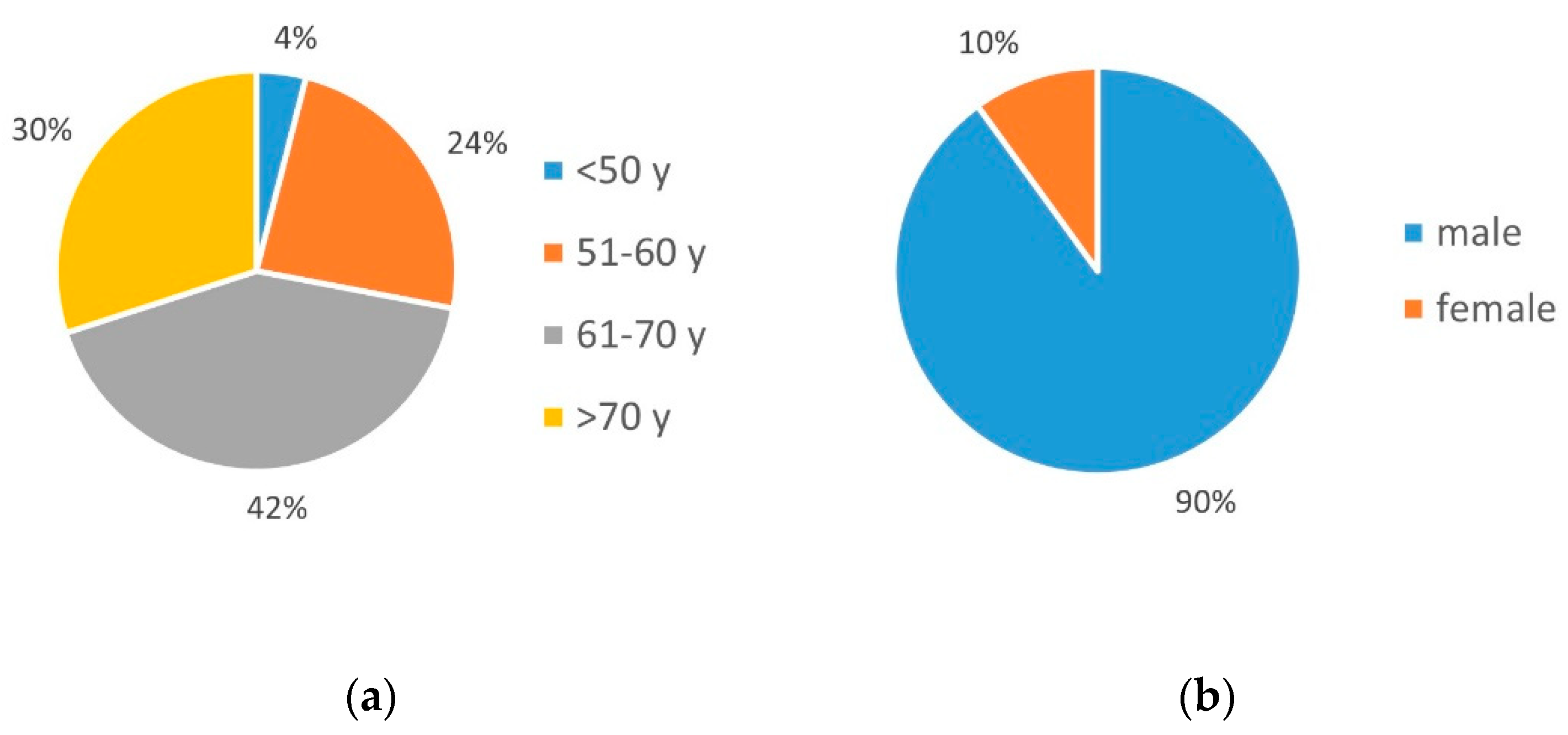
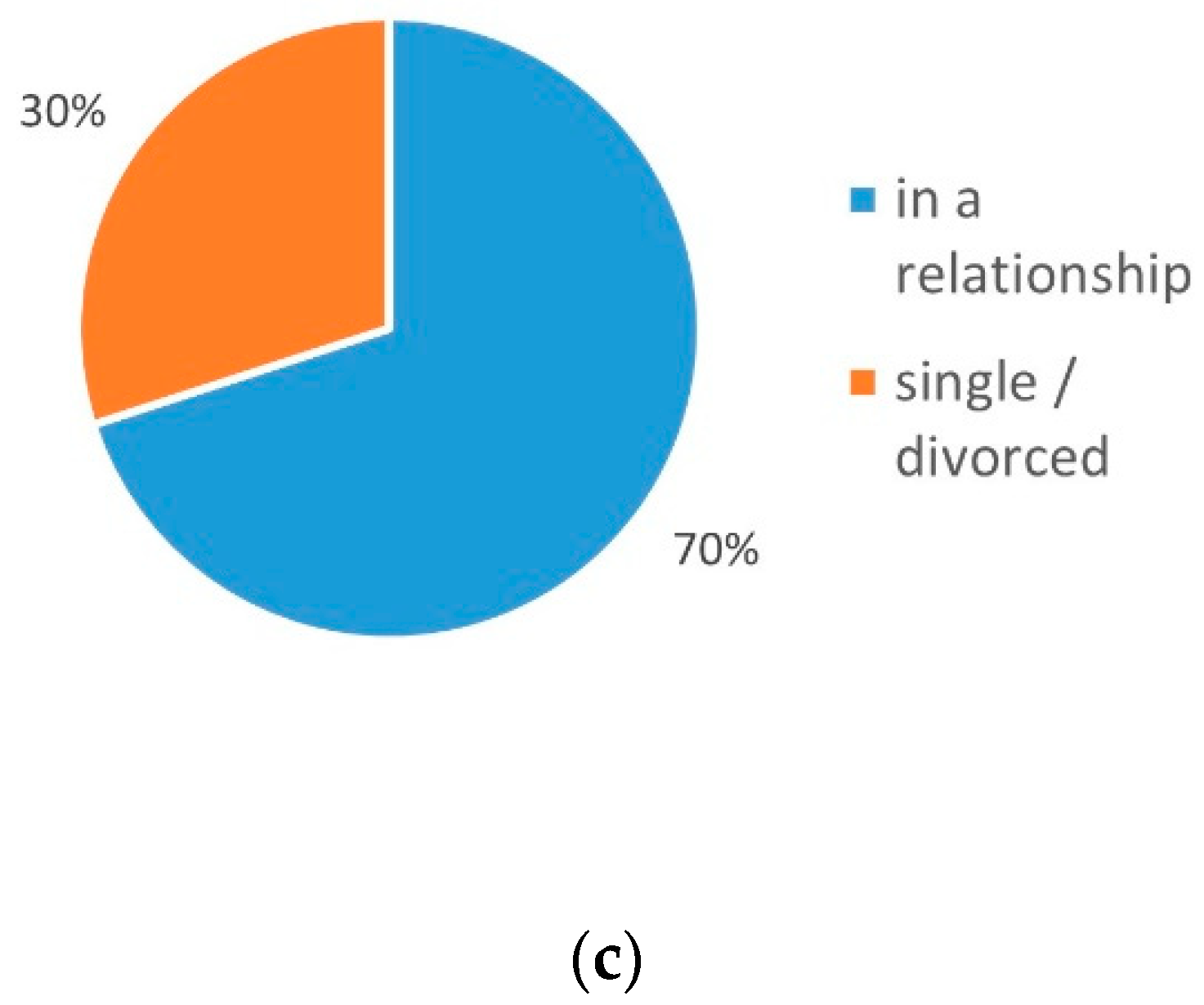
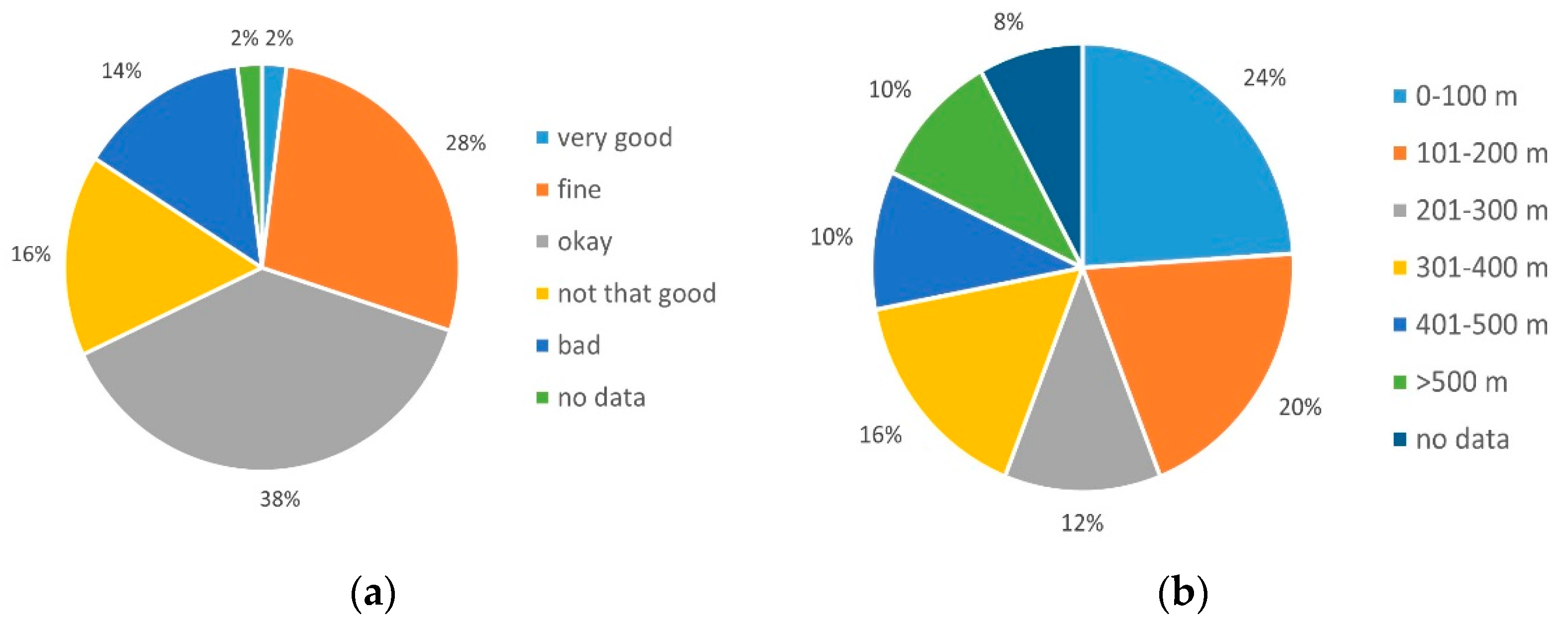
3.1. Population Characteristics
3.2. Device-Related Clinical Contacts
3.3. Acceptance and Concerns about a Telemedical Connection
- (1)
- Improvement of the health situation or the state of care;
- (2)
- Easier access to help;
- (3)
- Privacy and discomfort;
- (4)
- Patients’ concerns about the staff involved;
- (5)
- Telemedicine use as a complement to face-to-face contact;
- (6)
- Potential satisfaction with telemedicine application.
3.3.1. Improvement of the Health Situation/the Condition of Care
3.3.2. Easier Access Help
3.3.3. Privacy
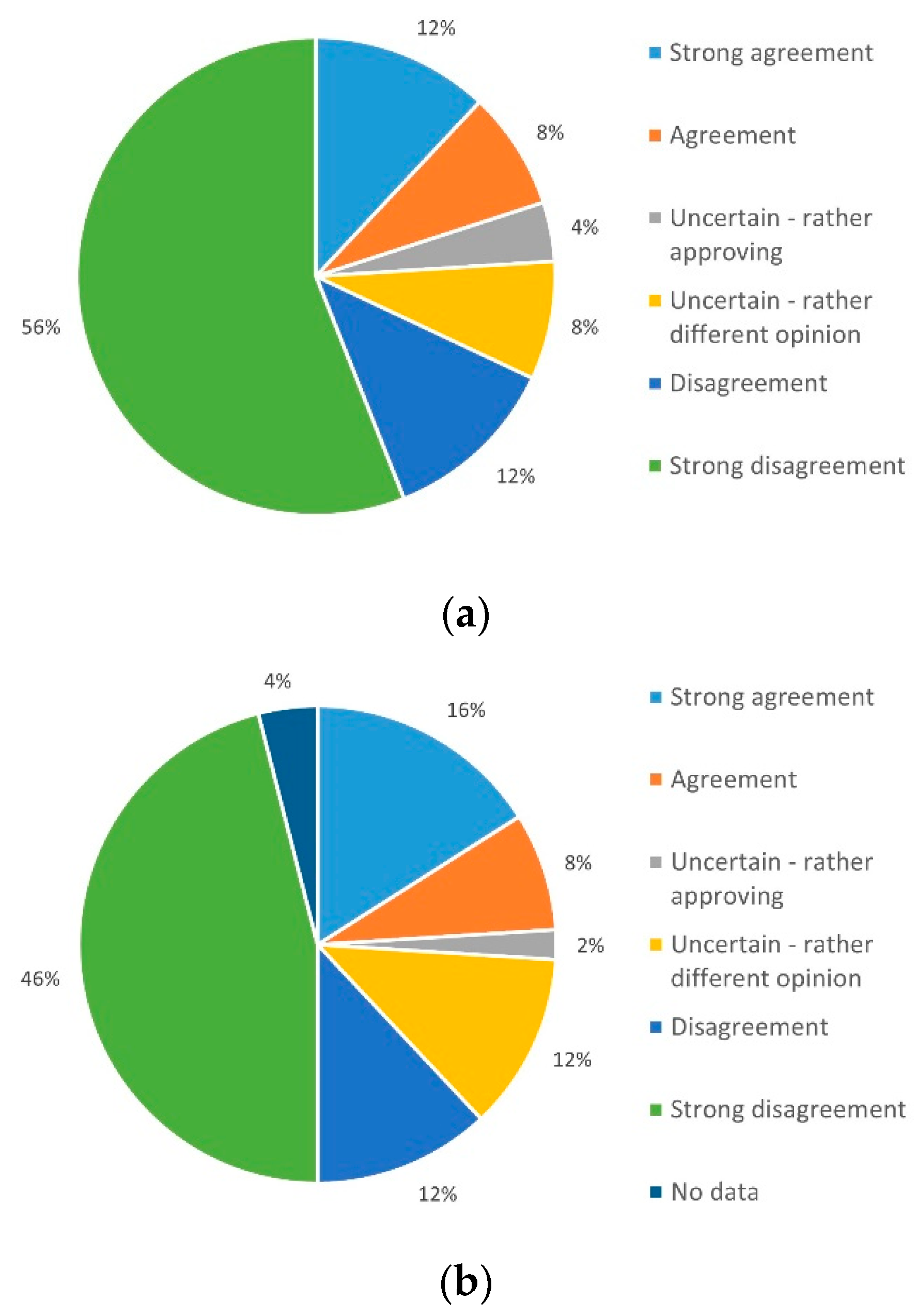
3.3.4. Concerns about the Quality of Care
3.3.5. Telemedicine as a Supplement
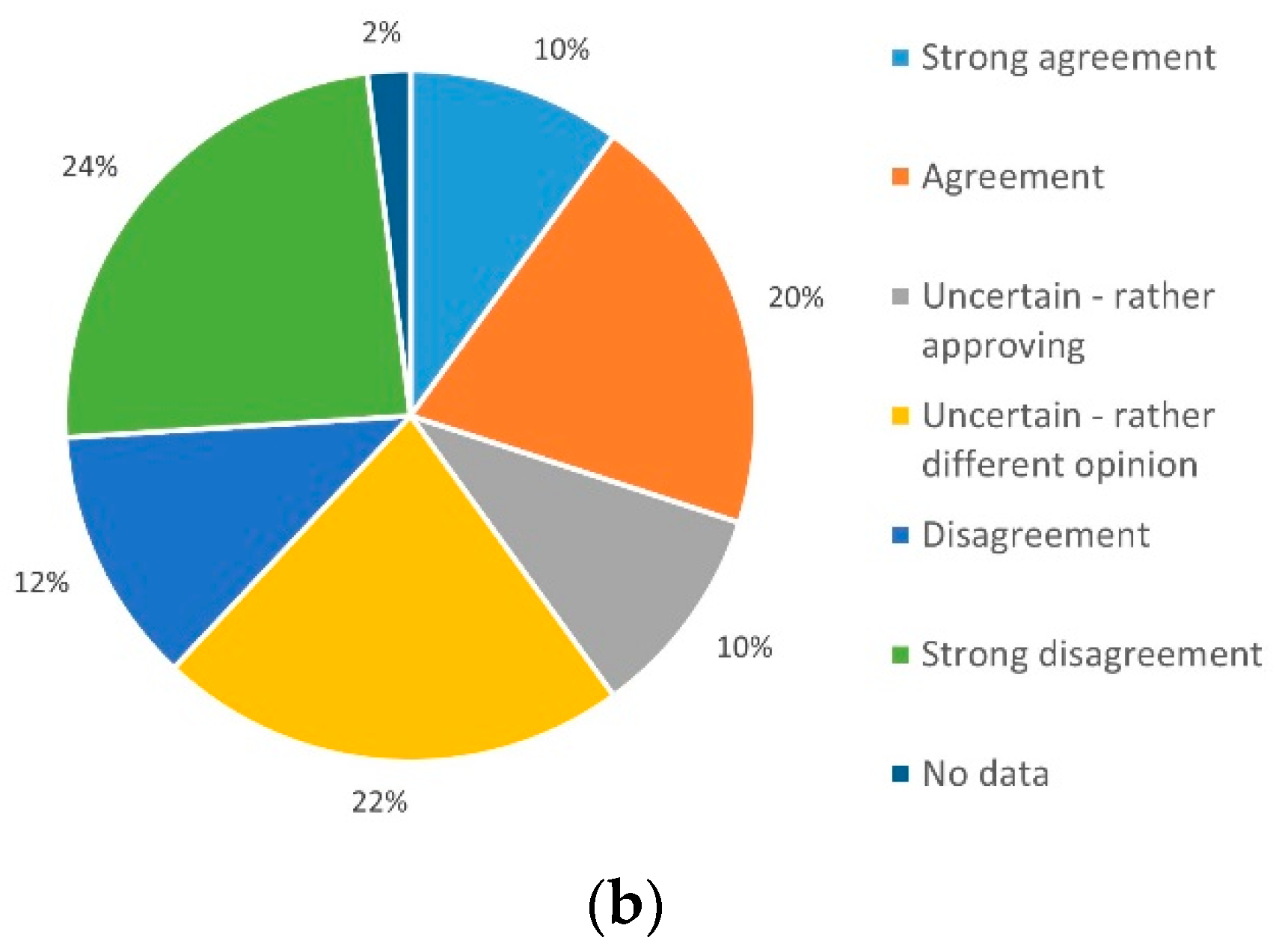
3.3.6. Potential Satisfaction with a Telemedical Application
4. Discussion
5. Conclusions
6. Limitations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Bundesausschuss, G. IQTIG_Qualitaetsreport 2020. 2020. Available online: https://iqtig.org/downloads/berichte/2019/IQTIG_Qualitaetsreport-2020_2021-02-11.pdf (accessed on 15 March 2022).
- Marx, G.; Rossaint, R.; Marx, N. Telekooperation—Telemonitoring—Teletherapie: Begriffserklärungen, in Telemedizin—Grundlagen und Praktische Anwendung in Stationären und Ambulanten Einrichtungen. 2020. Available online: https://ebin.pub/telemedizin-grundlagen-und-praktische-anwendung-in-stationren-und-ambulanten-einrichtungen-1-aufl-9783662606100-9783662606117.html (accessed on 15 March 2022).
- Reiss, N.; Schmidt, T.; Boeckelmann, M.; Schulte-Eistrup, S.; Hoffmann, J.D.; Feldmann, C.; Schmitto, J.D. Telemonitoring of left-ventricular assist device patients-current status and future challenges. J. Thorac. Dis. 2018, 10, S1794–S1801. [Google Scholar] [CrossRef] [PubMed]
- Contreras, C.M.; Metzger, G.A.; Beane, J.D.; Dedhia, P.H.; Ejaz, A.; Pawlik, T.M. Telemedicine: Patient-Provider Clinical Engagement During the COVID-19 Pandemic and Beyond. J. Gastrointest. Surg. 2020, 24, 1692–1697. [Google Scholar] [CrossRef] [PubMed]
- Grosman-Dziewiszek, P.; Wiatrak, B.; Jęśkowiak, I.; Szeląg, A. Patients’ Habits and the Role of Pharmacists and Telemedicine as Elements of a Modern Health Care System during the COVID-19 Pandemic. J. Clin. Med. 2021, 10, 4211. [Google Scholar] [CrossRef] [PubMed]
- Hirani, S.P.; Rixon, L.; Beynon, M.; Cartwright, M.; Cleanthous, S.; Selva, A.; Sanders, C.; Newman, S.P. Quantifying beliefs regarding telehealth: Development of the Whole Systems Demonstrator Service User Technology Acceptability Questionnaire. J. Telemed. Telecare 2017, 23, 460–469. [Google Scholar] [CrossRef] [PubMed]
- Mayring, P. Qualitative Inhaltsanalyse. Grundlagen und Techniken. 12., Überarbeitete 2012. Available online: https://www.beltz.de/fileadmin/beltz/leseproben/978-3-407-25730-7.pdf (accessed on 15 March 2022).
- Schloeglhofer, T.; Horvat, J.; Moscato, F.; Hartner, Z.; Necid, G.; Schwingenschloegl, H.; Riebandt, J.; Dimitrov, K.; Angleitner, P.; Wiedemann, D.; et al. A Standardized Telephone Intervention Algorithm Improves the Survival of Ventricular Assist Device Outpatients. Artif. Organs 2018, 42, 961–969. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Casida, J.M.; Aikens, J.E.; Craddock, H.; Aldrich, M.W.; Pagani, F.D. Development and Feasibility of Self-Management Application in Left-Ventricular Assist Devices. ASAIO J. 2018, 64, 159–167. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, T.; Mewes, P.; Hoffmann, J.D.; Müller-von Aschwege, F.; Glitza, J.I.; Schmitto, J.D.; Schulte-Eistrup, S.; Sindermann, J.R.; Reiss, N. Improved aftercare in LVAD patients: Development and feasibility of a smartphone application as a first step for telemonitoring. Artif. Organs 2020, 44, 248–256. [Google Scholar] [CrossRef] [PubMed]




| Hospital Contacts | ||
|---|---|---|
| Days of inpatient stay in 2017 Days of inpatient stay in 2018 | 19.48 | (max 70) |
| 11.42 | (max 60) | |
| Visits in outpatient ward/12 months | 6.81 |
| Efforts to Reach the Clinic | ||
|---|---|---|
| Distance residence-to-clinic | 49.63 km | (max 260 km) |
| Time to reach the clinic | <30 min: 48% | >30 min: 52% |
| Difficult to get to the clinic | No: 48% | Yes/partially: 52% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berg, T.; Benstoem, C.; Moza, A.K. VAD Patients’ Perception of Potential Telemedicine Support. Int. J. Environ. Res. Public Health 2022, 19, 3768. https://doi.org/10.3390/ijerph19073768
Berg T, Benstoem C, Moza AK. VAD Patients’ Perception of Potential Telemedicine Support. International Journal of Environmental Research and Public Health. 2022; 19(7):3768. https://doi.org/10.3390/ijerph19073768
Chicago/Turabian StyleBerg, Thomas, Carina Benstoem, and Ajay K. Moza. 2022. "VAD Patients’ Perception of Potential Telemedicine Support" International Journal of Environmental Research and Public Health 19, no. 7: 3768. https://doi.org/10.3390/ijerph19073768
APA StyleBerg, T., Benstoem, C., & Moza, A. K. (2022). VAD Patients’ Perception of Potential Telemedicine Support. International Journal of Environmental Research and Public Health, 19(7), 3768. https://doi.org/10.3390/ijerph19073768






